Abstract
Background
The obesity-hypertension link over the life course has not been well characterized although the prevalence of obesity and hypertension are increasing in the United States.
Methods and Results
We studied the association of body mass index (BMI) in young adulthood, into middle age, and through late life with risk of developing hypertension in 1132 white men of The Johns Hopkins Precursors Study, a prospective, cohort study. Over a median follow-up period of 46 years, 508 men developed hypertension. Obesity (BMI ≥ 30 kg/m2) in young adulthood was strongly associated with incident hypertension (hazard ratio (HR) = 4.17, 95% CI (2.34-7.42)). Overweight (BMI 25 to < 30 kg/m2) also signaled increased risk (HR = 1.58, 95% CI (1.28-1.96)). Men of normal weight at age 25 years who became overweight or obese at age 45 were at increased risk compared to men of normal weight at both times (HR = 1.57, 95% CI (1.20-2.07)), but not men who were overweight or obese at age 25 years who returned to normal weight at age 45 years (HR = 0.91, 95% CI (0.43-1.92)). After adjusting for time-dependent number of cigarettes smoked, cups of coffee taken, alcohol intake, physical activity, parental premature hypertension and baseline BMI, the rate of change in BMI over the life course, increased the risk of incident hypertension in a dose-response fashion, with the highest risk among men with the greatest increase in BMI (HR = 2.52, 95% CI (1.82-3.49)).
Conclusions
Our findings underscore the importance of higher weight and weight gain in increasing the risk of hypertension from young adulthood, through middle age, and into late life.
Keywords: Body Mass Index, Hypertension, Long term follow-up, Longitudinal cohort study, Men
INTRODUCTION
Epidemiological evidence suggests that the prevalence of hypertension is increasing1, 2 and obesity is a major public health concern.3 Previous investigations of the association between obesity and hypertension have been based on cross-sectional comparisons,4-11 short follow-up intervals,11-19 few assessments of blood pressure and weight,11, 13, 15-17, 20-23 follow-up only through middle age,17, 19, 22, 24 and adjustment only for baseline characteristics which are known to change with age.12, 22 Uncertainty remains about the magnitude of the risk of hypertension with obesity and overweight over the life course, and specifically, how changes in weight might modify the risk of hypertension against a background of secular and individual changing lifestyles.
The life course perspective contends that lifestyle and behavior in youth and middle age exert their influence on health later in life through established patterns and accumulation of effects that may take years to develop.25 We sought to estimate the association of weight and weight change from young adulthood, into middle age, and through late life with risk of developing hypertension, in The Johns Hopkins Precursors Study. This longitudinal cohort of former medical students consists of over 5 decades of follow-up with repeated, validated measures of body weight, blood pressure, and other lifestyle factors known to be associated with blood pressure. In contrast to studies that rely on retrospective reports of body weight or lifestyle factors, our study design provides considerable advantages because we have many assessments of the purported risk factor and factors that might distort estimates of risk (such as smoking, alcohol consumption, and levels of physical activity). Our primary hypothesis was that overweight and obesity would confer risk even when arising in middle age and late life, consistent with a model of accumulating risk throughout the life course.
METHODS
Study sample
The Johns Hopkins Precursors Study initiated in 1947 by Caroline Bedell Thomas to identify precursors of cardiovascular disease and premature death26 represents 57 years of a longitudinal cohort consisting of 1337 students who matriculated into the graduating classes of 1948 to 1964 of The Johns Hopkins University School of Medicine. Study procedures were approved by the School of Medicine Institutional Review Board.
Analysis was based on a median follow-up of 46 years. Yearly response rates average about 73% with 90% of the cohort responding at least once every 5 years. We excluded the small number of women (n=121). Men, of Asian ancestry (n=19), who had hypertension before graduation (n=19), who had no BMI measurement at baseline (n=23), who were not available for follow up (n=12), or who had no blood pressure measurements over follow up (n=10) were excluded. One man whose age at baseline was more than twice the median age of the cohort (23 years) at baseline was excluded. The remaining 1132 white men comprise the sample.
Measurement strategy
Body mass index
Body mass index calculated as weight in kilograms divided by the square of height in meters is an indicator of adiposity used in clinical and public health purposes.27, 28 In medical school, participants underwent a standardized medical history and physical examination including measurement of height, weight,29 and blood pressure.30 Follow up consisted of annual mailed questionnaires. From 1954 to 1985, questions about body weight were asked every 3 to 5 years. After 1985 questions on body weight were asked annually except in 1986, 1987, 1990, 1991, 1995 and 1996. Body weight and height have been validated in this cohort with self-reported height and weight highly correlated with measured weight (r = 0.98) and height (r = 0.95).31 Height at baseline was used to calculate BMI during follow up when weight was reported. Keeping the height the same throughout follow up ensured that any changes in BMI were reflective of changes in weight. The prevalence of missing weights ranged from 5-10%, depending on the age. For each of the age decades the percentage of participants for whom we had the actual BMI values were as follows, for ages between 20-29 years-96.3%, for 30-39 years-91.8%, for 40-49 years -94.3%, for ages 50-59 years-90.0%, for ages 60-69 years-89.7%. We estimated missing weights using a random effects model combining individual weights from the years available over follow up with cohort-wide data on linear trends in weight change over the entire follow up period.32
Blood pressure
Blood pressure was assessed on multiple occasions (a median of 9 times) while the participants were in medical school using a standardized protocol. The mean level of measurements in medical school was used to estimate the baseline blood pressure for the present analysis. During follow up using annual questionnaires, participants were asked to measure their blood pressure in the right arm in a seated position after five minutes of rest. In this sample, self-reported blood pressure was highly correlated with measured systolic (r = 0.72) and diastolic (r = 0.56) blood pressure31 comparable to the published correlation between ambulatory and clinic blood pressure measurements.33
Questionnaires included an inquiry about a diagnosis of and treatment for hypertension. Hypertension was defined as a blood pressure of 160/95 mm Hg reported on one annual questionnaire, greater than or equal to 140/90 mm Hg on 2 or more occasions, or hypertension requiring drug treatment.34 The mean of all reported blood pressure values was used when participants reported more than 1 blood pressure reading on a questionnaire. These criteria for hypertension are consistent with our prior work35, 36 and are conservative compared to the Seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure.37 A total of 35,268 blood pressure measurements yielded 16,821 annual BP estimates. For participants meeting criteria for hypertension, onset was defined as the first reported elevated reading. An End Point Committee consisting of five physicians reviewed annual questionnaires, blood pressure reports and medical records to reach consensus on the diagnosis of hypertension.
Covariates
Assessment of cigarette smoking, alcohol intake, physical activity and coffee drinking was carried out using standard questions at baseline and follow up.35 Cigarette smoking and coffee drinking were defined by time-dependent dichotomous variables reflecting changes in smoking behavior and coffee drinking during the entire follow-up. Methods of assessment of physical activity and alcohol intake varied over the follow-up. Physical activity was assessed in medical school and over follow-up using the question, “How much physical training have you had in the past month?” with response categories “none,” “little,” “moderate,” or “much.” In 1978, 1986, 1989, 1993, 1997, 2000, and 2003 participants were asked the number of times per week they engaged in physical activity vigorous enough to work up a sweat.38 Alcohol intake was assessed in medical school and every 5 years after graduation until 1984 by asking, “How much do you drink?” Possible responses were “never,” “occasional,” “varies” and “regular.” In 1978, 1986, and later, a quantity-frequency measure of alcohol consumption was administered. Based on data from 1978, when both questions were asked, alcohol intake data from all questionnaires were converted to a quantity-frequency scale. Responses to both questions have been strongly related to the incidence of hypertension in this cohort.34, 39 Parental history of hypertension was defined as a participant’s report of hypertension in a parent at baseline or at any point during follow-up, or a diagnosis of hypertension as either an underlying or other condition reported in the death certificate of a participant’s parent. Parental premature hypertension was defined as the development of hypertension before age 55 in a participant’s father or before age 65 in his mother. Hypertension in both parents had a strong independent association with incident hypertension in this cohort.36
Statistical analysis
We estimated cumulative incidence of hypertension associated with BMI at baseline for 3 categories of BMI (normal (<25.0 kg/m2), overweight (25.0 to <30.0 kg/m2), obese (≥30.0 kg/m2)) and BMI change using Kaplan-Meier analysis 40 and we tested for a difference in hypertension incidence using the log-rank test.41 The association of BMI with hypertension incidence was also assessed using BMI as a time-dependent continuous variable and with BMI at ages 25, 45 and, 65 years. We used a standard time-dependent approach, following each participant until development of hypertension or censoring, and updated the BMI for every participant during the follow-up interval. Hazard ratios (HR) and corresponding 95% confidence intervals (CIs) relating BMI to risk of hypertension were constructed employing the Cox proportional hazards model.42 Proportionality assumptions were assessed for Cox proportional hazards models using log-log plots for baseline BMI analyses and Schoenfeld tests for time-dependent analyses.43 In survival models, age was the time variable and persons who died were considered as censored.
To examine the hypothesis that risk of hypertension varied by the trajectory of BMI over the life course, we derived slopes of rate of BMI change, up to the age of diagnosis of hypertension, using random effects models.32 Participants without hypertension were kept in the analysis until the end of follow up. The hazard ratio of hypertension associated with rate of BMI change over follow up was calculated using quartiles of rate of BMI change modeled as a categorical variable in Cox proportional hazards analysis.42
Multivariate models were developed to adjust for possible confounding variables, including parental premature hypertension and time-dependent data during follow-up on number of cigarettes smoked, cups of coffee taken, alcohol intake, and physical activity. To estimate the effect of change in BMI category over 20 years from early adulthood to middle age on the risk of incident hypertension, we modeled change in BMI from age 25 to age 45 in Cox proportional hazards analysis.42 Tests of significance were 2-tailed with an α of .05.
RESULTS
Sample characteristics
Table 1 summarizes the characteristics of the 1132 men in medical school. The median BMI at baseline was 23.1 kg/m2. The mean age of men in all three BMI categories was similar (23 years) and they all had a normal mean diastolic blood pressure. Obese men had the highest mean systolic blood pressure of 127 mmHg and were more likely to smoke cigarettes (82%) than others. BMI in medical school was not related to coffee intake, alcohol drinking, physical activity or a history of parental premature hypertension at baseline.
Table 1.
Baseline characteristics of study sample according to body mass index (BMI in kg/m2) assessed in medical school. Data from The Johns Hopkins Precursors Study (1947-2005). Percents in parentheses represent column percents.
| Normal (BMI < 25) n = 923 |
Overweight (BMI 25 to < 30) n = 192 |
Obese (BMI ≥ 30) n = 17 |
Total n = 1132 |
|
|---|---|---|---|---|
| Age at BMI assessment | 23.1 (2.4) | 23.4 (2.9) | 23.1 (2.7) | 23.1 (2.5) |
| Body mass index, kg/m2 | 22.2 (1.7) | 26.5 (1.2) | 32.3 (2.1)† | 23.1 (2.5) |
| Systolic blood pressure, mmHg | 115 (8.5) | 119 (10.6) | 127 (14.6)† | 116 (9.2) |
| Diastolic blood pressure, mmHg | 69 (6.4) | 72 (7.2) | 77 (11.6)† | 70 (6.8) |
| Pulse pressure, mmHg | 46 (8.2) | 47 (9.6) | 50 (10.9) | 46 (8.5) |
| Coffee intake, cups per day | 2.2 (1.8) | 2.6 (2.1) | 2.8 (1.8) | 2.3 (1.8) |
| Alcohol, drinks per week | 6.4 (3.9) | 6.9 (4.2) | 6.8 (3.8) | 6.5 (4.0) |
| Vigorous exercise per week | 0.8 (1.1) | 0.8 (1.0) | 0.7 (0.7) | 0.8 (1.1) |
| Cigarette smokers, No. (%) | 437 (47.3) | 86 (44.8) | 14 (82.4)‡ | 537 (47.4) |
| Parental premature hypertension #, No. (%) | 257 (27.8) | 70 (36.5) | 9 (52.9) | 336 (29.7) |
Data are presented as mean (SD) unless otherwise specified. Denominators may vary because of missing data.
P<.001, from analysis of variance
P<.05, from χ2 analysis
Premature hypertension defined as development of hypertension before age 55 in a participant’s father or before age 65 in his mother. Includes either or both parents having premature hypertension.
Incident hypertension
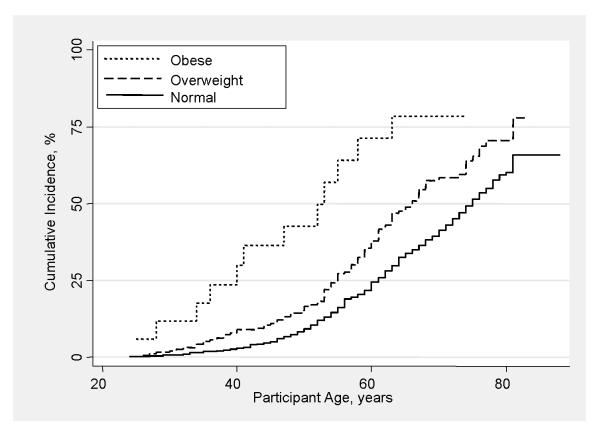
During a median follow up of 46 years, 508 men developed hypertension. The unadjusted cumulative incidence of hypertension was 0.3% at age 25 years, 6.5% at age 45 years, and 37% at age 65 years. A progressive increase in hypertension incidence was statistically significantly associated with higher BMI throughout follow-up (Figure 1).
Figure 1.
Cumulative incidence of hypertension by baseline body mass index (BMI) over 46 years of follow-up in 1132 men of The Johns Hopkins Precursors Study (1947-2005). p-value < 0.05 (log-rank test).
 Obese
Obese
 Overweight
Overweight
 Normal
Normal
Association of BMI with incident hypertension
Compared with men with normal BMI at baseline, overweight men were at one and a half times increased risk of developing hypertension (unadjusted HR = 1.58, 95% CI (1.28-1.96); Table 2)). Men who were obese at baseline had over a fourfold increased risk of developing hypertension (unadjusted HR = 4.17, 95% CI (2.34-7.42)). After adjustment for parental premature hypertension, alcohol drinking, physical activity, coffee drinking and cigarette smoking at baseline, the risk of developing hypertension compared to men with normal BMI at baseline was essentially unchanged. Proportionality assumptions were met for all models. Results were similar in models adjusting for time-dependent covariates. Cumulative incidence rates at age 65 years according to baseline BMI are provided in Table 2.
Table 2.
Hazard ratios and cumulative incidence of hypertension associated with baseline body mass index (kg/m2) among 1132 men in The Johns Hopkins Precursors Study. 95% confidence interval in parentheses.
| Baseline BMI | Number | Number of hypertension cases |
Cumulative incidence of hypertension at age 65 years (events / 100) |
Unadjusted hazard ratio |
Hazard ratio adjusted for baseline characteristics¶ |
Hazard ratio adjusted for time- dependent characteristics‡ |
|---|---|---|---|---|---|---|
| Normal (BMI <25) |
923 | 389 | 34 (31-37) | 1.00 | 1.00 | 1.00 |
| Overweight (BMI 25 to <30) |
192 | 107 | 49 (42-57) | 1.58 (1.28-1.96) | 1.65 (1.29-2.09) | 1.49 (1.15-1.95) |
| Obese (BMI ≥30) |
17 | 12 | 78 (54-95) | 4.17 (2.34-7.42) | 4.83 (2.47-9.44) | 2.79 (1.30-6.00) |
Models adjusted for parental premature hypertension and number of cigarettes smoked, cups of coffee taken, alcohol intake and physical activity measured at baseline.
Models adjusted for parental premature hypertension and time-dependent number of cigarettes smoked, cups of coffee taken, alcohol intake and physical activity.
Change in BMI and incident hypertension
Compared with the risk for men with normal BMI at age 25 years who remained so at age 45 years (Table 3), men who were normal at age 25 years but overweight or obese at age 45 years had a higher risk of developing hypertension (HR = 1.57, 95% CI (1.20-2.07)). Men who were overweight or obese at age 25 years who remained overweight or obese at age 45 years were at almost double the risk of developing hypertension (HR = 1.91, 95% CI (1.46-2.49)) when compared to men who were of normal BMI at both age 25 and 45 years. The small number of men who were overweight or obese at age 25 years but who lost weight by age 45 years had a hazard ratio of 0.91, 95% CI (0.43-1.92). Small numbers in change categories precluded the use of multivariate analyses. Cumulative incidence rates at age 65 years according to change in BMI category are provided in Table 3.
Table 3.
Hazard ratio and cumulative incidence of hypertension according to change in body mass index (kg/m2) from early adulthood to middle age among 871 men of The Johns Hopkins Precursors Study (men who developed hypertension before age 45 years were excluded). 95% confidence interval in parentheses.
| BMI at age 25 years |
BMI at age 45 years |
Number | Number of hypertension cases |
Cumulative incidence of hypertension at age 65 years (events / 100) |
Unadjusted hazard ratio |
|---|---|---|---|---|---|
| Normal | Normal | 584 | 224 | 29 (25-33) | 1.00 |
| Overweight or obese | Normal | 19 | 7 | 23 (9-51) | 0.91 (0.43-1.92) |
| Normal | Overweight or obese | 138 | 68 | 42 (34-52) | 1.57 (1.20-2.07) |
| Overweight or obese | Overweight or obese | 130 | 73 | 51 (42-60) | 1.91 (1.46-2.49) |
Treating BMI as a time-dependent variable, for each 1 kg/m2 higher BMI, the risk of developing hypertension was increased (HR = 1.06, 95% CI (1.04-1.08)). Examining BMI at specific ages, a 1 kg/m2 higher BMI was associated with higher risk of hypertension at age 25 years (HR = 1.12, 95% CI (1.08-1.17)), at age 45 years (HR = 1.12, 95% CI (1.08-1.15)), and at age 65 years (HR = 1.08, 95% CI (1.02-1.14)). Considering rate of change in BMI grouped according to quartiles, the risk of hypertension was higher in a dose-response fashion (Table 4). Point estimates associated with analysis of change in BMI were similar after multivariate adjustment.
Table 4.
Hazard ratio of hypertension according to rate of body mass index change (slope) quartiles over 46 years in 1132 men in The Johns Hopkins Precursors Study. Slopes were derived from random effects models using BMI values up to the age of diagnosis of hypertension. 95% confidence interval in parentheses.
| Rate of BMI change (slope in kg/m2 per year) |
Unadjusted hazard ratio |
Hazard ratio adjusted for BMI only |
Hazard ratio adjusted for baseline characteristics¶ |
Hazard ratio adjusted for time-dependent characteristics‡ |
|---|---|---|---|---|
| First Quartile (−11.1 to -−1.79) |
1.00 | 1.00 | 1.00 | 1.00 |
| Second Quartile (−1.80 to -−0.11) |
1.35 (1.03-1.77) | 1.43 (1.09-1.87) | 1.59 (1.18-2.16) | 1.51 (1.08-2.12) |
| Third Quartile (−0.10 to 1.59) |
1.84 (1.42-2.39) | 1.94 (1.49-2.52) | 2.13 (1.58-2.86) | 2.13 (1.53-2.97) |
| Fourth Quartile (1.60 to 15.9) |
2.37 (1.84-3.06) | 2.58 (1.99-3.33) | 2.48 (1.85-3.32) | 2.52 (1.82-3.49) |
Models adjusted for parental premature hypertension and baseline number of cigarettes smoked, cups of coffee taken, alcohol intake, physical activity and BMI measured at baseline.
Models adjusted for parental premature hypertension and time-dependent number of cigarettes smoked, cups of coffee taken, alcohol intake, physical activity and BMI measured at baseline.
DISCUSSION
In this long-term prospective study, men who were overweight or obese in early adulthood or middle age were at higher risk of hypertension later in life. Overweight or obese men were consistently at higher risk of hypertension across the entire period of follow-up. Obesity in young adulthood conferred a 3-fold risk of hypertension, even after accounting for change in life style factors over the life course. Men who were of normal weight in early adulthood but who became overweight or obese in midlife were twice as likely to develop hypertension than men who maintained a normal weight. The corollary is that men who maintain normal weight were at the lowest risk of hypertension after 46 years of follow-up.
Previous investigations had short follow-up time,11-19 ascertainment of blood pressure subject to recall bias,24, 44 assessment on only 2 occasions,11, 13, 15-17, 19-23 no adjustment for possible confounders during follow up,12, 19, 22, 45 or were limited to a narrow age window not extending beyond middle age.19, 20, 24 Our study examined young adults and tracked their body weight and blood pressure through middle age and draws strength from very high response rates, adjudication of incident hypertension diagnosis, and repeated measures of blood pressure and lifestyle factors over 46 years. Unlike other studies, we estimated individual trajectories of weight over the life course using random effects models allowing each person to have their own intercept and slope rather than being assigned a population average.
To gauge the extent to which BMI was related to hypertension risk in a dose-response fashion, we sorted respondents into quartiles based on rate of BMI change. Men in quartiles representing increasingly higher levels of BMI change were at increasingly higher risk, even after accounting for baseline characteristics and lifestyle factors over follow-up. The rate of change of BMI at any point during the life course was an independent predictor of risk, regardless of the level of BMI. Each 1 kg/m2 higher BMI was associated with increasing risk across the life course. For a 5 foot 9 inch man at age 25, a 10 pound weight gain over the life course translates to an 18% increased risk of hypertension. For a 65 year old man of the same height, a 10 pound weight gain translates to a 12% increased risk. Thus even a small weight gain starting early in life increases the risk for hypertension, while small weight gains not occurring until later in life continue to confer increased risk.
Few studies have examined the life course of BMI and risk of hypertension. Nyamdorj and coworkers assessed a community sample aged 25 to 74 years on 2 occasions 5 years apart and found a 1 standard deviation increase in BMI led to a 30% increased risk of hypertension compared to persons whose weight did not change.13 Based on a young community sample, Chuang and colleagues used assessments on 2 occasions about 10 years apart to find an increase in BMI increased risk about 15%.21 In the Nurses’ Health Study and the Health Professionals Follow-up Study, each increment in body weight assessed at baseline was associated with higher risk of hypertension after 10 years of follow-up, even within a range of BMI considered normal,45 but how risk of hypertension was modified by change in BMI was not reported. Consistent with our findings, Juonala and colleagues11 pooled data from 4 prospective studies and found that for persons who were overweight or obese as children but not as adults the risk of hypertension was comparable to the risk of children who remained at a normal BMI as adults. Adults who were obese were at increased risk, regardless of their weight in childhood, but in contrast to our study, the mean age of the participants was 11 years at baseline with a follow-up of 23 years.11 We tested the hypothesis that overweight or obesity would confer risk of development of hypertension beyond young adulthood. None of the studies took a life course perspective nor accounted for characteristics that change over time.
A methodological issue common to all longitudinal studies relates to misclassification of exposure (i.e., body weight) or outcome (i.e., hypertension). In this sample self-report of body weight and blood pressure were highly accurate when compared to in-person assessments.31 Misclassification because of a tendency to underreport weight or blood pressure at higher levels would be expected to bias our estimates towards the null. Indices of body fat may be most closely associated with incidence of hypertension,46 and because body fat shifts from peripheral to central sites with age, BMI may be a less sensitive indicator of adiposity than waist-to-hip ratio.47 Nevertheless, in men, BMI may be an adequate measure of percentage body fat.27, 48 Since measurement of body fat was impractical, weight adjusted for height was used.49 Our findings may not be generalizable to women, men of lower socioeconomic status, or ethnic minorities, especially with regard to absolute levels of risk, but our long term perspective shows how body weight influences risk even after accounting for changing lifestyle factors. We have no reason to believe that the relationship between obesity and overweight with hypertension in our sample is any different from other populations, even though the prevalence of risk factors may differ. No information on dietary factors associated with hypertension incidence was available. Multivariate analyses suggest little of the association of hypertension and BMI at baseline and over follow up was mediated through family history of hypertension or important time-dependent factors associated with blood pressure.
The temporal relationship established by the long follow up and repeated assessment of both body weight and blood pressure provides strong evidence for the association between trajectories of BMI and incident hypertension. Our findings suggest even a modest gain in weight beginning early in life was associated with a substantially higher risk of hypertension. Obesity and overweight continued to confer higher risk of hypertension even when occurring late in life.
Clinical Perspective.
In this long-term prospective cohort study, we studied the association of body mass index (BMI) with risk of developing hypertension from young adulthood, into middle age, and through late life. Repeated assessments of BMI, blood pressure and risk factors for developing hypertension over the life course enabled us to examine the influence of lifestyle and behavior in young adult life through middle age on health later in life. Obesity in young adulthood conferred a 3-fold risk of hypertension after 46 years of follow-up, even accounting for change in life style factors over the life course. Men who were of normal weight in early adulthood but who became overweight or obese in midlife were twice as likely to develop hypertension than men who maintained a normal weight. Loss of weight between young adulthood and middle age conferred no additional risk. Rate of change of BMI over the life course was an independent predictor of risk of hypertension, independent of the level of BMI, cigarette smoking, alcohol intake, physical activity and coffee drinking. Although the data were observational, the temporal relationship established by the long follow up and repeated assessment of both body weight and blood pressure provided strong evidence for the association between BMI and hypertension. This study showed that increase of weight at any time in the life course increased the risk of developing hypertension after adjusting for other risk factors.
Acknowledgments
FUNDING SOURCES: This work was supported in part by grants R01 AG01760, K24 DK02856, K24 MH070407 and UL1 RR 025005 from the National Institutes of Health.
Footnotes
CONFLICT OF INTEREST DISCLOSURES: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 2.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 4.He J, Klag MJ, Whelton PK, Chen JY, Qian MC, He GQ. Body mass and blood pressure in a lean population in southwestern China. Am J Epidemiol. 1994;139:380–389. doi: 10.1093/oxfordjournals.aje.a117010. [DOI] [PubMed] [Google Scholar]
- 5.Souza MG, Rivera IR, Silva MA, Carvalho AC. Relationship of obesity with high blood pressure in children and adolescents. Arq Bras Cardiol. 2010;94:714–719. doi: 10.1590/s0066-782x2010005000039. [DOI] [PubMed] [Google Scholar]
- 6.Leenen FH, McInnis NH, Fodor G. Obesity and the prevalence and management of hypertension in Ontario, Canada. Am J Hypertens. 2010;23:1000–1006. doi: 10.1038/ajh.2010.93. [DOI] [PubMed] [Google Scholar]
- 7.Mufunda J, Mebrahtu G, Usman A, Nyarango P, Kosia A, Ghebrat Y, Ogbamariam A, Masjuan M, Gebremichael A. The prevalence of hypertension and its relationship with obesity: results from a national blood pressure survey in Eritrea. J Hum Hypertens. 2006;20:59–65. doi: 10.1038/sj.jhh.1001924. [DOI] [PubMed] [Google Scholar]
- 8.Kastarinen MJ, Nissinen AM, Vartiainen EA, Jousilahti PJ, Korhonen HJ, Puska PM, Tuomilehto Blood pressure levels and obesity trends in hypertensive and normotensive Finnish population from 1982 to 1997. J Hypertens. 2000;18:255–262. doi: 10.1097/00004872-200018030-00003. [DOI] [PubMed] [Google Scholar]
- 9.Stamler R, Stamler J, Riedlinger WF, Algera G, Roberts RH. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA. 1978;240:1607–1610. doi: 10.1001/jama.240.15.1607. [DOI] [PubMed] [Google Scholar]
- 10.Dyer AR, Elliott P. The INTERSALT study: relations of body mass index to blood pressure. INTERSALT Co-operative Research Group. J Hum Hypertens. 1989;3:299–308. [PubMed] [Google Scholar]
- 11.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 12.Radi S, Lang T, Lauwers-Cances V, Chatellier G, Fauvel JP, Larabi L, De Gaudemaris R, IHPAF Group One-year hypertension incidence and its predictors in a working population: the IHPAF study. J Hum Hypertens. 2004;18:487–494. doi: 10.1038/sj.jhh.1001682. [DOI] [PubMed] [Google Scholar]
- 13.Nyamdorj R, Qiao Q, Soderberg S, Pitkaniemi J, Zimmet P, Shaw J, Alberti G, Nan H, Uusitalo U, Pauvaday V, Chitson P, Tuomilehto J. Comparison of body mass index with waist circumference, waist-to-hip ratio, and waist-to-stature ratio as a predictor of hypertension incidence in Mauritius. J Hypertens. 2008;26:866–870. doi: 10.1097/HJH.0b013e3282f624b7. [DOI] [PubMed] [Google Scholar]
- 14.Lakoski SG, Cushman M, Siscovick DS, Blumenthal RS, Palmas W, Burke G, Herrington DM. The relationship between inflammation, obesity and risk for hypertension in the Multi-Ethnic Study of Atherosclerosis (MESA) J Hum Hypertens. 2011;25:73–79. doi: 10.1038/jhh.2010.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arici M, Turgan C, Altun B, Sindel S, Erbay B, Derici U, Karatan O, Erdem Y, Hasanoglu E, Caglar S. Turkish Society of Hypertension and Renal Diseases. Hypertension incidence in Turkey (HinT): a population-based study. J Hypertens. 2010;28:240–244. doi: 10.1097/HJH.0b013e328332c36b. [DOI] [PubMed] [Google Scholar]
- 16.Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, Howard BV. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension. 2006;47:403–409. doi: 10.1161/01.HYP.0000200710.29498.80. [DOI] [PubMed] [Google Scholar]
- 17.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa-Takata K, Ohta T, Moritaki K, Gotou T, Inoue S. Obesity, weight change and risks for hypertension, diabetes and hypercholesterolemia in Japanese men. Eur J Clin Nutr. 2002;56:601–607. doi: 10.1038/sj.ejcn.1601364. [DOI] [PubMed] [Google Scholar]
- 19.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84:633–641. [PubMed] [Google Scholar]
- 20.Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, Derazne E, Tzur D, Gershnabel D, Grossman E, Karasik A, Shamiss A, Shai I. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension. 2010;56:203–209. doi: 10.1161/HYPERTENSIONAHA.109.146415. [DOI] [PubMed] [Google Scholar]
- 21.Chuang SY, Chou P, Hsu PF, Cheng HM, Tsai ST, Lin IF, Chen CH. Presence and progression of abdominal obesity are predictors of future high blood pressure and hypertension. Am J Hypertens. 2006;19:788–795. doi: 10.1016/j.amjhyper.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 22.Neser WB, Thomas J, Semenya K, Thomas DJ, Gillum RF. Obesity and hypertension in a longitudinal study of black physicians: the Meharry Cohort Study. J Chronic Dis. 1986;39:105–113. doi: 10.1016/0021-9681(86)90066-4. [DOI] [PubMed] [Google Scholar]
- 23.Garrison RJ, Kannel WB, Stokes J, 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16:235–251. doi: 10.1016/0091-7435(87)90087-9. [DOI] [PubMed] [Google Scholar]
- 24.Paffenbarger RS, Jr, Thorne MC, Wing AL. Chronic disease in former college students. VIII. Characteristics in youth predisposing to hypertension in later years. Am J Epidemiol. 1968;88:25–32. doi: 10.1093/oxfordjournals.aje.a120864. [DOI] [PubMed] [Google Scholar]
- 25.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- 26.Thomas CB. Observations on some possible precursors of essential hypertension and coronary artery disease. Bull Johns Hopkins Hosp. 1951;89:419–441. [PubMed] [Google Scholar]
- 27.Roche AF, Sievogel RM, Chumlea WC, Webb P. Grading body fatness from limited anthropometric data. Am J Clin Nutr. 1981;34:2831–2838. doi: 10.1093/ajcn/34.12.2831. [DOI] [PubMed] [Google Scholar]
- 28.Flegal KM. Commentary: Is there a best index of weight for height? Int J Epidemiol. 2011;40:44–46. doi: 10.1093/ije/dyq266. [DOI] [PubMed] [Google Scholar]
- 29.Brancati FL, Wang NY, Mead LA, Liang KY, Klag MJ. Body weight patterns from 20 to 49 years of age and subsequent risk for diabetes mellitus: the Johns Hopkins Precursors Study. Arch Intern Med. 1999;159:957–963. doi: 10.1001/archinte.159.9.957. [DOI] [PubMed] [Google Scholar]
- 30.Klag MJ, Ford DE, Mead LA, He J, Whelton PK, Liang KY, Levine DM. Serum cholesterol in young men and subsequent cardiovascular disease. N Engl J Med. 1993;328:313–318. doi: 10.1056/NEJM199302043280504. [DOI] [PubMed] [Google Scholar]
- 31.Klag MJ, He J, Mead LA, Ford DE, Pearson TA, Levine DM. Validity of physicians’ self-reports of cardiovascular disease risk factors. Ann Epidemiol. 1993;3:442–447. doi: 10.1016/1047-2797(93)90074-e. [DOI] [PubMed] [Google Scholar]
- 32.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 33.James GD, Pickering TG, Yee LS, Harshfield GA, Riva S, Laragh JH. The reproducibility of average ambulatory, home, and clinic pressures. Hypertension. 1988;11:545–549. doi: 10.1161/01.hyp.11.6.545. [DOI] [PubMed] [Google Scholar]
- 34.Lowry DR, Mead LA, Dannenberg AL, Klag MJ. A Longitudinal Study of Physical Activity and Incidence of Hypertension: The Johns Hopkins Precursors Study. Circulation. 1995;92:619. [Google Scholar]
- 35.Klag MJ, Wang NY, Meoni LA, Brancati FL, Cooper LA, Liang KY, Young JH, Ford DE. Coffee intake and risk of hypertension: the Johns Hopkins precursors study. Arch Intern Med. 2002;162:657–662. doi: 10.1001/archinte.162.6.657. [DOI] [PubMed] [Google Scholar]
- 36.Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168:643–648. doi: 10.1001/archinte.168.6.643. [DOI] [PubMed] [Google Scholar]
- 37.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 38.Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 39.Lowry DR, Mead LA, Dannenberg LA, Klag MJ. Alcohol Consumption and Incidence of Hypertension: The Johns Hopkins Precursors Study. Circulation. 1995:1–619. [Google Scholar]
- 40.Kaplan EL, Meier P. Non-parametric Estimation from Incomplete Observations. J Am Stat Assoc. 1958:457–481. [Google Scholar]
- 41.Peto R, Peto J. Asymptotically efficient rank invariant test procedures. J R Stat Soc Ser B. 1972:185–198. [Google Scholar]
- 42.Cox DR. Regression Models and Life Tables. J R Stat Soc Ser B. 1972:187–220. [Google Scholar]
- 43.Schoenfeld D. Chi-squared goodness-of-fit tests for the proportional hazards regression model. Biometrika. 1980;67:145–153. [Google Scholar]
- 44.Shuger SL, Sui X, Church TS, Meriwether RA, Blair SN. Body mass index as a predictor of hypertension incidence among initially healthy normotensive women. Am J Hypertens. 2008;21:613–619. doi: 10.1038/ajh.2008.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161:1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 46.Fuchs FD, Gus M, Moreira LB, Moraes RS, Wiehe M, Pereira GM, Fuchs SC. Anthropometric indices and the incidence of hypertension: a comparative analysis. Obes Res. 2005;13:1515–1517. doi: 10.1038/oby.2005.184. [DOI] [PubMed] [Google Scholar]
- 47.Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Despres JP. Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr. 1993;58:463–467. doi: 10.1093/ajcn/58.4.463. [DOI] [PubMed] [Google Scholar]
- 48.Oda E, Kawai R. Body mass index is more strongly associated with hypertension than waist circumference in apparently healthy Japanese men and women. Acta Diabetol. 2010;47(4):309–13. doi: 10.1007/s00592-010-0203-7. [DOI] [PubMed] [Google Scholar]
- 49.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]