Abstract
Background
African Americans are disproportionately affected by cardiovascular disease and cancer. Health promotion interventions hold promise for reducing health disparities.
Purpose
Promoting Health Among Teens (PHAT) is a brief, culturally tailored health education intervention to decrease cardiovascular disease and cancer risk for African Americans. This study evaluated the effects of PHAT for African American adolescents ages 14 to 17 in four eastern cities in the USA.
Methods
A randomized controlled design (N = 1,654) was used to determine differences in health knowledge, diet, physical activity, and substance use behaviors between PHAT participants and a sexual health promotion control group. Data were collected at baseline, three, six, and twelve months post intervention. Growth curve modeling was used to detect differences in health knowledge, dietary behaviors, physical activity, and substance use between PHAT and control group participants.
Results
PHAT participants had significantly greater knowledge gains but modest behavior changes compared to control group participants.
Discussion
PHAT is a promising intervention to increase knowledge and address selected health behaviors in African American youth.
Translation to Health Education Practice
Future attempts to execute PHAT should continue its emphasis on knowledge building while increasing intervention dosage and modifying length of time for intervention sessions.
BACKGROUND
African Americans are disproportionately affected by chronic diseases and unfavorable health conditions. Mortality and morbidity rates are significantly higher among this group than in Non-Hispanic Whites.1 In particular, African Americans have higher rates of cardiovascular disease and cancer than Whites.1 The age-adjusted death rate for heart disease among African Americans is approximately 271 per 100,000 compared to 207 per 100,000 for Non-Hispanic Whites.1 Age-adjusted incidence rates for all cancers is 470 per 100,000 for African Americans compared with 455 per 100,000 for Whites. 1
Poor dietary behaviors, lack of physical activity, increased alcohol consumption, tobacco use, and illicit drug use increases risks for cardiovascular disease and cancer.2-5 Research further suggests that dietary behaviors, physical activity, alcohol, tobacco, and drug use behaviors are heavily influenced during the developmental period of adolescence.6,7
Although cardiovascular disease and cancer rates in African American adolescent populations are lower than rates of African American adults, the behaviors and risk factors that contribute to health disparities are evident at a young age.8-11 African American youth are more likely to be obese, have type II diabetes, consume dietary fat, and engage in less physical activity than White youth.8-11 African Americans have significant health needs, yet general demonstrated health knowledge in this group warrants improvement.12-14 In order for African Americans to develop healthy behaviors in the present and realize health benefits throughout the life-course, strategies to reduce cardiovascular disease should include efforts to improve health knowledge, attitudes and behavior among adolescent populations.
Targeting adolescents for knowledge and behavior change is critical because they are not only cognitively and physically developing, but they are also developing decision-making abilities that directly impact their health. Adopting beneficial health habits during this formative period may translate into maintenance of better health behaviors and favorable health status in the future. Additionally, efforts to dissuade adolescents from harmful health behaviors during this period (i.e. substance abuse, lack of physical activity and poor dietary behaviors) have potential for preventing uptake of these behaviors in the future. Therefore, public health professionals who want to establish and maintain healthy behaviors in populations of interest may benefit from promoting healthy lifestyles during adolescence.
There have been a variety of interventions in the past twenty years to increase physical activity, improve dietary patterns, and reduce alcohol, tobacco and other drug use among adolescents,15-32 however early research on behavioral modification has often focused on a singular strategy of increasing knowledge.33 Although increased knowledge is not sufficient for behavior change, its importance cannot be understated. Individuals with higher levels of health knowledge may perform healthier behaviors at greater frequency than individuals who are less informed.34,35 In a school-based intervention, Reynolds and associates34 found that knowledge mediated behavior change and accounted for approximately 10% of the intervention effects in a program to increase consumption of fruits and vegetables among 4th graders. Kenkel's analysis of the relationship between schooling, health knowledge, and health behavior using the National Health Interview Survey found that increases in physical activity knowledge were associated with physical activity increases in general.35 However, meta-analysis of youth and adult physical activity programs suggests that health exercise knowledge inconsistently predicts spontaneous physical activity, and when it does, it does not encourage adherence to physical activity programs.36 Furthermore, findings regarding knowledge and substance use are less encouraging.35,37-42
Comprehensive school-based approaches addressing chronic disease prevention that integrate nutrition, physical activity, and substance abuse have had encouraging but mixed results over the past two decades.16,18-23,25-27 Despite considerable cardiovascular and cancer disease risk, most of the school-based studies did not address African American adolescent populations specifically.16,21,24,28-31 Of the studies reviewed, very few had study populations wherein the majority of participants were racial/ethnic minorities.16,21,24,28-31 Few addressed behavioral cardiovascular disease and cancer risk factors (dietary behaviors, physical activity, and substance use) simultaneously.20 Also, the internal validity of many of the school-based studies was threatened by attrition rates that exceeded 10%. Finally, these interventions have typically been time extensive, labor-intensive, and cost expensive. An alternative, approach is implementing brief, community-based programming to reduce cardiovascular disease and cancer risk. However, to date, this approach has yet to be sufficiently utilized and researched.
Even if community-based programs were designed that addressed these challenges, they must still be effective for improving health knowledge and behavior for the target audience. A promising strategy to enhance intervention effectiveness is using culturally-tailored curricula to increase health knowledge and improve health behavior. For African Americans in particular, this approach should invoke positive cultural characteristics that reflect the African American experience as well as address specific challenges to optimal health for this population.43 One such health behavior intervention, Promoting Health Among Teens (PHAT)44-47 is designed to improve health behavior among African American adolescents. However, the effectiveness of this intervention to improve health behavior has yet to be explored.
PURPOSE
The rationale for this study was to evaluate the effectiveness of the PHAT curriculum on dietary behaviors, physical activity, and substance use knowledge and behaviors among African American adolescents aged 14 to 17 in four mid-sized cities in the USA. Lack of physical activity, poor dietary behaviors and substance use have been associated with premature cardiovascular disease and cancer.2-5,8-11 An overview of the PHAT curriculum modules, goals and strategies is presented in Table 1.
Table 1.
PHAT Curriculum Overview
| Goals | Strategies/Methods | |
|---|---|---|
|
Module 1 Getting to know you and steps to making your dreams come true |
• Provide participants with an overview of the program. • Increase participant's personal investment in the program • Introduce group members to each other • Establish group rules • Build group cohesion, comfort, and feelings of safety and trust • Increase participants’ confidence about making proud and responsible decisions to protect themselves and their community from various health problems associated with cancer and cardiovascular disease |
• Mini-lecture • Group discussion • Goals and Dreams Timeline • Brainstorming • Sharing exercise |
|
Module 2 Health assessment and health habits |
• Help participants begin to identify their own health behaviors and health risks and how they can lead to various future health problems for cancer and cardiovascular disease • Have participants identify and describe the importance of focusing on their health behaviors and being responsible for their health and disease prevention |
• Group discussion • Health risk assessment survey • Brainstorming |
|
Module 3 You are what you eat: healthy meals |
• To help participants begin to assess their nutritional habits and develop better nutritional behaviors for cancer prevention • To help participants learn information about nutrition and how it relates to their cardiovascular health |
• Group discussion • Dietary intake assessment • Mini-lecture • Meal construction |
|
Module 4 You are what you do: Nutrition, physical activity, and your health |
• Increase participants’ knowledge about exercise and how it relates to their cardiovascular health and cancer prevention • Help participants assess their physical activity behaviors and develop improved PA behaviors themselves |
• Worksheet • Games • Video • Brainstorming • Group discussion • Roleplaying • Sharing exercise |
|
Module 5 You are what you do: Smoking behavior |
• Help participants analyze the impact of smoking cigarettes on their health, especially how it can lead to lung cancer • Help participants synthesize the strategies to say no to smoking cigarettes |
• Sharing exercise • Exercises • DVD viewing • Smoking IQ exercise survey |
|
Module 6 Breast and testicular examination: Early detection and prevention |
• Help participants apply information about breast and testicular cancer. • Help participants apply strategies for prevention and early detection of breast and testicular cancer |
• Group discussion • Video viewing • Breast self-exam demonstration • Testicular self-exam demonstration |
|
Module 7 You are what you do: Substance abuse and alcohol use behaviors |
• Help participants begin to identify and describe the impact of alcohol on cardiovascular health and cancer prevention • Help participants begin to identify and describe the effects of other substance abuse (marijuana, cocaine, et al) and their impact on overall health |
• Brainstroming • Group discussion • Game |
|
Module 8 Understanding yourself: Puberty and hygiene |
• Help the participants identify and describe their hygiene behaviors, their bodies, and their health status | • Group discussion • Video viewing • Health basketball game • Sharing exercise |
METHODS
Study Design
This study was a multisite adolescent cardiovascular and cancer risk reduction intervention conducted in Macon, GA, Providence, RI, Syracuse, NY, and Columbia, SC. The study used a repeated measures, randomized-control research design to compare the effects of an experimental and a control condition in each city.48 Cities were population and regionally balanced and matched on characteristics related to adolescent risk behaviors for urban African American adolescents in mid-sized cities. Pretest and posttest data were collected at baseline, three, six, and twelve month intervals. Data were collected from over 1,600 African American participants between the ages of 14-17. Participants were recruited in cohorts of approximately 25 youth per month and randomized into one of two conditions; the aforementioned PHAT program, or Focus on Youth (FOY) - a sexual risk reduction HIV/STI-prevention intervention. Randomization was based upon a complete randomization scheme and utilized computational random number tables. Identification numbers of possible participants were randomized into experimental or control conditions prior to workshop participation. Each workshop consisted of approximately 12-13 adolescents for each experimental condition (approximately 26 people for each cohort). The two intervention conditions were similar in frequency (number of sessions; two Saturday's back-to-back), length (duration of sessions-16 hours), and structure (level of active learning activities). There were sixteen cohorts in Columbia, Macon and Syracuse, and twenty in Providence. New cohorts were included each month for a one year and three month time period.
Participants
At least 400 African American adolescents between the ages 14-17 were recruited in each city for a total of 1,654 participants. Several strategies were used to recruit program participants including hiring recruitment specialists, partnering with community based organizations, street outreach, referrals, and respondent driven sampling.
Data Collection
After acquiring parental consent and youth assent, participants completed a baseline observation questionnaire using an Audio Computer Assisted Self-Interview (ACASI) on a laptop computer with (headphones for audio and screen for visual) questions that gathered data on participant's demographic characteristics and intervention-related knowledge and behavior. ACASI procedures have demonstrated effectiveness in collecting robust and accurate data of a sensitive and private nature.49,50 ACASI also demonstrates effectiveness in limiting social desirability of participant responses.36 Finally, the auditory component of the instrument that recites the question and response options helps reduce literacy-related challenges.
PHAT Program-Curriculum Description
PHAT is a culturally tailored intervention for African American adolescents, focusing on three dimensions of health behavior (dietary behavior, physical activity, and substance use) for premature cancer and cardiovascular disease prevention. The intervention used various interactive learning activities to increase health knowledge, develop health behavior skills, change attitudes, increase self-efficacy, and explore beliefs regarding personal health behaviors. PHAT has been used as an attention control condition for research projects focusing on sexual risk behavior reduction.44-47 However, the effectiveness of this intervention to improve health behavior has yet to be explored.
PHAT utilized cultural pride, goal setting, and instruction in dietary behaviors, physical activity, nutrition cognition, proper sleeping habits, and substance abuse.44-47 PHAT is designed to increase healthy behaviors of adolescents through the following: knowledge building, reexamination of beliefs regarding risk and consequences, development of skills to delineate and execute behaviors that reduce health risk, increasing self-efficacy to engage in health-beneficial behavior, and increasing motivation to implement healthy behaviors.44-47 PHAT was conducted using group facilitation, role-playing, games, and classroom multimedia messages. See Table 1 for more details regarding PHAT topics, goals, and strategies/activities.
Intervention Theory Base
This intervention was based on Social Cognitive Theory (SCT).51,52 The PHAT curriculum was designed to modify intrapersonal attributes that affect health behavior such as knowledge, self-efficacy, and perceived susceptibility. Furthermore, the program was designed to modify expectancies regarding health behaviors and subsequent health outcomes. It also promoted self-efficacy to perform healthy dietary, physical activity, and drug use behaviors. In particular, activities in this intervention were designed to increase confidence to conduct healthy behaviors and overcome barriers that prevent their execution. The program was also designed to raise awareness concerning how behaviors affect the community as well as how the community influences behaviors and personal beliefs. Finally, PHAT was designed to increase skills to execute behaviors that prevent cardiovascular disease and cancer.44-47
The PHAT program was implemented on two consecutive Saturdays on a monthly basis. Sessions were co-facilitated by trained interventionists at each site. Fidelity to the intervention protocol was assessed on a regular schedule (implementation of the curriculum was evaluated for at least 65% of sessions). Evaluation of curriculum fidelity suggests that the curriculum was correctly implemented at 95% of the sessions. At least half of the facilitators were African American to promote racial concordance.
Measures
The ACASI assessed dimensions of health and health related behavior. The variables of interest for this study were scores on general health knowledge and dietary, physical activity, and substance use behaviors.
Demographics
Several demographic variables were assessed to obtain a description of the sample. Participants were asked to provide their age, sex, ethnicity (Hispanic or Latino), racial background (African-American/Black, White/Caucasian, Asian or Pacific Islander, American Indian or Alaska Native, Mixed or Multiracial, Other), self-described racial identity, and eligibility for free or reduced price school lunch (an indicator of socioeconomic status). Demographic information was acquired during baseline assessments only.
Cardiovascular and Cancer Health Knowledge Instrumentation
Health knowledge was assessed using the Jemmott et al. 18-item General Health Knowledge scale.44-48 This scale assesses knowledge pertaining to alcohol, tobacco, marijuana, and cocaine usage, various types of cancers, cardiovascular disease and prevention methods, dietary behaviors, and physical activity behaviors. Response options for this measure are “Mostly True”, “Mostly False”, and “Don't Know.” Health knowledge was collected at all measurement intervals. This scale demonstrated an acceptable Cronbach alpha score of .76 and a Kuder-Richardson-20 score of .72. All “do not know” and “no” responses were coded as wrong answers. In turn, the score computed was the number of correct responses. An answer key was created and mean scores for both experimental conditions by sex were generated based on the number of correct answers.
Dietary Behaviors
Dietary behaviors were assessed using a 12-item index taken from the Youth Risk Behavioral Survey.53 This questionnaire assessed various behaviors including past week fruit consumption, past week vegetable consumption, past month vegetable consumption and past month fruit consumption. Past week fruit and vegetable consumption questions assessed number of days in the past week that persons consumed these food items. Response options for past month fruit and vegetable consumption utilized six-point Likert scale response options ranging from 1 (not engaging in a behavior at all in the past month) to 6 (engaging in a behavior 4 or more times a day).53
Physical Activity Behaviors
Physical activity behaviors were assessed using a three item questionnaire taken from the YRBS.53 The questionnaire assessed past week vigorous physical activity, past week moderate physical activity, and past week physical activity to strengthen or tone muscles.53 Response options ranged from 0 (no days) to 7 (everyday) for physical activity items.53
Substance Use Variables
Tobacco Use
Lifetime cigarette usage was assessed using a dichotomous measure for ever smoking.53 Past month cigarette usage was measured with a continuous item assessing the number of days that the participant smoked in the past 30 days.53
Alcohol Use
Lifetime alcohol use was assessed with a Likert scale (response options ranged from 1 (zero days of alcohol use) to 7 (100 or more days of alcohol use).53 Frequency of alcohol use was assessed with a continuous item asking the number of days the participant has consumed alcohol in the past month.53
Marijuana Use
The use of Marijuana was assessed using a dichotomous (yes/no) measure to detect lifetime marijuana usage and a continuous measure to determine frequency of use in the past 30 days.53
Data Analysis
Descriptive statistics at baseline were used to determine gender, age, grade, and eligibility for a free or reduced price lunch. Frequencies and percentages were ascertained to create a demographic description of the sample. Subsequent hierarchical linear growth curve modeling was used to determine differences between the experimental and control conditions.
Hierarchical Linear Growth Curve Modeling (HLM)
Hierarchical Linear Growth Curve Modeling analysis was used to detect differences in general health knowledge, dietary behavior, physical activity, and substance use between the experimental and control groups. This HLM procedure was also used to determine the significance of general health knowledge as a covariate in predicting health behavior.
Hierarchical Linear Growth Curve Modeling treats multiple observations with nesting, thereby allowing variation in the number of observations for each person as well as variation in spacing for data collection. This procedure also allowed participants to submit data at multiple time points without violating assumptions of independence.54 A two level hierarchical model allowed researchers to determine participants’ development with an individual growth trajectory. The trajectory is influenced by a variety of measurable individual characteristics (i.e., gender, time, and experimental condition). The parameters (slope and intercept) plus error of the participants’ observed development (Level 1) were the outcome variables. These parameters vary as a function of the aforementioned measurable individual characteristics (Level 2). We used this HLM procedure to assess differences in general health knowledge between the experimental and conditions while controlling for city.
A Proc Mix procedure was used for all analysis of ordinal and continuous outcomes and a Proc Glimmix procedure was used to detect growth curve differences for binary measures. All data were analyzed using Statistical Analysis Software (SAS) version 9.1.3.
RESULTS
Description of the Participants
A total of 1,796 participants from the four intervention sites submitted baseline data. Of these, 1,654 attended at least one workshop. Of workshop attendees, 1,542 (93%), 1,512 (91%), and 1,495(90%) participants submitted three, six, and twelve-month data respectively (Table 2). Approximately 60% (n=990) of the sample were females and 40% (n=664) were males (Table 2). Approximately 73% (n=1216) of the sample reported eligibility for a free or reduced price lunch (Table 2). Approximately 35% (n=574) of participants were aged 14 years, 28% (n=466) 15 years, 21% (n=349) 16 years, and 13% (n=220) 17 years (Table 2). Participants were randomized into two conditions with 834 (50.42%) to PHAT and 820 (49.58%) to FOY (Table 2). Ninety-two percent (N = 1522) of the total study sample reported being solely of African descent. Approximately 5% of the sample identified as racially mixed (n = 77), 0.06% (N=1) as American Indian or Alaska Native, 1% (n=19) as Asian or Pacific Islander, 2% (n=32) as other, and 0.19% (n=3) as Non-Hispanic White. Approximately 98% of the sample self-identified as African American despite these ethnic variations.
Table 2.
Demographics - Gender, Age, Grade, and Free/Reduced Price Lunch Variable
| n | Percentage | |
|---|---|---|
| Gender | ||
| Males | 664 | 40.23% |
| Females | 990 | 59.77% |
| Race/Ethnicity | ||
| African descent | 1522 | 92.02% |
| Non-Hispanic White | 3 | 0.18% |
| Hispanic/Latino | 78 | 4.72% |
| American Indian/Alaska Native | 1 | 0.06% |
| Asian/Pacific Island | 19 | 1.15% |
| Mixed | 77 | 4.66% |
| Other | 32 | 1.93% |
| Age | ||
| 12 | 1 | 0.06% |
| 13 | 41 | 2.47% |
| 14 | 574 | 34.70% |
| 15 | 466 | 28.12% |
| 16 | 349 | 21.24% |
| 17 | 220 | 13.28% |
| 18 | 2 | 0.12% |
| Grade | ||
| Grade 7 | 54 | 3.26% |
| Grade 8 | 247 | 14.90% |
| Grade 9 | 572 | 34.50% |
| Grade 10 | 429 | 25.87% |
| Grade 11 | 233 | 14.05% |
| Grade 12 | 96 | 5.79% |
| Ungraded/Other Grade | 13 | 0.78% |
| Not in School | 10 | 0.60% |
| Free or Reduced Lunch | ||
| Yes | 1216 | 73.34% |
| No | 260 | 15.68% |
| Don't Know | 168 | 10.13% |
| Experimental Status | ||
| PHAT | 834 | 50.42% |
| FOY | 820 | 49.58% |
HLM Growth Curve Analysis Results for General Health Knowledge
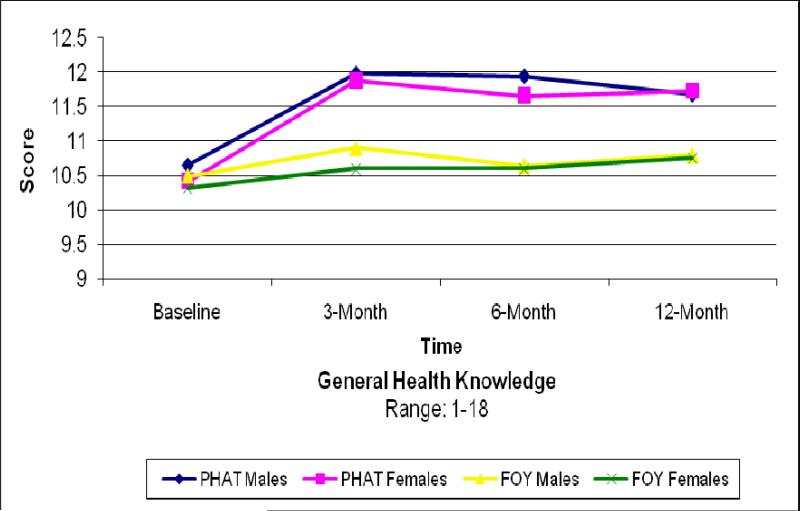
Table 3 displays the mean pretest and posttest knowledge scores for males and females in both experimental conditions. Separate analysis of variance suggests that there were no significant differences between experimental and control groups in knowledge scores at baseline. The intercept score indicates that the average score for general health knowledge, controlling for the personal level factors in the model was 11.09 (Table 4). Scores for knowledge increased at three-months for PHAT participants and remained higher than scores for FOY participants at the six and twelve month observation points (Figure 1).
Table 3.
Mean Scores and Standard Deviations for General Health Knowledge by Group, Gender, and Time
| Group | BASELINE | 3-MONTH | 6-MONTH | 12-MONTH | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | S.D. | N | Mean | S.D. | N | Mean | S.D. | N | Mean | S.D. | |
| PHAT | ||||||||||||
| Male | 338 | 10.65 | 2.66 | 309 | 11.98 | 3.04 | 303 | 11.94 | 3.22 | 299 | 11.68 | 3.27 |
| Female | 496 | 10.42 | 2.46 | 464 | 11.88 | 2.46 | 452 | 11.66 | 2.90 | 453 | 11.73 | 2.97 |
| Total | 834 | 10.51 | 2.54 | 773 | 11.92 | 2.76 | 755 | 11.77 | 3.03 | 752 | 11.71 | 3.09 |
| FOY | ||||||||||||
| Male | 326 | 10.49 | 2.67 | 303 | 10.90 | 2.99 | 297 | 10.64 | 3.17 | 282 | 10.80 | 3.23 |
| Female | 494 | 10.32 | 2.39 | 466 | 10.60 | 2.71 | 460 | 10.60 | 3.01 | 461 | 10.76 | 2.88 |
| Total | 820 | 10.39 | 2.50 | 769 | 10.72 | 2.82 | 757 | 10.62 | 3.07 | 743 | 10.77 | 3.01 |
Table 4.
Estimation of Level 1 Effects of General Health Knowledge and Fixed Effects of Level 2 Factors
| Fixed Effect | Coefficient | SE | T-value | P-value |
|---|---|---|---|---|
| Intercept | 11.09 | 0.23 | 48.73 | <0.0001 |
| Condition | 0.55 | 0.12 | 4.62 | <0.0001 |
| Gender | -0.24 | 0.12 | -2.01 | 0.0449 |
| Time | -0.03 | 0.07 | -0.41 | 0.6832 |
| Condition × Time | 0.16 | 0.04 | 4.27 | <0.0001 |
| Gender × Time | 0.06 | 0.04 | 1.56 | 0.1187 |
Condition: FOY vs PHAT
Gender: Male vs Female
Figure 1.
General Health Knowledge
Group × Gender × Time
As shown on Table 4, PHAT participants had significantly higher knowledge scores than FOY participants (p≤0.0001), and the rate of increase (slope) of condition was significantly higher among PHAT participants than FOY participants (p≤0.0001;Table 4). The initial status for male participants was significantly higher than that of females (p≤0.05), but the slopes for both sexes were comparable (Table 4).
Participants with greater general health knowledge for the centered health knowledge variable had significantly higher intercepts for past week fruit consumption (p≤0.01), past week vegetable consumption (p≤0.0001), past month vegetable consumption (p≤0.0001) past week moderate physical activity (p≤0.0001), past week physical activity to strengthen or tone muscles (p≤0.01) lifetime alcohol use (p≤0.01), and lifetime marijuana use (p≤0.05) (Table 5). Participants with lower general health knowledge had higher intercepts for past month alcohol use (p≤0.01) and past month marijuana use (p≤0.0001). Participants with lower general health knowledge scores had significantly greater slopes for lifetime alcohol use (p≤0.01).
Table 5.
HLM Growth Curve Analysis for Dietary and Physical Activity Behaviors
| Intercept | Condition | Sex | Time | Knowledge | Condition × Time | Sex × Time | Knowledge × Time | |
|---|---|---|---|---|---|---|---|---|
| Past Week Fruit | 3.43† | 0.06 | -0.36† | -0.03** | 0.03** | -0.02 | 0.02 | 0.00 |
| Past Month Fruit | 3.13† | 0.01 | -0.11** | 0.04 | 0.01 | 0.00 | 0.01 | 0.00 |
| Past Week Vegetable | 3.13† | -0.07 | 0.20* | 0.04 | 0.06† | -0.02 | -0.07 | -0.01 |
| Past Month Vegetable | 2.68† | -0.02 | 0.10 | 0.06 | 0.04† | 0.00 | -0.03 | -0.01** |
| Past Week VPA | 6.00† | -0.12 | -1.21† | -0.08 | 0.01 | 0.08* | -0.04 | 0.00 |
| Past Week MPA | 3.79† | -0.11 | -0.26** | 0.11 | 0.06† | 0.06 | -0.08* | -0.01 |
| Past Week S/T | 5.64† | -0.15 | -1.68† | -0.08 | 0.03** | 0.03 | -0.02 | 0.00 |
p≤0.05
p≤0.01
p≤0.0001
Condition: FOY vs PHAT
Gender: Male vs Female
VPA = Vigorous Physical Activity
MPA = Moderate Physical Activity
S/T = Physical Activity to Strengthen or Tone Muscles
HLM Growth Curve Analysis Results for Dietary Behavior
There were no differences in intercepts or slopes of participants in PHAT and FOY for dietary behavior (Table 5). Males had greater past week (p<0.0001) (Table 5) and past month (p≤0.01) fruit consumption than females. Females had greater past week vegetable consumption (p≤0.05). Past week fruit consumption (p<0.01) decreased as time progressed.
HLM Growth Curve Analysis Results for Physical Activity Behavior
The growth curves for moderate physical activity and physical activity to strengthen and tone muscles were not significantly different between PHAT and FOY participants. The level of engagement of vigorous physical activity was not significantly different between experimental conditions; however the rates of increase for participants in PHAT were higher than those in FOY (Table 5). Males demonstrated higher engagement in vigorous physical activity (p<0.0001), moderate physical activity (p<0.01), and physical activity to strengthen or tone muscles (p<0.0001) (Table 5). Males also demonstrated greater rates of increase for moderate physical activity (p<0.05) (Table 5). There were no significant differences in physical activity engagement from baseline until twelve months (Table 5).
HLM Growth Curve Analysis Results for Substance Abuse
There were no significant differences in growth curve results between experimental conditions for all past month substance abuse behavior variables, lifetime alcohol use, and lifetime tobacco use (Table 6). There were significantly higher rates of increase for PHAT participants in lifetime marijuana use (p<0.0001). Engagement in past month tobacco use (p<0.001), past month alcohol use (p<0.0001), lifetime marijuana use (p<0.01) and past month marijuana use (p<0.0001) was higher among males than females. Rates of increase were higher for males for past month tobacco use (p=0.05), and lifetime alcohol use (p<0.01), (Table 6). There were significant increases from baseline to twelve months in lifetime tobacco use (p<0.0001), past month tobacco use (p<0.05), and lifetime marijuana use (p<0.0001; Table 6).
Table 6.
HLM Growth Curve Analysis for Drug Use Behaviors
| Intercept | Condition | Sex | Time | Knowledge | Condition × Time | Sex × Time | Knowledge × Time | |
|---|---|---|---|---|---|---|---|---|
| Past Month Alcohol | 2.31† | 0.07 | -0.67† | 0.02 | -0.07** | 0.03 | -0.11 | -0.01 |
| Lifetime Alcohol | 2.45† | 0.05 | -0.09 | 0.26 | 0.02† | 0.00 | -0.04* | -0.01** |
| Lifetime Tobacco | 0.53† | 0.24 | -0.17 | 0.41† | 0.04 | 0.01 | -0.06 | -0.12 |
| Past Month Tobacco | 3.93† | 0.32 | -1.33** | 0.42† | -0.02 | 0.06 | -0.23* | 0.00 |
| Past Month Marijuana | 9.23† | 0.55 | -3.20† | 0.22 | -0.29† | -0.18 | 0.12 | -0.03 |
| Lifetime Marijuana | 0.17 | 0.01 | -0.62** | 0.40† | 0.06* | 0.56† | -0.08 | -0.03 |
p<0.05
p<0.01
p<0.0001
Condition: FOY vs PHAT
Gender: Male vs Female
DISCUSSION
Growth curve modeling indicated that participants in PHAT had significantly more gains in health knowledge than participants in FOY, however the effects on behavior were modest. Although this program was a brief intervention, participation in PHAT was associated with greater scores for health knowledge for at least one year after implementation. Furthermore, individuals with greater health knowledge demonstrated healthier behaviors.
Improving knowledge is an integral part of Health Education intervention research. Although PHAT participants had knowledge increases, it may differentially impact dietary, physical activity, and substance use behaviors.34-42 Although the PHAT program was brief, it elicited greater scores for health knowledge for at least one year after implementation. Moreover, people with greater knowledge scores demonstrated significantly more positive health behaviors. Results indicate that although behavioral outcomes were modest, improving knowledge is an effective first step in improving behavior if minor modifications to the curriculum are implemented. Continued research on this program and other health promotion interventions should evaluate the effectiveness of knowledge increases on specific health risk behaviors.
Results for the growth curve analysis between participants in PHAT and FOY were not significantly different for dietary behaviors. However, PHAT participants had significantly greater increases in vigorous physical activity. Several school-based studies have observed higher fruit and vegetable intake, lower fat-intake, and greater engagement of physical activity among experimental participants.16,19,20,24-26,28 However, community-based programs have generally been less successful than school-based efforts in facilitating healthy dietary behavior and physical activity initiation and maintenance.28-31 These findings are not surprising given the brevity of length and lower intervention dosages associated with community-based studies. Additionally, the methodology of school-based studies are dissimilar than that of brief, community-based research studies. For example, CATCH and the Minnesota Heart Health Project both modified access and availability of healthy food options for students, however these efforts are beyond the scope of this project.18,20 Taken together, these findings suggest that this study was similar to other community-based studies that produced modest intervention effects with regard to improving dietary behavior but was more effective in improving physical activity.
There were no significant changes for most substance use behaviors in this study. There have been a variety of studies that have observed significant differences in substance abuse among experimental and control participants.16,19,21,23,25,27 In a summary of the “elements of prevention” from meta-analyses, Sloboda55-58 suggests that the components of effective substance use prevention programs for adolescents include: addressing normative adolescent beliefs about the prevalence of substance use by peers; reinforcing perceived negative consequences of substance use for adolescents; providing life skills such as communication, decision-making and resistance opportunities; opportunities to practice these skills around real-life situations; and active engagement of adolescents in the education process. The PHAT curriculum had some of these elements (see Table 1) however the opportunities to practice decision-making and resistance skills were limited with the brief nature of the PHAT intervention.
Unlike these programs however, PHAT was considerably shorter and had less intervention dosage. Given the complexity of modifying drug use behavior among adolescents, higher intervention dosages may be more effective in reducing substance abuse among youth. In addition, caution is noted in two somewhat recent reports59,60 that suggest more limited effect sizes from adolescent substance use prevention interventions from the 1980's and 1990's that may not achieve the same effects for adolescents for the 21st century. In addition, in randomized trials, when comparisons are drawn from control groups, often the widespread availability of prevention programs means that controls may have been exposed to some drug prevention efforts. Thus, the comparisons are not as dramatic (statistically significant) with far smaller differences detected.58-60
A notable finding was that slopes for lifetime marijuana use were greater for PHAT participants. Although this finding was unexpected, it may be partially explained by the recognition that the control condition also addressed substance abuse behaviors within the context of HIV prevention (less dramatic comparisons).58-60 Additionally, meta-analysis suggests that knowledge level is correlated with marijuana use albeit less highly correlated than other predictors (prior drug use, poorer mental health, victimization).42 Further research should explore the effects of community-based programming on substance use for adolescents.
Though the results of this study indicate that PHAT had modest effects in improving dietary, physical activity, and substance abuse behaviors, there are strategies to elicit more favorable behavior change. First, it may be necessary to increase intervention dose for participants. Behavior change may not have been observed because appropriate doses of intervention were not applied to secure appropriate effects. A review of school-based dietary behavior literature suggests that higher dosages of intervention are associated with behavior change.61 Additionally, the PHAT intervention period may have been too brief for: 1) facilitators to develop rapport and gain the trust of participants, and 2) for participants to practice behaviors and develop the level of self-efficacy to effectively execute and sustain them. A longer intervention period may help encourage more favorable PHAT intervention effects.
Alternatively, another promising approach would be to maintain the dosage of the intervention but implement it beyond two Saturdays. The integrity of the program would remain if the content and dosage of the intervention were expanded over a longer period of time using this strategy. This approach shows potential, as the length of intervention may have been insufficient to allow participants time to process newly acquired information and fully execute cognitive and decision-making processes to stimulate behavior change. Spacing the same dose of an intervention over several sessions may allow more opportunities for validation and reinforcement of new beliefs and perceptions as well as granting opportunities to practice, enhance, and refine skills pertaining to improving health behavior.61,62 Research on interventions comparing programs of similar dosage and content but differing lengths found greater effectiveness among programs with longer implementation periods.63-66 These studies also suggest that condensing these programs decrease efficacy and inhibit more positive effects.63-66
Although programmatic efforts to improve dietary behavior among African American adolescents are critical, public health researchers must recognize the structural challenges (i.e. limited access and availability of healthy food options) to implement favorable dietary behaviors. Programs to improve healthy eating behavior may encounter challenges if there is a lack of healthy food available. Therefore, an emphasis on harm reduction strategies (coupled with larger advocacy efforts to promote health equity) may be advantageous in eliciting dietary behavior change among the population of interest. For instance, participants should be encouraged to select the healthiest foods available in the midst of a variety of unfavorable choices. Furthermore, greater benefit may be realized by emphasizing small, incremental changes to dietary behavior instead of large, sweeping modifications. For example, participants can be encouraged to increase water consumption by starting with small increases per day and gradually building to recommended amounts of intake.
Participants in this study may have encountered a variety of challenges in performing physical activity behaviors. For example, participants in both PHAT and FOY may have demonstrated less physical activity owing to a lack of safe areas to exercise, gang activity in local neighborhoods, or distance from gymnasiums or other facilities to exercise. However, there are several modifications that could strengthen execution of the PHAT curriculum. For example, emphasis can be placed on encouraging participants to engage in enjoyable activities (i.e. basketball, dancing, cheerleading, marching band) instead of more traditional physical activity (jogging, bike riding). Also, emphasis can be placed on incremental strategies to improve physical activity.
In order for researchers to observe greater benefit in substance abuse prevention with PHAT, it may be advantageous to expand the content regarding substance abuse as well as continuing its emphasis on the negative physiological, social, familial, and legal consequences of drug use. Additionally, the program should maintain its focus on reducing abuse of the most commonly used drugs among this population (i.e. alcohol, tobacco, and marijuana).
Limitations of this study should be noted. All demographic variables were self reported. However, several measures were performed to improve the quality of responses including use of identification numbers to increase confidentiality and using ACASI assessments to generate psychosocial questionnaire data. Also, there may have been varying levels of experience and effectiveness of the facilitators for this program. Several measures were taken to limit the differences between curriculum interventionists. All facilitators underwent standardized curriculum training. Also, 65% of the intervention sessions were observed and scored for fidelity of implementation. The fidelity of implementation scoring system suggests that 95% of curriculum sessions were correctly implemented. Finally, this study was executed among socioeconomically disadvantaged African American adolescents in four mid-sized cities the eastern United States and the findings may not be generalizable to other racial/ethnic populations, age groups, or geographic locales.
TRANSLATION TO HEALTH EDUCATION PRACTICE
PHAT is a culturally-tailored, brief intervention targeting African American adolescents that demonstrated significant knowledge gains and modest success in improving dietary, physical activity, and drug use behaviors. This study utilized a strong (randomized and controlled) research design that accounted for or evenly distributed most major threats to internal validity. Future attempts to execute the PHAT program and other health promotion programs should continue emphasis on knowledge building as knowledge is necessary for attitude and behavior change and greater knowledge scores are associated with healthier behaviors. The PHAT program may facilitate greater engagement in healthy behaviors for participants if a variety of strategies were taken including increasing the number of contact hours and spreading the workshops across several more days. More research should be conducted among economically disadvantaged African American youth populations to improve cardiovascular health and reduce negative cancer and other disease outcomes.
Acknowledgments
This research was supported by the National Institutes of Health; National Institute of Mental Health, [Grant Number 1-UO1-MH66802].
Contributor Information
Jelani C. Kerr, University of Windsor
Robert F. Valois, University of South Carolina
Naomi B. Farber, University of South Carolina
Peter A. Vanable, Syracuse University
Ralph J. DiClemente, Emory University
Laura Salazar, Georgia State University.
Larry K. Brown, Brown University
Michael P. Carey, Brown University
Daniel Romer, University of Pennsylvania.
Bonita Stanton, Wayne State University.
John B. Jemmott, III, University of Pennsylvania.
Loretta Sweet Jemmott, University of Pennsylvania.
A Melinda Spencer, University of South Carolina.
Lucy Annang, University of South Carolina.
REFERENCES
- 1.National Center for Health Statistics . Health, United States, 2010: With Special Feature on Death and Dying. Centers for Disease Control and Prevention; Hyattsville, MD: 2011. [PubMed] [Google Scholar]
- 2.Blackburn H. Physical activity and coronary heart disease: a brief update and population view. J Cardiac Rehab. 1983;3101(11)(17):1–74. [Google Scholar]
- 3.Haskell W. Cardiovascular benefits and risks of exercise: the scientific evidence. In: Strauss R, editor. Sports Medicine. Saunders; Philadelphia, PA: 1984. pp. 57–75. [Google Scholar]
- 4.US Department of Health and Human Services . The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. US Department of Health and Human Services; Rockville, MD: 2001. [Google Scholar]
- 5.Centers for Disease Control and Prevention . 1998 Surgeon General's Report - Tobacco use among US Racial/Ethnic Minority Groups. US Department of Health and Human Services; Rockville, MD: 1998. [Google Scholar]
- 6.Fardy P, White R, Clarke L, et al. Coronary risk factors and health behaviors in a diverse ethnic and cultural population of adolescents: a gender comparison. J Cardiopulmonary Rehab. 1994;14:52–60. [Google Scholar]
- 7.Srinivasan S, Bao W, Wattigney W, et al. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors; the Bogalusa Heart Study. Metabolism. 1996;45:235–240. doi: 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 8.Befort C, Kaur H, Nollen-Sullivan D, et al. Fruit, vegetable, and fat intake among Non-Hispanic Black and Non-Hispanic White adolescents: associations with home availability and food consumption settings. J Am Diet Assoc. 2006;106(3):367–373. doi: 10.1016/j.jada.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Youth Risk Behavior Surveillance - United States, 2005. MMWR Morb Moral Wkly Rep. 2006;55(SS05):1–108. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Youth Risk Behavior Surveillance-United States, 2007. MMWR Morb Moral Wkly Rep. 2008;57(SS04):1–131. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention . National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2007. U.S. Department of Health and Human Services, Centers for Disease control and Prevention; Atlanta, GA: 2008. [Google Scholar]
- 12.Denniston R. Cancer knowledge, attitudes, and practices among Black Americans. Prog Clin Biol Res. 1981;53:225–237. [PubMed] [Google Scholar]
- 13.Gates G, McDonald M. Comparison of dietary risk factors for cardiovascular disease in African-American and White women. J Am Diet Assoc. 1997;97(12):1394–1400. doi: 10.1016/S0002-8223(97)00338-6. [DOI] [PubMed] [Google Scholar]
- 14.Michielutte R, Diseker R. Racial differences in knowledge of cancer: a pilot study. Soc Sci Med. 1982;16:245–252. doi: 10.1016/0277-9536(82)90335-5. [DOI] [PubMed] [Google Scholar]
- 15.Bayne-Smith M, Fardy P, Azzollini A, et al. Improvements in heart health behaviors and reduction in coronary artery disease risk factors in urban teenaged girls through a school-based intervention: the PATH Program. Am J Public Health. 2004;94(9):1538–1543. doi: 10.2105/ajph.94.9.1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bush P, Zuckerman A, Taggart V, et al. Cardiovascular risk factor prevention in Black school children: the “Know Your Body” evaluation project. Health Educ Behav. 1989:215–227. doi: 10.1177/109019818901600206. Summer. [DOI] [PubMed] [Google Scholar]
- 17.Kelder S, Perry C, Klepp K. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am J Public Health. 1994;84(7):1121–1126. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelder S, Perry C, Lytle L, et al. Community-wide youth nutrition education: long-term outcomes of the Minnesota heart health program. Health Educ Res. 1995;10(2):119–131. doi: 10.1093/her/10.2.119-a. [DOI] [PubMed] [Google Scholar]
- 19.Killen J, Robinson T, Telch M, et al. The Stanford Adolescent Heart Health Program. Health Educ Behav. 1989;16(2):263–283. doi: 10.1177/109019818901600210. [DOI] [PubMed] [Google Scholar]
- 20.Luepker R, Perry C, McKinlay S, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity: The Child and Adolescent Trial for Cardiovascular Health (CATCH). JAMA. 1996;275(10):768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 21.Botvin G, Schinke S, Epstein J, et al. Effectiveness of culturally focused and generic skills training approaches to alcohol and drug use prevention among minority youths. Psychol Addict Behav. 1994;8(2):116–127. [Google Scholar]
- 22.Botvin G, Griffen K, Diaz T, et al. Preventing illicit drug use in adolescents: long-term follow-up data from a randomized control trial of a school population. Addict Behav. 2000;25(5):769–774. doi: 10.1016/s0306-4603(99)00050-7. [DOI] [PubMed] [Google Scholar]
- 23.Dent C, Sussman S, Stacy A. Project towards no drug abuse: generalizability to a general high school sample. Prev Med. 2001;32:514–520. doi: 10.1006/pmed.2001.0834. [DOI] [PubMed] [Google Scholar]
- 24.Holcomb J, Lira J, Kingery P, et al. Evaluation of Jump Into Action: a program to reduce the risk of non-insulin dependent diabetes mellitus in school children on the Texas-Mexico border. J Sch Health. 1998;68(7):282–288. doi: 10.1111/j.1746-1561.1998.tb00584.x. [DOI] [PubMed] [Google Scholar]
- 25.Perry C, Kelder S, Murray D, et al. Communitywide smoking prevention: long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 study. Am J Public Health. 1992;82(9):1210–1216. doi: 10.2105/ajph.82.9.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perry C, Klepp K, Halder A, et al. promoting healthy eating and physical activity patterns among adolescents: a pilot study of Slice of Life. Health Educ Res. 1987;2(2):93–103. [Google Scholar]
- 27.Perry C, Williams C, Komro K, et al. Project Northland: Long-term outcomes of community action to reduce alcohol use. Health Educ Res. 2002;17(1):117–132. doi: 10.1093/her/17.1.117. [DOI] [PubMed] [Google Scholar]
- 28.Resnicow K, Yaroch A, Davis A, et al. GO GIRLS!: Results from a nutrition and physical activity program for low-income, overweight African American adolescent females. Health Educ Behav. 2000;27(5):616–631. doi: 10.1177/109019810002700507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schinke S, Singer B, Cole K, et al. Reducing cancer risk among Native American adolescents. Prev Med. 1996;25:146–155. doi: 10.1006/pmed.1996.0040. [DOI] [PubMed] [Google Scholar]
- 30.Story M, Sherwood N, Himes J, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis. 2003;13:S1–S54. [PubMed] [Google Scholar]
- 31.Wadden T, Stunkard A, Rich L, et al. Obesity in Black adolescents girls: a controlled clinical trial of treatment by diet, behavior modification, and parental support. Pediatrics. 1990;85(3):345–352. [PubMed] [Google Scholar]
- 32.Wardle J, Paramenter K, Waller J. Nutrition knowledge and food intake. Appetite. 2000;34:269–275. doi: 10.1006/appe.1999.0311. [DOI] [PubMed] [Google Scholar]
- 33.Biles F. Why cardiovascular education in the schools - from an educational perspective. Health Education. 1982;13(1):17–18. [PubMed] [Google Scholar]
- 34.Reynolds K, Bishop B, Chou CP, et al. Contrasting mediating variables in two 5-a-day nutrition intervention programs. Prev Med. 2004;39:882–893. doi: 10.1016/j.ypmed.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 35.Kenkel D. Health behavior, health knowledge, and schooling. J Political Econ. 1991;99(2):287–305. [Google Scholar]
- 36.Dishman R, Sallis J, Orenstein D. The determinants of physical activity and exercise. Public Health Rep. 1985;100(2):158–171. [PMC free article] [PubMed] [Google Scholar]
- 37.Goodstat M. Drug education-a turn off? J Drug Educ. 1980;10:89–99. [Google Scholar]
- 38.Goodstat M. School-based drug education in North America: what is wrong? What can be done? J Sch Health. 1986;81(7):278–281. doi: 10.1111/j.1746-1561.1986.tb05751.x. [DOI] [PubMed] [Google Scholar]
- 39.Kinder B, Pape N, Walfish S. Drug and alcohol education programs: a review of outcome studies. Int J Addict. 1980;15:1035–1054. doi: 10.3109/10826088009040077. [DOI] [PubMed] [Google Scholar]
- 40.Schaps E, DiBartolo R, Moskowitz J, et al. A review of 127 drug abuse prevention program evaluations. J Drug Issues. 1981;11(1):17–43. [Google Scholar]
- 41.Bruvold W, Rundall T. A meta-analysis and theoretical review of school-based tobacco and alcohol intervention programs. Psychol Health. 1988;2(1):53–78. [Google Scholar]
- 42.Derzon J, Lipsey M. What good predictors of marijuana use are good for: a synthesis of research. School Psychol Int. 1999;20(1):69–85. [Google Scholar]
- 43.Resnicow K, Braithwaite R, Ahluwalia J, et al. Cultural sensivitity in public health: defined and demystified. Ethn Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- 44.Jemmott J, Jemmott L, Fong G. Reductions in HIV risk-associated sexual behaviors among Black male adolescents: effects of an AIDS prevention intervention. Am J Public Health. 1992;82(3):372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jemmott J, Jemmott L, Fong G. Abstinence and HIV-risk reduction interventions for African American adolescents: a randomized control trial. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 46.Jemmott J, Jemmott L, Fong G, et al. Reducing HIV risk-associated sexual behavior among African American adolescents: testing the generality of intervention effects. J Community Psychol. 1999;27(2):161–187. doi: 10.1007/BF02503158. [DOI] [PubMed] [Google Scholar]
- 47.Jemmott JB, 3rd, Jemmott LS, Fong GT. Efficacy of a theory-based abstinence-only intervention over 24 months: a randomized controlled tiral with young adolescents. Arch Pediatr Adolesc Med. 2010;164(2):154–159. doi: 10.1001/archpediatrics.2009.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shadish W, Cook T, Cambell T. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Houghton Mifflin; Boston, MA, New York, NY: 2002. [Google Scholar]
- 49.Des Jarlais D, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviors for HIV among injecting drug users: a quasi-randomized trial. Lancet. 1999;353:1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 50.Morrison-Beedy D, Carey M, Xin T. Accuracy of audio computer-assisted self-interviewing (ACASI) and self-administered questionnaires for the assessment of sexual behavior. AIDS Behav. 2006;10:541–552. doi: 10.1007/s10461-006-9081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 37:121–147. 982. [Google Scholar]
- 52.Bandura A. Social Foundations of Thought and Action. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 53.Centers for Disease Control and Prevention . Youth Risk Behavior System Survey. US Department of Health and Human Services; Atlanta, GA: 2005. [Google Scholar]
- 54.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Sage Publications; Newbury Park, CA: 2002. [Google Scholar]
- 55.Sloboda Z, David SL. Preventing drug abuse among children and adolescents: a research-based guide. 1997. NIH Publication No. 97-4212(A)
- 56.Sloboda Z, Petras H. A conceptual foundation for prevention. In: Sloboda Z, Petras H, editors. Advances in Prevention Science: Defining Prevention Science. Springer; New York, NY: In Press. [Google Scholar]
- 57.Sloboda Z. School prevention. In: Leukefield CG, editor. Adolescent Substance Abuse. Springer; New York, NY: 2009. pp. 191–212. [Google Scholar]
- 58.Sloboda Z. Background paper “Substance Abuse Prevention: Reviewing the Basic Elements of Prevention Intervention.” United Nations Office on Drugs and Crime. Vienna Interantional Centere; Vienna, Austria: 2012. International Standards on Drug Use Prevention. [Google Scholar]
- 59.Longshore D, Ellickson PL, McCaffrey, et al. School-based drug prevention among at-risk adolescents: effects of ALERT plus. Health Educ Behav. 2007;34:651–668. doi: 10.1177/1090198106294895. [DOI] [PubMed] [Google Scholar]
- 60.St. Pierre TL, Osgood DW, Mincemoyer CC, et al. Results of an independent evaluation of Project ALERT delivered in schools by cooperative extension. Prev Sci. 2005;6:305–317. doi: 10.1007/s11121-005-0015-0. [DOI] [PubMed] [Google Scholar]
- 61.Hoelscher D, Evans A, Parcel G, et al. Designing effective nutrition interventions for adolescents. J Am Diet Assoc. 2002;S102(3):s52–s63. doi: 10.1016/s0002-8223(02)90422-0. [DOI] [PubMed] [Google Scholar]
- 62.Tuckman B. Educational Psychology from Theory to Application. Harcourt Brace Jovanich; Fort Worth, TX: 1992. [Google Scholar]
- 63.Rothman-Borus M, Gwadz M, Fernandez I, et al. Timing of HIV interventions on reductions in sexual risk among adolescents. Am J Community Psychol. 1998;26:73–96. doi: 10.1023/a:1021834224454. [DOI] [PubMed] [Google Scholar]
- 64.Stanton B, Kim N, Galbraith J, Parrot M. Design issues addressed in published evaluations of adolescent HIV-risk reduction interventions: a review. J Adolesc Health. 1996;18:387–396. doi: 10.1016/1054-139X(95)00169-S. [DOI] [PubMed] [Google Scholar]
- 65.Kirby D. Emerging Answers: Research Findings on Programs to Reduce Teen Pregnancy. National Campaign to Prevent Teen Pregnancy; Washington, DC: 2001. [Google Scholar]
- 66.Robin L, Dittus P, Whitaker D, et al. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: a decade in review. J Adolesc Health. 2004;34:3–26. doi: 10.1016/s1054-139x(03)00244-1. [DOI] [PubMed] [Google Scholar]