Abstract
Wind disasters are responsible for tremendous physical destruction, injury, loss of life and economic damage. In this review, we discuss disaster preparedness and effective medical response to wind disasters. The epidemiology of disease and injury patterns observed in the early and late phases of wind disasters are reviewed. The authors highlight the importance of advance planning and adequate preparation as well as prompt and well-organized response to potential damage involving healthcare infrastructure and the associated consequences to the medical response system. Ways to minimize both the extent of infrastructure damage and its effects on the healthcare system are discussed, focusing on lessons learned from recent major wind disasters around the globe. Finally, aspects of healthcare delivery in disaster zones are reviewed.
Keywords: Comprehensive review, cyclone, disaster management, disaster preparedness, epidemiology, hurricane, injury patterns, tornado, wind disaster, wind disaster management
INTRODUCTION
Wind disasters (WDs) contribute to tremendous physical destruction, injury, loss of life, and economic damage. The effects of WDs may not be limited to wind damage, as concurrent heavy rains and flooding often wreak additional havoc.[1] While there is some evidence pointing towards increasing number of destructive wind phenomena over the last few decades, these findings are at least partly due to the fact that our observational capabilities and recording of such events have improved markedly, leading to greater public awareness of severe weather events worldwide.[2] In this review, we will focus on medical response to WDs, including epidemiologic and triage considerations.
WIND DISASTERS AS NATURAL CALAMITIES
A natural disaster is defined as an event of nature that overwhelms local resources and threatens the function and safety of the community. Disasters are the ultimate test of a community's emergency response capability. Planning is very difficult due to the unpredictable character of natural disasters. A thoughtful and well-organized emergency strategy that is flexible and adaptable in face of unforeseen circumstances is crucial. WDs may affect the economic, social, physical, and psychological fabric of any community.
In recent years, the combination of population growth and development along vulnerable coastal areas has led to an increase in hurricane-related deaths, injuries, and economic costs.[3] Most hurricane-driven mortality originates from secondary disasters (i.e., storm surges, flash flooding, and tornados) triggered by the original event. In coastal regions, the level of a hurricane's storm surge is one of the strongest predictors of mortality. Winds are the second deadliest aspect of a hurricane, often causing property damage (collapse of houses and other man-made structures). In a hurricane, many injuries are caused by airborne objects. The most common non-fatal traumatic injury pattern in a hurricane consists of superficial lacerations from airborne glass and/or other debris.[4,5]
In the hours following a major natural disaster, the immediate rescue efforts originate from the affected community itself. Local resources are quickly recruited and organized to address the immediate needs at hand. Within the first 24 hours, the focus must remain on ensuring that the most critically ill and accessible patients receive the appropriate medical attention. However, as with many natural disasters, the situation is further complicated by the massive disruption of critical infrastructure that prevents an appropriately organized and comprehensive medical response.[6] Consequently, nearly all members of a given community and/or region are affected by a WD.
OVERVIEW OF WIND DISASTER TYPES
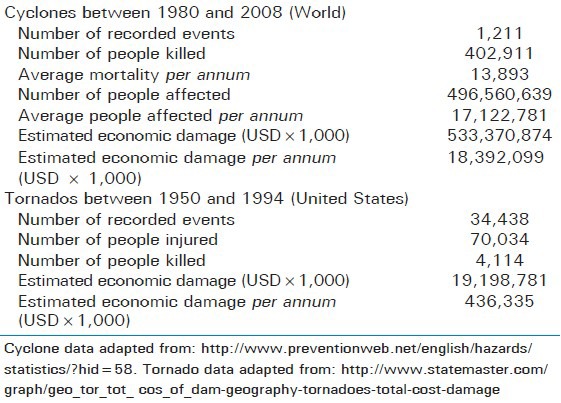
WDs such as hurricanes and tornados occur relatively frequently and affect our lives in multiple ways. The estimated average annual damage caused by WDs exceeds $6 billion, constituting more than 50% of all total weather-related damage and more than 40% of total natural disaster-related damage.[7,8] These costs are exemplified by the approximately $26.5 billion in losses from Hurricane Andrew in 1992[9] and the $1.2 billion in damages caused by the May 1999 Oklahoma Tornado.[10] The magnitude of human and economic impact associated with wind disasters is presented in Table 1.
Table 1.
Impact of cyclones and tornados
Tornados
Tornados usually develop during intense thunderstorms classified as “supercell thunderstorms”.[11] Within these storms, tornados result from updrafts created by solar warming of the earth's surface. These updrafts then develop into a vortex with strong rotary winds and violent pressure changes.[12] In an average year, 800 tornados are reported in the United States.[11] Due to the relatively brief or absent warning, a tornado gives a community little time to prepare or seek shelter, and the morbidity and mortality is proportionally higher compared to other WDs.
Tornado outbreaks are among some of the most destructive weather phenomena.[2] During the last 50 years, tornados have been documented to cause at least 9,000 deaths[12] and over 70,000 injuries.[11] During the same period of time, the cumulative monetary damages exceeded $20 trillion,[11] and almost 100,000 applications for federal disaster assistance have been submitted as a result of tornados between 1970-1980.[11] In the United States, May tends to be the peak month for tornado occurrence in the Southern plains states, while the upper Midwest and Great Lakes region suffer the highest frequency in the summer months.[11]
Cyclones/Hurricanes
Cyclones may be referred to as ‘typhoons’ or ‘hurricanes’. A cyclone is an atmospheric system characterized by the rapid inward circulation of an air mass around a low-pressure center, accompanied by destructive weather. These weather events rotate clockwise in the Southern hemisphere and counterclockwise in the Northern hemisphere and typically number 10-15 per annum. Tropical cyclones in the North Atlantic, the North east Pacific east of the International Date Line or the South Pacific with sustained winds >74 mph are termed hurricanes. Storms that start in the Southern Pacific between longitudes of 100-180 degrees east are called typhoons. These storms have the potential of causing massive destruction due to wind, rain, and flood damage.
The United States ranks first in the number of annual hurricane impacts.[13] For the period 1900-2004, hurricane mortality for the United States was approximately 15,000. Interestingly, half of these deaths occurred in 1900 when the deadliest hurricane (and the deadliest natural disaster) in U.S. history killed 7,200 people in Galveston, Texas. Three other hurricanes in the U.S. have been especially devastating-1,836 people perished in a hurricane that pummeled Florida's Lake Okeechobee region in 1928, 408 people died in the 1935 Florida Keys Labor Day “Storm of the Century”, the most intense hurricane ever recorded for the United States, and approximately 1,000 people died as a result of Hurricane Katrina in 2005.[13,14]
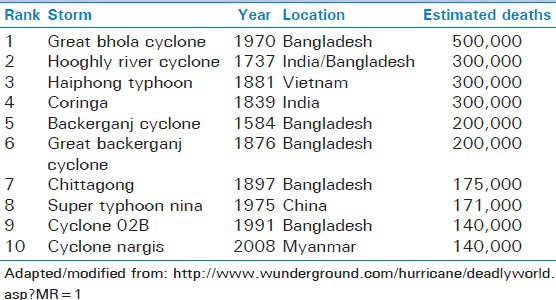
In developing nations, cyclone mortality continues to be significant [Table 2], with deaths occurring primarily during the storm surge of the cyclone impact phase. This is in contrast with developed nations, where tropical cyclone mortality has declined markedly, and the majority of deaths now occur in the post-impact period.[13] Typhoon Saomei in Southern China had a death rate 530 times that of Hurricane Andrew. In a recent article describing Saomei, injuries were highest with the first peak of wind speed and were associated with living in houses directly facing the sea. Other risks included failure to reinforce doors or windows, staying in a damaged room, near a window or door.[15]
Table 2.
Ten deadliest wind storms since 1737
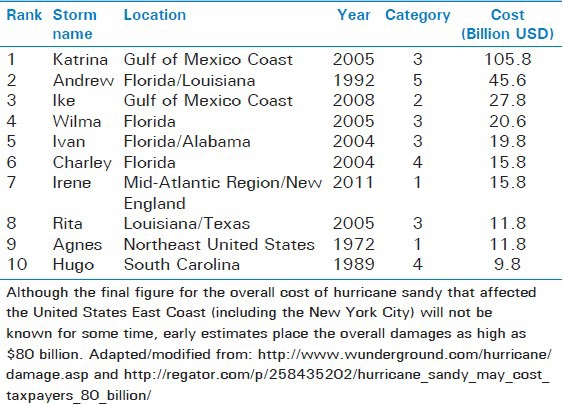
Public health consequences associated with hurricanes include storm-related mortality, injury, infectious disease, psychosocial effects, displacement and homelessness, damage to healthcare infrastructure, disruption of public health services, transformation of ecosystems, social dislocation, loss of jobs and livelihood, and economic crisis.[1,9,16] As with mortality, these are disproportionately worse in developing nations.[13] Hurricanes are among the costliest of WDs [Table 3]. Prior to Hurricane Katrina (preliminary cost, $100 billion), Hurricane Andrew was the most expensive disaster event in the United States ($35.6 billion).[13,17] A recent menace along the eastern coast of the U.S., Hurricane Sandy, in 2012, was the largest reported hurricane arising in the Atlantic and was estimated to result in a cost of $60 billion, including $20 billion in property damages and with at least 110 fatalities.[18]
Table 3.
Costliest wind storms in modern history
PHYSICAL INJURY PATTERNS BY WIND DISASTER TYPES
Cyclones: Storm-associated injury
For hurricanes, trauma represents the major cause of death and the primary cause of morbidity. Minor trauma is common. The top three cyclone-related injuries are lacerations, blunt trauma, and puncture wounds, with 80% of these injuries being confined to the feet and lower extremities.[13] This is in contrast to tornados, with head and neck trauma more commonly seen. See Table 4 for additional details.
Table 4.
Impact of wind disasters on victims and healthcare facilities. Injury patterns, health concerns, and healthcare facility preparations/responses are categorized according to disaster phase
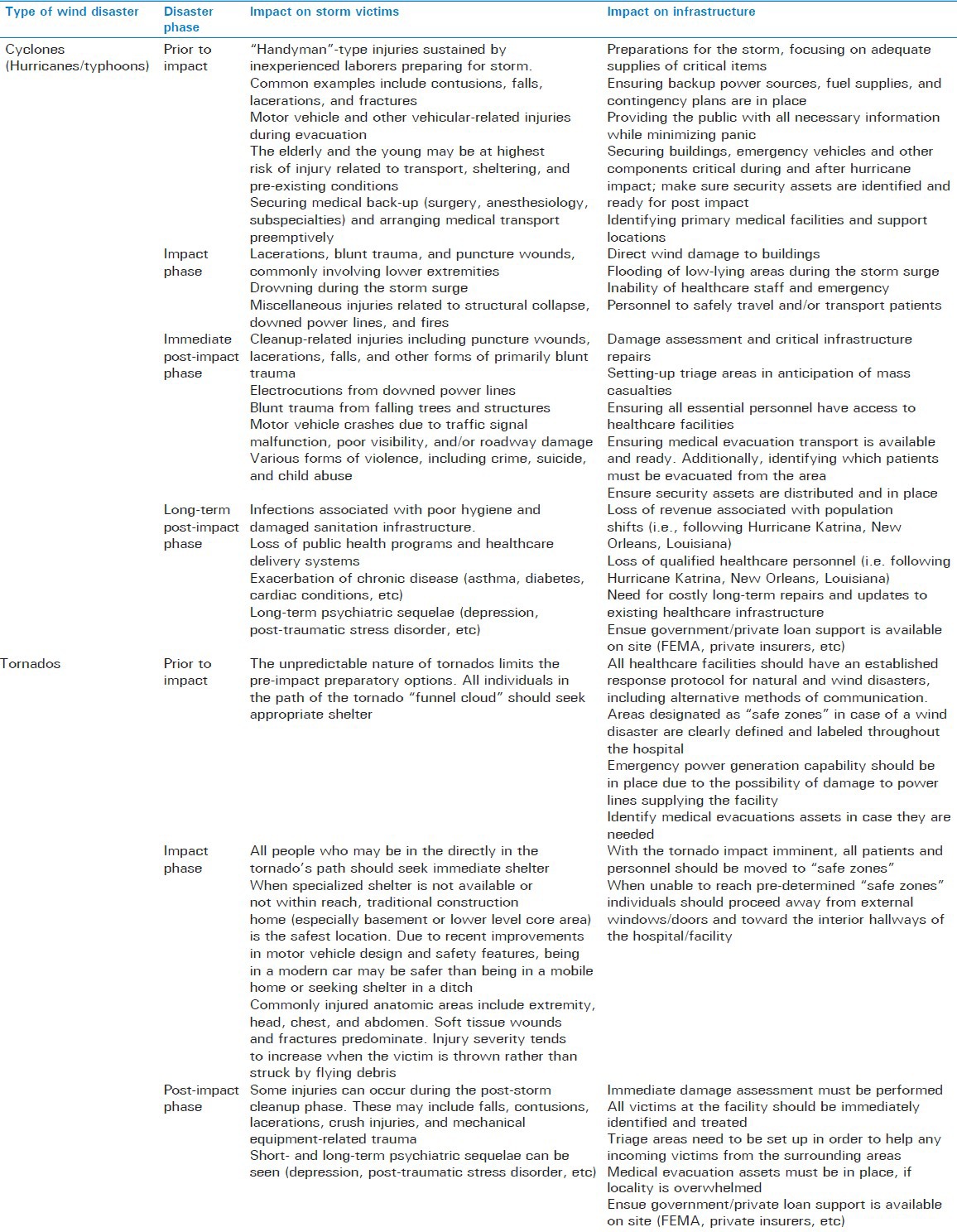
Cyclones: Injury prior to impact
Prior to storm impact, injuries such as falls, blunt trauma, lacerations, and muscle strains may occur as preparations to secure homes and businesses are hurriedly undertaken.[13] Injuries also occur during mass evacuations, including potential increases in motor vehicle crashes.[19,20,21] The elderly and the young both are particularly vulnerable to injury during transport and sheltering.[20,21,22] Structural collapse, wind-borne debris, and falling trees and power lines are hazardous during impact and after the storm.
Cyclones: Injury during the impact phase
Victims may be directly exposed to the harmful forces of wind, rain, flood, or storm surge as a consequence of damage to their shelter or attempts to drive to safety while the storm is raging.[13] Prior to the implementation of warning, evacuation, and shelter systems, drowning from storm surge accounted for 90% of cyclone-attributable mortality.[13] High-density settlement in low-lying areas with poor housing construction increases risks.[23] Much like in a tornado, occupancy of a mobile home during the impact phase poses a high risk for injury or death. Prior to 1990, the majority of deaths due to hurricanes in the US occurred at the time of impact and were attributed to drowning in storm surges. As hurricane forecasting and evacuation/shelter procedures have improved, there has been a shift in hurricane mortality. Storm-surge drowning deaths have decreased, leaving the majority of impact phase deaths due to high-velocity winds,[13] and much storm-related mortality and morbidity now occurs during the post-impact period.
Cyclones: Injury during the post-impact phase
Injuries seen during the post-impact phase include puncture wounds, lacerations, falls, and trauma related to cleanup.[13] Burns may occur from the use of candles, open fires, portable stoves, or gas-powered generators during power outages; concomitantly, an increase in carbon monoxide toxicities may be seen.[24] Prominent causes of death and injury include electrocutions from downed power lines, chain-saw injuries, blunt trauma from falling trees and structures, and motor vehicle fatalities occurring during the early post-impact period.[22] A significant number of people experience fear and distress at the time of the disaster, though most return to normal functioning.[13] Some may develop experience post-traumatic stress disorder (PTSD) or major depression, and rates of suicide and child abuse appear to rise following natural disasters.[13]
Tornado-associated injuries
Risk factors for injury and death during a tornado include poor building anchorage, occupant location other than a basement, age over 70 years, and high wind strength.[25] The serious injury rate for occupants in mobile homes has been calculated at 85.1 per 1,000 as compared to 3 per 1,000 for standard construction homes.[11] The elderly may be less likely to receive warning or take effective protective actions, and co-morbid medical conditions can contribute to slowed reaction and increased risk of morbidity and mortality.[11,22,26]
Injury patterns from tornados tend to involve multiple systems.[12] Commonly injured anatomic regions included the chest (45%), abdomen (27%), extremity (91%), and head (45%).[12] Furthermore, trauma severity increases if the victim is thrown rather than struck by flying debris.[12] Most of the serious injuries and deaths are the result of the victims or solid objects becoming airborne or structural collapse, with mortality being most frequently attributed to head trauma, followed by crush injuries to the chest, abdomen, and pelvis.[11,12] Most tornado fatalities die at the scene and tend to be either in exposed areas or in mobile homes.
Soft tissue wounds are among the most frequently reported injuries, usually resulting from debris accelerated by winds. Additional soft tissue injury can occur when fine particles of soil, mud, sand, and water strike the skin at high speeds. These particles can also obscure other more serious injuries.[11] Wounds tend to be deep and contaminated with soil, foreign bodies, and other debris and are most often in exposed areas of the body, such as the head and neck.[11] Fractures are the next most frequent nonfatal injury associated with tornados and are the most common reason for hospital admission. Many fractures are open and contaminated.
Patients may also present for treatment of conditions not directly related to the storm. The most common reasons for indirectly related health effects during a case study of an Oklahoma tornado were medical conditions not related to injury, injuries incurred while preparing for the tornados, inhalation injuries, and injuries occurring during cleanup activities.[27] PTSD rates following tornados have been reported between 2-59%, with children and the elderly at higher risk.[11] See Table 4 for additional details.
INFECTIOUS AND PUBLIC HEALTH CONSIDERATIONS
After the acute phase of a natural disaster, the focus of the emergency personnel changes from triage and treatment to assessing and addressing public health concerns. Survivors change their focus from identifying and recognizing problems to restoration and reconstruction. The most pressing public health concerns include quickly establishing adequate hygiene protocols, controlling the outbreak of endemic diseases, and re-establishing routine health activities through the utilization of outside medical aid or the establishment temporary hospitals and clinics in suitable locations.[28] The application of any medical system to a disaster region depends heavily upon the local conditions, equipment availability, prevailing practices, and the number of victims.[29] One of the primary goals of local health and government officials is to restore normal operations of local hospitals and clinics, disease monitoring systems, and other public health programs. Vector control programs are the single most effective method of controling diseases such as malaria, while vaccination programs are extremely effective for preventing outbreaks of illnesses such as measles, whooping cough, and poliomyelitis.[30] It is important to note that most deaths are caused by injuries from the natural disaster, not by disease.[13]
Cyclones
Outbreaks of infectious diseases following hurricanes are more common in the developing world. Several factors favor the emergence of infectious diseases following hurricanes in developing nations, including high endemic rates of disease, low immunization rates, lack of clean water, poor sanitation, prolonged crowding in shelters, and inadequate nutrition. Prolonged disruption of public health services is more likely to occur in developing countries and may contribute to an increase in disease.[13] Both early and ongoing surveillance are necessary to detect increases in infectious diseases, including those with prolonged incubation periods (hepatitis, tuberculosis) and those characterized by later emergence due to delayed vector proliferation.
Tornados
Tornado wounds tend to be highly contaminated with foreign material and result in a high incidence of infectious complications. Wound infections from tornado injuries are usually polymicrobial, with Gram-negative species such as Escherichia coli, Klebsiella, Serratia, Proteus, and Pseudomonas species being prominent.[11] Following the 2011 Joplin, Missouri tornado, a dangerous outbreak of mucormycosis was observed among survivors with multiple injuries and secondary wound infections.[31,32] Because of the high infection rates in wounds closed primarily, some authors recommend delayed primary closure of wounds caused by tornados.[11]
INJURY PREVENTION
Cyclones
Effective forecasting, warning, evacuation, and sheltering are primary approaches to reducing hurricane-related mortality and morbidity for persons who reside in high-risk locales.[13] Tropical cyclones can be detected at formation and are tracked with precision. Forecasters can fairly accurately determine the location, trajectory, central pressure, wind speed, storm surge, point of landfall, and rainfall production. Additionally, 24 hour news availability has allowed for improved warning systems, with frequently updated guidance regarding preparation, protection, evacuation, and sheltering.[13] After forecasting and warning, evacuation must occur, starting with keys and barrier islands and then coastal areas.[33] Intimately tied to effective evacuation procedures is the availability of safe shelters.[34] Observation of hurricane mortality patterns in developed nations suggests a need for specific guidance and education on post-impact hazards such as downed power lines and falling trees.[13]
Tornados
Advanced warning of an approaching tornado and the response that ensues are the most important factors in reducing morbidity and mortality.[11] A ‘Tornado Watch’ indicates conditions facilitating the development of tornados, while a ‘Tornado Warning’ indicates either visual or radar detection of a tornado.
Because of increased morbidity and mortality that comes by residing in a mobile home, current recommendations are to leave the mobile home and seek more substantial shelter. Mobile home parks should provide communal tornado shelters for occupants.[11] Being in a motor vehicle is also associated with increased risk when compared to a conventional home.[11] If outdoors, people should seek shelter or lie low in a ditch face-down while covering the head, and while previous recommendations were to evacuate motor vehicles during a WD, improved car designs and increasing safety profiles, remaining in a motor vehicle may be safer than seeking shelter in a mobile home or in a ditch.[27,35] Taking shelter in a standard constructed home is the safest option, with the basement being the safest location during a tornado and an interior room a reasonable second choice.[25] A single story house may be safer than a multi-story house.[11] Individuals who fail to find cover under solid objects have a higher incidence of injuries, and blankets, mattresses, as well as pillows may offer some protection. It is also believed that stricter anchorage requirements in building codes might mitigate tornado damage and deaths.[25]
DAMAGE TO HEALTHCARE FACILITIES AND INFRASTRUCTURE
In the event where a hospital is damaged or affected by a natural disaster, contingency plans and protocols must always be ready for implementation [Table 4]. A review of recent major natural disasters in United States shows that damage or collapse of a hospital is uncommon. Many of the disaster response protocols were redesigned in the 1970s account for this possibility. Instead, loss of power or water supply is more likely.[16] Although most hospitals in North America are equipped with at least one backup system to provide some functional redundancy even in the worst of scenarios, this does not guarantee that continuity of care can be preserved during a WD, as exemplified by the recent power failure at the New York University (NYU) hospital during Hurricane Sandy.[14,16] The situation may be even more complicated in developing countries, where power failures or even structural damage may be common when disaster strikes. In many cases, hospitals and clinics have received no additional disaster protection over the rest of the community, leaving the area at risk during a major catastrophe.[36] A natural disaster may also damage other emergency resources such as roads, vehicles, and aircraft. This is most disruptive in the early stages of the rescue operation, as many victims require transportation to medical centers. Studies show that in large-scale disasters, in the absence of ambulances, many victims are often brought to medical centers in taxis and private vehicles.[36]
Of note, patients and visitors in hospitals and other structures at risk for severe damage and flooding may require evacuation. Obviously, this is most effective when accomplished in the preparation phase of an approaching storm but may also continue throughout the post-impact stage. This often necessitates a significant number of personnel and equipment and is facilitated by a well-rehearsed evacuation plan with contingency provisions for escape routes and supplies. Lessons learned from Hurricane Sandy also include raising the placement of generators out of basements and low-lying areas as well as appropriate positioning of fuel and pumps above flood levels.[37]
In the wake of recent Hurricane Sandy, many healthcare entities are still reeling as they attempt to become functional once again. At the time of this writing, several weeks after the hurricane, three New York City hospitals remain closed and are struggling to progress toward restoring daily operation.[38] Initial estimates of healthcare-specific damages in New York alone were as high as $3.1 billion.[39]
The extensive damage incurred by medical facilities following WD's can greatly impact a health care system and those it serves. Following Hurricane Katrina, the Federal Emergency Management Agency (FEMA) was reorganized, including substantial new authority to remedy gaps that became apparent following the most devastating natural disaster in United States history.[40] Two grant programs exist within FEMA to assist communities in mitigating the effects of wind hazards - the Hazard Mitigation Grant Program and the Pre-Disaster Mitigation Competitive Grant Program. Government agencies may apply through States to receive funding from these programs. With their aid, hospitals have managed to cope with WDs by maintaining functionality and improving preparedness.[41]
While it is important to repair existing facilities and to resume full-operational status, an equally important goal is to limit potential damage from future WDs by implementing new strategies. This is usually done by retrofitting facilities to protect building integrity or by adding safe rooms to existing facilities to help reduce injuries and mortality from wind or wind-borne debris.[42] For example, Memorial Hospital Gulfport replaced their roof with a membrane structure that includes a cap sheet and replaced windows with a resin anodized aluminum substance for less vulnerability to breakage.[43] West Jefferson, one of the three hospitals that remained open in New Orleans, is working on securing a water line from the utility or establishing a deep well on hospital grounds. They are also working on a new power plant that can address power supply issues in the event of another hurricane.[44]
DESTRUCTION OF STORAGE FACILITIES AND LOSS OF SUPPLIES
Just as hospitals and emergency vehicles are easily damaged or destroyed by natural disasters, so are medical supply depots and storage facilities. The damage or destruction of essential medical stores carrying medications, dressings, intravenous lines and other supplies can compound an already desperate situation. In the aftermath of any disaster, hospitals and clinics will require additional supplies to accommodate the increase in admissions. The number of victims may overwhelm the resources of the medical system.
The critical infrastructure of a community is vital to both the well-being and public health of its members. Damage to power grids and fuel lines can have far reaching consequences. As exemplified in the severe winter storm that hit the eastern United States and Canada in 1998, as well as during the aftermath of Hurricane Sandy, an extended disruption in power delivery can leave homeowners vulnerable to the extreme cold as well as disrupt most forms of communication.[45,46] A prolonged period of time without power may lead to significant public health issues.
Finally, many communities require an adequate electricity supply in order to properly treat or pump their drinking water. The loss of a potable water supply is one of the most devastating long-term effects from a natural disaster. With an extended power outage, drinking water is at risk of contamination. This circumstance is compounded by the fact that individuals may lack even the ability to boil the water they do receive.[45]
Crucial to maintaining functionality are back-up energy sources, water stores, food and medical supplies, mobile facilities, transportation and communication capabilities, and adequate staffing. Memorial Hospital Gulfport, a 400-bed facility serving the Mississippi Gulf Coast showed both exemplary preparedness and response to Hurricane Katrina. Their response included a back-up energy source of diesel storage tanks that provided 3-4 days of fuel, 4 emergency generators and 3 stand-by generators. Also critical was a hospital-wide power down process which included limiting the number of powered-on CT scanners and unutilized computers.[43] The hospital facility also had access to a well as an alternate water source.
The utility of adequate mobile facilities is highlighted in the story of Sumter Regional Hospital in Georgia, struck by a tornado in March 2007. Assisted by FEMA, a local emergency response center and an urgent-care center were fashioned from tents. The impromptu center functioned as a regional emergency care and an obstetrics suite. Patients not requiring acute medical care were transported via the town's four ambulances to other regional medical centers.[47]
Communication is critical to patient care, transportation, and maintaining functionality across facilities. Hurricane-response preparedness for healthcare institutions must incorporate a strategy to ensure communication among workers, realizing that usual communication methods may be unavailable for some time.[44] Coping with damage and loss to facilities is certainly not a one-time event. Rather, it is a progressive and ongoing, multidisciplinary process only possible thanks to the dedication of administration, physicians, nursing staff, mechanics, engineers, technical support, and area volunteers. Additionally, it is crucial to maintain good relationships with distributors and contractors outside the area as well as various professional societies.[47]
IMPACT OF WIND DISASTERS ON HEALTHCARE COSTS
WDs can have a significant impact on the delivery and cost of healthcare in the affected geographic region. These costs may be immediate, intermediate, or long-term, and some may result indirectly from the effects of the disaster. As demonstrated by the recent Hurricane Sandy, immediate damage to hospital structures, equipment, and access routes can carry significant associated monetary costs.[48] The subsequent sections briefly discuss important considerations regarding the impact of WDs on healthcare costs.
Immediate healthcare costs
The immediate costs of WDs include the cost of property destruction, economic loss, as well as the immediate disaster relief. Injuries to victims and rescue personnel consume vast amounts of material and human resources, and loss of infrastructure can be overwhelming. After Hurricane Katrina, approximately 80% of the hospital beds in New Orleans (50% in the city and surrounding parishes combined), the only Level 1 Trauma facility, and 75% of the safety net community clinics remained closed.[49] Likewise, the 2012 Hurricane Sandy inflicted damage to many New York and New Jersey hospitals, forcing patient evacuations and imposing massive financial burden.[37,38] Some of the direct costs of these disasters can be readily calculated, such as the supplies and materials used to directly treat injuries to those involved, whether initial victims or rescue workers. Other costs become more difficult to determine, such as depreciation on equipment used during relief efforts, or even the cost of rescue personnel.
Intermediate healthcare costs
After the immediate relief efforts subside, attention turns to the rebuilding of the health care infrastructure. Infrastructure needs in most severely affected areas may actually decrease, as many victims displaced by the disaster may permanently relocate (i.e., post-Hurricane Katrina)[50] Of course, such displacement can represent “expenditure shift” of the healthcare costs outside of the immediately affected area rather than a true decrease in costs. Another question that arises is whether it is better to repair damaged infrastructure, or to completely rebuild facilities to reflect the needs of state-of-the-art health care. Louisiana State University (LSU) estimated the repair costs for University and Charity Hospitals to be $117.4 and $257.7 million, respectively, far greater than the FEMA estimate of $12.4 and $23.9 million, in part because LSU's estimate included correcting some preexisting deficiencies.[50] Because federal funding would only allow replacement of the facility if repair costs exceed 50% of the total facility value, alternative funding was required for the difference between the federal aid for repair and the replacement costs. Uncertainty in funding may affect difficulty with staff retention and attraction of displaced staff back to the community, creating long-term implications for the local availability of healthcare. Healthcare facilities’ revenues may be significantly altered by the relocation of providers, the shift from outpatient to inpatient care, and the increase in the proportion of uninsured patients.[51]
Healthcare systems can ameliorate the effects of disasters by using Electronic Health Records (EHR) and appropriate disaster recovery plans to speed the patients’ ability to receive appropriate care by allowing the access to records remotely, as seen after the Joplin, Missouri tornado in 2011.[52] EHR's have also been used to maintain continuity of care for Veteran's Administration patients after the 2005 Gulf storms.[53]
Victims of WD's may experience exacerbations of existing medical conditions or develop new medical conditions related to lack of supplies, temporary or damaged housing, and reduced healthcare access. At times, respiratory conditions such as allergies and asthma can be aggravated after WDs. This appears limited to individuals with pre-existing asthma or reactive airway conditions, including rescue/recovery workers.[54] Routine health maintenance can be disrupted with long-term consequences such as increased total health care costs, reduced life expectancy, and reduced quality-adjusted life expectancy. Worsened diabetes care has been estimated to increase health care costs in University and Charity Hospital patients post-Katrina by estimated $504 million.[55] Weeks to months after a disaster, victims may suffer from various psychological disorders, including PTSD or general anxiety disorder.[56] When compared to general population, survivors of Hurricane Katrina were approximately 10 times more likely to develop PTSD.[57] Similarly worrisome trends have been reported among typhoon survivors.[58] Symptoms may include night terrors, sudden phobias, grief, depression, guilt, insomnia, loss of appetite or flashbacks, and hallucinations.[59] Psychological recovery is dependent upon the timely recognition of symptoms and the availability of appropriate support. Generally, the severity of psychological conditions is directly dependent on the magnitude of the disaster and the community's ability to cope and recover. Handling the increased mental health needs of persons affected by Hurricanes Rita and Katrina has been estimated at $12.5 billion.[60]
Long-term healthcare costs
Changes in the long term healthcare infrastructure can have a significant impact on the population. Permanent closure of hospitals and the move of healthcare personnel out of the area diminish the availability of health care in the region. In 2010, 48% of physicians, who graduated from residency programs, were practicing in the state where they were trained.[61] Consequently, even temporary relocations of resident physicians in midst of their training may lead to long term health care shortages in the storm-affected area. Long-term stability of the physician training may be threatened by the decrease in available hospital beds and patients needed to satisfy accreditation and training requirements. The number of physicians in the New Orleans area declined by almost 75% after Katrina.[62]
Long-term changes in hurricane victims’ patterns of healthcare use may also be seen, necessitating changes in the support systems used to provide care.[63] Chronic stress can lead to medication and therapeutic noncompliance, and the changes in the healthcare environment can lead to increased incidence of acute myocardial infarction.[64] While it is difficult to ascertain precise costs to society due to increased hospitalizations from cardiac disease and lost productivity, it is clear that this has a long-term economic impact. Similarly, death rates in New Orleans were reported to be higher in the months after Hurricane Katrina, and mental health needs also increased, both contributing to long-term decreases in productivity of the populace.[65]
WDs AND MEDICAL/SURGICAL INTERVENTION
WDs can produce overwhelming medical circumstances, not only for the victims, but also for the providers of care, and governments at large. The provision of perioperative care encompasses the Emergency Department Services (ED), Anesthesiology, Surgery and Critical Care services, as well as primary care services. While scenarios may vary, the intervention of medical teams seems to fall into two broad categories, (i) insertion of a team into a situation in which they must provide all care, typically in areas with marginal medical service infrastructure, and (ii) interventions that occur as a team is inserted and provides ED services, triage and general medical care with anesthesiology, surgical services, and critical care services outside of the immediate area of insertion. There are also two subgroups associated with each category, (a) short-term support (days to weeks), and (b) long term support (months). Medical teams inserted into such an environment must realize they will initially see acute trauma, soon to be followed by treatment of chronic illnesses. Furthermore, there may be a surge of pediatric and obstetrical patients for which the medical teams must prepare.
While much of our knowledge regarding medical support for natural disasters comes from earthquake support[66,67,68,69,70] and the general military experience,[71,72,73] there have been recent experiences with hurricanes Andrew, Katrina, tropical storms (such as Allison in Texas), and various tornados which have added to our knowledge of WD medical support. National taskforces have come together and produced recommendations for mass disasters, but much of these supportive recommendations have been in response to the potential of bioterrorism or viral/influenza pandemics.[74,75,76,77,78]
The Israeli Defense Force's (IDF) response to the Haitian Earthquake of 2010 provides an example of a well-prepared medical system that can travel rapidly and provide excellent, self-contained disaster care. Within 90 hours of the event, the IDF traveled 6,000 miles and set up a fully operational hospital within 8 hours of arrival. This consisted of a full pharmacy and a fully functioning laboratory (chemistry, urine, hematology, arterial blood gases, and microbiology with autoclaves). They also carried tents, latrines, and generators, along with 109 personnel, including “computer and communication specialists, security staff, kitchen staff, carpenters, plumbers, mechanics, and a burial team”,[69] as well as necessary medical personnel, operating rooms, and intensive care beds. They had a choice before departure from Israel to choose a “light” primary care hospital or a “sophisticated” hospital. Sophistication was chosen because of the IDF experience in China (1976), Armenia (1988), and Japan (1995). Trauma accounted for 66% of their injuries, and 63% of all patients were hospitalized. Orthopedic surgery was the most prominent specialty, running 3-4 operating rooms around the clock. The IDF emphasizes the concept of ‘surge capacity’ and its importance to effective intervention when medical capabilities are overwhelmed. Within 48 hours, the IDF was at full capacity and could only care for a new patient if another was discharged. Similar experience has been reported in the 1988 Armenian earthquake,[66] the 1999 earthquake in Duzce, Turkey,[67] and the 2003 earthquake in Bam, Iran.[68]
While most of the IDF experience comes from earthquakes, Noji's review of anticipated injury patterns in five tropical cyclones (Tracy 1974, David 1979, Frederic 1984, Elena 1988, and Hugo 1989) confirms that almost two-thirds of injuries affected the lower limb, and hand injuries were next in frequency, many of which occurred after the initial disaster and during the clean-up phase.[79] This epidemiological pattern of injury makes many WD scenarios similar to those of earthquakes, allowing us to use the experiences for educational and preparation purposes.
In contrast to the disasters described above, in which infrastructure was eliminated, Alson et al., provide a commentary on Hurricane Andrew (1992), and describe the typical intervention of a volunteer, civilian special operations response team in an area in which much of the infrastructure remained intact.[5] During Andrew, the medical response teams provided general care, and most of the trauma occurred during the restoration and clean-up activities. The United States Air Force (USAF), on the other hand, needed to respond to the unexpectedly severe Tropical Storm Allison in June 2001 and brought a military model to a civilian scenario in Houston, Texas, with medical infrastructure severely damaged.[80] The USAF inserted a 25-bed expeditionary hospital, arrived onsite within hours, and closely collaborated with Disaster Medical Assistance Teams (DMAT) from Oklahoma and New Mexico. The DMAT provided only primary care, the mission to allow off-loading of the surrounding ED and to allow the more serious trauma cases to be treated at the remaining level I trauma center.[5] The USAF determined that they would have to treat 175 patients per 24 hours (maximum) and that such a pace would require troops to be rotated every two weeks. Multiple important lessons were learned in Houston: (a) Command/control functions were hampered because the military unit was housed at two different locations; (b) there was a need for a public affairs officer to effectively interact with the press; (c) military transports worked well, but civilian trucking contractors were unreliable; (d) this unit was effective for surgical needs but had a shortage of medications for chronic diseases; (e) many laboratory supplies were perishable; and (f) more “robust” radiology package was needed.[80] Surge capacity caused rapid increases in demand for medical treatment at levels for which they were not initially prepared, prompting further infrastructure development toward efficiency of insertion and deployment of medical personnel at surge capacity.
WDs at their worst will cause the civilian or military teams to work in an austere environment.[71] Such disasters essentially simulate the military field environment, and the recent wars in the Middle East offer some parallels with regards to WDs, from the most basic to the more sophisticated elements of care.[73,81] Several important points that have been learned from recent military experience should be emphasized in the provision of critical care in the austere environment in civilian catastrophes.[72] The first is the importance of an effective aeromedical evacuation system with critical care capabilities. This not only was effective in the Middle East conflicts[82] but also during Hurricane Katrina. Also, logistical components such as oxygen, power, climate control, communication, sanitation, food, water, and lodging require attention. Special emphasis, however, should be placed on oxygen, as its necessity is a significant burden in the field and conservation is of paramount importance.[72] Third, although triage is an important and dynamic life-saving process, its ethical considerations frequently provide dilemmas in the field.[83] In the realm of laboratory and monitoring capabilities, capnography is highly desired, i- STAT® (Abbott Point of Care, Abbott Laboratories, Abbott Park, Illinois, USA) portable point-of-care laboratory analyzers are valuable, and ultrasound has a growing role.[81,84]
A mention of the practice of anesthesiology should be made at this juncture.[85] When providing surgical services in the field during a catastrophe, forward-deployed anesthesia services are forced to work with limited electrical support and little or no compressed gas sources. The portable drawover vaporizer is the device of choice according to the U.S. military [Figure 1a]. It can function without electricity or a compressed gas source. When electricity is available and the need for a ventilator is evident, portable low-profile ventilators can be used with the drawover vaporizer, with or without compressed gas [Figure 1b]. When general anesthesia is not possible, total intravenous and regional approaches have been applied successfully in disaster scenarios.
Figure 1.

An example of a portable drawover vaporizer (Left) similar to devices used by military organizations. Such devices can function without electricity or a compressed gas source. When electricity is available and formal ventilator support is needed, a portable mechanical ventilator (Right) can be used with the drawover vaporizer. Such portable ventilators can be used with or without compressed gas
In the austere environment of a WD, recent experience has shown that sophisticated critical care with available portable technologies can be provided.[81,86] Rather than associate the equipment and technology with critical care, intensive care should imply the vigilant attention of a skilled multi-disciplinary team.[71] Some examples of portable equipment use in austere/disaster settings include the hand-held ultrasound for injury and intravascular volume assessment[81,87] or advanced hemodynamic monitoring using the esophageal Doppler probe.[86] Preparation, anticipation, and vigilance are mandatory in all aspects of WD management.
TRANSPORTING VICTIMS/PATIENTS
Disruption of transportation routes often interferes with the initial medical emergency response. For example, hurricanes and associated flooding can render roads, bridges, tunnels, and telephone lines out of service.[16] Hurricanes, cyclones, or tornados can also “ground” rescue helicopters and other aircraft. Just as emergency vehicles are prevented from reaching critically ill victims, patients in private vehicles may also be prevented from reaching hospitals and clinics.
Upon arrival to the affected area, first responders must assess the scene and determine if hazards are present. Power outages, downed electrical lines, and obstructing debris are commonplace and may hinder rescue and transportation efforts. Specific hazards associated with working in WD areas include: (a) Hazardous driving conditions; (b) falls due to slippery walkways; (c) falling/flying objects such as tree limbs and utility poles; (d) electrical hazards from power lines or objects in contact with fallen power lines; (e) burns from fires caused by energized line contact; or (f) equipment failure.[88]
The principles of patient transportation during WDs are similar to those used in other natural disasters. Initial field triage establishes the patient's condition and medical needs. Critical patients should be transported first, and the urgency of medical transport is dictated by first responders. In the setting of threat to life or limb, the level of urgency is designated as “urgent and needing immediate evacuation”. Otherwise, a patient can be designated non-urgent, and evacuation can be postponed.[89] This selection must be based on the assessment of a patient's injuries, the available hospital's capabilities and capacities, and the system's available resources. For those that are severely injured, transportation to a designated trauma center is recommended. Good communication with the receiving facility is important to prevent overwhelming the facility. In large-scale disasters, it may be necessary to transport patients to hospitals in a wider area.[90]
While evaluating a patient for transport, basic life-support care should be given. This includes stabilization of airway, breathing, and circulation parameters. Injured patients should be placed in spinal precautions prior to transport. During transportation, measures to alleviate pain and prevent hypothermia should be taken. Communication with the receiving facility should include: (a) Brief history of the injury; (b) current status of the patient including vital signs, physical exam, pertinent history, any treatment rendered, and any updates or developments en route; and (c) mode of transport, destination, and estimated time of arrival.[91]
CONCLUSION
WDs have a multitude of deleterious effects on a community. In order to assess the impact of WDs on the healthcare of the affected populace, considerations must include more than just immediate relief efforts. Long-term changes in the physical and mental health of the populace, coupled with changes in healthcare infrastructure lead to significant and lasting financial and quality of life consequences. Following major WDs, the impact of these events may continue for decades and may arguably be demonstrated for generations to come. The devastation that accompanies such events may be ameliorated by aggressive preparation and response during the impact phase, expeditious clean-up, treatment, and restoration of local infrastructure and public health measures, as well as appropriate subsequent interventions based on lessons learned from each disaster.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Stephani J. Power Outages, Flooding Persist as Sandy Tracks North. 2012. [Last cited on 2012 Nov 17]. Available from: http://www.insurancenetworking.com/news/power-outages-flooding-persist-as-sandy-tracks-north-31277-1.html .
- 2.Verbout SM. Tornado outbreaks associated with land-falling tropical cyclones in the Atlantic Basin. 6th Conference on Coastal Atmospheric and Oceanic Prediction and Processes. 2005 [Google Scholar]
- 3.Kunkel KE, Pielke RA, Changnon SA. Temporal fluctuations in weather and climate extremes that cause economic and human health impacts: A review. Bull Am Met Soc. 1999;80:1077–98. [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Morbidity and mortality associated with Hurricane Floyd-North Carolina, September-October 1999. MMWR Morb Mortal Wkly Rep. 2000;49:369–72. [PubMed] [Google Scholar]
- 5.Alson R, Alexander D, Leonard RB, Stringer LW. Analysis of medical treatment at a field hospital following Hurricane Andrew, 1992. Ann Emerg Med. 1993;22:1721–8. doi: 10.1016/s0196-0644(05)81312-5. [DOI] [PubMed] [Google Scholar]
- 6.Bissell RA, Becker BM, Burkle FM., Jr Health care personnel in disaster response. Reversible roles or territorial imperatives? Emerg Med Clin North Am. 1996;14:267–88. doi: 10.1016/s0733-8627(05)70251-0. [DOI] [PubMed] [Google Scholar]
- 7.Peterson CJ. Catastrophic wind damage to North American forests and the potential impact of climate change. Sci Total Environ. 2000;262:287–311. doi: 10.1016/s0048-9697(00)00529-5. [DOI] [PubMed] [Google Scholar]
- 8.Gresham CA, Williams TM, Lipscomb DJ. Hurricane Hugo wind damage to southeastern United-States coastal forest tree species. Biotropica. 1991;23:420–6. [Google Scholar]
- 9.Schwanitz L. Hospitals, employees face devastating losses in aftermath of Hurricane Andrew. OR Manager. 1992;8(1):21–2. [PubMed] [Google Scholar]
- 10.Hogan DE, Askins DC, Osburn AE. The May 3, 1999, tornado in Oklahoma City. Ann Emerg Med. 1999;34:225–6. doi: 10.1016/s0196-0644(99)70235-0. [DOI] [PubMed] [Google Scholar]
- 11.Bohonos JJ, Hogan DE. The medical impact of tornadoes in North America. J Emerg Med. 1999;17:67–73. doi: 10.1016/s0736-4679(98)00125-5. [DOI] [PubMed] [Google Scholar]
- 12.Millie M, Senkowski C, Stuart L, Davis F, Ochsner G, Boyd C. Tornado disaster in rural Georgia: Triage response, injury patterns, lessons learned. Am Surg. 2000;66:223–8. [PubMed] [Google Scholar]
- 13.Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: The dynamics of disaster, disease, and development. Epidemiol Rev. 2005;27:21–35. doi: 10.1093/epirev/mxi011. [DOI] [PubMed] [Google Scholar]
- 14.Brunkard J, Namulanda G, Ratard R. Hurricane Katrina deaths, Louisiana, 2005. Disaster Med Public Health Prep. 2008;2:215–23. doi: 10.1097/DMP.0b013e31818aaf55. [DOI] [PubMed] [Google Scholar]
- 15.Shen J, Feng Z, Zeng G, Zhu BP. Risk factors for injury during Typhoon Saomei. Epidemiology. 2009;20:892–5. doi: 10.1097/EDE.0b013e3181bb552f. [DOI] [PubMed] [Google Scholar]
- 16.Pearson C, Young J. NYU hospital evacuated after generator failure, patients at other nyc hospitals relocated (Update) 2012. [Last cited on 2012 Nov 17]. Available from: http://www.huffingtonpost.com/2012/10/30/nyu-hospital-evacuation-sandy_n_2043922.html .
- 17.McLaughlin KA, Fairbank JA, Gruber MJ, Jones RT, Lakoma MD, Pfefferbaum B. Serious emotional disturbance among youths exposed to Hurricane Katrina 2 years postdisaster. J Am Acad Child Adolesc Psychiatry. 2009;48:1069–78. doi: 10.1097/CHI.0b013e3181b76697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rugaber CS, Crutsinger M. Hurricane Sandy Estimated to Cost $60 Billion. 2012. [Last cited on 2012 Nov 17]. Available from: http://business.time.com/2012/10/31/hurricane-sandy-estimated-to-cost-60-billion .
- 19.Dow K, Cutter SL. Crying wolf: Repeat responses to hurricane evacuation orders. Coastal Management. 1998;26:237–52. [Google Scholar]
- 20.Grabowski JG, Simmons JD, Eichelberger MR. Preventing unintentional pediatric injuries at evacuation centers. J Trauma. 2009;67(Suppl 2):S94–5. doi: 10.1097/TA.0b013e3181ac81c9. [DOI] [PubMed] [Google Scholar]
- 21.Paul BK. Human injuries caused by Bangladesh's cyclone Sidr: An empirical study. Natural Hazards. 2010;54:483–95. [Google Scholar]
- 22.Keller J. Mapping Hurricane Sandy's Deadly Toll. 2012. [Last cited on 2012 Nov 17]. Available from: http://www.nytimes.com/interactive/2012/11/17/nyregion/hurricane-sandy-map.html .
- 23.Kates RW, Colten CE, Laska S, Leatherman SP. Reconstruction of New Orleans after Hurricane Katrina: A research perspective. Proc Natl Acad Sci USA. 2006;103:14653–60. doi: 10.1073/pnas.0605726103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drewniak M, Roberts K. Christie administration urges precautions on use of alternative heating devices during extended power outages. 2012. [Last cited on 2012 Nov 17]. Available from: http://nj.gov/governor/news/news/552012/approved/20121105c.html .
- 25.Carter AO, Millson ME, Allen DE. Epidemiologic study of deaths and injuries due to tornadoes. Am J Epidemiol. 1989;130:1209–18. doi: 10.1093/oxfordjournals.aje.a115449. [DOI] [PubMed] [Google Scholar]
- 26.Schmidlin TW, King PS. Risk factors for death in the 27 March 1994 Georgia and Alabama tornadoes. Disasters. 1995;19:170–7. doi: 10.1111/j.1467-7717.1995.tb00367.x. [DOI] [PubMed] [Google Scholar]
- 27.Daley WR, Brown S, Archer P, Kruger E, Jordan F, Batts D, et al. Risk of tornado-related death and injury in Oklahoma, May 3, 1999. Am J Epidemiol. 2005;161:1144–50. doi: 10.1093/aje/kwi142. [DOI] [PubMed] [Google Scholar]
- 28.Mcconnell C. Coping with natural disasters: The role of local health personnel and the community-WHO. Disasters. 1989;13:376–7. [Google Scholar]
- 29.Seaman J. Manual for disaster relief work-Skeet M. Disasters. 1977;1:333–4. [Google Scholar]
- 30.Bulle WF. Epidemiology of natural disasters-Seaman J. Disasters. 1984;8:234–5. [Google Scholar]
- 31.Maugh II, Thomas H. Lethal fungus adds to tornado woes in Joplin. 2012. [Last cited on 2012 Nov 18]. Available from: http://articles.latimes.com/2011/jun/11/health/la-he-joplin-fungus-20110611 .
- 32.CNN. Rare fungal infection strikes Joplin tornado victims. 2011. [Last cited on 2012 Nov 18]. Available from: http://www.cnn.com/2011/US/06/10/missouri.joplin.fungus/index.html .
- 33.Dopp T. Christie orders New Jersey's Barrier Islands, casinos evacuated. 2012. [Last cited on 2012 Nov 18]. Available from: http://www.bloomberg.com/news/2012-10-27/christie-orders-new-jersey-s-barrier-islands-casinos-evacuated.html .
- 34.OEM. NYC hazards: Hurricane sheltering. 2012. [Last cited on 2012 Nov 18]. Available from: http://www.nyc.gov/html/oem/html/hazards/storms_sheltering.shtml .
- 35.Noji EK, Sivertson KT. Injury prevention in natural disasters: A theoretical framework. Disasters. 1987;11:290–6. [Google Scholar]
- 36.Arnold JL, Corte DF. International emergency medicine: Recent trends and future challenges. Eur J Emerg Med. 2003;10:180–8. doi: 10.1097/00063110-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Goodman JD, Moynihan C. Patients evacuated from city medical center after power failure. 2012. [Last cited on 2012 Nov 16]. Available from: http://www.nytimes.com/2012/10/30/nyregion/patients-evacuated-from-nyu-langone-after-power-failure.html .
- 38.Dolan J. New York News: 3 New York City hospitals remain closed after Sandy. 2012. [Last cited on 2012 Nov 17]. Available from: http://abclocal.go.com/wabc/story?section=news/local/new_york and id=8884597 .
- 39.Cheung-Larivee K. Hurricane Sandy costs New York $3.1 B in healthcare damages. 2012. [Last cited on 2012 Dec 5]. Available from: http://www.fiercehealthcare.com/story/hurricane-sandy-costs-new-york-31b-healthcare-damages/2012-11-29 .
- 40.FEMA. Confined space medicine. 2001. [Last accessed on 2012 March 7]. Available from: http://www.fema.gov/pdf/emergency/usr/unit5.pdf .
- 41.FEMA. Federal Emergency Management Agency. 2012. [Last cited on 2012 Feb 16]. Available from: http://www.fema.gov .
- 42.Washington, DC: Department of Homeland Security/Federal Emergency Management Agency; 2006. FEMA. Procedures for developing scopes of work for wind retrofit projects. [Google Scholar]
- 43.VHA. VHA Foundation. 2012. [Last cited on 2012 Feb 16]. Available from: https://www.vhafoundation.org/DisasterRelief/Pages/Default.aspx .
- 44.Hounsell D. Hospitals serve as ports in a storm. 2005. [Last cited on 2012 Feb 16]. Available from: http://www.facilitiesnet.com/emergencypreparedness/article/Ports-in-a-Storm-3546# .
- 45.The ice storm of the century: How affected hospitals and communities dealt with the challenges of a unique, prolonged emergency. Hosp Secur Saf Manage. 1998;18:5–9. [PubMed] [Google Scholar]
- 46.Stebner B, Warren L. Even FEMA offices shut ‘due to bad weather’ after snow storm batters Sandy victims and leaves thousands stranded and without power. 2012. [Last cited on 2012 Nov 18]. Available from: http://www.dailymail.co.uk/news/article-2229316/East-Coast-fresh-chaos-thousands-stranded-power-Sandy-victims-hit-snow-storm.html .
- 47.Newman R. The Sumpter tornado: Their hospital in ruins, Georgia hospitalists aid in recovery. The Hospitalist. 2007;11:1–4. [Google Scholar]
- 48.Hartocollis A. A flooded mess that was a medical gem. 2012. [Last cited on 2012 Nov 16]. Available from: http://www.nytimes.com/2012/11/10/nyregion/damage-from-hurricane-sandy-could-cost-nyu-langone-millions.html?_r=0 .
- 49.Washington DC: United States Government Accountability Office; 2006. GAO. Hurricane Katrina: Status of the health care system in New Orleans and difficult decisions related to efforts to rebuild it approximately 6 months after Hurricane Katrina, U.S.G.A. Office. [Google Scholar]
- 50.Schneider A, Rousseau D. Washington DC: The kaiser commission on medicaid and the uninsured; 2005. Addressing the health care impact of Hurricane Katrina, T.H.J.K.F. Foundation. [Google Scholar]
- 51.Breaux JA, French M, Richardson WS. Effect of natural disaster on routine surgery. J Am Coll Surg. 2009;209:352–5. doi: 10.1016/j.jamcollsurg.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Washington DC: U. S. Department of Health and Human Services; 2012. HHS. The tornado and a patient's Electronic Health Record (EHR), U.S.Do.Ha.H. Services. [Google Scholar]
- 53.Brown SH, Fischetti LF, Graham G, Bates J, Lancaster AE, McDaniel D, et al. Use of electronic health records in disaster response: The experience of Department of Veterans Affairs after Hurricane Katrina. Am J Public Health. 2007;97(Suppl 1):S136–41. doi: 10.2105/AJPH.2006.104943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bernstein RS, Baxter PJ, Falk H, Ing R, Foster L, Frost F, et al. Immediate public health concerns and actions in volcanic eruptions: Lessons from the Mount St. Helens eruptions, May 18-October 18, 1980. Am J Public Health. 1986;76(Suppl 3):25–37. doi: 10.2105/ajph.76.suppl.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, et al. Impact of a natural disaster on diabetes: Exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32:1632–8. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greenough G, McGeehin M, Bernard SM, Trtanj J, Riad J, Engelberg D. The potential impacts of climate variability and change on health impacts of extreme weather events in the United States. Environ Health Perspect. 2001;109(Suppl 2):191–8. doi: 10.1289/ehp.109-1240666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mills MA, Edmondson D, Park CL. Trauma and stress response among Hurricane Katrina evacuees. Am J Public Health. 2007;97(Suppl 1):S116–23. doi: 10.2105/AJPH.2006.086678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, et al. Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. J Trauma Stress. 2009;22:180–8. doi: 10.1002/jts.20404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ngo EB. When disasters and age collide: Reviewing vulnerability of the elderly. Nat Hazards Rev. 2001;2:80–9. [Google Scholar]
- 60.Schoenbaum M, Butler B, Kataoka S, Norquist G, Springgate B, Sullivan G, et al. Promoting mental health recovery after hurricanes Katrina and Rita: What can be done at what cost. Arch Gen Psychiatry. 2009;66:906–14. doi: 10.1001/archgenpsychiatry.2009.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Washington DC: AAMC; 2011. AAMC. 2011 State Physician Workforce Data Book, A.o.A.M. Colleges. [Google Scholar]
- 62.Rudowitz R, Rowland D, Shartzer A. Health care in New Orleans before and after Hurricane Katrina. Health Aff (Millwood) 2006;25:w393–406. doi: 10.1377/hlthaff.25.w393. [DOI] [PubMed] [Google Scholar]
- 63.Domino ME, Fried B, Moon Y, Olinick J, Yoon J. Disasters and the public health safety net: Hurricane Floyd hits the North Carolina Medicaid program. Am J Public Health. 2003;93:1122–7. doi: 10.2105/ajph.93.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gautam S, Menachem J, Srivastav SK, Delafontaine P, Irimpen A. Effect of Hurricane Katrina on the incidence of acute coronary syndrome at a primary angioplasty center in New Orleans. Disaster Med Public Health Prep. 2009;3:144–50. doi: 10.1097/DMP.0b013e3181b9db91. [DOI] [PubMed] [Google Scholar]
- 65.Weisler RH, Barbee JG, 4th, Townsend MH. Mental health and recovery in the Gulf Coast after Hurricanes Katrina and Rita. JAMA. 2006;296:585–8. doi: 10.1001/jama.296.5.585. [DOI] [PubMed] [Google Scholar]
- 66.Pesola G, Bayshtok V, Kvetan V. American critical care team at a foreign disaster site: The Armenian experience. Crit Care Med. 1989;17:582–5. doi: 10.1097/00003246-198906000-00021. [DOI] [PubMed] [Google Scholar]
- 67.Bar-Dayan Y, Leiba A, Beard P, Mankuta D, Engelhart D, Beer Y, et al. A multidisciplinary field hospital as a substitute for medical hospital care in the aftermath of an earthquake: The experience of the Israeli Defense Forces Field Hospital in Duzce, Turkey, 1999. Prehosp Disaster Med. 2005;20:103–6. doi: 10.1017/s1049023x00002272. [DOI] [PubMed] [Google Scholar]
- 68.Owens PJ, Forgione A, Jr, Briggs S. Challenges of international disaster relief: Use of a deployable rapid assembly shelter and surgical hospital. Disaster Manag Response. 2005;3:11–6. doi: 10.1016/j.dmr.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 69.Kreiss Y, Merin O, Peleg K, Levy G, Vinker S, Sagi R, et al. Early disaster response in Haiti: The Israeli field hospital experience. Ann Intern Med. 2010;153:45–8. doi: 10.7326/0003-4819-153-1-201007060-00253. [DOI] [PubMed] [Google Scholar]
- 70.Halpern P, Rosen B, Carasso S, Sorkine P, Wolf Y, Benedek P, et al. Intensive care in a field hospital in an urban disaster area: Lessons from the August 1999 earthquake in Turkey. Crit Care Med. 2003;31:1410–4. doi: 10.1097/01.CCM.0000059439.07851.BD. [DOI] [PubMed] [Google Scholar]
- 71.Grathwohl KW, Venticinque SG. Organizational characteristics of the austere intensive care unit: The evolution of military trauma and critical care medicine; applications for civilian medical care systems. Crit Care Med. 2008;36(Suppl 7):S275–83. doi: 10.1097/CCM.0b013e31817da825. [DOI] [PubMed] [Google Scholar]
- 72.Venticinque SG, Grathwohl KW. Critical care in the austere environment: Providing exceptional care in unusual places. Crit Care Med. 2008;36(Suppl 7):S284–92. doi: 10.1097/CCM.0b013e31817da8ec. [DOI] [PubMed] [Google Scholar]
- 73.Grathwohl KW, Venticinque SG, Blackbourne LH, Jenkins DH. The evolution of military trauma and critical care medicine: Applications for civilian medical care systems. Crit Care Med. 2008;36(Suppl 7):S253–4. doi: 10.1097/CCM.0b013e31817e325a. [DOI] [PubMed] [Google Scholar]
- 74.Devereaux AV, Dichter JR, Christian MD, Dubler NN, Sandrock CE, Hick JL, et al. Definitive care for the critically ill during a disaster: A framework for allocation of scarce resources in mass critical care: From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(Suppl 5):51S–66. doi: 10.1378/chest.07-2693. [DOI] [PubMed] [Google Scholar]
- 75.Rubinson L, Hick JL, Curtis JR, Branson RD, Burns S, Christian MD, et al. Definitive care for the critically ill during a disaster: Medical resources for surge capacity: From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(Suppl 5):32S–50. doi: 10.1378/chest.07-2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rubinson L, Hick JL, Hanfling DG, Devereaux AV, Dichter JR, Christian MD, et al. Definitive care for the critically ill during a disaster: A framework for optimizing critical care surge capacity: From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(Suppl 5):18S–31S. doi: 10.1378/chest.07-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Christian MD, Devereaux AV, Dichter JR, Geiling JA, Rubinson L. Definitive care for the critically ill during a disaster: Current capabilities and limitations: From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(Suppl 5):8S–17S. doi: 10.1378/chest.07-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Devereaux A, Christian MD, Dichter JR, Geiling JA, Rubinson L. Task Force for Mass Critical Care. Summary of suggestions from the Task Force for Mass Critical Care summit, January 26-27, 2007. Chest. 2008;133(Suppl 5):1S–7. doi: 10.1378/chest.08-0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Noji EK. Analysis of medical needs during disasters caused by tropical cyclones: Anticipated injury patterns. J Trop Med Hyg. 1993;96:370–6. [PubMed] [Google Scholar]
- 80.D’Amore AR, Hardin CK. Air Force expeditionary medical support unit at the Houston floods: Use of a military model in civilian disaster response. Mil Med. 2005;170:103–8. [PubMed] [Google Scholar]
- 81.Stawicki SP, Howard JM, Pryor JP, Bahner DP, Whitmill ML, Dean AJ. Portable ultrasonography in mass casualty incidents: The CAVEAT examination. World J Orthop. 2010;1:10–9. doi: 10.5312/wjo.v1.i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Beninati W, Meyer MT, Carter TE. The critical care air transport program. Crit Care Med. 2008;36(Suppl 7):S370–6. doi: 10.1097/CCM.0b013e31817e3143. [DOI] [PubMed] [Google Scholar]
- 83.Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y. The Israeli field hospital in Haiti-ethical dilemmas in early disaster response. N Engl J Med. 2010;362:e38. doi: 10.1056/NEJMp1001693. [DOI] [PubMed] [Google Scholar]
- 84.Stawicki PS, Braslow B, Gracias VH. Exploring measurement biases associated with esophageal Doppler monitoring in critically ill patients in intensive care unit. Ann Thorac Med. 2007;2:148–53. doi: 10.4103/1817-1737.36548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mongan PD, Via DK. Training the combat anesthesiologist of tomorrow. 2012. [Last cited on 2012 March 2]. Available from: http://www.asahq.org/Kknowledge-Base/Bull-Pen/Academic-Anesthesiologist-of-Tomorrow.aspx .
- 86.Stawicki SP. Use of the esophageal echo-Doppler to guide intensive care unit resuscitations: A retrospective study. Indian J Crit Care Med. 2007;11:54–60. [Google Scholar]
- 87.Stawicki SP, Braslow BM, Panebianco NL, Kirkpatrick JN, Gracias VH, Hayden GE, et al. Intensivist use of hand-carried ultrasonography to measure IVC collapsibility in estimating intravascular volume status: Correlations with CVP. J Am Coll Surg. 2009;209:55–61. doi: 10.1016/j.jamcollsurg.2009.02.062. [DOI] [PubMed] [Google Scholar]
- 88.OSHA. Frequently asked questions for worker safety and health during hurricanes and tornados. 2012. [Last accessed on January 30, 2013]. Available from: http://www.osha.gov/OshDoc/data_Hurricane_Facts/faq_storms.html .
- 89.Ran Y, Hadad E, Daher S, Ganor O, Yegorov Y, Katzenell U, et al. Triage and air evacuation strategy for mass casualty events: A model based on combat experience. Mil Med. 2011;176:647–51. doi: 10.7205/milmed-d-10-00390. [DOI] [PubMed] [Google Scholar]
- 90.Rojavin Y, Seamon MJ, Tripathi RS, Papadimos TJ, Galwankar S, Kman N, et al. Civilian nuclear incidents: An overview of historical, medical, and scientific aspects. J Emerg Trauma Shock. 2011;4:260–72. doi: 10.4103/0974-2700.82219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ingraham D. Trauma triage, transport and transfer guidelines. 2002. [Last accessed on 2013 Jan 31]. Available from: http://dhss.alaska.gov/dph/Emergency/Documents/ems/assets/Downloads/Trauma_Triage_Transport_Transfer_Guide_02.pdf .


