Abstract
Objective
Diminished cholesterol efflux activity of apolipoprotein B (apoB)–depleted serum is associated with prevalent coronary artery disease, but its prognostic value for incident cardiovascular events is unclear. We investigated the relationship of cholesterol efflux activity with both prevalent coronary artery disease and incident development of major adverse cardiovascular events (death, myocardial infarction, or stroke).
Approach and Results
Cholesterol efflux activity from free cholesterol–enriched macrophages was measured in 2 case– control cohorts: (1) an angiographic cohort (n=1150) comprising stable subjects undergoing elective diagnostic coronary angiography and (2) an outpatient cohort (n=577). Analysis of media from cholesterol efflux assays revealed that the high-density lipoprotein fraction (1.063<d<1.21) contained only a minority (≈40%) of [14C]cholesterol released, with the majority found within the lipoprotein particle–depleted fraction, where ≈60% was recovered after apolipoprotein A1 immunoprecipitation. Albumin immunoprecipitation recovered another ≈30% of radiolabeled cholesterol within this fraction. Enhanced cholesterol efflux activity from ATP-binding cassette transporter A1–stimulated macrophages was associated with reduced risk of prevalent coronary artery disease in unadjusted models within both cohorts; however, the inverse risk relationship remained significant after adjustment for traditional coronary artery disease risk factors only within the outpatient cohort. Surprisingly, higher cholesterol efflux activity was associated with increase in prospective (3 years) risk of myocardial infarction/stroke (adjusted hazard ratio, 2.19; 95% confidence interval, 1.02–4.74) and major adverse cardiovascular events (adjusted hazard ratio, 1.85; 95% confidence interval, 1.11–3.06).
Conclusions
Heightened cholesterol efflux to apoB-depleted serum was paradoxically associated with increased prospective risk for myocardial infarction, stroke, and death. The majority of released radiolabeled cholesterol from macrophages in cholesterol efflux activity assays does not reside within a high-density lipoprotein particle.
Keywords: cholesterol efflux, high-density lipoprotein-cholesterol, macrophage, prognosis
Cholesterol ester-laden macrophages, classically known as foam cells, are prominent features of atherosclerotic lesions and are widely recognized as an early cellular hallmark of atherosclerotic plaque development and lesion progression during coronary artery disease (CAD).1 Cholesterol efflux from cholesterol ester-laden macrophages within the artery wall, the first and most likely rate-limiting step of the reverse cholesterol transport pathway, is critical in maintaining intracellular cholesterol homeostasis.2 Circulating high-density lipoprotein-cholesterol (HDLc) mass is inversely associated with incident cardiovascular disease risks, yet it is recognized to also serve as only a weak surrogate measure of HDL particle functionality in the reverse cholesterol transport process.2,3 Recent genetic studies question the causal relationship between low-circulating HDLc levels and heightened cardiovascular risks,4,5 and treatment strategies designed to raise HDLc levels have thus far not improved hard (ie, myo-cardial infarction [MI], stroke, and death) outcomes.5–7 Despite these issues, there is a general belief, and certainly a hope, that measures of HDL particle function, beyond HDLc mass, may provide additive clinical prognostic value, as well as serve as a guide for therapeutics targeting apolipoprotein A1 (apoA1) or HDLc elevation and the reverse cholesterol transport process.8
Recent clinical studies aimed at assessing functional measures of HDL efflux activity have provided some hope for the concept that HDL functional measures may provide improved prognostic value or aid in monitoring HDL-targeted therapies. Using polyethylene glycol (PEG) as a convenient way to precipitate apolipoprotein B (apoB)–containing lipoproteins from serum leaving apoB-depleted serum as a surrogate for HDL functional measures, the collaborative research team of Drs Rader, Rothblatt, and colleagues recently reported that the cholesterol efflux measured from free cholesterol (FC)–enriched cultured macrophages to apoB-depleted serum as cholesterol acceptor was inversely associated with the history of CAD independent of HDLc levels.9 These seminal studies raise the exciting possibility that assays that monitor some form of HDL functionality, as opposed to HDLc mass, may provide important and clinically relevant information.
Despite the exciting recent findings suggesting cell-based measures of cholesterol efflux activity may provide enhanced prognostic value for risk of prevalent CAD, it should be noted that to date, there is no information available on the relationship between macrophage cholesterol efflux activity measures from patient serum or plasma samples in large-scale clinical studies and incident cardiovascular event risks (eg, future risk for MI, stroke, or death). The use of cell-based measures in large-scale clinical studies is difficult and requires extreme care to demonstrate reproducibility, linearity with respect to time and concentration of intended measures, and characterization of assumptions inherent in what is being measured. In the case of macrophage cholesterol efflux activity measurements, it is fair to say that there is limited information reported on what activity measurements represent. For example, remarkably, analysis of what compartment (eg, HDL particle versus alternatives) within the media which radiolabeled cholesterol tracer released from macrophages resides in is not available. In the present studies, we attempt to answer several of these questions and investigate the relationship of cholesterol efflux activity measurement using apoB-depleted serum as cholesterol acceptor, and free radiolabeled cholesterol– enriched macrophages as cholesterol donor, with both prevalent CAD and incident major adverse cardiovascular event (MACE) risks (heart attack, stroke, or death).
Materials and Methods
Materials and Methods are available in the online-only Supplement.
Results
HDL Is a Minor Acceptor, and Lipid-Poor ApoA1 Forms a Significant Acceptor, of [14C]Cholesterol in Media Recovered From Macrophage Cholesterol Efflux Assays
Recent macrophage cholesterol efflux studies using patient samples have used apoB-depleted serum as a surrogate for HDL function by precipitating apoB-containing particles with addition of PEG.9,10 In initial control studies, we, therefore, sought to examine 2 basic assumptions in macrophage cholesterol efflux assays using PEG-treated serum: (1) the efficiency of PEG induced apoB depletion and the impact of PEG treatment on HDL-related parameters and (2) the compartments within the media that macrophage derived [14C]cholesterol partitions into (ie, what proportion of released radiolabeled cholesterol actually resides in a particle that has buoyant density characteristics of an HDL particle or is associated with apoA1?). Multiple serum samples from outpatient cohort and healthy volunteer pools with normal HDLc and apoA1 levels (Table I in the online-only Data Supplement) or an angiographic cohort (to assess Lp(a) removal efficiency) were treated with PEG using established methods to form apoB-depleted serum10,11 and then analyzed. Quantitative removal of apoB and Lp(a) (essentially no detectable remaining) and quantitative recovery of apoA1 (100.1±1.4%) and apoA2 (99.5±1.5%) were observed (Figure I in the online-only Data Supplement). In addition, reasonably complete recovery of HDLc (89.2±4.6%), the activity of the HDL-associated protein paraoxonase-1 (91.2±3.3%), and albumin (99.7±1.4%) were observed (Figure I in the online-only Data Supplement). Separate control studies confirmed the integrity of apoA1-containing HDL after PEG treatment (ie, that PEG treatment did not dissociate apoA1 from HDL) by showing that compared with control (vehicle-treated HDL), no significant change in recovery of apoA1 in HDL versus the d>1.21 fraction was observed in samples before versus after PEG treatment and repeat buoyant density ultracentrifugation isolation of the HDL fraction (Table II in the online-only Data Supplement). Collectively, these control studies showed reasonable selectivity for both recovery of HDL-related parameters and complete removal of apoB and Lp(a)-containing particles from apoB-depleted serum used for the macrophage cholesterol efflux experiments.
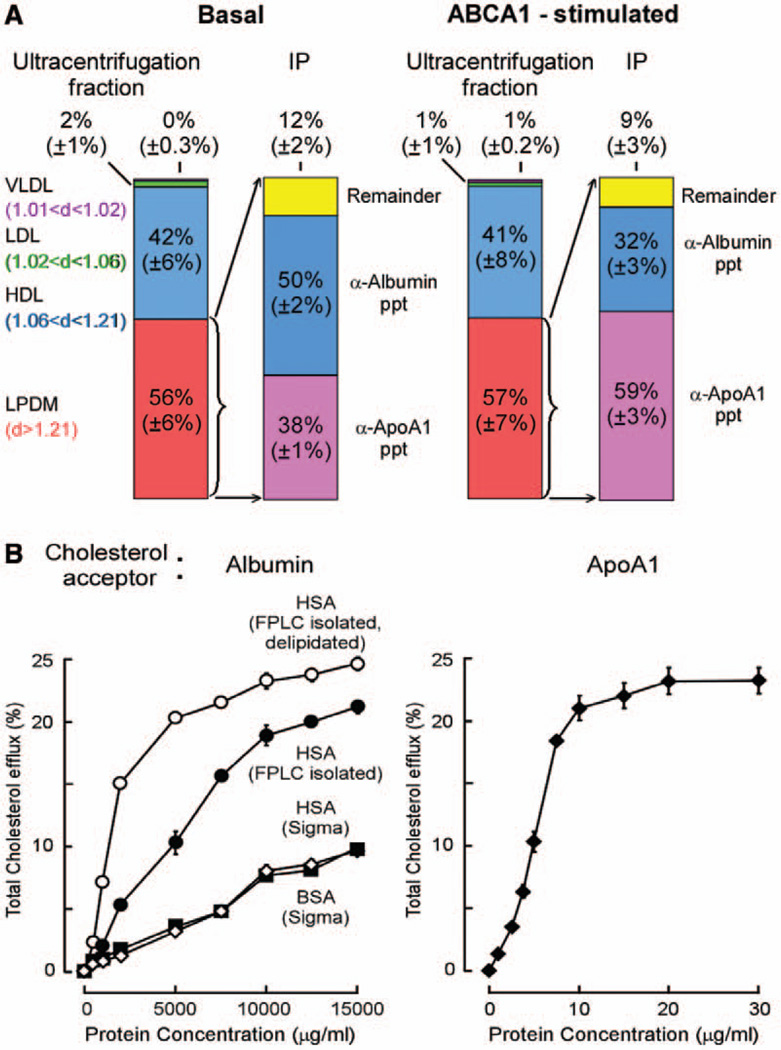
We next sought to test the assumption that HDL serves as the major acceptor of radiolabeled cholesterol in the macrophage cholesterol efflux experiment, a prerequisite for claiming that macrophage efflux experiments serve as a surrogate measure of HDL functionality. For these studies, different serum samples (n=4) from healthy volunteer pools were again used (normal range HDLc and apoA1 for each sample; Table I in the online-only Data Supplement). Cultured RAW264.7 macrophages were enriched with [14C]cholesterol as described under Methods in the online-only Data Supplement, and then apoB-depleted serum (1.4%) was used as cholesterol acceptor for macrophages under basal conditions, as well as after macrophage ATP-binding cassette transporter A1 (ABCA1) stimulation as described under Methods in the online-only Data Supplement. To separate the different lipoprotein fractions from recovered media for scintillation counting, we elected to use buoyant density isolation methods adjusting density stepwise with the low salt D2O/sucrose methodology, thus avoiding the chaotropic and high ionic strength issues associated with KBr.12 Figure 1A illustrates the distribution of recovered [14C]cholesterol in lipoprotein fractions within media from radiolabeled cholesterol–enriched macrophages under both basal (quiescent) state and on ABCA1 stimulation. Unexpectedly, the HDL fraction (1.063<d<1.21) harbored only a minority (≈42%) of [14C]cholesterol recovered in media from apoB-depleted serum under both conditions, with the majority of [14C]cholesterol (≈57%) found within the lipoprotein-depleted fraction. Further examination of the lipoprotein-depleted fraction within recovered media revealed that ≈60% of the radiolabeled cholesterol was associated with apoA1 and another ≈30% of radiolabeled cholesterol was associated with albumin (Figure 1A; Figures II and III in the online-only Data Supplement). Under basal condition, 38% of radiolabeled cholesterol was associated with apoA1 and 50% of radiolabeled cholesterol was associated with albumin. Thus, although HDL particles (1.063<d<1.21) are quantitatively only a minor acceptor of cholesterol in macrophage cholesterol efflux assays using apoB-depleted serum as cholesterol acceptor, the assays clearly do reflect apoA1 functionality in large part because 75% of total radiolabeled cholesterol recovered within media from the cultured macrophages was associated with apoA1.
Figure 1.
A, Distribution of radiolabeled choles terol found in various cholesterol acceptor serum fractions, RAW264.7 macrophages were incubated in the absence (basal) or presence (ATP-binding cassette transporter A1 [ABCA1] stimulated) of 8-Br-cAMP as indicated with media containing apoB-depleted serum (1.4% vol/vol) in cholesterol efflux assays, as described in Methods in the online-only Data Supplement. Radiolabeled cholesterol in the indicated lipoprotein and lipoprotein-depleted fractions (densities are indicated) after stepwise buoyant density ultracentrifugation was quantified as described in Methods in the online-only Data Supplement. The distribution of radiolabeled-cho-lesterol in lipoprotein-depleted media as assessed after immunoprecipitation (IP) of apolipoprotein A1 (apoA1) and albumin using anti-apoA1 mouse monoclonal antibodies and antialbumin antibodies as described in Methods in the online-only Data Supplement. Results represent mean±SD for 4 separate experiments. B, (Left) Dose–response curves of various sources of albumin (bovine and human albumin from Sigma; fast performance liquid chro-matography (FPLC) -isolated human serum albumin [HSA] and FPLC-isolated and delipidated HSA) on total cholesterol efflux in [3H]-cholesterol-loaded RAW cells, and (right) isolated human apoA1. HDL indicates high-density lipoprotein; LDL, low-density lipoprotein; and VLDL, very low–density lipoprotein.
Because of the somewhat surprising findings with human albumin (or an albumin-associated protein) serving as a quantitatively significant acceptor of cholesterol under the cholesterol efflux experimental conditions used, we elected to perform further studies examining human serum albumin. As shown, although a significantly poorer acceptor of cholesterol than apoA1, human albumin, nonetheless, promoted cholesterol efflux in a dose-dependent fashion with broad linear range (Figure 1B; see Figure IV in the online-only Data Supplement for human serum albumin purity). Further, somewhat surprisingly, freshly isolated human serum albumin of purity (>98%) even greater than that of commercial sources showed up to 5-fold enhanced cholesterol acceptor activity. Although the specific activity for cholesterol acceptor activity for human albumin is much lower than that of apoA1 (≈280-fold), because of its higher concentration, the predicted relative contribution of albumin to total cholesterol acceptor activity is approximately one-tenth that for apoA1 under normal plasma concentrations of albumin and apoA1 (Table III in the online-only Data Supplement). Collectively, between apoA1 and albumin, 88±1.5% of radiolabeled cholesterol acceptor activity was accounted for under basal (nonstimulated) conditions and 90±2% with ABCA1 stimulation (Figure 1).
Further Characterization of Cellular Cholesterol Efflux Activity Assay
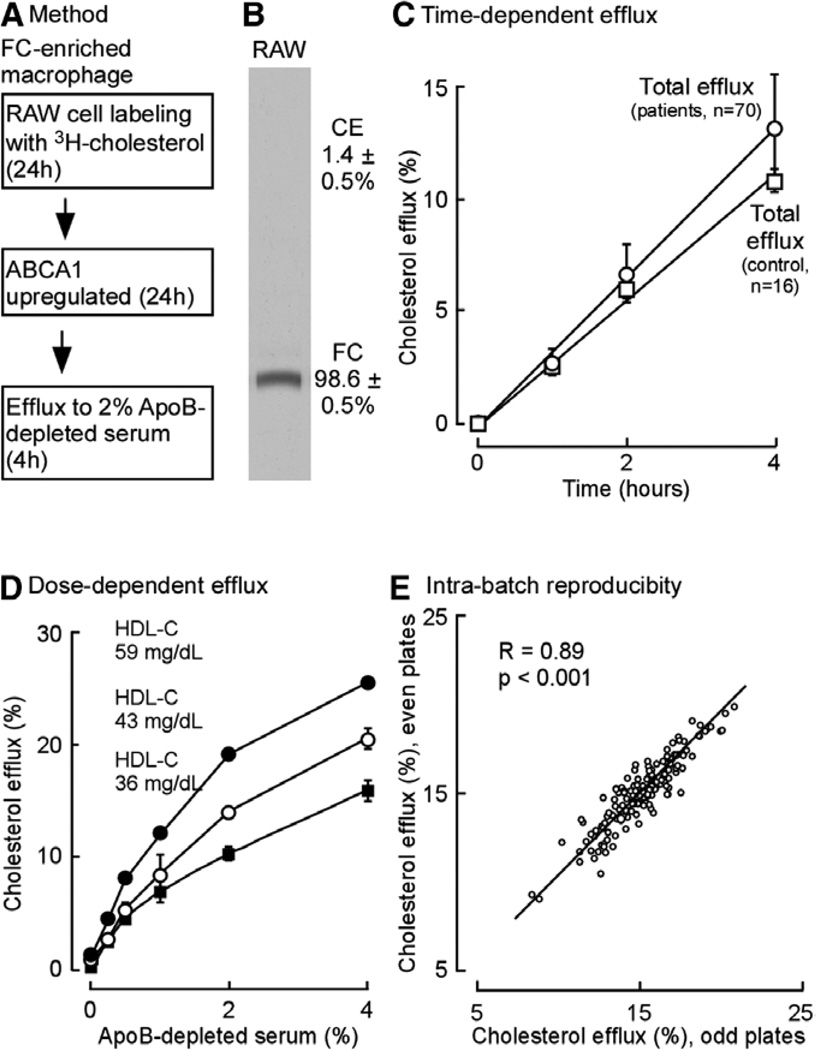
We next decided to examine the conditions used for cholesterol efflux activity assay using apoB-depleted serum as cholesterol acceptor. The cholesterol efflux activity assay used in the present studies is described in detail within Methods in the online-only Data Supplement. Figure 2 and Figures V and VI in the online-only Data Supplement provide assay characteristics and compare and contrast the assay used with different macrophage cell lines as well. Briefly, the assay format used is illustrated in Figure 2A following methodology similar to that recently reported by Drs Rader, Rothblat, and colleagues (Figure 2A).9,10 Here, macrophages (typically RAW264.7 cells, but also J774A.1 cells where indicated) were labeled with [14C or 3H] cholesterol, and then after stimulation of ABCA1 expression, cholesterol efflux was measured by counting radiolabeled cholesterol recovered in media containing apoB-depleted serum as cholesterol acceptor. Although a proprietary acylCoA:cholesterol acyl transferase inhibitor used by Drs Rader, Rothblatt, and colleagues9,10 to prevent labeling of the cholesterol ester pool was not available for use in the present studies, under the conditions used, virtually all radiolabeled cholesterol loaded into the macrophages was found to be free (98.6±0.5%), with only 1.4±0.5% found within the cholesterol ester pool (Figure 2B). Further assay characterization studies confirmed that the extent of cholesterol efflux activity measured from the FC-enriched macrophage efflux assay was linear over the time frame examined for both patient and healthy volunteer pooled samples under the conditions used (Figure 2C). Moreover, the final apoB-depleted serum concentration used in media in the present studies (2%) was chosen to be close to that used by Rader, Rothblat, and colleagues (2.8% apoB-depleted serum),9 despite the fact that total ABCA1-stimulated cholesterol efflux measured was within the curvilinear range of the graph examining final serum concentration versus efflux measurement (Figure 2D). Figure 2E illustrates the intra batch reproducibility of cholesterol efflux activity measures using the FC-enriched macrophage cholesterol efflux assay with apoB-depleted serum as the cholesterol acceptor from murine macrophage RAW 264.7 cells, the preferred cell type used throughout the duration of the studies. We selected the murine macrophage RAW 264.7 cell for most studies because they demonstrated, in our hands, better growing characteristics, more reproducible cholesterol labeling, and improved reproducibility of final efflux measures, likely related to improved adherence during wash steps. In addition, they show a modestly higher ABCA1-dependent efflux. However, because others have reported cholesterol efflux results using J774A.1 macrophages, as an additional control, we performed multiple control studies using macrophage cholesterol efflux assays using identical samples comparing results between murine macrophage RAW 264.7 cells and J774A.1 cells (first set of comparisons; Figure V in the online-only Data Supplement). For these studies, apoB-depleted serum as cholesterol acceptor was used from a random sampling of subjects with documented CAD (n=36) and subjects without known CAD (n=27) to ensure that comparable efflux results were observed among both disease and nondisease subjects using these distinct macrophage cell lines. As noted, both total cholesterol efflux and ABCA1-dependent efflux activities measured between these 2 cell lines under the conditions used are highly correlated (for total cholesterol efflux: R=0.92, P<0.001, for all subjects; and R=0.95 and 0.89, P<0.001 for each, for CAD, and non-CAD). Additional control studies showed that under the conditions used, interassay variations for cholesterol efflux measures from plate to plate across different days (control samples of 8 per plate, 304 plates total) showed excellent reproducibility, with overall coefficient of variation=5.3% throughout the study samples (Figure VI in the online-only Data Supplement).
Figure 2.
Cholesterol efflux assay methodology and characterization. A, General scheme of cholesterol efflux assay used. B, Autoradiogram and quantification of cellular [14C] free cholesterol (FC) and [14C]cholesterylester (CE) found in [14C] cholesterol-loaded macrophage RAW cells. C, Time course of total cholesterol efflux to 2% serum, vol/vol (pool made from random sampling of the indicated number [n] of patient samples from the outpatient cohort and control serum pool, high-density lipoprotein-cholesterol [HDLc] 59 mg/dL, used). D, Dose-dependent efflux for total cholesterol from RAW264.7 cells incubated with the indicated final concentration (vol/vol) of apolipoprotein B (apoB)–depleted human serum as cholesterol acceptor. Serum pools with different HDLc levels as indicated were used. Values shown are an average of at least triplicate measurements. E, Intra batch apoB-depleted serum total cholesterol efflux assay reproducibility was plotted as even plates vs odd plates in the same batch, Spearman correlation coeffi-cient (R=0.89; P<0.001). ABCA1 indicates ATP-binding cassette transporter A1.
Confrmation of Inverse Association Between Cholesterol Efflux Activity and Prevalent CAD Using ApoB-Depleted Serum as Cholesterol Acceptor From FC-Enriched Macrophages
The 2 study cohorts examined consisted of a total of 1727 subjects with baseline clinical characteristics summarized in Table 1 according to cohorts and stratified by CAD status. As expected, subjects with CAD in either the angiographic cohort (cohort A) or the outpatient cohort (cohort B) had a greater prevalence of cardiovascular risk factors, such as diabetes mellitus, hypertension, smoking, elevated body mass index, and more frequent use of cardiovascular drugs. Subjects with CAD in both cohorts were more likely to have lower HDLc and apoA1 levels.
Table 1.
Baseline Characteristics of the Case–Control Cohorts
| Cohort A: Stable Angiographic Case–Control Cohort (n=1150) |
Cohort B: Outpatient Case–Control Cohort (n=577) |
|||||
|---|---|---|---|---|---|---|
| Characteristics | Controls (n=279) | Patients With Angiographically Confrmed CAD (n=871) |
P Value | Controls (n=431) | Patients With CAD (n=146) |
P Value |
| Age, y | 72±6 | 61±11 | <0.001 | 53±15 | 59±11 | <0.001 |
| Sex (men), % | 54 | 67 | <0.001 | 35 | 70 | <0.001 |
| DM, % | 11 | 26 | <0.001 | 6 | 30 | <0.001 |
| HTN, % | 63 | 75 | <0.001 | 26 | 66 | <0.001 |
| Smoking, % | 54 | 69 | <0.001 | 8 | 12 | 0.183 |
| CAD, % | 0 | 100 | <0.001 | 0 | 100 | <0.001 |
| Total cholesterol, mg/dL |
161 (145–187) | 164 (142–188) | 0.784 | 199 (171–229) | 179 (130–214) | <0.001 |
| LDL, mg/dL | 97 (82–113) | 96 (79–117) | 0.975 | 117 (94–145) | 89 (61–131) | <0.001 |
| HDL, mg/dL | 39 (32–46) | 33 (28–39) | <0.001 | 53 (45–65) | 44 (36–52) | <0.001 |
| Triglycerides, mg/dL | 89 (69–128) | 131 (96–189) | <0.001 | 112 (79–162) | 136 (82–214) | 0.003 |
| Albumin, g/dL | 3.9 (3.7–4.1) | 4.1 (3.9–4.3) | <0.001 | 4.4 (4.2–4.6) | 4.5 (4.2–4.7) | 0.001 |
| apoA1, mg/dL | 125 (107–138) | 116 (105–132) | <0.001 | 149 (131–169) | 136 (121–146) | <0.001 |
| apoA2, mg/dL | 32 (28–35) | 33 (29–36) | 0.01 | 38 (34–43) | 33 (27–38) | <0.001 |
| Framingham ATP III risk score |
9 (8–12) | 8 (6–11) | <0.001 | 4 (2–8) | 6 (2–8) | 0.122 |
| BMI, kg/m2 | 26.8 (24–31.4) | 28.7 (26–32.2) | <0.001 | 29.4 (24.7–34.1) | 31.2 (27.4–34.1) | 0.036 |
| Baseline medications, % | ||||||
| ACE inhibitors | 41 | 53 | 0.001 | 5 | 37 | <0.001 |
| β-Blockers | 43 | 72 | <0.001 | 5 | 56 | <0.001 |
| Statin | 32 | 71 | <0.001 | 11 | 59 | <0.001 |
| Aspirin | 58 | 83 | <0.001 | 50 | 60 | 0.138 |
ACE indicates angiotensin-converting enzyme; apo, apolipoprotein; BMI, body mass index; CAD, coronary artery disease; DM, diabetes mellitus; HDL, high-density lipoprotein; HTN, hypertension; and LDL, low-density lipoprotein.
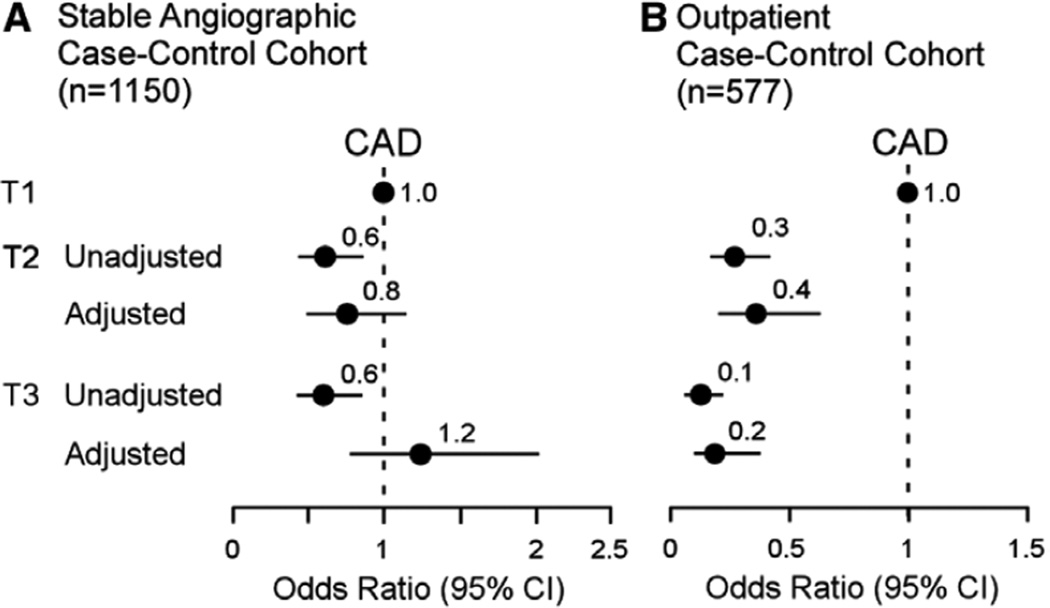
As expected, cholesterol efflux activity to apoB-depleted serum as cholesterol acceptor was inversely associated with risk of prevalent CAD in unadjusted models within both the stable angiographic cohort (unadjusted odds ratio, 0.60; 95% confidence interval [CI], 0.42–0.85; P<0.01) and the outpatient cohort (unadjusted odds ratio, 0.11; 95% CI, 0.06–0.20; P<0.01; Figure 3A and 3B). After adjustment for traditional risk factors, the inverse risk for prevalent CAD associated with elevated cholesterol efflux was attenuated within the stable angiographic cohort, but remained significant within the outpatient cohort (Figure 3A and 3B).
Figure 3.
Forrest plot indicating prevalent coronary artery disease (CAD) risk in stable angiographic and outpatient cohorts. Apolipoprotein B–depleted serum as the cholesterol acceptor in cholesterol efflux assays. A, Relationship between total cholesterol efflux activity and prevalent CAD plotted from low to high tertiles in the angiographic cohort. B, Outpatient cohort. Multilogistic regression model included adjustments for age, sex, smoking, diabetes mel-litus, hypertension, low-density lipoprotein-cholesterol, and high-density lipoprotein-cholesterol levels. Patient sample size (n) is indicated. The 5% to 95% confidence interval (CI) is indicated by line length.
Paradoxical Finding of Positive Association Between Enhanced Cholesterol Efflux Activity and Increased Risk for Incident Major Adverse Cardiovascular Events
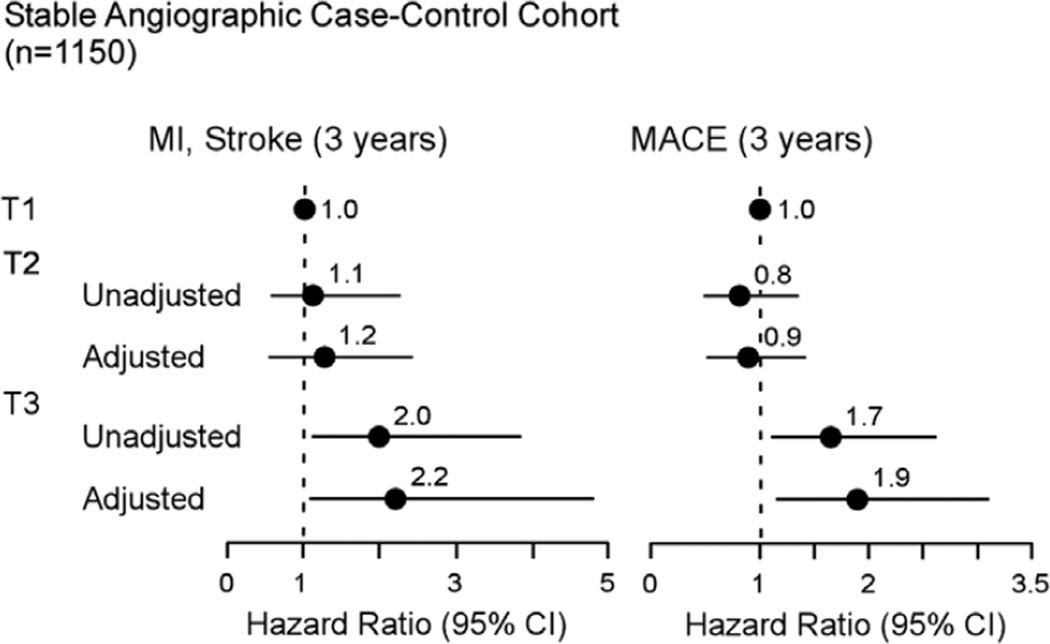
We next examined the relationship between cholesterol efflux activity and incident risk for MACE (MI, stroke, or death) over the ensuing 3-year period after sample collection from subjects within the stable angiographic cohort, the only cohort with longitudinal outcome data. Surprisingly, subjects in the highest tertile of cholesterol efflux activity (relative to lowest tertile) showed a significantly higher risk for incident nonfatal MI/stroke (unadjusted hazards ratio, 1.98; 95% CI, 1.04–3.78; P<0.05) and increased risk of incident MACE (unadjusted hazards ratio, 1.66; 95% CI, 1.07–2.58; P<0.05). These positive associations remained significant after adjustments for traditional cardiovascular risk factors, with subjects having highest versus lowest tertile of cholesterol efflux still showing increased risk of incident MI/stroke (adjusted hazards ratio, 2.19; 95% CI, 1.02– 4.74; P<0.05) and incident MACE at 3 years (adjusted hazards ratio, 1.85; 95% CI, 1.11–3.06; P<0.05; Figure 4).
Figure 4.
Forrest plot indicating incident cardiovascular risks for the stable angiographic cohort. Relationship between total cholesterol efflux activity and incident (3 years) risk of myocardial infarction (MI)/stroke (left) or major adverse cardiovascular event (MACE; MI, stroke, or death; right) plotted from low to high tertiles. Multilogistic regression model included either no adjustments or adjustments for age, sex, smoking, diabetes mellitus, hypertension, low-density lipoprotein-cholesterol, and high-density lipoprotein-cholesterol levels as indicated. The 5% to 95% confdence interval (CI) is indicated by line length.
The observation of higher cholesterol efflux being associated with higher incident MACE risks was surprising. We, therefore, examined the relationships between the cholesterol efflux activity measured and HDL-related parameters, as well as other blood-based assays. As expected, strong and statistically significant positive associations were noted between cholesterol efflux activity measured and levels of HDLc, apoA1, and apoA2 within both the angiographic cohort and the outpatient cohort (Table 2). Further, the magnitude of the observed positive associations was similar to that previously reported using similar cholesterol efflux activity assays with apoB-depleted serum as cholesterol acceptor.9 In a further effort to understand the associations observed between cholesterol efflux measures and lipoproteinrelated parameters, we stratified each cohort by the presence versus absence of cardiovascular phenotypes (eg, CAD versus non-CAD for both cohorts; and also presence versus absence of incident MI/stroke or MACE in the stable angiographic cohort where longitudinal outcomes were available). These analyses still showed within each subgroup the anticipated positive association between enhanced cholesterol efflux measurement and enhanced level of HDLc, and HDL-related lipoproteins apoA1 and apoA2 (Table IV in the online-only Data Supplement). Thus, the cholesterol efflux measures performed all showed positive associations, as expected, with HDL and HDL-related lipoprotein measures within the entire cohort and within the different subgroups.
Table 2.
Correlation Coeffcients Between High-Density Lipoprotein/Lipoprotein-Related Variables and Apolipoprotein B–Depleted Serum Total Cholesterol Efflux Cholesterol Efflux
| ApoB-Depleted Serum Total Cholesterol Efflux |
||
|---|---|---|
| Angiographic Cohort (n=1150) |
Outpatient Cohort (n=577) | |
| HDL cholesterol | 0.45 (P<0.001) | 0.52 (P<0.001) |
| apoA1 | 0.56 (P<0.001) | 0.61 (P<0.001) |
| apoA2 | 0.45 (P<0.001) | 0.55 (P<0.001) |
| Albumin | 0.04 (P=0.19) | −0.05 (P=0.236) |
apo indicates apolipoprotein; and HDL, high-density lipoprotein.
In an additional series of analyses, we also thought it reasonable to examine whether traditional cardiovascular risk factors associate with prevalent and incident cardiovascular risks as anticipated in the stable angiographic cohort given the unanticipated findings. Comparison of several recognized cardiovascular risk factors and the cholesterol efflux measures performed versus risk for prevalent CAD or incident (3 years) MACE in multiple logistic regression models is shown in Figure VII in the online-only Data Supplement. As expected, diabetes mellitus, hypertension and smoking were each associated to increased risk of CAD and showed strong trend toward increased risk of MACE, whereas HDLc level was inversely associated with prevalent risk of CAD and showed trend toward negative association with incident MACE risk. Low-density lipoprotein-cholesterol in this cohort was not associated with either CAD or MACE risk, a finding observed previously and commonly seen among highly medicated cohorts. Remarkably, total cholesterol efflux activity (here modeled as continuous variable) showed strong trend toward increased risk of CAD and significant positive association with incident risk of MACE at 3 years and with point estimate for MACE risk similar in magnitude to that observed for diabetes mellitus, hypertension, and smoking (Figure VII in the online-only Data Supplement).
Discussion
This study was initially intended to answer some presumably simple questions about cellular cholesterol efflux activity measures and incident risks for cardiovascular disease. In the end, however, it has generated more questions than it has answered. First and foremost perhaps is the question of what exactly do radiolabeled cholesterol efflux activity assays as recently reported and performed herein actually measure?
One simple yet key finding is the observation that the majority of radiolabeled FC tracer released from cholesterol-enriched macrophages does not reside within the HDL particle, but rather, within the lipoprotein-depleted fraction after buoyant density removal of lipoprotein particles. This partitioning was initially observed with traditional KBr-dependent buoyant density isolation of lipoprotein fractions from cell efflux assay media (not shown). Because of concerns of lipoprotein composition alterations and release of exchangeable lipoproteins from particles under the high salt concentrations that exist during such isolation procedures, we, therefore, opted to repeat all studies using the low salt, D2O/sucrose method for lipoprotein ultracentrifugation isolations to minimize apoA1 shedding from the HDL particle. Despite this precaution, we still observed the same surprising results that the majority of counts reside within the lipoprotein-depleted fraction (Figure 1). Further analyses of the lipoprotein-depleted media fraction remaining after removal of lipoproteins revealed ≈60% of the counts are associated with apoA1, with a full 40% remaining despite quantitative removal of apoA1. Thus, ≈75% of radiolabeled cholesterol interacts with apoA1 as cholesterol acceptor within media, but this observation also begs the question of what the other major cholesterol acceptors are during the cholesterol efflux activity assay.
To investigate which other proteins might participate in cholesterol acceptance in these assays, we considered other exchangeable lipoproteins (eg, apoE, apoCs, etc) or amphipathic proteins, such as serum amyloid A, because other exchangeable lipoproteins13 have been reported to also be capable of serving as cholesterol acceptors, although their contribution within the serum compartment remains to be established. However, early on we performed immunoprecipitation studies for human albumin and observed that the vast majority of residual counts in the lipoprotein-depleted media, not counting the apoA1 contribution, could be accounted for by albumin immunodepletion, hence we pursued this line of inquiry in the present studies. We suspect significant proportions of these counts bind directly to albumin, but also recognize that the albumin-associated proteome is vast, and think it prudent to note that we cannot exclude the possibility that trace levels of ≥1 albumin-associated (lipo)proteins with cholesterol acceptor activity (especially if comparable with apoA1, which is ≈300-fold higher than albumin per gram of protein) may coimmunoprecipitate with the albumin, and thus theoretically could contribute to a portion of the cholesterol acceptor activity attributed to albumin. Our data with highly purified albumin with no visible-associated lipoproteins clearly show that albumin itself can promote cholesterol efflux, albeit at a far poorer specific activity than apoA1. It is also interesting to note that other investigators recently noted recombi-nant human albumin can serve as cholesterol acceptor and showed that several site-specific mutations can significantly reduce the cholesterol acceptor activity of the protein.14 It is important to note that we observed different sources of human serum albumin had significantly different cholesterol acceptor activity, suggesting that a conformationally intact albumin is needed for full cholesterol acceptor activity.
Another question the present studies raise is whether apoB-depleted serum even represents a reasonable estimate of cholesterol acceptor activity within the vascular compartment. We chose to use apoB-depleted serum in the present studies because the seminal studies of Khera et al9 suggested that it might serve as a good functional measure of HDL and might predict incident CVD risks. However, apoB-containing lipoprotein particles are known acceptors of cholesterol,15,16 and red blood cells represent a dynamic pool for cholesterol exchange and participates in reverse cholesterol transport.17 Recognition that HDL particles serve as only a minor acceptor (≈40%) of radiolabeled cholesterol within apoB-depleted serum during the currently reported cholesterol efflux activity assay provides rationale to question whether such assays serve as a surrogate measure for HDL functional activity. As discussed below, the assay may reflect even more importantly the lipid-poor apoA1 pool and its relationship to incident MACE risk.
Perhaps the most surprising finding within this study is how complex the relationship is between cellular cholesterol efflux measurements and cardiovascular phenotypes (atherosclerotic plaque development, which is related to prevalent CAD, versus plaque vulnerability-associated phenotypes, such as incident MI/stroke or MACE risks). Review of the literature reveals that prior studies have suggested possible complications to the simplistic view that measures of cholesterol efflux activity are inversely related to cardiac risks. For example, de Vries et al18 reported that studies using a fibroblast cell line in a small nested case–control design for cardiovascular disease observed that cholesterol efflux measures were not significantly correlated with cardiovascular events. In a different study by Chirinos et al,19 cholesterol efflux activity was measured in vitro using cultured human skin fibroblasts by incubation with serum from subjects undergoing coronary angiography. Efflux in this assay was not measured by radiola-beled cholesterol liberated into media, but rather, by the ability of serum to deplete the intracellular cholesterol pool available for esterification by the acylCoA:cholesterol acyl transferase reaction (ie, higher efflux was indicated by lower cellular acylCoA:cholesterol acyl transferase activity). Decreased cellular acylCoA:cholesterol acyl transferase activity in this small case–control study was independently positively associated with increased risk of MACE and death,19 similar to the results observed in the present studies. In another small study, cholesterol efflux to plasma from hypertriglyceridemic patients with diabetes mellitus, subjects with a CAD risk equivalent, was increased compared with efflux to plasma from those with normotriglyceridemic or healthy controls.20 Finally, in a recent case–control study of obese subjects, plasmas from insulin-resistant individuals showed greater cholesterol efflux activity compared with subjects demonstrating insulin sensitivity.21
Each of the above studies was small, used alternative cell types, and alternative cholesterol acceptors (whole serum, or plasma, and not apoB-depleted serum). They also looked at different aspects of cholesterol efflux (either tracer studies or cellular cholesterol mass in 1 case). But all underscore the large number of possible assays and methodologies, and the possibility that the selection of the cellular cholesterol efflux system may be a critical determinant in performance of such ex vivo HDL functionality assays. One strength of the present studies is it large size, and the efforts made to perform assays under conditions that closely mirror those of the seminal findings of Khera et al.9 It is worth noting that using such an assay, and both study design and patient populations similar to that recently reported,9 we too observed that cholesterol efflux activity using apoB-depleted serum as cholesterol acceptor and FC-labeled macrophages was inversely associated (unadjusted) with prevalent CAD status in both cohorts examined. We also observed the anticipated positive associations between cholesterol efflux measures and levels of HDLc, and HDL-related lipoproteins (apoA1 and apoA2) within both cohorts and within subjects with versus without various cardiovascular disease phenotypes. Two important differences between this study and that recently reported9 are the selection criterion of patient cohort used and the distribution of cholesterol efflux values within each population. In the previous report,9 the majority of the patients were a small subset selected from 2 much larger clinical studies and assigned to either case or control status. In contrast, the main results reported here (angiographic cohort) were obtained from sequential participants enrolled in the study GeneBank.22–26 The distribution of values for cholesterol efflux was much broader in the case– control study reported by Khera et al,9 with max/min ratio equal to 8. In contrast, the sequential subjects from the angio-graphic cohort studied herein demonstrated a max/min ratio for cholesterol efflux measures equal to only 3. This narrower distribution of values likely contributes to the loss of statistical significance in the relationship between CAD prevalence and cellular cholesterol efflux after adjustment for other risk factors in the angiographic cohort. Notably, in the sequential outpatient cohort used in this study, we also observed a strong inverse correlation that remained significant after adjustment for traditional risks factors between cellular cholesterol efflux measured using apoB-depleted serum as cholesterol acceptor and the prevalence of CAD. Consequently, the strength of relationship between prevalence of CAD and cholesterol efflux seems to be cohort dependent.
However, a totally unanticipated observation was the positive association between increased cellular cholesterol efflux measures and increased prospective risks for cardiovascular events (MI/stroke and MACE). Control studies confirmed that macrophage cell type did not have significant effect on the cholesterol efflux measures because comparisons between J774A.1 and RAW264.7 macrophages revealed highly correlated assay values among both patients and healthy control subjects alike (Figure V in the online-only Data Supplement). In a separate set of control studies comparing the 2 distinct macrophage cell lines, similar results were observed—here for apoB-depleted serum from 80 random subjects to compare total and cAMP-independent cholesterol efflux elicited from either RAW 264.7 or J774A.1 cells (Figures VIII and VIIII in the online-only Data Supplement). Under the conditions used, the absolute magnitude of the cAMP-independent efflux was identical for both cell lines within the accuracy of the assay and highly correlated (R=0.96; P<0.001). Although the magnitude of the total cholesterol efflux in the presence of cAMP was almost 2× higher for the RAW264.7 than for J774A.1 cells, the correlation of results between those cell lines remained excellent (R=0.91; P<0.001). The major difference between those 2 cell lines was the magnitude, both absolute and relative, for the cAMP-dependent cholesterol efflux. Results obtained with the J774A.1 cell line, described above, are remarkably consistent with those published10 in a methodological characterization of the assay that was subsequently used to characterize the relationship between prevalence of CAD and cholesterol efflux.9 This is true with regard to both absolute magnitude of the cholesterol efflux and minor contribution of the cAMP-dependent component to the total cholesterol efflux (Figure 110). Further, it should be noted that in separate analyses, the relationship between apoA1 levels and incident MACE risk within the stable angiographic cohort showed the anticipated inverse association, with subjects in the lowest 5 percentile (<89 mg/dL) versus the highest 5 per-centile (≥153 mg/dL) of apoA1 values having a frequency of experiencing MACE (3 years) of 22.2% versus 10.2%, respectively. Thus, on the whole, congruent results were observed with prior published studies using apoB-depleted serum and the present studies, and the anticipated inverse relationship between apoA1 levels and incident MACE risk.
Thus, perhaps the paradoxical relationship observed between higher cholesterol efflux and higher prospective risk for cardiovascular events in the present study is not paradoxical at all. The name cholesterol efflux activity conjures images of an active function of the target cell, pumping cholesterol into the media for a passively waiting acceptor. Perhaps the name of the assay itself is somewhat of a misnomer. One interpretation of the present observations is that the capacity of the media (in this case, apoB-depleted serum) to accept cholesterol itself is an equally relevant measure and is related to a subject’s propensity to develop vulnerable plaque (ie, incident cardiovascular event risk). Indeed, enhanced cholesterol acceptor capacity within the apoB-depleted serum fraction was positively associated with increased 3-year incident risks for MI/stroke and MACE (MI/stroke or death). It also begs mentioning that there may be a disconnect between cholesterol efflux measures and the development of atherosclerotic plaque, versus the development of vulnerable plaque. Further examination of these relationships is clearly warranted and in alternative types of patient populations. It should also be noted that the magnitude of the positive association between the efflux measures made and prospective risks for MI, stroke, or death in the present studies was quite large and significant. Moreover, it remained significant with minimal diminution after adjustments for traditional cardiovascular risk factors (Figure 4; Figure VII in the online-only Data Supplement).
The present analyses are, to our knowledge, the first larger scale prospective study that determines the association of cellular cholesterol efflux activity using apoB-depleted serum as cholesterol acceptor with both prevalent CAD disease risks and future risks for experiencing MACE. We speculate that ABCA1-dependent cholesterol efflux pathway may play a key role in these apparently paradoxical results because using apoB-depleted serum as cholesterol acceptor, ABCA1-dependent cholesterol efflux activity represents a significant proportion of total efflux activity measured under the conditions used (where ABCA1 levels were stimulated). The use of alternative efflux activity assays, whether following cholesterol mass or alternative cholesterol efflux pathways, may provide different results. The relationship between such analyses and incident risks for MACE remains to be reported. Smaller, lipid-poor pre-β-HDL particles, named for their electropho-retic behavior and not for their buoyant density, are reported to be primary acceptors of cholesterol from the ABCA1 transporter in macrophages.3,11,27–29 Previous studies have reported that ABCA1-dependent cholesterol efflux is correlated with the concentration of pre-β-HDL.10 Further, pre–β-HDL is reportedly positively correlated with coronary heart disease and history of MI.30–32 These latter studies are not cellular cholesterol efflux activity measures, but rather, quantify lipid-poor apoA1 forms, or in 1 case, cholesterol exchange into a low molecular weight form apoA1-containing species as measured by an ultrafiltration-isotope dilution technique.30–32 T o our knowledge, what proportion, if any, of pre-β-HDL particles have density of an HDL particle (between 1.063 and 1.21) is unknown. The majority of radiolabeled cholesterol released to the media during the current cholesterol efflux measurements, whether using basal or ABCA1-stimulated macrophages, remained in the lipoprotein-depleted compartment, although a significant portion of the counts within the lipoprotein-depleted fraction was associated with apoA1. It is conceivable that subject sera with greatest ability to accept cholesterol may contain increased levels of lipid poor and not HDL-associated apoA1 or other lipoproteins, although this remains speculative and merits further investigation. Indeed, lipoprotein subfractionation studies were not performed in the present cohort and is another limitation of the present studies. Whether such measures track with cholesterol efflux measures with apoB-depleted serum as cholesterol acceptor, or incident MACE risk, is a question that requires further investigation. Examination of the correlations between cholesterol efflux measures among the different subjects in the cohorts examined demonstrates an interesting trend in all subcohorts (Table II in the online-only Data Supplement) for decreased strength of the correlation between the cholesterol efflux measured and the HDL-related parameter (HDLc, apoA1, and apoA2) in disease versus nondisease subgroups, suggesting a weaker (as a result of dysfunctional component?) association during cardiovascular disease. It is noteworthy that we have shown that oxidative modification of HDL by the myeloperoxi-dase system leads to functional impairment (loss of ABCA1 cholesterol efflux activity) and loss of lipid binding function, in general, for the oxidized apoA1.33
Recent large-scale genetic studies in humans raise doubts as to whether genetic variants that control circulating HDLc concentrations are causally linked to prevalent cardiovascular disease risks and atherosclerotic heart disease pathogenesis.4 These results, coupled with the recognition that HDLc mass is not a reliable index of cholesterol flux through the HDL particle/pathway, have led for the search for assays that both gauge HDL functions and may serve as aids in guiding HDL and apoA1-targeted therapies currently under investigation. The present results challenge several established views regarding the cellular cholesterol efflux activity assay and point for the need of additional studies to better understand both what these assays are monitoring and how best to monitor the many distinct functions of HDL in a practical manner amenable to translation into clinical studies, and preferably, clinical practice. One last finding of the present studies that is worth highlighting is the positive association between measured cellular cholesterol efflux and incident MACE risk observed. This relationship was quite strong and remained significant after multivariate adjustments. The biological process(es) it measures seems to track with incident MACE risk. The genetic variants and key biochemical determinants that control cholesterol acceptor capacity of a subject (at least for apoB-depleted serum) warrant further investigation, as do further studies examining the effect of using alternative cholesterol acceptors, such as whole serum.
Supplementary Material
Significance.
Despite observing diminished cholesterol efflux activity of apolipoprotein B–depleted serum is associated with prevalent coronary artery disease, heightened cholesterol efflux to apolipoprotein B–depleted serum was paradoxically associated with increased prospective risk for myocardial infarction, stroke, and death. The majority of released radiolabeled cholesterol from macrophages in cholesterol efflux activity assays does not reside within an high-density lipoprotein particle, although 75% was associated with apolipoprotein A1. The present studies imply that subjects with apolipoprotein B–depleted sera with greatest capacity to accept cholesterol from cholesterol-laden macrophages are at greatest prospective risk for myocardial infarction, stroke, or death. Further development and characterization of high-density lipoprotein functional measures and their relationship with incident cardiovascular event risks are needed.
Acknowledgments
We thank Michael Pepoy, Barbara Sullivan, Sarah Neale, Alan Pratt, Thomas Tallant, Jiannong Dai, Haihong Guo, Desire Riedy, and Alys Jordan for their assistance.
Sources of Funding
This research was supported by National Institutes of Health grant P01HL098055 and by the Fondation LeDucq. GeneBank has been supported by National Institutes of Health grants P01HL076491, R01HL103866, R01HL103931, and P20HL113452 and the Cleveland Clinic Clinical Research Unit of the Case Western Reserve University The Clinical and Translational Science Collaborative (UL1TR 000439-06). Dr Hazen is also partially supported by a gift from the Leonard Krieger Foundation.
Footnotes
The online-only Data Supplement is available with this article at http://atvb.ahajournals.org/lookup/suppl/doi:10.1161/ATVBAHA.113.301373/-/DC1.
Disclosures
Dr Tang has previously received research grant support from Abbott Laboratories. Drs Hazen and Smith report being listed as coinventors on pending and issued patents held by the Cleveland Clinic relating to cardiovascular diagnostics and therapeutics. Dr Hazen reports having been paid as a consultant or speaker for the following companies: Abbott Diagnostics, Cleveland Heart Laboratory, Esperion, Lilly, Liposcience Inc, Merck & Co, Inc, and Pfizer Inc. Dr Hazen reports receiving research funds from Abbott, Cleveland Heart Laboratory, Liposcience Inc, and Pfizer Inc. Dr Hazen reports having the right to receive royalty payments for inventions or discoveries related to cardiovascular diagnostics or therapeutics from the companies shown below: Abbott Laboratories, Inc, Cleveland Heart Laboratory, Esperion, Frantz Biomarkers, LLC, Liposcience Inc, and Siemens. Dr Smith reports having been paid as a consultant and receiving research funds from for Esperion. Dr Smith reports having the right to receive royalty payments for inventions or discoveries related to cardiovascular diagnostics or therapeutics from Cleveland Heart Laboratory and Esperion. Dr Mosior is an employee of Eli Lilly and Company and owns Eli Lilly company stock.
References
- 1.Maxfield FR, Tabas I. Role of cholesterol and lipid organization in disease. Nature. 2005;438:612–621. doi: 10.1038/nature04399. [DOI] [PubMed] [Google Scholar]
- 2.Rosenson RS, Brewer HB, Jr, Davidson WS, Fayad ZA, Fuster V, Goldstein J, Hellerstein M, Jiang XC, Phillips MC, Rader DJ, Remaley AT, Rothblat GH, Tall AR, Yvan-Charvet L. Cholesterol efflux and atheroprotection: advancing the concept of reverse cholesterol transport. Circulation. 2012;125:1905–1919. doi: 10.1161/CIRCULATIONAHA.111.066589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navab M, Reddy ST, Van Lenten BJ, Fogelman AM. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011;8:222–232. doi: 10.1038/nrcardio.2010.222. [DOI] [PubMed] [Google Scholar]
- 4.Voight BF, Peloso GM, Orho-Melander M, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380:572–580. doi: 10.1016/S0140-6736(12)60312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, McBride R, Teo K, Weintraub W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–2267. doi: 10.1056/NEJMoa1107579. [DOI] [PubMed] [Google Scholar]
- 6.Nissen SE, Tuzcu EM, Brewer HB, Sipahi I, Nicholls SJ, Ganz P, Schoenhagen P, Waters DD, Pepine CJ, Crowe TD, Davidson MH, Deanfield JE, Wisniewski LM, Hanyok JJ, Kassalow LM. ACATIntravascular Atherosclerosis Treatment Evaluation (ACTIVATE) Investigators Effect of ACAT inhibition on the progression of coronary atherosclerosis. N Engl J Med. 2006;354:1253–1263. doi: 10.1056/NEJMoa054699. [DOI] [PubMed] [Google Scholar]
- 7.Nissen SE, Tardif JC, Nicholls SJ, Revkin JH, Shear CL, Duggan WT, Ruzyllo W, Bachinsky WB, Lasala GP, Lasala GP, Tuzcu EM. ILLUSTRATE Investigators Effect of torcetrapib on the progression of coronary atherosclerosis. N Engl J Med. 2007;356:1304–1316. doi: 10.1056/NEJMoa070635. [DOI] [PubMed] [Google Scholar]
- 8.Rader DJ, Tall AR. The not-so-simple HDL story: Is it time to revise the HDL cholesterol hypothesis? Nat Med. 2012;18:1344–1346. doi: 10.1038/nm.2937. [DOI] [PubMed] [Google Scholar]
- 9.Khera AV, Cuchel M, de la Llera-Moya M, Rodrigues A, Burke MF, Jafri K, French BC, Phillips JA, Mucksavage ML, Wilensky RL, Mohler ER, Rothblat GH, Rader DJ. Cholesterol efflux capacity, high-density lipopro-tein function, and atherosclerosis. N Engl J Med. 2011;364:127–135. doi: 10.1056/NEJMoa1001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de la Llera-Moya M, Drazul-Schrader D, Asztalos BF, Cuchel M, Rader DJ, Rothblat GH. The ability to promote efflux via ABCA1 determines the capacity of serum specimens with similar high-density lipoprotein cholesterol to remove cholesterol from macrophages. Arterioscler Thromb Vasc Biol. 2010;30:796–801. doi: 10.1161/ATVBAHA.109.199158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asztalos BF, de la Llera-Moya M, Dallal GE, Horvath KV, Schaefer EJ, Rothblat GH. Differential effects of HDL subpopulations on cellular ABCA1- and SR-BI-mediated cholesterol efflux. J Lipid Res. 2005;46:2246–2253. doi: 10.1194/jlr.M500187-JLR200. [DOI] [PubMed] [Google Scholar]
- 12.Ståhlman M, Davidsson P, Kanmert I, Rosengren B, Borén J, Fagerberg B, Camejo G. Proteomics and lipids of lipoproteins isolated at low salt concentrations in D2O/sucrose or in KBr. J Lipid Res. 2008;49:481–490. doi: 10.1194/jlr.D700025-JLR200. [DOI] [PubMed] [Google Scholar]
- 13.Travis AJ, Kopf GS. The role of cholesterol efflux in regulating the fertilization potential of mammalian spermatozoa. J Clin Invest. 2002;110:731–736. doi: 10.1172/JCI16392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ha JS, Ha CE, Chao JT, Petersen CE, Theriault A, Bhagavan NV. Human serum albumin and its structural variants mediate cholesterol efflux from cultured endothelial cells. Biochim Biophys Acta. 2003;1640:119–128. doi: 10.1016/s0167-4889(03)00027-2. [DOI] [PubMed] [Google Scholar]
- 15.Brown MS, Goldstein JL. The receptor model for transport of cholesterol in plasma. Ann N Y Acad Sci. 1985;454:178–182. doi: 10.1111/j.1749-6632.1985.tb11856.x. [DOI] [PubMed] [Google Scholar]
- 16.Tall AR, Yvan-Charvet L, Terasaka N, Pagler T, Wang N. HDL, ABC transporters, and cholesterol efflux: implications for the treatment of atherosclerosis. Cell Metab. 2008;7:365–375. doi: 10.1016/j.cmet.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Hung KT, Berisha SZ, Ritchey BM, Santore J, Smith JD. Red blood cells play a role in reverse cholesterol transport. Arterioscler Thromb Vasc Biol. 2012;32:1460–1465. doi: 10.1161/ATVBAHA.112.248971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Vries R, Groen AK, Dullaart RP. Cholesterol efflux capacity and atherosclerosis. N Engl J Med. 2011;364:1473–1474. doi: 10.1056/NEJMc1101853. author reply 1474. [DOI] [PubMed] [Google Scholar]
- 19.Chirinos JA, Zambrano JP, Chakko S, Schob A, Goldberg RB, Perez G, Mendez AJ. Ability of serum to decrease cellular acylCoA:cholesterol acyl transferase activity predicts cardiovascular outcomes. Circulation. 2005;112:2446–2453. doi: 10.1161/CIRCULATIONAHA.104.521815. [DOI] [PubMed] [Google Scholar]
- 20.de Vries R, Groen AK, Perton FG, Dallinga-Thie GM, van Wijland MJ, Dikkeschei LD, Wolffenbuttel BH, van Tol A, Dullaart RP. Increased cholesterol efflux from cultured fibroblasts to plasma from hypertriglyc-eridemic type 2 diabetic patients: roles of pre beta-HDL, phospholipid transfer protein and cholesterol esterification. Atherosclerosis. 2008;196:733–741. doi: 10.1016/j.atherosclerosis.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 21.Nestel P, Hoang A, Sviridov D, Straznicky N. Cholesterol efflux from mac-rophages is influenced differentially by plasmas from overweight insulin-sensitive and -resistant subjects. Int J Obes (Lond) 2012;36:407–413. doi: 10.1038/ijo.2011.170. [DOI] [PubMed] [Google Scholar]
- 22.Brennan ML, Reddy A, Tang WH, Wu Y, Brennan DM, Hsu A, Mann SA, Hammer PL, Hazen SL. Comprehensive peroxidase-based hematologic profiling for the prediction of 1-year myocardial infarction and death. Circulation. 2010;122:70–79. doi: 10.1161/CIRCULATIONAHA.109.881581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Z, Nicholls SJ, Rodriguez ER, Kummu O, Hörkkö S, Barnard J, Reynolds WF, Topol EJ, DiDonato JA, Hazen SL. Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nat Med. 2007;13:1176–1184. doi: 10.1038/nm1637. [DOI] [PubMed] [Google Scholar]
- 24.Wang Z, Tang WH, Cho L, Brennan DM, Hazen SL. Targeted metabolo-mic evaluation of arginine methylation and cardiovascular risks: potential mechanisms beyond nitric oxide synthase inhibition. Arterioscler Thromb Vasc Biol. 2009;29:1383–1391. doi: 10.1161/ATVBAHA.109.185645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang WH, Wang Z, Cho L, Brennan DM, Hazen SL. Diminished global arginine bioavailability and increased arginine catabolism as metabolic profile of increased cardiovascular risk. J Am Coll Cardiol. 2009;53:2061–2067. doi: 10.1016/j.jacc.2009.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphati-dylcholine promotes cardiovascular disease. Nature. 2011;472:57–63. doi: 10.1038/nature09922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asztalos BF, Cupples LA, Demissie S, Horvath KV, Cox CE, Batista MC, Schaefer EJ. High-density lipoprotein subpopulation profile and coronary heart disease prevalence in male participants of the Framingham Offspring Study. Arterioscler Thromb Vasc Biol. 2004;24:2181–2187. doi: 10.1161/01.ATV.0000146325.93749.a8. [DOI] [PubMed] [Google Scholar]
- 28.Mulya A, Lee JY, Gebre AK, Thomas MJ, Colvin PL, Parks JS. Minimal lipidation of pre-beta HDL by ABCA1 results in reduced ability to interact with ABCA1. Arterioscler Thromb Vasc Biol. 2007;27:1828–1836. doi: 10.1161/ATVBAHA.107.142455. [DOI] [PubMed] [Google Scholar]
- 29.Favari E, Lee M, Calabresi L, Franceschini G, Zimetti F, Bernini F, Kovanen PT. Depletion of pre-beta-high density lipoprotein by human chymase impairs ATP-binding cassette transporter A1- but not scavenger receptor class B type I-mediated lipid efflux to high density lipoprotein. J Biol Chem. 2004;279:9930–9936. doi: 10.1074/jbc.M312476200. [DOI] [PubMed] [Google Scholar]
- 30.Kane JP, Malloy MJ. Prebeta-1 HDL and coronary heart disease. Curr Opin Lipidol. 2012;23:367–371. doi: 10.1097/MOL.0b013e328353eef1. [DOI] [PubMed] [Google Scholar]
- 31.Guey LT, Pullinger CR, Ishida BY, O’Connor PM, Zellner C, Francone OL, Laramie JM, Naya-Vigne JM, Siradze KA, Deedwania P, Redberg RF, Frost PH, Seymour AB, Kane JP, Malloy MJ. Relation of increased prebeta-1 high-density lipoprotein levels to risk of coronary heart disease. Am J Cardiol. 2011;108:360–366. doi: 10.1016/j.amjcard.2011.03.054. [DOI] [PubMed] [Google Scholar]
- 32.de Vries R, Perton FG, van Tol A, Dullaart RP. Carotid intima media thickness is related positively to plasma pre β-high density lipoproteins in non-diabetic subjects. Clin Chim Acta. 2012;413:473–477. doi: 10.1016/j.cca.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Zheng L, Settle M, Brubaker G, Schmitt D, Hazen SL, Smith JD, Kinter M. Localization of nitration and chlorination sites on apolipoprotein A–I catalyzed by myeloperoxidase in human atheroma and associated oxida-tive impairment in ABCA1-dependent cholesterol efflux from macro-phages. J Biol Chem. 2005;280:38–47. doi: 10.1074/jbc.M407019200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.