Abstract
Background:
Depression is found to be common among patients with diabetes and it is associated with poor outcomes in disease control. This study was carried out to find out the proportion and determinants associated with depression among patients with established type 2 diabetes mellitus (T2DM) in various tertiary care hospitals in Mangalore city of south India.
Materials and Methods:
This study was conducted in one government and three private tertiary care hospitals in Mangalore in December 2010. All consenting patients with confirmed diagnosis of T2DM were interviewed and screened for depression by administering the 9-item PRIME-MD Patient Health Questionnaire (PHQ-9).
Results:
Of the 230 T2DM patients, 119 (51.7%) were males. The mean age of all participants was 53.61 ± 10.7 years. The median duration of T2DM was found to be 12.1 ± 7.35 years. Among the participants, 71 (30.9%) met the criteria for moderate depression, 33 (14.3%) for severe depression, and the remaining 126 (54.8%) had no clinically significant depression. Only 26 (11.3%) patients were already aware that they were depressed, of whom just 3 had taken medical consultation. Among the risk factors, depression was found to be significantly associated with older age, female gender, low socioeconomic status, unskilled and retired employment status, having complications due to T2DM or comorbidities like hypertension and coronary artery disease, being overweight and being on insulin syringe injections.
Conclusion:
This study found a high proportion of depression among patients with T2DM. Therefore the care of individuals with diabetes mellitus (DM) should include the screening and possible treatment of depression in order to achieve and sustain treatment goals.
Keywords: Depressive disorder, determinants, Diabetes Mellitus Type 2, health care facilities, risk factors
INTRODUCTION
Diabetes is a chronic disease which affects virtually every organ in the human system. The World Health Organization projected that 300 million people will suffer from diabetes by 2025. India has the second largest number of diabetic population in the world and it is expected that there will be 69.9 million diabetic populations in India by 2025.[1]
Depression is common among patients with type 2 diabetes mellitus (T2DM) and it is associated with worst diabetes outcomes.[2,3] Compared with patients with diabetes alone, patients with depression and diabetes have shown poor diligence in maintaining dietary restrictions and exercise, poorer self-management and poor medication adherence.[4,5] Thus they are more likely to suffer from uncontrolled hyperglycemia and complications, thereby resulting in increased health care use and costs, increased disability, lost productivity and higher mortality rates.[6,7]
Having diabetes and depression may also be associated with higher risk of suicide, with some reports of a 10-fold increased risk of suicide and suicidal ideation.[8,9] While depression may contribute to poor diabetes-related outcomes, diabetes and its complications may also contribute to poor depression outcomes.[10,11,12] Depression is still largely unrecognized by physicians managing patients with diabetes mellitus (DM).[13] It is estimated that only one-third of people with both DM and major depression are recognized and appropriately treated for both disorders.[14] The available data regarding the prevalence of depression in T2DM patients in India are limited. Therefore recognition of depression becomes important as cost-effective treatment is available resulting in improvement of diabetic care as well.[15,16] With this background we investigated the proportion of depression and its determinants among patients with T2DM attending various tertiary care hospitals i.e. those with multispecialty inpatient care in Mangalore, a coastal city in south India.
MATERIALS AND METHODS
This cross-sectional study was done in three private hospitals namely Kasturba Medical College Hospital in Attavar, Kasturba Medical College Hospital near Ambedkar circle and Father Muller's Hospital and one government hospital namely Wenlock Hospital during the study period of 1 month in December 2010. Permission to do the study in these hospitals was obtained from the respective medical superintendent of each hospital. Later, all confirmed patients with T2DM visiting outpatient clinic and those admitted in wards were evaluated. The nature and purpose of the study was explained and full confidentiality assured. Written informed consent was subsequently obtained from patients who agreed to participate. The study protocol was approved by the institute's Ethics Committee.
Sample size of 230 was calculated by considering the prevalence of depression to be 41% among T2DM patients from a previously conducted study[17] and keeping the power of the study at 85% with an allowable error of 15%.
Data regarding demographic and socioeconomic factors, clinical details such as duration of illness, modality of treatment and presence of other comorbidities or complications due to DM were collected by interviewing the patient and supplemented from patient records. Socioeconomic status was assessed using modified Kuppuswamy's socioeconomic scale.[18]
Depression was assessed by administering the Kannada (local language) version of PRIME-MD Patient Health Questionnaire (PHQ-9).[19]
It has been validated in Indian population and is considered to be a reliable tool for diagnosis of depression.[20] The PHQ-9 is used to make provisional diagnosis of depressive disorder as well as it provides a severity score for depressive disorder. For the diagnosis of depression, scores of more than 15 were classified as severe depression requiring treatment, scores between 5 and 14 were classified as moderate depression and scores below 5 as patient without clinically significant depression. Therefore a patient obtaining a score of 5 or more was labeled to have depression. Each questionnaire took approximately 35-40 min to fill up.
A PHQ-9 score of 10 or greater has been found to have sensitivity for major depression of 88% and specificity of 88%.[21] The other scales used for diagnosis of depression like International Classification of Diseases - 10 (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) were found to have a sensitivity of 80.5% and 84.8% respectively and a specificity of 78.3% and 67.7%, respectively.[22]
Glycemic control was assessed by recording their HbA1c (non-diabetic reference range of 4.1-6.0%), which is reported to be a reliable indicator of blood glucose level for the last 3 months prior to testing.[23] To determine the glycemic status, HbA1c level was categorized as: a level less than 7% as good glycemic control, 7-8 as fair glycemic control and more than 8% as poor glycemic control.
Standing body height (to the nearest 0.1 cm) was measured with a commercial stadiometer. A digital scale with an accuracy of ±100 g was used to measure body weight. Body mass index (BMI) (kg/m2) was calculated by dividing weight (in kilograms) by the square of height (in meters) as a measure of total adiposity.
Exclusion criteria
Those who had psychiatric problems before diagnosis of diabetes, family history of depression, patients aged below 15 years, type 1 diabetes mellitus patients and seriously ill patients were excluded from the study.
Descriptive statistics were used to summarize the data. Chi-square test and Fisher exact test were used to test the association for categorical variables. The significance level was set at 5%. Results were expressed as odds ratio (OR) and 95% confidence intervals (CI). Cronbach alpha was calculated to assess internal consistency of PHQ-9. All statistical analyses were carried out using Statistical Package for Social Sciences (SSPS) (Version 17.0, USA).
RESULTS
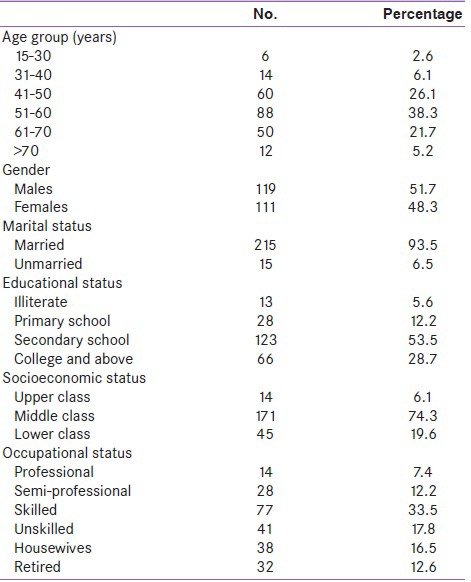
Socio-demographic profile of the study population is shown in Table 1. Out of the total 230 patients, 111 (48.3%) were inpatients. Majority (38.3%) of the participants were aged between 51 and 60 years. Mean age and standard deviation of all participants was 53.61 ± 10.7 years. Males (51.7%) were slightly more than females. Overall 74.3% of participants belonged to the middle socioeconomic class.
Table 1.
Socio-demographic distribution of study population (N=230)
Screening for depression among participants was done using PHQ-9. Internal consistency of PHQ-9 was 0.81 indicating good consistency of this psychometric scale in the study population.
A total of 104 (45.2%) were found to suffer from depression, of which 71 (30.9%) had a moderate level of depression and the rest 33 (14.3%) had severe depression. Of these 104 people, majority (78 (75%)) were unaware about their depressive status. Of the 26 people who were already aware that they were depressed, only 3 (11.5%) had consulted a doctor for this condition. Average duration of time since the detection of diabetes was 12.10 ± 7.35 years.
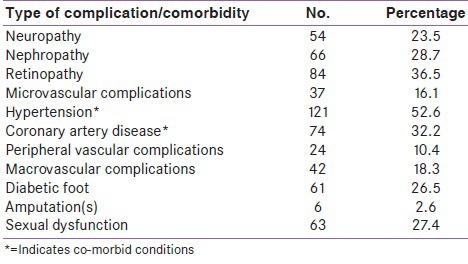
The commonest comorbidity with DM was hypertension seen in more than half of the participants followed by coronary artery disease seen in about one-third of the participants. Among the complications, retinopathy (84 (36.5%))followed by nephropathy (66 (28.7%)) were the commonest as shown in Table 2.
Table 2.
Distribution of patients based on comorbidities* and complications due to diabetes mellitus (N=230)
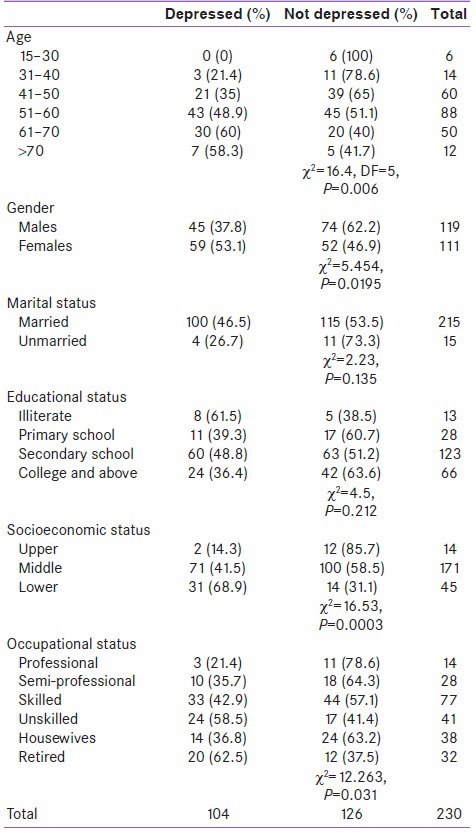
Depression was found to be associated with patients above the age of 60 years (P = 0.006), female gender (P = 0.0195), patients from lower socioeconomic status (P = 0.0003), retired patients and those in unskilled occupations (P = 0.031) [Table 3].
Table 3.
Association of level of depression with the age, gender, marital status, socioeconomic status, education and occupation of participants
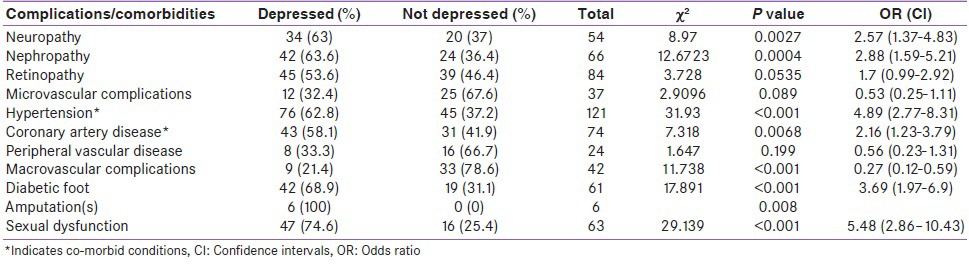
Eighty-four (36.5%) patients had complications or other comorbidities in addition to being diabetic. This group had significantly greater proportion of patients who were depressed (64 (76.2%)) compared to the other group of patients without complications or comorbidities where the proportion of depressed patients was 40 (27.4%) (χ2 = 51.25, P < 0.001).
Presence of complications like neuropathy, nephropathy, macrovascular complications, diabetic foot, amputations and sexual dysfunction was significantly associated with depression among the participants. Presence of comorbidities such as hypertension and coronary heart disease was also significantly associated with depression [Table 4].
Table 4.
Association between depression and presence of complications or co-morbidities* among diabetic patients (N=230)
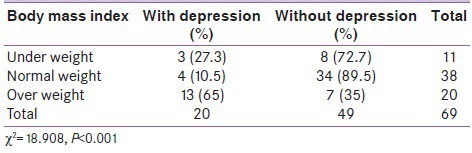
Patients who were overweight were found to be significantly more depressed than patients of normal weight or underweight (P < 0.001) as shown in Table 5.
Table 5.
Association between depression and body mass index of diabetic patients (n=69)
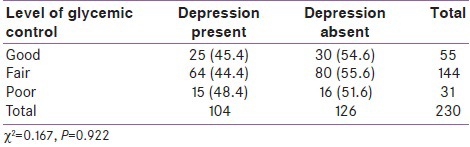
Patients receiving treatment in the form of insulin syringe injections were found to be more depressed compared to patients receiving insulin as pen devices or patients on blood sugar lowering drugs (P < 0.001) as shown in Table 6. However, the level of sugar control was not found to be associated with depression among patients as shown in Table 7.
Table 6.
Association between depression in diabetic patients and the type of treatment
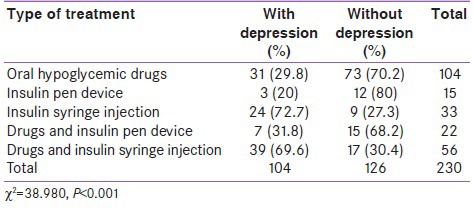
Table 7.
Association between glycemic control among patients and level of depression
DISCUSSION
Depression negatively affects quality of life, treatment outcome and medication adherence of patients with DM. The prevalence of depression among the participants in the current study was found to be 45.2%. This was higher than the findings of other studies where it ranged from 33 to 41%.[17,24,25,26,27] However, studies done in Trivandrum and US found the prevalence of depression among T2DM patients to be slightly more than 70%.[28,29]
On the other hand, the prevalence of severe depression which was 14.3% in this study was lower than the observations made in the above studies where it ranged from 18 to 20%.[17,25,30]
A number of risk factors in the current study were found to be associated with depression. Patients aged above 60 years were found to be significantly more depressed than patients of other age groups. This could probably be because people of this age group are usually retired and thus would be totally dependent on their family members to meet their treatment expenses. However several other studies have reported no association between age and prevalence of depression among T2DM patients.[24,25,31,32,33]
It has been found in the present study that depression was more significant among female patients which has been supported by other studies.[11,24,25,26,27,33,34,35,36,37] It is known that major depression occurs twice as frequently in women than in men[35] and seems to be influenced by estrogen levels.[38] Another explanation toward women being more depressed could be the social role attributed to women (passivity, dependence and emotional expression) which possibly allows them to be more emotional and extroversive.[34]
No association was seen between marital status and depression in the present study which is similar to the observations made in a study done in Bahrain.[24] However, single respondents have shown higher depression score than their married counterparts in several other studies.[25,27,33,39]
Educational status was not found to be associated with depression in the present study which is consistent with the findings of few other studies.[17,30,39] But many other studies found significant association between the two.[11,25,40,41,42]
In the present study, occupation was also found to be a risk factor. Depression was found to be more among patients who were doing unskilled work or among those who were retired. This could be probably due to financial burden imposed by the disease on these groups.
In a study done in Bangladesh housewives were found to suffer the most from severe depression, whereas retired persons were found to suffer the most from mild to moderate depression (P < 0.05). This study reported that overall depression was highest among housewives and lowest among businessmen.[25] However another study done in US reported no significant association between depression and the respondents’ employment status (P = 0.84).[33]
Socioeconomic status in this study was found to be significantly associated with depression which is consistent with other study findings.[43,44,45] DM is a chronic physical disorder which cannot be cured but can only be controlled. It thus requires lifestyle alterations, lifelong medication and its adherence for its successful treatment. Therefore individuals with low earning power face the twin burdens of paying for health care, which is largely out-of-pocket expenditure in India and meeting the needs of their family.
In the study done in US no significant association was found between depression and monthly income which is in contrast with our observations.[33]
Presence of complications among the study participants was found to be significantly associated with depression in the present study which is similar to the observations made in a study done in Bangladesh.[25]
In a study done in Chandigarh it was observed that presence of neuropathy, nephropathy and diabetic foot disease was significantly associated with depression among diabetic patients.[17] The Bahrain-based study found presence of nephropathy and ischemic heart disease to be significantly associated with depression.[24] Few other studies observed nephropathy, neuropathy, macrovascular complications and sexual dysfunction to be significantly associated with depression.[31,39,46] These observations are in accordance with our findings. Conditions like peripheral vascular disease, microvascular complications and retinopathy were not associated with depression, which has been supported by the findings of the studies done in Bahrain and Greece.[24,26]
The present study also found the presence of other comorbidities like hypertension and coronary artery disease to be associated with depression which was also observed by Jose et al. in their study.[27] But in the study done in Trivandrum no association was reported between the presence of comorbidities or complications and the presence of depression among DM patients.[28]
Patients who were overweight were found to be significantly more depressed than patients of normal weight or underweight in the present study. A number of other studies also found statistically significant association between obesity (BMI ≥30 kg/m2) and depression among T2DM patients.[6,17,24,34,47,48,49,50,51] Probable reason for this could be that obesity is often associated with a reduction in self-esteem and social and psychological problems. In few other studies however no association was established.[25,26,41,52]
It was also found in this study that patients receiving treatment in the form of insulin syringe injections were more depressed than other treatment groups. The Bahrain, Jordanian and US based studies reported insulin users to be significantly more likely to develop severe depression than users of oral anti-diabetic agents.[11,24,29] The Bangladesh-based study reported that treatment with oral anti-diabetic drugs and insulin together was associated with mild to moderate depression while only insulin use was associated with severe depression (P < 0.01). This study also found the depression score to be higher in those who used syringe for insulin administration than among pen users (P < 0.05).[25] This could be because of the patients finding insulin as the most burdensome treatment compared to oral treatment.[53] Another reason for higher prevalence of depression among insulin-treated patients could be the pain of injection. Only the Chandigarh-based study reported no significant association of depression with insulin use among patients.[17]
Although control of blood sugar levels is the major factor in diabetes management, this criteria with respect to poor blood sugar control was not associated with depression among these patients. Rather factors like presence of complications and other comorbidities due to the disease were associated with depression among diabetic patients.
So even though one is having T2DM, it is not the tight or strict control of blood sugar that is going to influence depressive symptoms but the chronic complications of diabetes. In such a scenario what we are measuring as depression may also be psychological distress associated with managing their complications and comorbidities, which clinically can be called as adjustment disorder. Difference between depressive disorder and adjustment disorder is that for the latter, the main treatment is improving or removing the underlying risk factor or condition or stressor. Several other studies however, reported a significant association between the blood glucose level or HbA1c level and depression which was different from ours.[25,26,27,28,32,37,43,46]
Limitations
This study was conducted among patients coming to tertiary hospital setup and not on general population. Hence a possible selection bias cannot not be excluded as only the more concerned diabetic patients might be seeking specialized diabetes care. Cross-sectional design of this study could be a limitation as it prevents the researcher to infer about the causality between depression and diabetes. Recall bias cannot be totally eliminated but has been minimized by reviewing the documents and validating the data. Height and weight of majority of participants could not be recorded due to feasibility reasons.
CONCLUSION
This study has identified that a high proportion of T2DM patients (45.3%) suffer from depression. The study has also highlighted some of the factors associated with depression such as elderly age, female gender, low socioeconomic status, unskilled employment and retirement from occupation, complications due to DM, being overweight and being on insulin syringe injections. The findings of the current study should be replicated in order to formulate effective intervention programs. The care of individuals with diabetes mellitus should include the screening and possible treatment for depression in order to achieve and sustain treatment goals considering the fact that only one-fourth of patients with depression were actually aware about their depressive status in this study. Identifying depression early will further improve the quality of life of diabetes patients and also reduce overall treatment costs, which are generally unaffordable by most individuals with this disease in India. Clearly identifying diabetic patients with comorbid depression, knowledge about effective psychological support and improving access to effective treatments should be public health and research priority.
ACKNOWLEDGMENT
The authors of this study would like to thank Ms. Priyanka Guntur, Ms. Renu Ramesh, Mr. Purushotham C. N., Mr. Arjun Asok, Mr. Dudaram Chaudhary, Mr. Dinesh Jeyabalan, MBBS students of Kasturba Medical College, Mangalore for their help in data collection. We also thank the medical superintendents for permitting us to do the study in their hospitals.
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.King H, Auburt RE, Herman WH. Global burden of diabetes 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care. 2000;23:934–42. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- 3.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: A meta analysis. Psychosom Med. 2001;63:619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 5.Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med. 1984;100:258–68. doi: 10.7326/0003-4819-100-2-258. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 7.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 8.Goldston DB, Kovacs M, Ho VY, Parrone PL, Stiffler L. Suicidal ideation and suicide attempts among youth with insulin-dependent diabetes mellitus. J Am Acad Child Adolesc Psychiatry. 1994;33:240–6. doi: 10.1097/00004583-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Goldston DB, Kelley AE, Reboussin DM, Daniel SS, Smith JA, Schwartz RP, et al. Suicidal ideation and behavior and noncompliance with the medical regimen among diabetic adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36:1528–36. doi: 10.1016/S0890-8567(09)66561-8. [DOI] [PubMed] [Google Scholar]
- 10.McHale M, Hendrikz J, Dann F, Kenardy J. Screening for depression in patients with diabetes mellitus. Psychosom Med. 2008;70:869–74. doi: 10.1097/PSY.0b013e318186dea9. [DOI] [PubMed] [Google Scholar]
- 11.Al-Amer RM, Sobeh MM, Zayed AA, Al-Domi HA. Depression among adults with diabetes in Jordan: Risk factors and relationship to blood sugar control. J Diabetes Complications. 2011;25:247–52. doi: 10.1016/j.jdiacomp.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican americans with type 2 diabetes. Diabetes Care. 2003;26:2822–8. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 13.James BO, Omoaregba JO, Eze G, Morakinyo O. Depression among patients with diabetes mellitus in a Nigerian teaching hospital. South Afr J Psychiatry. 2010;16:61–4. [Google Scholar]
- 14.Lustman PJ, Harper GW. Nonpsychiatric physicians’ identification and treatment of depression in patients with diabetes. Compr Psychiatry. 1987;28:22–7. doi: 10.1016/0010-440x(87)90040-x. [DOI] [PubMed] [Google Scholar]
- 15.Lustman PJ, Griffith LS, Freedland KE, Kissel SS, Clouse RE. Cognitive behavior therapy for depression in type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med. 1998;129:613–21. doi: 10.7326/0003-4819-129-8-199810150-00005. [DOI] [PubMed] [Google Scholar]
- 16.Pyne JM, Rost KM, Zhang M, Williams DK, Smith J, Fortney J. Cost-effectiveness of a primary care depression intervention. J Gen Intern Med. 2003;18:432–41. doi: 10.1046/j.1525-1497.2003.20611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 18.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 19.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 20.Kochhar PH, Rajadhyaksha SS, Suvarna VR. Translation and validation of brief patients health questionnaire against DSM IV as a tool to diagnose major depressive disorder in Indian patients. J Postgrad Med. 2007;53:102–7. doi: 10.4103/0022-3859.32209. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psych Ann. 2002;32:1–7. [Google Scholar]
- 22.Almeida OP, Almeida SA. Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry. 1999;14:858–65. doi: 10.1002/(sici)1099-1166(199910)14:10<858::aid-gps35>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 23.Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med. 1984;310:341–6. doi: 10.1056/NEJM198402093100602. [DOI] [PubMed] [Google Scholar]
- 24.Nasser J, Habib F, Hasan M, Khalil N. Prevalence of depression among people with diabetes attending diabetes clinics at primary health settings. Bahrain Med Bull. 2009;31:1–7. [Google Scholar]
- 25.Rahman M, Rahman MA, Flora MS, Rakibuz-Zaman M. Depression and associated factors in diabetic patients attending an urban hospital of Bangladesh. Int J Collaborat Res Intern Med Public Health. 2011;3:65–76. [Google Scholar]
- 26.Sotiropoulos A, Papazafiropoulou A, Apostolou O, Kokolaki A, Gikas A, Pappas S. Prevalence of depressive symptoms among noninsulin treated Greek type 2 diabetic subjects. BMC Res Notes. 2008;1:101. doi: 10.1186/1756-0500-1-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Téllez-Zenteno JF, Cardiel MH. Risk factors associated with depression in patients with type 2 diabetes mellitus. Arch Med Res. 2002;33:53–60. doi: 10.1016/s0188-4409(01)00349-6. [DOI] [PubMed] [Google Scholar]
- 28.Iype T, Shaji SK, Balakrishnan A, Charles D, Varghese AA, Antony TP. Cognition in type 2 diabetes: Association with vascular risk factors, complications of diabetes and depression. Ann Indian Acad Neurol. 2009;12:25–7. doi: 10.4103/0972-2327.48848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah BM, Gupchup GV, Borrego ME, Raisch DW, Knapp KK. Depressive symptoms in patients with type 2 diabetes in the ambulatory care setting: Opportunities to improve outcomes in the course of routine care. J Am Pharm Assoc. 2008;48:737–43. doi: 10.1331/JAPhA.2008.07078. [DOI] [PubMed] [Google Scholar]
- 30.Agbir TM, Audu MD, Adebowale TO, Goar SG. Depression among medical outpatients with diabetes: A cross-sectional study at Jos University Teaching Hospital, Jos, Nigeria. Ann Afr Med. 2010;9:5–10. doi: 10.4103/1596-3519.62617. [DOI] [PubMed] [Google Scholar]
- 31.Lloyd CE, Dyer PH, Barnett AH. Prevalence of symptoms of depression and anxiety in a diabetic clinic population. Diabet Med. 2000;17:198–202. doi: 10.1046/j.1464-5491.2000.00260.x. [DOI] [PubMed] [Google Scholar]
- 32.Larijani B, Bayat MK, Gorgani MK, Bandarian F, Akhondzadeh S, Sadjadi SA. Association between depression and diabetes. German J Psychiatry. 2004;7:62–5. [Google Scholar]
- 33.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1068–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 34.Roupa Z, Koulouri A, Sotiropoulou P, Makrinika E, Marneras X, Lahana I, et al. Anxiety and depression in patients with type 2 diabetes mellitus, depending on sex and body mass index. Health Sci J. 2009;3:32–40. [Google Scholar]
- 35.Culbertson FM. Depression and gender. An international review. Am Psychol. 1997;52:25–31. doi: 10.1037//0003-066x.52.1.25. [DOI] [PubMed] [Google Scholar]
- 36.Lee HJ, Chapa D, Kao CW, Jones D, Kapustin J, Smith J, et al. Depression, quality of life, and glycemic control in individuals with type 2 diabetes. J Am Acad Nurse Pract. 2009;21:214–24. doi: 10.1111/j.1745-7599.2009.00396.x. [DOI] [PubMed] [Google Scholar]
- 37.Shobhana R, Rama Rao P, Lavanya A, Padma C, Vijay V, Ramachandran A. Quality of life and diabetes integration among subjects with type 2 diabetes. J Assoc Physicians India. 2003;51:363–5. [PubMed] [Google Scholar]
- 38.Archer JS. NAMS/Solvay resident essay award. Relationship between estrogen, serotonin, and depression. Menopause. 1999;6:71–8. [PubMed] [Google Scholar]
- 39.Miyaoka Y, Miyaoka H, Motomiya T, Kitamura S, Asai M. Impact of sociodemographic and diabetes related characteristics on depressive state among non-insulin-dependent diabetic patients. Psychiatry Clin Neurosci. 1997;51:203–6. doi: 10.1111/j.1440-1819.1997.tb02583.x. [DOI] [PubMed] [Google Scholar]
- 40.Engum A, Mykletun A, Midthjell K, Holen A, Dahl AA. Depression and diabetes: A large population-based study of sociodemographic, lifestyle and clinical factors associated with depression in type 1 and type 2 diabetes. Diabetes Care. 2005;28:1904–9. doi: 10.2337/diacare.28.8.1904. [DOI] [PubMed] [Google Scholar]
- 41.Fisher L, Chesla CA, Mullan JT, Skaff MM, Kanter RA. Contributors to depression in Latino and European-American patients with type 2 diabetes. Diabetes Care. 2001;24:1751–7. doi: 10.2337/diacare.24.10.1751. [DOI] [PubMed] [Google Scholar]
- 42.Pouwer F, Snoek FJ. Association between symptoms of depression and glycaemic control may be unstable across gender. Diabet Med. 2001;18:595–8. doi: 10.1046/j.1464-5491.2001.00499.x. [DOI] [PubMed] [Google Scholar]
- 43.Collins MM, Corcoran P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med. 2009;26:153–61. doi: 10.1111/j.1464-5491.2008.02648.x. [DOI] [PubMed] [Google Scholar]
- 44.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity and diabetes. J Psychosom Res. 2002;53:891–5. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 45.Thomas J, Jones G, Scarinci I, Brantley P. A descriptive and comparative study of the prevalence of depressive and anxiety disorders in low-income adults with type 2 diabetes and other chronic illnesses. Diabetes Care. 2003;26:2311–7. doi: 10.2337/diacare.26.8.2311. [DOI] [PubMed] [Google Scholar]
- 46.de Groot M, Jacobson AM, Samson JA, Welch G. Glycemic control and major depression in patients with type 1 and type 2 diabetes mellitus. J Psychosom Res. 1999;46:425–35. doi: 10.1016/s0022-3999(99)00014-8. [DOI] [PubMed] [Google Scholar]
- 47.Peyrot M, Rubin RR. Levels and risks of depression and anxiety symptomatology among diabetic adults. Diabetes Care. 1997;20:585–90. doi: 10.2337/diacare.20.4.585. [DOI] [PubMed] [Google Scholar]
- 48.Katon W, von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914–20. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 49.Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16:1167–78. doi: 10.2337/diacare.16.8.1167. [DOI] [PubMed] [Google Scholar]
- 50.Sacco WP, Wells KJ, Friedman A, Matthew R, Perez S, Vaughan CA. Adherence, body mass index and depression in adults with type 2 diabetes: The mediational role of diabetes symptoms and self-efficacy. Health Psychol. 2007;26:693–700. doi: 10.1037/0278-6133.26.6.693. [DOI] [PubMed] [Google Scholar]
- 51.Balhara Y, Sagar R. Correlates of anxiety and depression among patients with type 2 diabetes mellitus. Indian J Endocrinol Metab. 2011;15:50–4. doi: 10.4103/2230-8210.83057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Asghar S, Hussain A, Ali SM, Khan AK, Magnusson A. Prevalence of depression and diabetes: A population-based study from rural Bangladesh. Diabetic Med. 2007;24:872–7. doi: 10.1111/j.1464-5491.2007.02136.x. [DOI] [PubMed] [Google Scholar]
- 53.Vijan S, Hayward RA, Ronis DL, Hofer TP. Brief report: The burden of diabetes therapy: Implications for the design of effective patient-centered treatment regimens. J Gen Intern Med. 2005;20:479–82. doi: 10.1111/j.1525-1497.2005.0117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


