Abstract
Purpose
To determine the effect of a 45° reclining sitting posture on swallowing in patients with dysphagia.
Materials and Methods
Thirty-four patients with dysphagia were evaluated. Videofluoroscopic swallowing study was performed for each patient in 90° upright and in 45° reclining sitting posture. Patients swallowed 5 types of boluses twice: sequentially 2 mL thin liquid, 5 mL thin liquid, thick liquid, yogurt, and cooked rice. Data such as the penetration-aspiration scale (PAS), oral transit time (OTT), pharyngeal delay time (PDT), pharyngeal transit time (PTT), residue in valleculae and pyriform sinuses, premature bolus loss, and nasal penetration were obtained.
Results
The mean PAS on the 2 mL thin liquid decreased significantly in the 45° reclining sitting posture (p=0.007). The mean PAS on 5 mL thin liquid in the 45° reclining sitting posture showed decreasing tendency. The residue in valleculae decreased significantly for all boluses in the 45° reclining sitting posture (p<0.001, p=0.002, p=0.003, p<0.001, p=0.020, respectively). The residue in pyriform sinuses increased significantly on 5 mL thin liquid, thick liquid, and yogurt (p=0.031, p=0.020, p=0.002, respectively). There were no significant differences in OTT, PDT, PTT, premature bolus loss, and nasal penetration between both postures.
Conclusion
PAS on 2 mL thin liquid and residue in valleculae on all types of boluses were decreased in a 45° reclining sitting posture. Therefore, we believe that the 45° reclining sitting posture on swallowing is beneficial for the patients with penetration or aspiration on small amounts of thin liquid and large amounts of residue in valleculae.
Keywords: Dysphagia, posture, swallowing
INTRODUCTION
Dysphagia develops from various diseases of the central nervous system, such as stroke, brain tumors, and traumatic brain injury, as well as oral and laryngopharyngeal tumors and head and neck surgery.1 When dysphagia develops, patients cannot easily ingest food, and this can cause aspiration of the lower respiratory system and complications, such as pneumonia, bronchitis, pulmonary abscess, and sepsis.2 Thus, appropriate evaluation and treatment in the early phase of dysphagia are critical to reduce the danger of developing complications and the length of stay in hospital.3,4
In general, various rehabilitation methods for dysphagia are used clinically, such as stimulation, dietary modification using changes of viscosity or size, swallowing exercise, postural techniques, and swallowing maneuvers. Among these, postural techniques are used to change the patients' environment, but not their swallowing function, to compensate for anatomical and physiological deficiencies. These postural methods can reduce airway aspiration by changing the passage and speed of ingested food, which is good for patients who are in the early phases, or before recovery or before the treatment effects of dysphagia appear.2,4,5
Among various dysphagia evaluation methods, the videofluoroscopic swallowing study (hereafter VFSS) is a standard test that is currently most commonly used. It can give the functional anatomy-based visual and time information during swallowing; thus, it is a useful test.3,6 However, in many cases of acute patients, it is difficult to evaluate them in an upright sitting position with the VFSS method. It was observed, for example, that the patients who were experiencing the early stages of stroke experienced difficulties during the test because of their weakened trunk muscles and balance impairment. In the case of spinal cord injury patients, they also have difficulties in maintaining a sitting posture during the test because of orthostatic hypotension symptoms and a weakness of the trunk muscle. Thus, we tried testing on a 45° reclining sitting position instead of usual 90° upright sitting position.
There are a few research articles on the effects of various postures on swallowing. Rasley, et al.7 reported that the lateral decubitus posture reduces aspiration in oropharyngeal dysphagia patients, Larnert and Ekberg8 reported that 30 degrees of leaning back while sitting was good enough to reduce aspiration in cerebral palsy patients, and Ha, et al.9 reported that the supine position reduces aspiration in the cases of neurogenic dysphagia patients. However, previous research did not use various objective and specific results of the VFSS test.
In this study, we compared the objective results of two sitting postures, sitting up at 90° and leaning back at 45°, using VFSS.
MATERIALS AND METHODS
Subjects
Outpatients and inpatients of the Department of Physical Medicine and Rehabilitation at Chonbuk National University Hospital during March and September 2011 were recruited. We also recruited patients who had symptoms of dysphagia, such as coughing or choking during their meal, referred to our department from other departments. However, several patients who could not maintain their posture for the VFSS test or who could not follow the instructions during the test because of impaired cognitive function were excluded. Total thirty-four patients were participated in this study (25 males and 9 females, with a mean age of 58.2 years). Patient's characteristics are described in Table 1.
Table 1.
Characteristics of Patients
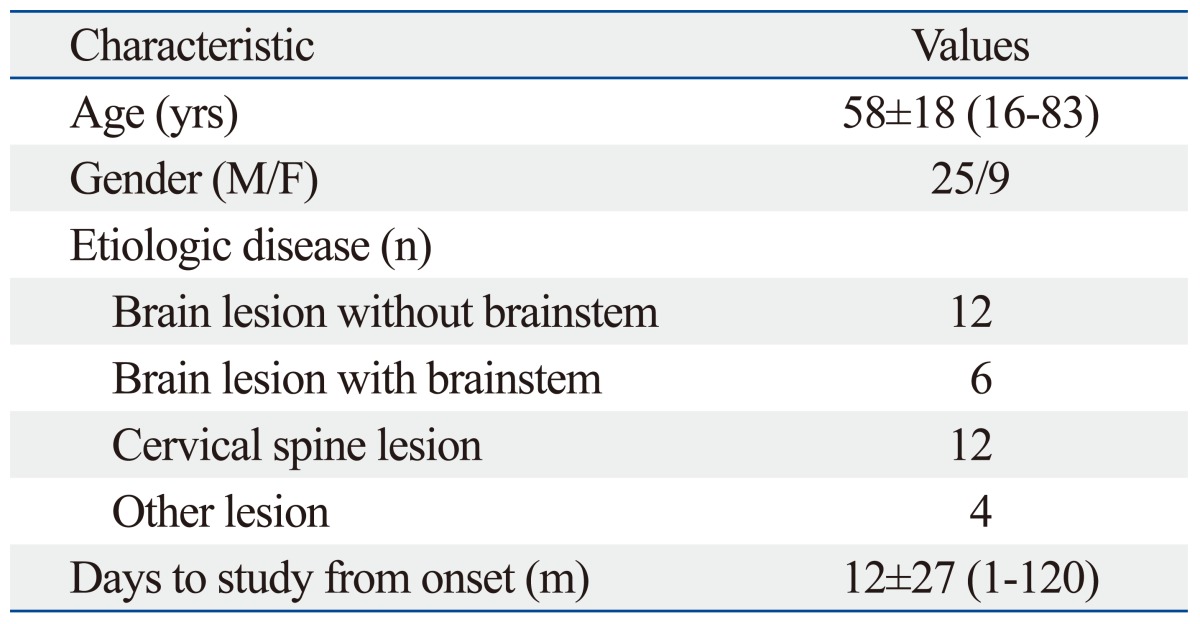
Age and days to study from onset values presented as mean±SD (range).
Methods
Videofluoroscopic swallowing study (VFSS)
The VFSS of dysphagia patients was conducted by a rehabilitation doctor in the videofluoroscopic test room. While fluoroscopically watching the lateral side of the subjects sitting up at 90°, they were asked to swallow 2 mL of thin liquid, 5 mL of thin liquid, thick liquid, yogurt, and rice in turn, two times each. For radiopacity, barium solution, made of 375 grams of Solotop HD (Taejoon Pharm, Seoul, Korea) and 360 cc of water, was used. To make the thin liquid, the barium solution was diluted with water, with a ratio of 48 to 52, to make thick liquid, Toromi-Up (Nisshi Oilio, Tokyo, Japan) was added. In the other diets, barium solution was added for good visualization during VFSS. After VFSS in 90° upright sitting position, the same protocol was used while the patients were asked to take a posture of 45° reclined sitting. And the head and neck were kept in neutral position. VFSS was conducted rather flexibly considering the subjects' severity of dysphagia, general condition, and coordination.
Data analysis
The whole procedure of VFSS was recorded with video tapes, which can record 30 frames per second (one frame takes 0.033 second). Next, the video tapes were analyzed for penetration-aspiration scale (hereafter PAS),10 oral transit time, pharyngeal delay time, pharyngeal transit time, residue in valleculae and pyriform sinuses, premature bolus loss, and nasal penetration. Analysis was conducted by 2 rehabilitation doctors who were blinded to the patient's clinical stutus, and conclusions were reached by mutual agreement.
Oral transit time was measured from the moment when the main bolus began to move backward to the moment when the front part of the main bolus arrived at the lower part of the ramus of the mandible. Premature bolus loss was not considered, and only the main bolus was the object of the measurement. Pharyngeal delay time was measured from the moment when the main bolus arrived at the lower part of the ramus of the mandible to the moment when the larynx began to rise. Pharyngeal transit time was measured from the moment when the main bolus arrived at the lower part of the ramus of the mandible to the moment when the rear part of the main bolus transited the cricopharyngeus.1,5
The residue in the valleculae and pyriform sinuses was measured in four grades: grade 0: there was no residue left; grade 1: the residue was less than 10 percent; grade 2: the residue was between 10 and 50 percent; and grade 3: the residue was over 50 percent.3 We checked if there was premature bolus loss or not, and nasal penetration at the end of uvula was analyzed with lateral view of the VFSS.
Statistical analysis
For statistical analysis, Paired t-test and Pearson chi-squared test of the SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) for Windows were used, and cases under 0.05 of p-value were considered statistically significant.
RESULTS
Penetration-aspiration scale
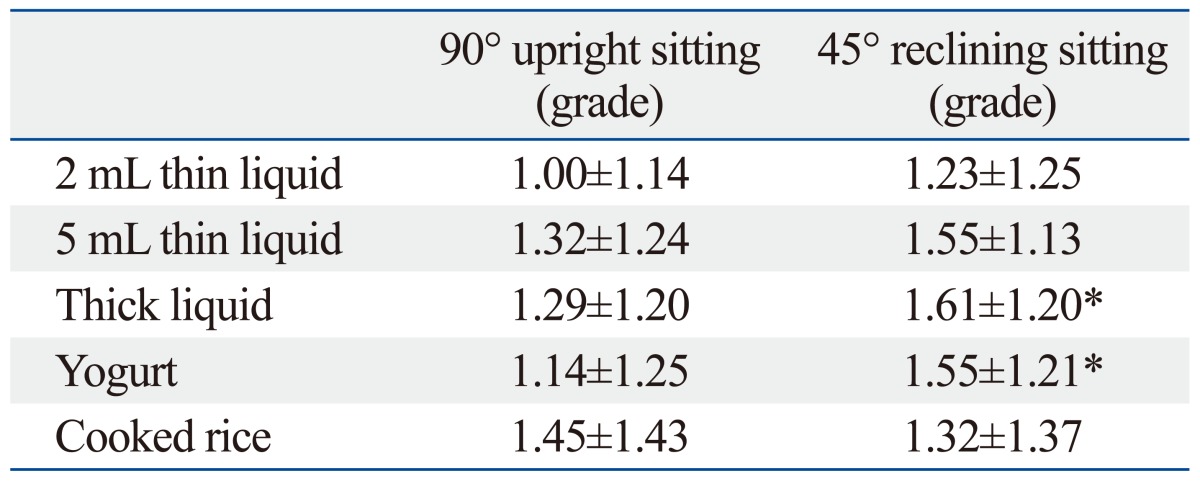
In the cases of 2 mL and 5 mL thin liquids, the PAS of sitting up at 45° was reduced significantly in comparison with sitting up at 90° (p<0.05) (Table 2). In the other types of trial food, there was no significant difference in PAS according to postural change.
Table 2.
Penetration-Aspiration Scale in 90° Upright and 45° Reclining Sitting Posture
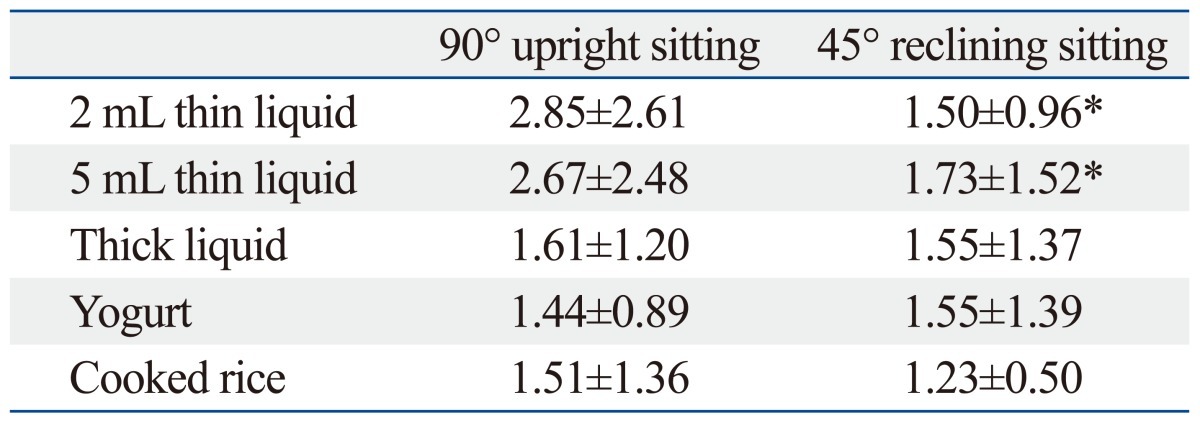
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
Oral transit time, pharyngeal delay time, and pharyngeal transit time
In these three measurements, there was no significant difference according to the postural change (Table 3, 4 and 5).
Table 3.
Oral Transit Time in 90° Upright and 45° Reclining Sitting Posture
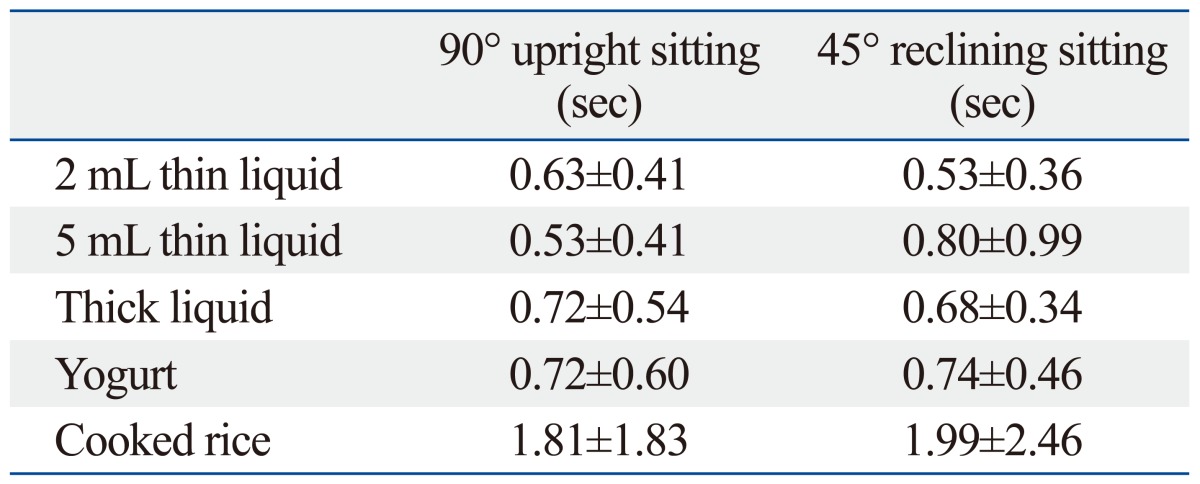
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
Table 4.
Pharyngeal Delay Time in 90° Upright and 45° Reclining Sitting Posture
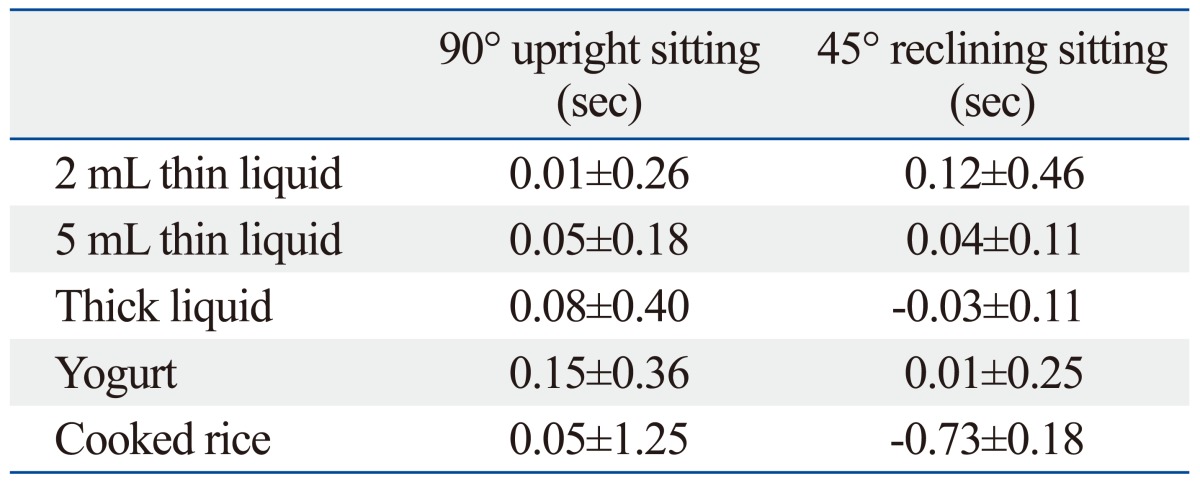
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
Table 5.
Pharyngeal Transit Time in 90° Upright and 45° Reclining Sitting Posture
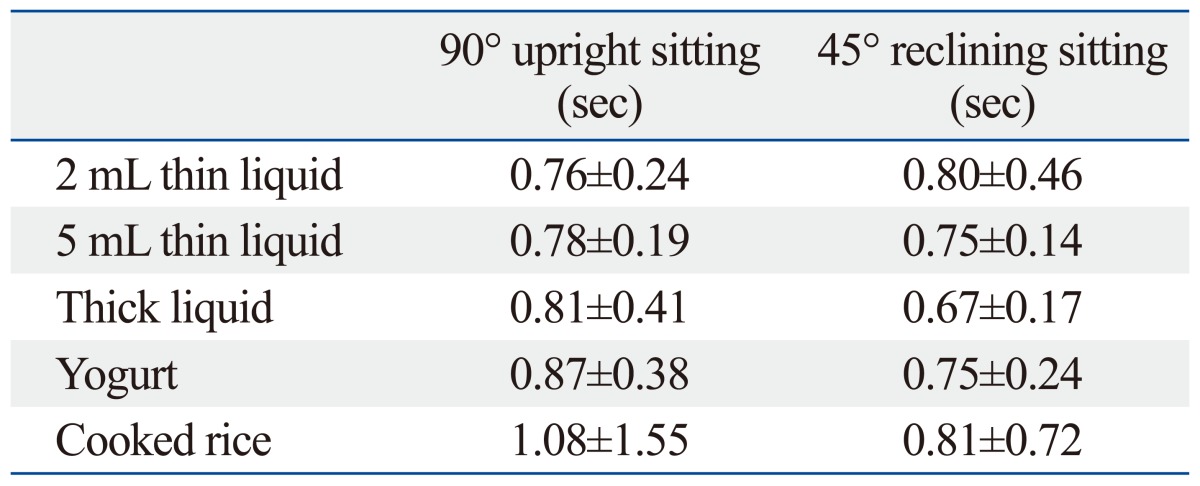
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
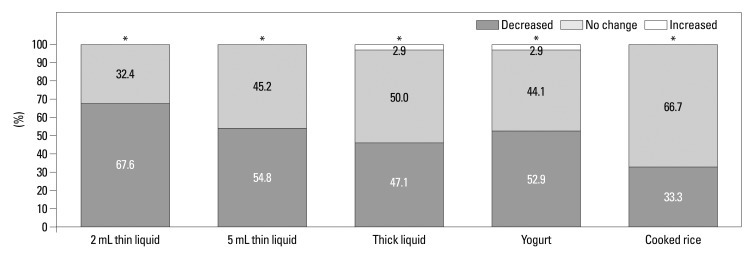
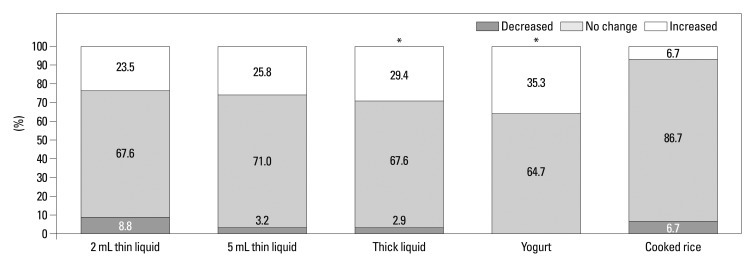
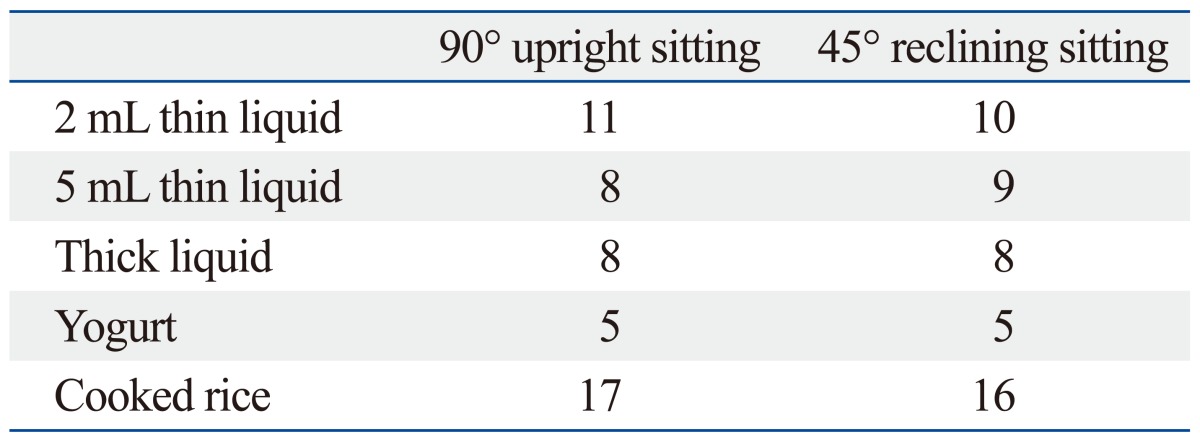
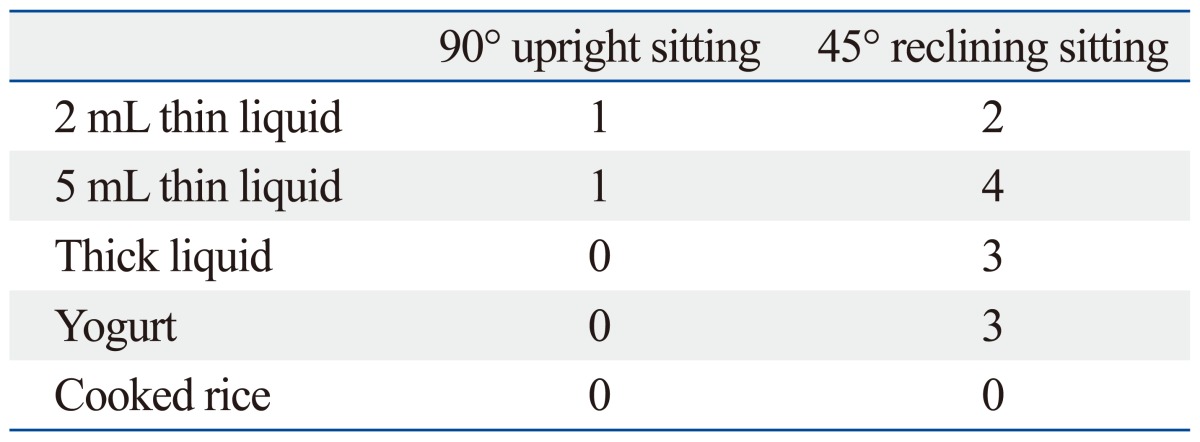
Grades of residue
Grades of residue in valleculae decreased significantly in all diets at 45° reclined sitting than at 90° upright sitting (p<0.05) (Table 6). These decreases were greatest in 2 mL thin liquid. Decrease in 2 mL thin liquid was seen in 23 patients (67.6%) (Fig. 1). However, most of the patients didn't show changes in grades of residue in pyriform sinuses, except the cases of thick liquid and yogurt in which there were significant increases at 45° reclined sitting (p<0.05) (Table 7, Fig. 2).
Table 6.
Residue in Valleculae in 90° Upright and 45° Reclining Sitting Posture
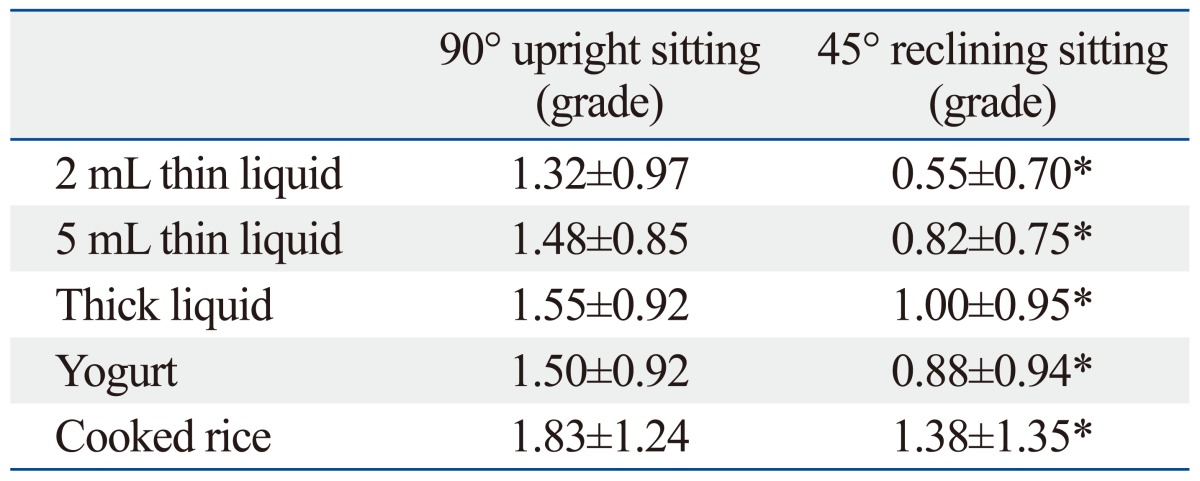
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
Fig. 1.
Changes of residue in valleculae. Significant decreases were seen in all boluses at 45° reclining sitting posture compared with 90° upright posture. *p<0.05.
Table 7.
Residue in Pyriform Sinuses in 90° Upright and 45° Reclining Sitting Posture
Values are mean±SD.
*p<0.05 in comparison with 90° upright sitting.
Fig. 2.
Changes of residue in pyriform sinuses. Significant increases were seen in thick liguid and yogurt at 45° reclining sitting posture compared with 90° upright posture. *p<0.05.
Premature bolus loss and nasal penetration
Premature bolus loss was not significantly related to postural change (Table 8), and nasal penetration showed a tendency of increase, but not statistically significant (Table 9).
Table 8.
Premature Bolus Loss in 90° Upright and 45° Reclining Sitting Posture
Values are number of patients.
*p<0.05 in comparison with 90° upright sitting.
Table 9.
Nasal Penetration in 90° Upright and 45° Reclining Sitting Posture
Values are number of patients.
*p<0.05 in comparison with 90° upright sitting.
DISCUSSION
Currently, various methods are being applied to dysphagia patients. The order of introducing these various therapies is as follows: generally, postural change is used, then swallowing technique, and finally dietary modification, if necessary.4,5 While various postural techniques, such as a chin tuck, head rotation, and head tilt, have been introduced, most of previous researches have been focused on the effects of postural change in the head and neck while sitting up. Thus, there has been very little research on how various postures other than sitting up can influence dysphagia. Postural change can be effective when it is applied appropriately to the patients' anatomical or physiological swallowing disability in order to reduce the aspiration of water or food effectively across a wide range of patients.5,7
As the trachea is in front of the esophagus while sitting up straight and the trachea is above the esophagus while leaning back or lying down, aspiration into the trachea can be reduced because of gravity.5,11 Larnert and Ekberg8 reported that aspiration decreased in the cases of puree and liquid with the patients leaning back at 30 degrees compared to straight sitting, and Ha, et al.9 also reported the aspiration decrease at 5 mL of liquid on supine posture compared to sitting up. In our study, the aspiration decrease in the thin liquid while leaning back at 45 degrees was observed compared to sitting up, and there was no significant difference in the diets with higher viscosity. This result is due to the fact that the gravity effect is relatively reduced according to postural change in the case of a high viscosity diet.
We were unable to determine oral transit time, pharyngeal delay time and pharyngeal transit time according to sitting posture change. Thus, it is highly possible that the 45° leaning back posture would raise the chin, thus making the swallowing reflex weaker, and the effect of gravity on the moving bolus would be reduced to make the transit time longer. In this study, however, there was no significant delay in oral transit time, pharyngeal delay time, and pharyngeal transit time between sitting up and leaning back 45°, indicating that the VFSS test of leaning back at 45° can be an appropriate test method for the patients who cannot keep the posture of sitting up at 90°. In addition, as leaning back at a 45° position did not create any delays in oral transit time, pharyngeal delay time, or pharyngeal transit time, this posture can be recommended as effective for dysphagia patients.
Rasley, et al.7 reported that the lateral decubitus posture decreased aspiration for patients who had residue in their pharynx because that posture reduced residue. In our study, the residue in valleculae was reduced whereas that of pyriform was slightly increased in cases of thick liquid and yogurt at a 45° sitting. This is due to the fact that the bolus passes along the anterior wall through the laryngeal valleculae and epiglottis while sitting up, whereas it passes through the posterior wall of the pharynx and arrives at the pyriform in a lying position. Therefore, it is highly likely that 45° reclining position is an effective compensation technique in case of increased residue in the valleculae, but not in the case of increased residue in the pyriform.
Ha, et al.9 reported a reduced premature bolus loss at the supine posture because of a retrodisplacement of the tongue due to gravity while lying down, compared to sitting up. However, in our study, leaning back at 45° did not significant change premature bolus loss compared to sitting up at 90° because retrodisplacement effect of the tongue was not big enough to cause the change.
Similar to the findings of Ha, et al.9 on an increase in nasal penetration due to a lying down posture, our study showed a slight increase in nasal penetration while leaning back at 45° than straight sitting, but our finding did not reach statistical significance. This is because the level of the nasal cavity and the pharynx is the same while lying down, while the nasal cavity is located higher than the pharynx in the 45° leaning back position. Thus, nasal penetration frequency could be reduced because of the gravity effect. Compared to the problem of increasing nasal penetration when the aspiration of a liquid diet could be reduced while lying down, the 45° sitting could be a competitive postural technique, since it not only reduces aspiration, but it also minimizes the side effect of nasal penetration.
There are some limitations to this study. The first limitation is the lack of analysis about function, such as hyoid bone or upper esophageal sphincter. The second limitation is the fact that patients' etiologic diseases are heterogeneous, thus limiting practical application of 45° reclining position for the disease-specific dysphagia rehabilitation. Therefore, further studies should additionally measure various object of VFSS about swallowing function, and also further analysis according to each etiology is needed. Then, they will contribute to the understanding of effect of body position on dysphagia physiology and development of related treatment.
In conclusion, compared to straight sitting, aspiration of thin liquid was reduced and the amount of residue in the valleculae was reduced, and there was no increase in oral transmit time, pharyngeal delay time, pharyngeal transmit time, or nasal penetration in the 45° leaning back sitting posture. Thus, in patients who are diagnosed as experiencing aspiration of a liquid diet, or have much residue in the valleculae in the VFSS, leaning back at 45° would be an effective compensation technique. In addition, for patients who cannot maintain straight sitting on VFSS, leaning back at 45° may be an appropriate technique. We believe that the 45° reclined sitting posture would reduce the tube feeding period and bring forward oral feeding than straight sitting.
ACKNOWLEDGEMENTS
This study was supported by research funds of Chonbuk National University in 2013, and by the Fund of Biomedical Research Institute, Chonbuk National University Hospital.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Han TR, Paik NJ, Park JW. The clinical functional scale for dysphagia in stroke patients. Korean J Stroke. 2001;3:153–157. [Google Scholar]
- 2.Park YH, Kim HS. Clinical Evaluation of the Swallowing. J Korean Dysphagia Soc. 2011;1:19–24. [Google Scholar]
- 3.Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001;82:677–682. doi: 10.1053/apmr.2001.21939. [DOI] [PubMed] [Google Scholar]
- 4.Han TR, Paik NJ, Kim IS. Dysphagia. In: Han TR, Bang MS, editors. Rehabilitation medicine. 3rd ed. Seoul: Koonja Press; 2008. pp. 369–391. [Google Scholar]
- 5.Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: pro-ed; 1998. [Google Scholar]
- 6.Rosenbek JC, Roecker EB, Wood JL, Robbins J. Thermal application reduces the duration of stage transition in dysphagia after stroke. Dysphagia. 1996;11:225–233. doi: 10.1007/BF00265206. [DOI] [PubMed] [Google Scholar]
- 7.Rasley A, Logemann JA, Kahrilas PJ, Rademaker AW, Pauloski BR, Dodds WJ. Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. AJR Am J Roentgenol. 1993;160:1005–1009. doi: 10.2214/ajr.160.5.8470567. [DOI] [PubMed] [Google Scholar]
- 8.Larnert G, Ekberg O. Positioning improves the oral and pharyngeal swallowing function in children with cerebral palsy. Acta Paediatr. 1995;84:689–692. doi: 10.1111/j.1651-2227.1995.tb13730.x. [DOI] [PubMed] [Google Scholar]
- 9.Ha JS, Park SO, An HM, Park IS. The usefulness of supine position on swallowing of liquid diet in neurogenic dysphagia: comparison with sitting position. J Korean Acad Rehabil Med. 2001;25:916–922. [Google Scholar]
- 10.Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–98. doi: 10.1007/BF00417897. [DOI] [PubMed] [Google Scholar]
- 11.Tsubahara A. Principles and practice of dysphagia management. Seoul: Koonja Press; 2011. [Google Scholar]