Abstract
Objectives
Despite large public investments in condom distribution programs for HIV prevention among men who have sex with men (MSM), few evaluations have documented the reach of condom distribution programs or whether free condoms distributed to MSM are actually used. Among MSM recruited from social networking and dating websites, we examined the proportion who reported acquiring and using free condoms, and associations between select characteristics and reported acquisition and use of free condoms.
Methods
We used baseline data from a prospective, online cohort of U.S. MSM. Participants reported acquiring free condoms in the 12 months before interview and, for those who acquired condoms and had anal intercourse, use of the free condoms they acquired. We used multivariable log binomial regression models to describe factors associated with self-reported acquisition and use of condoms.
Results
Of the 2,893 men in the analytic sample, 1,701 (59%) reported acquiring free condoms in the past year. Acquisition of free condoms was higher for men who were younger, more educated, recently tested for HIV, and had higher numbers of sex partners. Seventy-three percent of men who acquired free condoms reported using them; use was higher for men who were black, had been recently tested for HIV, and reported greater numbers of sex partners.
Conclusions
Most MSM in our online sample reported receiving free condoms, and most who acquired free condoms reported using them. These data suggest that condom distribution programs have reasonable reach and utility as part of a comprehensive package of HIV prevention interventions for U.S. MSM.
Men who have sex with men (MSM) are the group at highest risk for HIV infection in the U.S. In 2010, 61% of all new human immunodeficiency virus (HIV) diagnoses in the U.S. were among MSM,1 who only account for an estimated 2% of the U.S. population.2 Further, MSM have been the only risk group in which HIV incidence has been increasing since the early 1990s.3
Condoms have been identified as a method to prevent sexual transmission of HIV since the early phases of the HIV epidemic in the U.S. In 1986, the Centers for Disease Control and Prevention issued a recommendation for the use of condoms to prevent sexual transmission of HIV, even prior to definitive findings of the effectiveness of condoms to prevent HIV transmission had been released.4 Since that time, condoms have been recognized as the most effective method to prevent the sexual transmission of HIV, aside from abstinence,5–8 and condom promotion remains a mainstay of HIV prevention strategies, including the National HIV/Acquired Immunodeficiency Syndrome (AIDS) Strategy for the United States.9
Although the effectiveness of condoms to prevent HIV transmission is well recognized, studies have noted that barriers to obtaining condoms, such as cost10 and embarrassment associated with purchasing condoms,11 may prevent condom use. Given the demonstrated benefits of condoms coupled with the fact that barriers to purchasing condoms may prevent condom acquisition, many health departments, clinics, community-based organizations, and AIDS service organizations have implemented free condom distribution programs to ensure those individuals most at risk for HIV infection, such as MSM, have access to condoms.12–14 Regardless of the size of the program, distributing free condoms requires the dedication of significant resources. For example, Louisiana's statewide condom availability program, which distributed more than 33 million condoms from 1994 to 1996, cost an estimated $3 million during the three-year period.15 The Free Condom Initiative by the New York City Department of Health and Mental Hygiene (NYC DOHMH) distributed 17.3 million condoms in 2006 at a cost of $1.59 million.13
Because of the considerable financial and organizational commitment involved in distributing free condoms, understanding the impact of free condom distribution is essential. Although it is important to define key indicators, such as the number of condoms distributed,16 to measure a program's success, it is critical to determine the type of individuals receiving free condoms to ensure that those most at risk for HIV infection both have access to and make use of free condoms. To date, few studies have examined factors associated with acquisition and use of free condoms among MSM; those studies that have been conducted have been limited in geographic region to either one state17 or to urban areas.18 To address these research gaps, we examined characteristics associated with acquisition and use of free condoms using data from a national online HIV prevention survey.
METHODS
Recruitment and study design
MSM were recruited from August to December 2010 through selective placement of banner advertisements on social networking and Internet dating websites, including Facebook, MySpace, Black Gay Chat, and Adam4Adam. Eligible participants were male, ≥18 years of age, and reported sex with a male in the past 12 months. After providing informed consent, men completed a 60-minute survey that included questions on condom acquisition and use, demographics, sexual risk behaviors, sexual partner history, and HIV testing history.
Measures and statistical analysis
We analyzed data from participants who completed the condom receipt and use questions, which appeared in the final eighth of the survey. To examine the frequency of acquisition and use of free condoms by our study population, we asked respondents, “In the past 12 months, have you received free condoms?” Participants who reported receiving free condoms were asked, “Have you used any of the free condoms you received?” To examine the characteristics associated with the use of free condoms, we limited the analysis to include only those participants who indicated that they had anal sex with a male sex partner in the past 12 months.
Because the condom questions appeared near the end of the survey, we also compared the characteristics of participants who started but did not complete the survey with those who completed the survey to assess any potential selection bias among the study population included in the analysis.
We identified two variables as main effects of interest for acquisition and use of free condoms—race/ethnicity and age. To facilitate comparisons between our study results and national data,19 men <25 years of age were categorized into two age groups: 18–19 and 20–24 years of age. Men aged ࣙ25 years were categorized in five-year age groups. Potential confounders were identified based on a literature review and expert opinion and included: education level, yearly income, sexual identity, having received an HIV test, HIV status, gender of sex partners (i.e., only men or men and women), number of male sex partners, and having used the Internet to meet a sex partner (all behaviors in the 12 months before interview). Having had unprotected anal intercourse (UAI) with a male sex partner in the past 12 months was also examined as an independent factor of interest for the analysis of free condom acquisition, and having had ࣙ1 main male sex partners in the past 12 months was included as an independent variable of interest in the analysis of free condom usage.
We used log binomial regression models to examine bivariate and multivariate associations between the independent factors and the two outcomes of interest—having acquired free condoms in the past 12 months and use of free condoms acquired—and reported them as adjusted prevalence ratios with 95% confidence intervals. All variables, regardless of the results from the bivariate analysis, were considered in the multivariable models. Backward elimination was used to determine which variables were significantly associated (p<0.05) with the outcome variables of interest. Because race/ethnicity and age were the primary independent factors of interest in the analysis, these variables were retained in each model during backward elimination, regardless of their significance. Other independent variables that remained in the model at the conclusion of backward elimination were considered for two-way interactions. Using retained regressors from the reduced model, all two-way interactions were considered together with a p-value adjusted for simultaneous assessment to result in an aggregate alpha of 0.05 for evaluation of interaction. All data analyses were performed using SAS® version 9.2.20
RESULTS
Of the 9,980 participants who were eligible to participate in the survey, 8,503 (85%) provided informed consent and, of those, 6,104 (72%) began the survey (data not shown). Characteristics of participants by survey completion status are provided in Table 1. Forty-seven percent of participants (n=2,847/6,104) completed the baseline survey in its entirety. Among all participants, slightly less than half were white and approximately one-quarter were black. More than 40% of participants were <25 years of age and approximately one-third were college-educated. Participants were predominantly gay-identified and HIV-negative, and the vast majority reported having sex with only male sex partners in the past 12 months.
Table 1.
Characteristics of MSM enrolled in an online HIV prevention study (n=6,104), by survey completion status: U.S., 2010
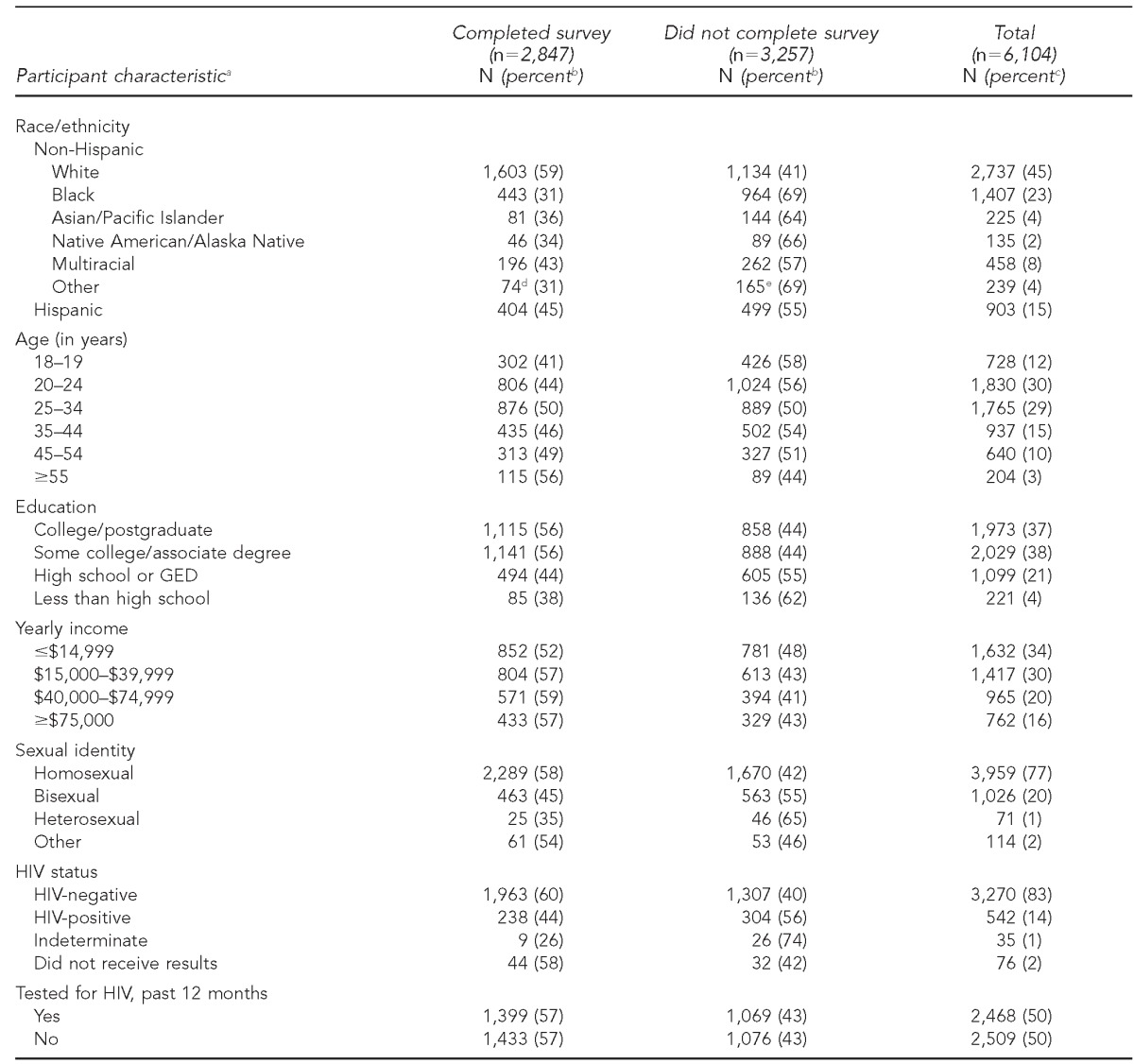
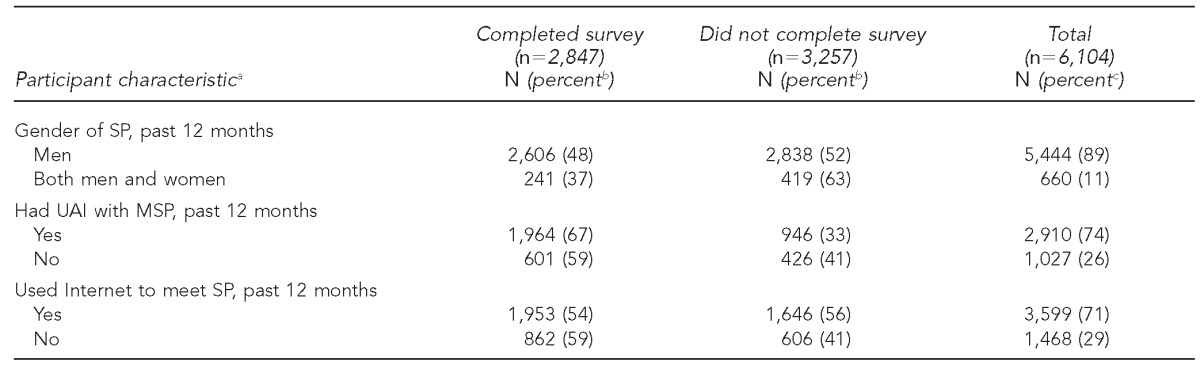
aTotals for most variables do not equal total number of respondents due to missing values.
bRepresents percentage of participants who completed or did not complete survey, among those with that characteristic (row percent)
cRepresents percentage of total participants (column percent)
dIncludes “other” (n=50) and “prefer not to answer” (n=24)
eIncludes “other” (n=103) and “prefer not to answer” (n=62)
MSM = men who have sex with men
HIV = human immunodeficiency virus
GED = general equivalency diploma
SP = sex partner
UAI = unprotected anal intercourse
MSP = male sex partner
Survey completion was higher among men from specific strata: men were more likely to complete the survey if they were white vs. nonwhite, >19 years vs. 18–19 years of age, gay-identified vs. non-gay-identifed, HIV-negative vs. HIV-positive, reported UAI in the past year vs. no UAI reported in the past year, or had only male sex partners vs. male and female sex partners (Table 1). Residence data available for a subset of participants revealed the following geographic distribution21: Northeast (15%), Midwest (18%), South (41%), and West (25%) (data not shown).
Of the 6,104 participants who began the baseline survey, 2,893 (47%) answered the question about acquiring free condoms, and 1,701 (59%) indicated that they had acquired free condoms in the past 12 months (data not shown). Some participants who provided information on the outcomes did not complete all items after the condom questions, so the number with complete data for this analysis was higher than the number completing the entire survey.
In the multivariable model (Table 2), acquiring free condoms was associated with reporting greater than a high school education, receiving an HIV test in the past 12 months, and reporting more than two male sex partners in the past 12 months. Men aged 45–54 years were less likely to report acquiring free condoms compared with men aged 18–19 years, and men reporting UAI in the past 12 months were also less likely to report acquiring free condoms compared with men who did not report UAI in the past 12 months. Although in the bivariate analysis men who reported using the Internet to meet a sex partner in the past year were more likely to receive free condoms than men who did not meet a sex partner on the Internet, this association was not significant in the multivariable model because of confounding with number of sex partners (data not shown).
Table 2.
Factors associated with self-reported acquisition and use of free condoms in the past 12 months among MSM enrolled in an online HIV prevention study (n=6,104): U.S., 2010
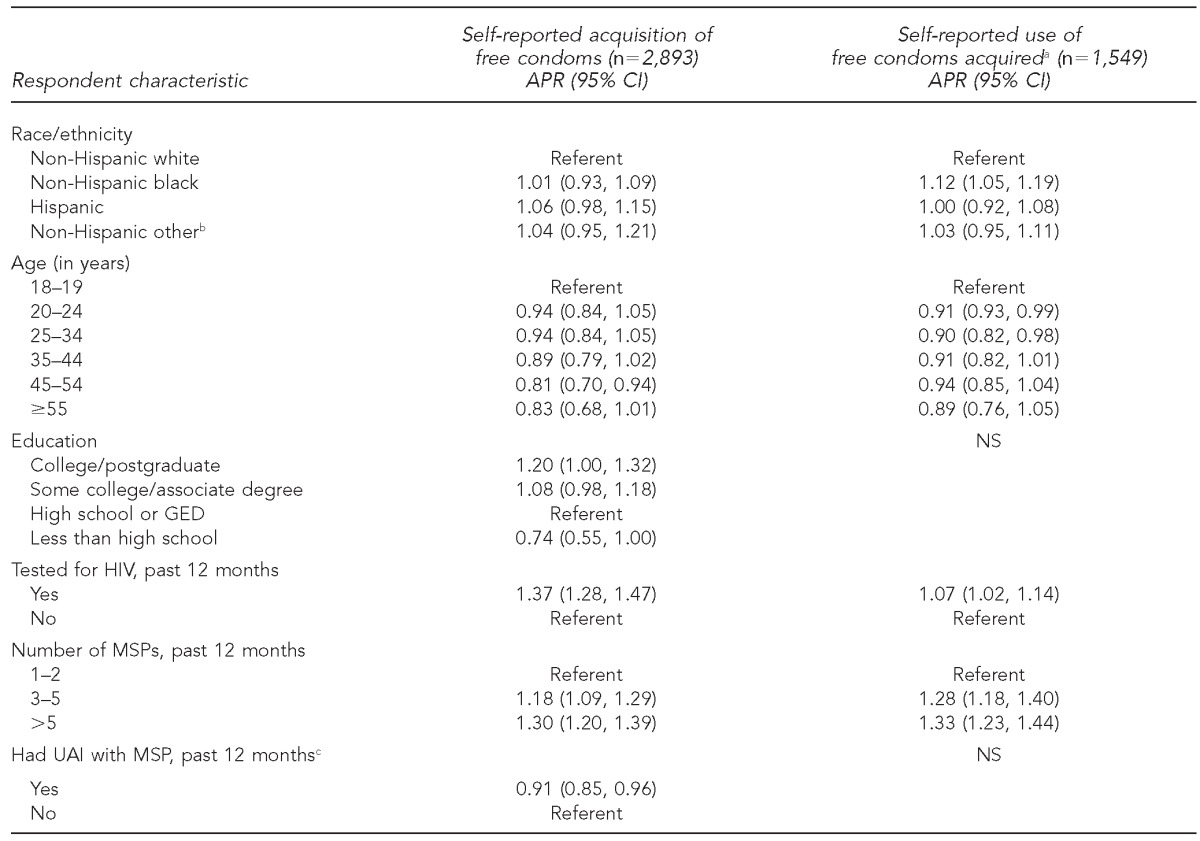
aAmong men who reported having anal sex in the past 12 months
bIncludes Asian/Pacific Islander, Native American/Alaska Native, multiracial, other, and prefer not to answer
cNot included as a variable in the multivariate log binomial model of the association between select characteristics and the use of free condoms
MSM = men who have sex with men
HIV = human immunodeficiency virus
APR = adjusted prevalence ratio
CI = confidence interval
NS = not significant
GED = general equivalency diploma
MSP = male sex partner
UAI = unprotected anal intercourse
Of the 1,701 men who reported receiving free condoms in the past 12 months, 1,549 (91%) responded to the survey question regarding the use of free condoms and reported having anal sex with a male partner in the past 12 months (data not shown). Table 2 describes the characteristics associated with using free condoms. Approximately 73% (n=1,127/1,549) of participants reported using the free condoms that they had acquired (data not shown). Reported use of free condoms was associated with black vs. white race/ethnicity, receiving vs. not receiving an HIV test in the past 12 months, and greater numbers of sex partners. There was no significant two-way interaction in either model.
DISCUSSION
Although condom distribution programs have existed in the U.S. for more than 30 years, few studies to date have examined the characteristics of individuals who acquire and use free condoms. To our knowledge, this analysis identified for the first time factors associated with the reported acquisition and use of free condoms by a geographically diverse group of MSM enrolled in an online HIV behavioral risk study. Overall, slightly less than 60% of our MSM population indicated that they had acquired free condoms in the past 12 months and, of those, approximately three-quarters of men who also indicated that they had had anal sex in the past year reported using the free condoms they had acquired.
Our data suggest that MSM who reported acquiring free condoms were more likely to be younger and have greater than a high school education than those who did not acquire free condoms, while men who reported using the free condoms were more likely to be black than white. Having received an HIV test in the past year was associated with both acquiring and using free condoms. This finding is unsurprising, considering that many HIV testing clinics and centers distribute free condoms. However, it is notable that, among men who reported acquiring free condoms, those who had been tested for HIV were significantly more likely to report using the free condoms they had acquired than those who had not been HIV tested recently. Similar risk-reducing behaviors post-HIV testing have been noted among HIV-positive men,22 and this result may suggest that a specific aspect of the HIV testing process (i.e., pre- or posttest counseling) encouraged these participants to use their free condoms. Alternatively, men who sought testing may have been inherently more motivated to reduce their risk of HIV acquisition.
It is also of note that men in our sample who reported acquiring free condoms were significantly less likely to report having UAI in the past 12 months. This may suggest that increasing condom accessibility increases condom use,14 or it could reflect a bias for men intending to use condoms to accept them if offered. Further, men with more than two male sex partners were more likely to report both acquiring and using free condoms compared with men with one to two partners, suggesting that free condom distribution may be benefiting those at high risk (i.e., men with more sex partners).
Among our respondents, approximately 59% reported acquiring free condoms in the past year. This figure is well below survey data from the 2003–2005 National HIV Behavioral Surveillance System (NHBS), in which 80% of MSM respondents reported receiving free condoms.18 Although there is an approximate five- to seven-year time span between our survey and the 2003–2005 NHBS, it is unlikely that the distribution of free condoms in the U.S. has decreased to levels that would account for the discrepancy seen between the two surveys. Instead, it is possible that, because NHBS MSM respondents are recruited from physical venues where MSM congregate (which are often the same locations where free condoms are distributed), the 2003–2005 NHBS overrepresented the proportion of all MSM who were in receipt of free condoms. Our data, in which MSM were recruited from a variety of social networking websites, reflect an estimate that includes non-venue-attending MSM.
Although fewer than 60% of our respondents acquired free condoms in the past 12 months, approximately 75% reported using the free condoms that they received, and those who used their condoms were more likely to be black than white. When considering the resources to distribute free condoms, it is a promising finding that the majority of MSM who reported both acquiring free condoms and having anal sex do use the free condoms that they obtain. Specifically, the fact that black men, who are at increased risk for HIV -infection among MSM, are more likely to use free condoms than white men is encouraging for the continuation of condom distribution programs. Further, 80% of young MSM aged 18–19 years in our sample reported using free condoms, an encouraging finding considering that young MSM are more likely to be unaware of their HIV infection than MSM of older age groups.19
Limitations
This study had a number of limitations. First, the two outcomes of this study were self-reported; therefore, reported acquisition and especially use of free condoms was likely overestimated.23,24 However, because the condom usage question was asked in the context of free condoms (i.e., we only asked if participants used their free condoms, not if they used any condoms), the extent of misclassification in our estimate might have been limited. Further, relative to in-person interviews, responses to sensitive questions in computerized interviews may be less susceptible to socially describable bias.25 Additionally, participants in the study were not representative of MSM who use social networking sites or MSM in the U.S., and we have previously characterized the potential selection and retention biases among MSM recruited into online surveys.26 A further selection bias may have been introduced due to the fact that the condom questions appeared in the final section of the survey, and less than half of our study population responded to the questions of interest. An analysis of the participants who did and did not complete the survey revealed that those participants who completed the survey were not representative of all consenting participants. Additionally, because this study relied on self-reported characteristics of participants, misclassification of race/ethnicity, age, or other respondent characteristics may have occurred. There was also the potential for recall bias, as we asked participants to report on their acquisition and use of free condoms from the past year. Further, we did not ask participants where they received free condoms; this information may have been useful in understanding where MSM are able to access free condoms. Also, we cannot exclude the possibility that free condoms that were received actually displaced condoms that would have otherwise been purchased by respondents, so the impact of condom distribution on increasing condom use was not evaluable in our study. Finally, it is possible that condom users in our population were more likely to pick up free condoms than men who do not use condoms; therefore, we do not assert causality based on our analysis.
CONCLUSIONS
The results of our study may provide guidance in the development and implementation of free condom distribution programs. First, our results suggest that distributed condoms are reportedly used and, although the relationship may not be causal, that men who reported acquiring free condoms were less likely to report UAI. Further, men with more male sex partners were more likely than those with fewer partners to both acquire and use free condoms. Second, our results suggest that receiving an HIV test was associated with both acquisition and use of free condoms. If causal, this association could represent an added benefit to the counseling and actual HIV testing that occurs during the session, and further emphasizes the importance of promoting HIV testing with counseling for MSM. Finally, we identified that, overall, a smaller proportion of our Internet-using MSM population reported acquiring free condoms compared with MSM previously sampled from venues, suggesting that additional outreach to venues other than where MSM congregate (e.g., commercial pharmacies/drug stores, grocery stores) may be beneficial. Because more than two-thirds of our study population indicated using the Internet to meet a sex partner in the past 12 months and were no more likely to acquire or use free condoms compared with men who did not use the Internet to meet a sex partner, the implementation of an Internet-based free condom ordering system may provide an opportunity to obtain free condoms for those MSM who do not frequent physical venues. Such a Web-based condom ordering system has been developed by the NYC DOHMH, but the distribution is limited to health and social service organizations, and is currently not available to individuals.13 Although this type of system would require extensive resources to operate, it would have the potential to reach a large population of MSM—including those residing outside metropolitan areas and those who do not typically access venues where condoms are distributed. Alternatively, online resources that provide locations where individuals may locate free condoms may also be of benefit. These programs, such as one in New York City,27 may be especially relevant in dense urban areas.
Condom distribution programs are a mainstay of HIV prevention programs in the U.S. but are difficult to evaluate aside from process measures. Despite the limitations of our analysis, we have collected data from a large, geographically diverse group of MSM about coverage of condom distribution and use of distributed condoms. Given the size of national investments in condom distribution, it would be advisable to strengthen the understanding of the impact of such programs. Triangulation of data from multiple, complementary sources would result in a richer understanding of these programs and in clearer understandings of how to leverage existing resources. In the meantime, according to our data, condom distribution programs appear to reach appropriately high-risk men, and a substantial majority of distributed condoms are reported to be used. This finding suggests that such programs should be retained as a part of a comprehensive HIV prevention approach for MSM.28
Footnotes
This research was supported by grants from the National Institute on Minority Health and Health Disparities (NIMHD) (RC1MD004370) and the Emory Center for Acquired Immunodeficiency Syndrome Research (CFAR) (P30 AI050409). The findings and conclusions in this article are those of the authors and do not necessarily represent the views of NIMHD or the Emory CFAR. This study was reviewed and approved by the Institutional Review Board of Emory University.
The authors thank Nicole Luisi for data management support and Adam Carpenter for editorial support.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Atlanta: CDC; 2012. Mar, [cited 2012 May 8]. HIV surveillance report: diagnoses of HIV infection and AIDS in the United States and dependent areas, 2010. Also available from: URL: http://www.cdc.gov/hiv/topics/surveillance/resources/reports. [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) HIV among gay and bisexual men. 2013. May, [cited 2013 Apr 16]. Available from: URL: http://www.cdc.gov/hiv/topics/msm/pdf/msm.pdf.
- 3.Sullivan PS, Wolitski RJ. HIV infection among gay and bisexual men. In: Wolitski R, Stall R, Valdiserri RO, editors. Unequal oppportunity: health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. pp. 220–47. [Google Scholar]
- 4.Additional recommendations to reduce sexual and drug abuse-related transmission of human T-lymphotropic virus type III/lymphadenopathy-associated virus. MMWR Morb Mortal Wkly Rep. 1986;35(10):152–5. [PubMed] [Google Scholar]
- 5.Update: barrier protection against HIV infection and other sexually transmitted diseases. MMWR Morb Mortal Wkly Rep. 1993;42(30):589–91. 597. [PubMed] [Google Scholar]
- 6.Varghese B, Maher JE, Peterman TA, Branson BM, Steketee RW. Reducing the risk of sexual HIV transmission: quantifying the per-act risk for HIV on the basis of choice of partner, sex act, and condom use. Sex Transm Dis. 2002;29:38–43. doi: 10.1097/00007435-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Weller S, Davis K. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002;(1):CD003255. doi: 10.1002/14651858.CD003255. [DOI] [PubMed] [Google Scholar]
- 8.Warner DL, Hatcher RA. A meta-analysis of condom effectiveness in reducing sexually transmitted HIV. Soc Sci Med. 1994;38:1169–70. doi: 10.1016/0277-9536(94)90233-x. [DOI] [PubMed] [Google Scholar]
- 9.The White House (US), Office of National AIDS Policy. National HIV/AIDS strategy for the United States. Washington: The White House; 2010. [cited 2011 Apr 27]. Also available from: URL: http://www.aids.gov/federal-resources/policies/national-hiv-aids-strategy/nhas.pdf. [Google Scholar]
- 10.Cohen D, Scribner R, Bedimo R, Farley TA. Cost as a barrier to condom use: the evidence for condom subsidies in the United States. Am J Public Health. 1999;89:567–8. doi: 10.2105/ajph.89.4.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore SG, Dahl DW, Gorn GJ, Weinberg CB. Coping with condom embarrassment. Psychol Health Med. 2006;11:70–9. doi: 10.1080/13548500500093696. [DOI] [PubMed] [Google Scholar]
- 12.Cohen DA. Condom availability for HIV/STD prevention. AIDS Patient Care STDS. 1999;13:731–7. doi: 10.1089/apc.1999.13.731. [DOI] [PubMed] [Google Scholar]
- 13.Renaud TC, Bocour A, Irvine MK, Bernstein KT, Begier EM, Sepkowitz KA, et al. The free condom initiative: promoting condom availability and use in New York City. Public Health Rep. 2009;124:481–9. doi: 10.1177/003335490912400404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen DA, Farley TA, Bedimo-Etame JR, Scribner R, Ward W, Kendall C, et al. Implementation of condom social marketing in Louisiana, 1993 to 1996. Am J Public Health. 1999;89:204–8. doi: 10.2105/ajph.89.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedimo AL, Pinkerton SD, Cohen DA, Gray B, Farley TA. Condom distribution: a cost-utility analysis. Int J STD AIDS. 2002;13:384–92. doi: 10.1258/095646202760029804. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (US) Condom distribution as a structural level intervention. 2010. Oct, [cited 2013 May 15]. Available from: URL: http://www.cdc.gov/hiv/pdf/prevention_programs_condom_distribution.pdf.
- 17.Rhodes SD, Hergenrather KC, Yee LJ, Wilkin AM, Clarke TL, Wooldredge R, et al. Condom acquisition and preferences within a sample of sexually active gay and bisexual men in the southern United States. AIDS Patient Care STDS. 2007;21:861–70. doi: 10.1089/apc.2007.0027. [DOI] [PubMed] [Google Scholar]
- 18.Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [PubMed] [Google Scholar]
- 19.Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–7. [PubMed] [Google Scholar]
- 20.SAS Institute, Inc. SAS®: Version 9.2 for Windows. Cary (NC): SAS Institute, Inc.; 2009. [Google Scholar]
- 21.Census Bureau (US) Census regions and divisions of the United States. [cited 2012 Oct 21]. Available from: URL: https://www.census.gov/geo/www/us_regdiv.pdf.
- 22.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 23.Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108:339–62. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- 24.Gray RH. Use of hormonal contraceptives and risk of HIV-1 transmission. Lancet Infect Dis. 2012;12 doi: 10.1016/S1473-3099(12)70111-1. author reply 510-1. [DOI] [PubMed] [Google Scholar]
- 25.Kissinger P, Rice J, Farley T, Trimm S, Jewitt K, Margavio V, et al. Application of computer-assisted interviews to sexual behavior research. Am J Epidemiol. 1999;149:950–4. doi: 10.1093/oxfordjournals.aje.a009739. [DOI] [PubMed] [Google Scholar]
- 26.Sullivan PS, Khosropour CM, Luisi N, Amsden M, Coggia T, Wingood GM, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13:e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.New York City Department of Health and Mental Hygiene. Site locator. [cited 2013 Apr 16]. Available from: URL: https://a816-healthpsi.nyc.gov/DispensingSiteLocator/mainView.do.
- 28.Sullivan PS, Carballo-Diéguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–99. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


