Abstract
Background:
Circadian rhythm sleep disorders are a presentation of sleep disorders in patients with multiple sclerosis (MS). This study aims to compare this problem in MS patients with healthy people and to determine its association with chronic fatigue in MS patients.
Materials and Methods:
A case-control study was performed on 120 MS patients and 60 healthy subjects matched for age and sex, in 2009 in MS Clinic Alzahra Hospital. Sleep quality, rhythm and fatigue severity were assessed using PSQI (Pittsburgh sleep quality index) and FSS (Fatigue severity Scale) questionnaires, respectively. Its reliability and validity has been confirmed in several studies (Cronbach's alpha = 0.83). This index has seven sections including patient's assessment of his/her sleep, sleep duration, efficacy of routine sleep, sleep disorders, use of hypnotic medication, and dysfunction in daily activities.
Results:
Circadian rhythm sleep disorder was more frequent in MS patients relative to healthy subjects (P: 0.002). It was higher in MS patients with severe fatigue relative to MS patients with mild fatigue (P: 0.05). Fatigue severity was 49.9 ± 8.2 and 22.5 ± 7.4 in the first and second group, respectively. PSQI index was 7.9 ± 4.5 in patients with severe fatigue and 5.9 ± 4.5 in patients with mild fatigue and 4.5 ± 2.4 in the control group (P: 0.0001).
Conclusion:
Circadian rhythm sleep disorders are more frequent in MS patients and those with fatigue. Recognition and management of circadian rhythm sleep disorders in MS patients, especially those with fatigue may be helpful in improving care of these patients.
Keywords: Chronic fatigue, circadian rhythm sleep disorder, fatigue severity scale, multiple sclerosis, Pittsburg sleep quality index
INTRODUCTION
Multiple sclerosis is an autoimmune demyelinative disease of the central nervous system. Its prevalence is about 2.5 million people worldwide.[1] It usually affects people 20-50 years old and is more prevalent in women.[2]
Circadian rhythm disorder is defined as discrepancy between patient's sleep pattern and normal sleep pattern. These disorders cause complaints of insomnia, hypersomnia and finally lead to impaired functionality and low quality of life.[3] Circadian rhythm sleep disorders may be due to external and internal factors. External factors include jet lag and sleep disorders due to shift work. Internal factors are of several types: In delayed sleep phase syndrome, sleep starts with ≥2 h delay. In advanced sleep-phase syndrome sleep start is sooner than normal, around 6-9 pm and the patient wakes up sooner than normal, about 2-5 am. In non-24 h sleep-wake syndrome sleep starts increasingly later every day. In irregular sleep pattern, sleep pattern is very irregular so that patients wake up at night and take naps during daytime.[4,5]
Fatigue is the most common reported symptom in MS patients.[6] It is associated with lower quality of life. It is defined as lack of physical and mental energy perceived by the patient that prevents ordinary activities.[7,8] Physiopathologic basis of fatigue in MS patients is complicated and underlying mechanisms are not well known. It might be related to MS process or secondary to sleep disorders or depression.[9]
While sleep makes one third of every human's life, its quality affects the other two third. In a study, prevalence of sleep complaints was three fold in MS patients.[10] Taphoorn and colleagues found no circadian rhythm sleep disorder in MS patients but Soorensen found abnormalities of circadian sleep rhythm in relapsing remitting MS.[11,12] Attarian compared 15 MS patients with complain of fatigue with 15 MS patients without fatigue and found that there is significant association between chronic fatigue and circadian rhythm sleep disorder in MS patients.[13]
Few studies have investigated the role of fatigue in sleep disorder in MS patients, especially circadian rhythm sleep disorders. This study aims to investigate the frequency of circadian rhythm sleep disorders in MS patients compared with control group with respect to different severity fatigue.
MATERIALS AND METHODS
A case control study was performed in 2009 in MS Clinic Alzahra Hospital in Isfahan. Inclusion criteria were: Age >18 years old, EDSS score ≥2 and history of relapsing remitting MS for at least two years. Exclusion criteria were acute relapse phase, substance abuse, taking sedatives or immunosuppressive agents, comorbid condition or pregnancy.
MS patients with relapsing remitting type referring to Alzahra Hospital MS Clinic were recruited using easy sampling method. Their healthy family members or relatives were included in the control group after matching for age and sex.
Assessment of patients’ disability was performed using EDSS (Expanded disability scale score). This is a standard questionnaire.[14,15]
Sleep quality was assessed using Pittsburgh sleep quality index (PSQI).[16,17] Its reliability and validity has been confirmed in several studies (Cronbach's alpha = 0.83). This index has seven sections including patient's assessment of his/her sleep, sleep duration, efficacy of routine sleep, sleep disorders, use of hypnotic medication, and dysfunction in daily activities. Every item scores between 0-3. 0 means that the patient had not have the condition in the previous month and 3 means that it had happened at least three times in the previous week. A score of 5 or higher means low sleep quality. Circadian rhythm sleep disorder was assessed by the four first questions.
Fatigue severity was assessed using FSS (Fatigue Severity Scale). The reliability and validity of this questionnaire has been determined before. It contains nine questions with Likert scale, ranging from 1-7. Lower scores mean disagreement and higher scores show agreement. A score of 36 or higher is regarded as severe chronic fatigue and lower than that is mild fatigue.
One hundred and twenty MS patients including those with mild and severe fatigue were studied. Sixty healthy subjects who were family members or relatives of patients and were matched for age and sex were the control group.
After getting informed consent EDSS and FSS questionnaires were completed in the case group and demographic data and PSQI in both groups. The data was analyzed using Ki square and independent sample t-test using SPSS software package (version 16, SPSS Inc., Chicago, IL).
RESULTS
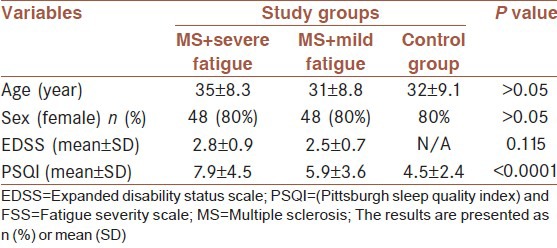
Mean age of studied subjects was 33 ± 8.8 years. Each group included 48 women (80%) and 12 men (20%). Patients and control group were matched for age and sex. EDSS was 2.8 ± 0.9 in patients with severe fatigue and 2.5 ± 0.7 in patients with mild fatigue. Fatigue severity was 49.9 ± 8.2 and 22.5 ± 7.4 in the first and second group, respectively. PSQI index was 7.9 ± 4.5 in patients with severe fatigue and 5.9 ± 4.5 in patients with mild fatigue and 4.5 ± 2.4 in the control group (P: 0.0001).
Circadian rhythm sleep disorders including advanced sleep phase syndrome, delayed sleep phase syndrome and irregular sleep wake pattern were found in 4 (6.7%), 7 (11.7%) and 20 (33.3%) patients, respectively. Twenty-nine patients (48.3%) did not have circadian rhythm sleep disorder.
In MS patients with mild fatigue, 2 (3.3%), 11 (18.3%) and 5 (8.3%) had advanced sleep phase syndrome, delayed sleep phase syndrome and irregular sleep wake pattern syndrome, respectively. Forty-two (70%) patients did not have circadian rhythm sleep disorder. In the control group the disorders were found in 1 (1.7%), 7 (11.7%) and 6 (10%) patients, respectively (P: 0.002). PSQI was 6.5 ± 0.7, 7.4 ± 4.3 and 3 ± 9.8 in three types of sleep disorder in MS patients with severe fatigue, and 5.1 ± 3.1 for patients without rhythm disorder (P: 0.015). In the control group the PSQI scale was 6, 7.7 ± 2.4 and 7 ± 1.6 in three groups of rhythm disorder, respectively. It was 3.6 ± 1.8 in patients without rhythm disorder (P: 0.0001) [Table 1].
Table 1.
Mean of EDSS, FSS and PSQI in MS patients and control group
DISCUSSION
In this study various types of circadian sleep disorder including advanced sleep phase syndrome, delayed sleep phase syndrome and irregular sleep wake pattern in MS patients with mild and severe fatigue were compared with healthy subjects. Circadian sleep rhythm disorders were higher significantly in MS patients relative to healthy subjects. They were higher in patients with severe fatigue compared with patients with mild fatigue.
The etiology of fatigue in MS patients is not well known. Metabolic derangement and structural abnormalities in nerve tracts related to basal ganglia, thalamus, limbic system and neocortex are involved in the pathophysiology of fatigue.[16] Sleep disorders, especially circadian rhythm sleep disorder may be an important factor in MS fatigue.[18] However, fatigue must be differentiated from sleepiness related to sleep disorder.
MS is associated with various types of sleep disorders.[19,20] The frequency of circadian sleep rhythm is not known in the Iranian general population or in MS patients.[21] Circadian rhythm varies according to age, cultural and geographical conditions.[5] These disorders lead to insomnia, excessive day sleep or both. This leads to dysfunction at school, work or socially.[4]
A study in Iranian patients similar to our study showed circadian sleep rhythm in MS patients with fatigue.[13] However, another study did not show any circadian sleep rhythm in MS patients.[12] These findings support more vulnerability of biological clock in MS patients. Different findings might be due to small sample size, simultaneous mood disorders, lack of discrimination between various MS classes, using medication, and different cultural and social background. Circadian rhythm sleep disorder cannot be related solely to fatigue as it is a multifactorial phenomenon.
Anatomic location of demyelinative lesions (such as optic nerve and hypothalamus) may have a role in the pathogenesis of sleep disorder.[12] Demyelination of nerve fibers and tracts may impair biological clock. Confirming the association between anatomic location of demyelinative plaques with types of sleep disorder, especially circadian sleep rhythm needs further assessment usin g MRI and functional MRI.
The findings of this study showed that circadian sleep rhythm disorders are more frequent in MS patients and those with fatigue. Recognition and management of circadian rhythm disorders in MS patients, especially those with MS fatigue may be helpful in improving care of these patients.
It is suggested that MS patients suffering from fatigue be evaluated for circadian rhythm sleep disorders. Larger studies are needed to determine frequency of sleep disorders in MS patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ramagopalan SV, Sadovnick AD. Epidemiology of multiple sclerosis. Neurol Clin. 2011;29:207–17. doi: 10.1016/j.ncl.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Rojas JI, Patrucco L, Besada C, Funes J, Cristiano E. Sex-related differences in atrophy and lesion load in multiple sclerosis patients. Neurologia. 2012 doi: 10.1016/j.nrl.2012.10.008. In Press. [DOI] [PubMed] [Google Scholar]
- 3.diagnostic and coding manual. 2nd ed. Westchester: American Academy of Sleep; 2007. Medicine, A.A.o.S. The international classification of sleep disorders. [Google Scholar]
- 4.Sack RL, Auckley D, Auger RR, Carskadon MA, Wright KP, Jr, Vitiello MV, et al. Circadian rhythm sleep disorders: Part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine review. Sleep. 2007;30:1484–501. doi: 10.1093/sleep/30.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sack RL, Auckley D, Auger RR, Carskadon MA, Wright KP, Jr, Vitiello MV, et al. Circadian rhythm sleep disorders: Part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep. 2007;30:1460–83. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan F, McPhail T, Brand C, Turner-Stokes L, Kilpatrick T. Multiple sclerosis: Disability profile and quality of life in an Australian community cohort. Int J Rehabil Res. 2006;29:87–96. doi: 10.1097/01.mrr.0000194393.56772.62. [DOI] [PubMed] [Google Scholar]
- 7.Iriarte J, Subirá ML, Castro P. Modalities of fatigue in multiple sclerosis: Correlation with clinical and biological factors. Mult Scler. 2000;6:124–30. doi: 10.1177/135245850000600212. [DOI] [PubMed] [Google Scholar]
- 8.Turpin KV, Carroll LJ, Cassidy JD, Hader WJ. Deterioration in the health-related quality of life of persons with multiple sclerosis: The possible warning signs. Mult Scler. 2007;13:1038–45. doi: 10.1177/1352458507078393. [DOI] [PubMed] [Google Scholar]
- 9.Washington, DC: The Council; 1998. Guidelines, M.S.C.f.C.P., Fatigue and multiple sclerosis: Evidence-based management strategies for fatigue in multiple sclerosis. [Google Scholar]
- 10.Clark CM, Fleming JA, Li D, Oger J, Klonoff H, Paty D. Sleep disturbance, depression, and lesion site in patients with multiple sclerosis. Arch Neurol. 1992;49:641–3. doi: 10.1001/archneur.1992.00530300077013. [DOI] [PubMed] [Google Scholar]
- 11.Søorensen KV, Alslev T, Christensen SE, Jensen NB, Orskov H. CSF somatostatin in multiple sclerosis: Reversible loss of diurnal oscillation in relapses. Neurology. 1987;37:1050–3. doi: 10.1212/wnl.37.6.1050. [DOI] [PubMed] [Google Scholar]
- 12.Taphoorn MJ, van Someren E, Snoek FJ, Strijers RL, Swaab DF, Visscher F, et al. Fatigue, sleep disturbances and circadian rhythm in multiple sclerosis. J Neurol. 1993;240:446–8. doi: 10.1007/BF00867360. [DOI] [PubMed] [Google Scholar]
- 13.Attarian HP, Brown KM, Duntley SP, Carter JD, Cross AH. The relationship of sleep disturbances and fatigue in multiple sclerosis. Arch Neurol. 2004;61:525–8. doi: 10.1001/archneur.61.4.525. [DOI] [PubMed] [Google Scholar]
- 14.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 15.Kurtzke JF. Natural history and clinical outcome measures for multiple sclerosis studies. Why at the present time does EDSS scale remain a preferred outcome measure to evaluate disease evolution? Neurol Sci. 2000;21:339–41. doi: 10.1007/s100720070047. [DOI] [PubMed] [Google Scholar]
- 16.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 18.Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet. 2004;363:978–88. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- 19.Ferini-Strambi L, Filippi M, Martinelli V, Oldani A, Rovaris M, Zucconi M, et al. Nocturnal sleep study in multiple sclerosis: Correlations with clinical and brain magnetic resonance imaging findings. J Neurol Sci. 1994;125:194–7. doi: 10.1016/0022-510x(94)90035-3. [DOI] [PubMed] [Google Scholar]
- 20.Tachibana N, Howard RS, Hirsch NP, Miller DH, Moseley IF, Fish D. Sleep problems in multiple sclerosis. Eur Neurol. 1994;34:320–3. doi: 10.1159/000117070. [DOI] [PubMed] [Google Scholar]
- 21.Najafi MR, Saadatnia M, Saffarifard A, Keyhanian K, Davoudi V. Epidemiology of restless legs syndrome in the Iranian population. Sleep Biol Rhythms. 2011;9:56–9. [Google Scholar]


