Abstract
Many veterans returning from Afghanistan and Iraq experience serious mental health (MH) concerns including substance use disorders (SUD), post-traumatic stress disorder, traumatic brain injury, depression, or serious psychological distress (SPD). This article uses data from the 2004 to 2010 National Survey on Drug Use and Health to examine the prevalence of unmet MH needs among veterans aged 21 to 34 in the general population. The prevalence of untreated SUD among veterans (16%) was twice as high as untreated SPD (8%), a nonspecific diagnosis of serious MH concerns. Surprisingly, similar rates of untreated SUD and SPD were found among a nonveteran comparison sample matched on gender and age. These findings suggest that reducing unmet need for MH treatment for veterans in the general population may require improving outreach to all Americans and creating greater acceptance for MH treatment. The need for further analyses of reasons for not obtaining treatment is discussed.
INTRODUCTION
Veterans reintegrating into civilian life after serving in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) have been facing mental health (MH) concerns, especially post-traumatic stress disorder (PTSD), traumatic brain injury (TBI), depression, and substance use disorders (SUD).1-4 Prior research has evaluated the prevalence of MH concerns and opportunities for treatment at various points in the military/veteran career including postdeployment, among those being treated at Veterans Affairs (VA) facilities, and in the general population.1,5-7 This article analyzes the prevalence and covariates of unmet need for MH treatment among young veterans in the general population using data collected by the National Survey on Drug Use and Health (NSDUH).
There are various reasons veterans may not be in treatment at the VA. They may be receiving treatment elsewhere. Alternatively, some research indicates that onset or attenuation of symptoms can be delayed, especially for PTSD.1,8 On a related matter, people often delay for years after onset before obtaining MH treatment.9 Thus, some veterans with unmet need at any time will eventually receive treatment. There are also various reasons veterans avoid MH treatment. Some may not be screened for MH problems or not encouraged to seek treatment for problems such as hazardous drinking behaviors.10,11 Many wish to treat their problems on their own.12 Many veterans and military personnel attach a stigma to MH treatment, especially SUDs, which they or their peers perceive as inconsistent with the mental toughness prized in the military.5,7,12,13 Other research identifies negative attitude toward MH care as a major factor.13 The prevalence of unmet MH treatment need in the general population is reduced to the extent that people receive successful treatment and their concerns are addressed.
More than half of the OEF/OIF veterans coming in contact with the VA for any reason had MH concerns.14 Among those seeking treatment, the covariates differ substantially across disorders. Studies indicate PTSD was higher among veterans who were male, African American, younger, and married or divorced.15 In contrast, depression was higher among those who were female, White non-Hispanic, older, divorced/separated/widowed, enlisted, in the Army, and Reserve/National Guard.16 SUDs were more common among veterans who were male, younger, not married, enlisted, and in the Army17; Hispanic veterans were less likely to have a drug use disorder (DUD) but not an alcohol use disorder (AUD).17
In 2007–2008, the RAND Corporation conducted a survey of 1,965 OEF/OIF veterans to estimate the prevalence of MH concerns among veterans in the general population, who were not necessarily in contact with the VA.18 PTSD was higher among veterans who were female, Hispanic, enlisted, and in the Army, which differs substantially from the covariates in the VA study described above. The covariates of major depressive episode (MDE) were similar to those for PTSD: female, Hispanic, and enlisted. TBI did not vary significantly with any veteran characteristics.
The Substance Abuse and Mental Health Services Administration (SAMHSA) has used the NSDUH to produce a series of articles examining MH concerns and unmet treatment need among veterans in the general population. They found Serious Psychological Distress (SPD)—a nonspecific diagnosis of serious MH concerns19—was higher among veterans who were female, younger, and whose families earned less than $20,000 per year.20 MDE was higher among those who were female and younger.21 60% of veterans with an MDE received past-year treatment.21 SUDs were more common among veterans who were younger and whose families earned less than $20,000 per year.20 In 2003, 85% of veterans dependent on alcohol or drugs had not received treatment, which was slightly better than the 91% in a comparable nonveteran population.22
The SAMHSA reports are short and limited. Wagner et al23 provided a more extensive analysis of SUDs among veterans interviewed by the NSDUH 2000–2003. They found the prevalence of SUDs among veterans was 7.0%, which was not statistically different from the 6.8% among comparable nonveterans. Few veterans received SUD treatment in the past year (0.8%), but this percentage was higher than among comparable nonveterans (0.5%). This article replicates prior NSDUH analyses of veterans using recent data and presents findings regarding SUD, SPD, and unmet need for treatment as well as their covariates. The conclusion examines the implications of the findings with regard to the provision of outreach, screening, and treatment programs.
METHODS
Participants
The NSDUH is the primary source of statistical information on the use of illicit drugs and alcohol in the civilian, noninstitutionalized population of the United States.24 The survey employs a multilevel stratified hierarchical sampling procedure. Participants are interviewed face-to-face in their place of residence. Audio computer-assisted self-interviewing is used to assure confidentiality for sensitive questions. Participants receive $30 for completing the survey. This analysis used the NSDUH public-release data for 2004 through 2010 obtained from the Interuniversity Consortium for Political and Social Research. From 2004 to 2010, the response rate varied between 74% and 77%.25-31 The complete sample includes 118,625 participants aged 21 to 34 of whom 3,826 (3%) are veterans. All analyses presented used sample weights, stratification information, and complex samples procedures to obtain unbiased estimates and accurate statistical tests that control for design effects.
Unfortunately, the NSDUH does not distinguish OEF/OIF veterans from those who served elsewhere. The NSDUH asks a single question about veteran status, “Have you ever been in the United States armed forces?” It was assumed that many of the youngest veterans would have served more recently and served in Iraq and/or Afghanistan. Accordingly, the analysis was restricted to younger veterans aged 21 to 34 at the time of the interview. A comparable nonveterans group was constructed by standardizing the weights of the nonveteran subsample to match the age and gender distribution of the veteran subsample, a conventional demographic procedure used by SAMHSA in their analyses of veterans.22
Measures
The primary dependent variables were SUD and SPD in the past year. The NSDUH defines SUD as abuse or dependence on alcohol or illicit drugs based on Diagnostic and Statistical Manual of Mental Disorders criteria.19,32 To measure SPD, the NSDUH uses the K6 screener, which was designed to identify serious impairment from any MH concern other than SUD with six short questions (e.g., “How often did you feel nervous?”) rated on a scale from none to all of the time.19,33
Analyses
The article presents population estimates of SUD and SPD. Unmet need for SUD or SPD treatment was estimated as those participants with the condition who did not receive treatment in the past year. The analysis also examined self-reported need for treatment provided in response to the question, “During the past 12 months, was there any time when you needed MH treatment or counseling for yourself but didn’t get it?”25 Separate estimates of unmet need for treatment were calculated for the veterans and the standardized nonveterans population as well as the unstandardized population of all NSDUH participants aged 21 to 34.
Logistic regression was used to estimate how the prevalence of past-year SPD and SUD varied across participant characteristics including veteran status, gender, race/ethnicity, age, education, employment, family income, marital status, urbanicity, and interview year. Unfortunately, the NSDUH public use datasets do not include a measure of region, which precluded its analysis. The NSDUH urbanicity measure is also quite limited indicating only whether a participant lives in a core-based statistical area (CBSA) or a more rural location. The NSDUH measure of race/ethnicity distinguishes White non-Hispanic, African American non-Hispanic, and Hispanic participants.25 The remaining less common categories were combined. Logistic regression was also used to estimate the likelihood that a person with SPD received MH treatment and similarly that a person with SUD received alcohol or drug treatment. Each regression model included an interaction term for each variable with veteran status (e.g., veteran × gender) to identify whether the covariates for veterans differed from those of the general population. Because of the large sample size, many parameter estimates were statistically significant. Accordingly, the analysis placed greater emphasis on parameter estimates that were not only statistically significant but also substantial such as an odds ratio greater than 1.5.
RESULTS
Sample Characteristics
Table I presents the characteristics of the subsample of NSDUH participants aged 21 to 34 interviewed in 2004–2010. The nonveteran demographic entries for gender, age, and race/ethnicity were not standardized. The subsequent measures of social integration were standardized to control for differences in gender and age between veterans and non-veterans. The total column is not standardized by gender and race. It thus gives much greater weight to females than the prior columns. Consequently, characteristics that are more common among females such as poverty were higher among the total population than among either the veteran or the standardized nonveteran subpopulations. Veterans were much more likely to be male, were slightly older (perhaps because younger persons are more likely to be still in the service), and were more likely to be White or African American as opposed to Hispanic or other.
TABLE I.
Characteristics of NSDUH Participants Aged 21 to 34, 2004–2010
| Veterans | Nonveterans | Total | |
|---|---|---|---|
| Sample Size (Unweighted) | 3,826 | 114,793 | 118,625 |
| Gender (Unstandardized) (%) | |||
| Male | 82.1** | 48.3 | 49.7 |
| Female | 17.9** | 51.7 | 50.3 |
| Race/Ethnicity | |||
| (Unstandardized) (%) | |||
| White (Non-Hispanic) | 67.3** | 60.1 | 60.3 |
| African American (Non-Hispanic) |
15.5** | 12.9 | 13.0 |
| Hispanic | 12.0** | 19.6 | 19.3 |
| Other | 5.2** | 7.5 | 7.4 |
| Mean Age | 28.7** | 27.4 | 27.4 |
| (Unstandardized) (%) | |||
| Education (%) | |||
| No High School Degree | 4.2** | 15.9 | 14.1 |
| High School Degree | 35.0** | 28.2 | 27.6 |
| Some College | 42.4** | 25.7 | 29.5 |
| College Degree | 18.4** | 30.1 | 28.9 |
| Employment (%) | |||
| Full Time | 70.6 | 71.5 | 60.9 |
| Part Time | 11.8 | 13.2 | 17.8 |
| Unemployed | 5.8 | 5.3 | 5.5 |
| Other | 11.8* | 10.0 | 15.8 |
| Family Income (%) | |||
| Below Poverty | 7.1** | 13.5 | 16.8 |
| Near Poverty (100–200%) | 22.5 | 21.7 | 22.6 |
| Higher Income (>200%) | 70.4** | 64.8 | 60.6 |
| Marital Status | |||
| Married | 48.6** | 42.9 | 39.9 |
| Separated/Divorced/Widowed | 16.2** | 7.1 | 7.4 |
| Single | 35.2** | 50.0 | 52.8 |
| Urbanicity | |||
| Within a CBSA | 90.7** | 92.7 | 92.7 |
| Outside of Any CBSA | 9.3** | 7.3 | 7.3 |
Difference between veterans and nonveterans was statistically significant at the α = 0.05 level;
Difference between veterans and nonveterans was statistically significant at the α = 0.01 level.
Veterans were more likely to have completed high school (generally a requirement to enter the military) and more likely to have gone to college, though less likely to have graduated. Veterans and nonveterans had relatively similar employment profiles. Veterans were less likely to be living in poverty. Veterans were more likely to be married, an important protective factor; however, they were also more likely to be separated, divorced, or widowed, which is often associated with MH concerns as either a cause or a consequence. More than 90% of the sample lived in a CBSA, although veterans were slightly more likely to live in a more rural area outside of any CBSA.
Prevalence of SUD and SPD
Table II compares the rates of substance use, SUD, and SPD between veterans and comparable nonveterans. Veterans were not more likely than nonveterans to use illegal drugs or be dependent on them. Most veterans (75%) reported having consumed alcohol in the past month, slightly more than nonveterans (68%). However, veterans were not more likely than nonveterans to binge drink (defined as 5 or more drinks in a single session), drink heavily (defined as binge drinking on 5 or more of the past 30 days), or have an AUD. Veterans in the general population were slightly more likely to have SPD than their nonveteran counterparts (14% vs. 12%) and even more likely than nonveterans to have had an MDE (10% vs. 7%). There was substantial overlap between SUD and SPD; 5% of veterans had both conditions representing 29% of those with SUD and 38% of those with SPD.
TABLE II.
Variation in SUD and MH Disorders by Veteran Status
| % by Subpopulation |
|||
|---|---|---|---|
| Veterans | Nonveteransa | Total | |
| Past-Month Use | |||
| Any Alcohol | 74.6** | 68.0 | 64.8 |
| Binge Drinking (5+ Drinks) | 43.8 | 44.0 | 38.7 |
| Heavy Drinking (5+ Binges) | 14.2 | 14.7 | 12.1 |
| Marijuana | 11.0 | 12.4 | 11.4 |
| Cocaine (Any Form) | 1.6 | 1.9 | 1.6 |
| Hallucinogens | 0.9 | 0.9 | 0.9 |
| Pain Killers | 3.5 | 3.4 | 3.3 |
| SUD (Past-Year Abuse or Dependence) | |||
| Alcohol or Drugs | 17.7 | 18.2 | 16.2 |
| Alcohol | 15.3 | 15.4 | 13.6 |
| Any Illicit Drug | 4.9 | 5.4 | 5.0 |
| Marijuana | 2.8 | 3.2 | 2.9 |
| Any Illicit Drug Except Marijuana |
2.4 | 2.8 | 2.6 |
| Pain Killers | l.1 | 1.2 | 1.2 |
| Any Psychotherapeutic | 1.6 | 1.4 | 1.5 |
| MH Disorder (Past Year) | |||
| Serious Psychiatric Distress | 13.8* | 12.0 | 14.8 |
| MDE | 9.5** | 6.7 | 8.5 |
| Co-Occurring SUD and SPD | 5.2 | 4.4 | 4.6 |
Difference between veterans and nonveterans was statistically significant at the α = 0.05 level;
Difference between veterans and nonveterans was statistically significant at the α = 0.01 level.
Standardized to veteran sample by gender and age.
Table III examines the covariates of SUD and SPD. The variation with veteran status was not statistically significant in either model, although several of the interaction terms were, especially for SPD. Unlike in the previous tables, the first column for each model presents the factors for all NSDUH participants (nonveteran and veteran) and the second column presents the interaction terms identifying how veterans differ from nonveterans. The factor most associated with variation in both SPD and SUD based on the Wald statistic was gender, although with the opposite effects between the models. Men were twice as likely as women to have SUD. In contrast, women were 70% more likely to have SPD. The second most significant factor was marital status. Being married was strongly associated with lower SUD and SPD. This is consistent with the idea that marriage serves as a protective factor against MH concerns. However, there is a possibility of reverse causation—that MH concerns can contribute to the dissolution of a relationship. Consistent with this altemative explanation, being separated, widowed, or divorced was associated with higher rates of SPD (but not SUD). SUD and SPD were higher among Whites, higher among the unemployed, and declined modestly with educational level. SUD (but not SPD) declined with age and was slightly higher within a CBSA than more rural location.
TABLE III.
Variation in MH Disorders (Logistic Regression)
| Odds Ratio (Wald Statistic) of a MH Disorder |
||||
|---|---|---|---|---|
| SUD |
SPD |
|||
| Overall | Vets | Overall | Vets | |
| Intercept or Base Odds | 0.33 | 0.14 | ||
| Veteran Status | n/a | (0.0) | n/a | (0.7) |
| Nonveterana | n/a | — | n/a | — |
| Veteran | n/a | — | n/a | — |
| Gender | (842.3)** | (2.0) | (398.3)** | (0.1) |
| Malea | 1.0 | — | 1.0 | — |
| Female | 0.5 | — | 1.7 | — |
| Race/Ethnicity | (85.0)** | (2.3) | (82.9)** | (0.9) |
| White (Non-Hispanic)a | 1.0 | — | 1.0 | — |
| African American (Non-Hispanic) |
0.6 | — | 0.6 | — |
| Hispanic | 0.7 | — | 0.6 | — |
| Other | 0.6 | — | 0.7 | — |
| Age | (31.6)** | (1.9) | (4.4) | (2.6)* |
| 21 | 1.5 | — | — | 2.2 |
| 22–23 | 1.5 | — | — | 1.1 |
| 24–25 | 1.4 | — | — | 1.0 |
| 26–29 | 1.2 | — | — | 1.1 |
| 30–34a | 1.0 | — | — | 1.0 |
| Education | (11.6)** | (0.1) | (25.1)** | (1.9) |
| No High School Degree | 1.2 | — | 1.1 | — |
| High School Degreea | 1.0 | — | 1.0 | — |
| Some College | 1.1 | — | 1.1 | — |
| College Degree | 1.0 | — | 0.8 | — |
| Employment | (18.6)** | (1.2) | (56.9)** | (0.3) |
| Full Timea | 1.0 | — | 1.0 | — |
| Part Time | 1.0 | — | 1.1 | — |
| Unemployed | 1.4 | — | 1.8 | — |
| Other | 0.9 | — | 1.3 | — |
| Family Income | (1.8) | (0.2) | (16.4)** | (4.5)* |
| Below Poverty | — | — | 1.2 | 1.4 |
| Near Poverty (100–200%) | — | — | 1.1 | 1.7 |
| Higher Income (>200%)a | — | — | 1.0 | 1.0 |
| Marital Status | (292.7)** | (1.1) | (186.2)** | (0.8) |
| Married | 0.4 | — | 0.6 | — |
| Separated/Divorced/ Widowed |
1.0 | — | 1.5 | — |
| Singlea | 1.0 | — | 1.0 | — |
| Urbanicity | (19.0)** | (3.1) | (0.0) | (0.3) |
| Within a CBSAa | 1.0 | — | — | — |
| Outside of Any CBSA | 0.8 | — | — | — |
| Year | (1.2) | (2.5)* | (1.8) | (2.1) |
| 2004 | — | 0.7 | — | — |
| 2005 | — | 0.6 | — | — |
| 2006 | — | 0.6 | — | — |
| 2007 | — | 0.7 | — | — |
| 2008 | — | 0.7 | — | — |
| 2009 | — | 1.4 | — | — |
| 2010a | — | 1.0 | — | — |
n/a, not applicable.
Wald statistic was significant at the α = 0.05 level;
Wald statistic was significant at the α = 0.01 level.
Reference category.
SPD (but not SUD) was higher among the poor and near poor (those earning above the poverty level but below twice this level). The interaction terms indicate that poor and near poor veterans were even more likely to have experienced SPD than comparable nonveterans. Having more than 1 covariate that differs from the reference population in a logistic regression results in a multiplicative compound effect on the odds.34 The rate of SPD was 20% higher than among those of higher income and the rate among poor veterans was 40% higher than among poor persons in general. Thus, poor veterans were 70% more likely (1.2 × 1.4 ≈ 1.7) to have SPD than the reference population of otherwise comparable wealthier nonveterans. Near poor veterans were nearly twice as likely (1.1 × 1.7 ≈ 1.9). Veterans aged 21 were more likely to have SPD, though rates were similar among those aged 22 to 34. Among veterans, SUD was lower in 2004–2008, only 60% to 70% as in 2010 and 40% higher in 2009. We do not have any meaningful explanation for this observation at this time.
Figure 1 examines the extent of met and unmet treatment needs in the past year for SUD and SPD. The figure shows that whereas 18% of veterans met the criteria for SUD, only 2% received treatment and an estimated 16% of all veterans in the general population did not receive treatment. In strong contrast, relatively few (1%) veterans reported that they had an unmet need for SUD treatment. Surprisingly, the extent of SUD and the percentages of met and unmet treatment needs among nonveterans were very similar to those among veterans.
FIGURE 1.
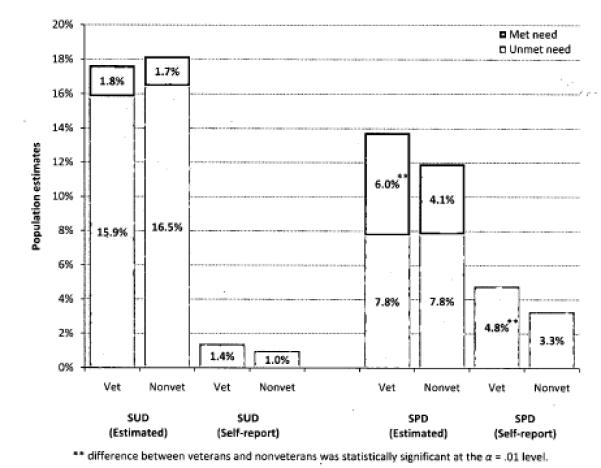
Met and unmet need for SUD and SPD treatment among veterans and nonveterans.
SPD was slightly less common than SUD in the general population and much more likely to have been treated. About half as many veterans (8%) and nonveterans had untreated SPD as SUD. The rate of treatment for SPD among veterans (43%) was much higher than among nonveterans (34%). Veterans (5%) were also more likely to self-report an unmet need for SPD treatment than nonveterans (3%).
Table IV examines variation in treatment for SUD and SPD. There were many similarities between the models and several very noticeable differences. The strongest association with SPD treatment was gender. Women were nearly twice as likely to receive treatment for SPD as men but comparably likely to receive treatment for SUD. Whites were about twice as likely to receive treatment for both SUD and SPD as African Americans and Hispanics. This difference was even more pronounced among minority veterans, with the one exception of Hispanic veterans who were almost as likely to receive treatment for SPD (but not SUD) as their nonveteran counterparts.
TABLE IV.
Variation in Receipt of Treatment Among Participants With MH Disorders
| Odds-Ratio (Wald Statistic) |
||||
|---|---|---|---|---|
| SUD |
SPD |
|||
| Overall | Vets | Overall | Vets | |
| Intercept or Base Odds | 0.20 | 0.63 | ||
| Veteran Status | n/a | (0.8) | n/a | (0.1) |
| Nonveterana | n/a | — | n/a | — |
| Veteran | n/a | — | n/a | — |
| Gender | (2.8) | (2.2) | (161.3)** | (0.7) |
| Malea | — | — | 1.0 | — |
| Female | — | — | 1.9 | — |
| Race/Ethnicity | (12.8)** | (3.6)* | (60.4)** | (5.6)** |
| White (Non-Hispanic)a | 1.0 | 1.0 | 1.0 | 1.0 |
| African American (Non-Hispanic) |
0.5 | 0.7 | 0.5 | 0.5 |
| Hispanic | 0.6 | 0.3 | 0.4 | 0.8 |
| Other | 0.6 | 3.7 | 0.4 | 4.2 |
| Age | (5.5)** | (3.4)* | (28.6)** | (0.7) |
| 21 | 0.6 | 3.2 | 0.5 | — |
| 22–23 | 0.7 | 0.9 | 0.5 | — |
| 24–25 | 0.9 | 0.4 | 0.6 | — |
| 26–29 | 0.9 | 0.5 | 0.8 | — |
| 30–34a | 1.0 | 1.0 | 1.0 | — |
| Education | (35.4)** | (2.8)* | (7.6)** | (2.3) |
| No High School Degree | 1.3 | 0.4 | 0.9 | — |
| High School Degreea | 1.0 | 1.0 | 1.0 | — |
| Some College | 0.6 | 1.6 | 1.1 | — |
| College Degree | 0.3 | 3.2 | 1.3 | — |
| Employment | (8.6)** | (0.7) | (29.9)** | (1.1) |
| Full Timea | 1.0 | — | 1.0 | — |
| Part Time | 1.2 | — | 1.3 | — |
| Unemployed | 1.5 | — | 1.3 | — |
| Other | 1.8 | — | 1.9 | — |
| Family Income | (2.9) | (1.3) | (1.7) | (6.4)** |
| Below Poverty | — | — | — | 0.3 |
| Near Poverty (100–200%) | — | — | — | 1.2 |
| Higher Income (>200%)a | — | — | — | 1.0 |
| Marital Status | (18.2)** | (0.0) | (2.7) | (1.0) |
| Married | 0.5 | — | — | — |
| Separated/Divorced/ Widowed |
1.3 | — | — | — |
| Singlea | 1.0 | — | — | — |
| Urbanicity | (0.6) | (0.1) | (0.4) | (0.4) |
| Within a CBSAa | — | — | — | — |
| Outside of Any CBSA | — | — | — | — |
| Year | (1.5) | (2.1) | (2.1) | (0.7) |
| 2004 | — | — | — | — |
| 2005 | — | — | — | — |
| 2006 | — | — | — | — |
| 2007 | — | — | — | — |
| 2008 | — | — | — | — |
| 2009 | — | — | — | — |
| 2010a | — | — | — | — |
Wald statistic was significant at the α = 0.05 level;
Wald statistic was significant at the α = 0.01 level.
Reference category.
Treatment for both SUD and SPD increased with age. Persons who were employed were less likely to have received treatment for both SUD and SPD. This relationship however could be quite complex. Those employed full time may have had less opportunity to seek treatment or altematively been concerned that the stigma of treatment could affect how they are perceived at work. Additionally, persons with serious MH concerns may have been compelled to leave their jobs, at least temporarily, as they attended to their treatment.
More educated persons were less likely to have received treatment for SUD but more likely for SPD. However, the parameter estimates (as near multiplicative inverses) indicate that the decrease in SUD treatment with education does not pertain to veterans. Notably, poor veterans were only 30% as likely to have received treatment for SPD but not SUD. Married persons were less likely to have received treatment for SUD; those who were separated, widowed, or divorced were more likely. Interview year was not associated with variation in the receipt of treatment.
DISCUSSION
The NSDUH data indicate that a substantial portion of young veterans in the general population have SUD (18%) or SPD (14%). Most of the SUDs involved use of alcohol and not illegal drugs or unauthorized use of prescription drugs. These rates underestimate the total number of veterans who are struggling with MH concerns because they do not include veterans living in institutions including VA hospitals, substance abuse treatment programs, and homeless shelters. Surprisingly, the rate of SUD among comparable nonveterans in the general population was about the same and the rate of SPD only a few percentage points lower than among veterans. The covariates among veterans were also similar to those among nonveterans with only a few exceptions. Most notably, veterans living in low-income families (up to 200% of the poverty level) were more likely to have SPD but not SUD. The rates of SUD and SPD among veterans in the general population were no higher than among comparable nonveterans. This finding is consistent with the possibility that the Department of Defense and VA MH screening and referral programs may be quite effective overall. An altemative interpretation is that the rates of MH concerns in the general population is substantial and needs to be addressed.
This analysis suggests treatment programs are reaching very few persons with SUDs in the general population. Only 10% of veterans who screened positive for SUD had received treatment in the past year. As a result, an estimated 16% of veterans in the general population were dealing with an untreated SUD. Again, the rate was similar for comparable nonveterans. Of note, African American and Hispanic veterans who screened positive for SUD or SPD were much less likely to have received treatment in the past year. Accordingly, research needs to focus on the specific reasons African American and Hispanic veterans are not seeking treatment.
Interestingly, only 1% of all veterans reported an unmet need for alcohol or drug treatment compared to the 16% of unmet need for treatment estimated. There are several possible explanations for this disparity. One possibility is instrumentation; the NSDUH screener might identify many less serious SUD cases. Another and more likely possibility is denial—a reluctance to admit a need for treatment.
Treatment rates for SPD were higher than for SUD and higher for veterans than nonveterans. Less than half of veterans (43%) who met criteria for SPD reported receiving treatment in the past year. However, the rate for comparable nonveterans was even lower (34%). The self-report rate of unmet treatment need among veterans was fairly close to the screener-based estimate. The gap was wider for nonveterans. Overall, these findings indicate that outreach programs aimed at veterans in the general community are fairly effective. A substantial proportion of veterans with MH concerns other than SUD are receiving treatment. This could be the result of programs available to returning veterans and existing out-reach programs. Other veterans are aware that they need MH treatment but are not obtaining it. Further research needs to examine the reasons why veterans who are aware of their MH problems are not getting treatment. Veterans who screened positive for SPD who were either African American, Hispanic, or living in an impoverished family (below the poverty line) were significantly less likely to have received treatment. Further research into their reasons for not getting treatment is needed to identify likely historical, cultural, and financial barriers to treatment for these subpopulations.
The findings presented established that veterans in the general population have similar levels of SUD and SPD as comparable nonveterans, which is not necessarily good since most MH concerns in the general population go untreated in any year.35,36 More importantly, veterans are more likely to be aware of their need for SPD treatment and more likely to receive it. These findings suggest an altemative approach to serving MH concerns among veterans. Perhaps, there are barriers and cultural norms that discourage both veterans and nonveterans from seeking treatment, especially for SUDs which mostly involves the use of alcohol. Perhaps, the larger need is to increase MH outreach and services to the general population at large, including veterans and nonveterans alike. In this manner, the goal would be to increase treatment seeking as part of the broader American culture. This could be coupled with financial assistance and greatly reduce the stigma or perceptions of vulnerability associated with getting treatment. This effort might prove more effective than any veteran-specific program and bring the remaining veteran population in need of treatment into contact with providers and social service organizations. It would have the further benefit of getting nonveterans with treatment needs into treatment.
Limitations and Future Directions
A comparison of veterans’ and nonveterans’ reasons for not entering treatment would provide further insight into whether this type of strategy might prove successful. Indeed, it would be useful to understand why those who do not think they have a problem would not enter treatment too. Hoge et al7 obtained this information from a sample of military personnel by asking participants to, “Rate each of the possible concerns that might affect your decision to receive MH counseling or services if you ever had a problem.” The responses for those who screened positive for MH concerns were different from those who did not. In contrast, the NSDUH only asks about reasons for not going to treatment of those who reported having had a need for treatment in the past year but did not get it.37 It would be highly useful if the NSDUH revised their questions and skip patterns to match those of Hoge et al to identify the larger attitude about MH treatment prevailing in society, not just among those in need of treatment.
All in all, the NSDUH proved to be an extremely valuable resource for this study. Indeed, the results of this analysis for unmet treatment need have identified important directions for further research into reasons for not getting treatment, especially for SPD. The public-release NSDUH data include the information regarding reasons and barriers to treatment that could support this additional effort. A major limitation of the NSDUH is the lack of information about military service. For the purposes of our analysis and based on the larger veterans’ MH literature, we would ideally like to see additional military service questions added to the NSDUH including the following: When did you return from your last tour of duty? Where were you deployed? Did you experience combat? Were you enlisted or an officer? In which branch did you serve? And, in which component did you serve (Active Duty, Reserves, or National Guard)? This additional information would further the usefulness of the NSDUH for analyzing health concerns and tracking trends among veterans in the general population, who are not necessarily in contact with the VA.
ACKNOWLEDGMENTS
This research was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA R0l AA020178).
Footnotes
Publisher's Disclaimer: Copyright of Military Medicine is the property of Association of Military Surgeons of the United States and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
REFERENCES
- 1.Institute of Medicine . Returning Home from Iraq and Afghanistan: Preliminary Assessment of Readjustment Needs of Veterans, Service Members and Their Families. National Academies Press; Washington, DC: 2010. Available at http://www.nap.edu; accessed March 16, 2012. [PubMed] [Google Scholar]
- 2.Finley EP. Fields of Combat: Understanding PTSD Among Veterans of Iraq and Afghanistan. Cornell; Ithaca, NY: 2011. [Google Scholar]
- 3.Tanielian T, Jaycox LH. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. RAND; Santa Monica, CA: 2008. Available at www.rand.org/pubs/monographs; accessed March 16, 2012. [Google Scholar]
- 4.Ender MG. American Soldiers in Iraq: McSoldiers or Innovative Professionals? Routledge; New York: 2009. [Google Scholar]
- 5.American Psychological Association . American Psychological Association; Washington, DC: 2007. The Psychological Needs of U.S. Military Service Members and Their Families: A Preliminary Report. Available at http://www.ptsd.ne.gov/publications/military-deployment-task-force-report.pdf; accessed March 16, 2012. [Google Scholar]
- 6.Watkins KE, Pincus HA, Paddock S, et al. Care for veterans with mental and substance use disorders: good performance, but room to improve on many measures. Health Aff. 2011;30(11):2194–203. doi: 10.1377/hlthaff.2011.0509. [DOI] [PubMed] [Google Scholar]
- 7.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 8.Andrews B, Brewin CR, Philpott R, Stewart L. Delayed-onset posttraumatic stress disorder: a systematic review of the evidence. Am J Psychiatry. 2007;164(9):1319–26. doi: 10.1176/appi.ajp.2007.06091491. [DOI] [PubMed] [Google Scholar]
- 9.Wang PS, Berglund PA, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–13. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun PS, Elter JR, Jones ER, Jr., Kudler H, Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among U.S. Veterans of the wars in Iraq and Afghanistan. J Clin Psychiatry. 2008;69(11):1686–93. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- 11.Seal KH, Cohen G, Bertenthal D, Cohen BE, Maguen S, Daley A. Reducing barriers to mental health and social services for Iraq and Afghanistan veterans: outcomes of an integrated primary care clinic. J Gen Intern Med. 2011;26(10):1160–7. doi: 10.1007/s11606-011-1746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown MC, Creel AH, Engel CC, Herrell RK, Hoge CW. Factors associated with interest in receiving help for mental health problems in combat veterans returning from deployment to Iraq. J Nerv Ment Dis. 2011;199(10):797–801. doi: 10.1097/NMD.0b013e31822fc9bf. [DOI] [PubMed] [Google Scholar]
- 13.Kim PY, Britt TW, Klocko RP, Riviere LA, Adler AB. Stigma, negative attitudes about treatment and utilization of mental health care among soldiers. Mil Psychol. 2011;23:65–81. [Google Scholar]
- 14.Veterans Health Administration . Veterans Health Administration; 2012. Analysis of VA Health Care Utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF) and Operation New Dawn (OND) Veterans, cumulative from 1st Qtr FY 2002 through 1st Qtr FY 2012. Available at http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtrl.pdf; accessed May 22, 2012. [Google Scholar]
- 15.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476–82. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 16.Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100(12):2450–6. doi: 10.2105/AJPH.2009.166165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Schell TL, Marshall GN. Survey of individuals previously deployed for OEF/OIF. In: Tanielian T, Jaycox LH, editors. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. RAND; Santa Monica, CA: 2008. pp. 87–115. Available at www.rand.org/pubs/monographs; accessed March 16, 2012. [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration . Results from the 2009 National Survey on Drug Use and Health: Mental Health Findings. SAMHSA; Rockville, MD: 2010. Available at http://www.samhsa.gov; accessed March 16, 2012. [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration . The NSDUH Report: Serious Psychological Distress and Substance Use Disorder among Veterans. SAMHSA; Rockville, MD: 2007. Available at http://www.samhsa.gov; accessed March 16, 2012. [Google Scholar]
- 21.Substance Abuse and Mental Health Services Administration . The NSDUH Report: Major Depressive Episode and Treatment for Depression among Veterans Aged 21–39. SAMHSA; Rockville, MD: 2008. Available at http://www.samhsa.gov; accessed March 16, 2012. [Google Scholar]
- 22.Substance Abuse and Mental Health Services Administration . The NSDUH Report: Substance Use, Dependence and Treatment among Veterans. SAMHSA; Rockville, MD: 2005. Available at http://www.samhsa.gov; accessed March 16, 2012. [Google Scholar]
- 23.Wagner TH, Harris KM, Federman B, Lanting D, Yesenia L, Humphreys K. Prevalence of substance use disorders among veterans and comparable nonveterans from the National Survey on Drug Use and Health. Psychol Serv. 2007;4(3):149–57. [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration . Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. SAMHSA; Rockville, MD: 2010. Available at http://www.samhsa.gov; accessed March 16, 2012. [Google Scholar]
- 25.Substance Abuse and Mental Health Services Administration . 2009 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2010. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 26.Substance Abuse and Mental Health Services Administration . 2008 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2009. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration . 2007 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2008. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 28.Substance Abuse and Mental Health Services Administration . 2006 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2007. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 29.Substance Abuse and Mental Health Services Administration . 2005 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2006. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 30.Substance Abuse and Mental Health Services Administration . 2004 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2005. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed March 16, 2012. [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration . 2010 National Survey on Drug Use and Health Public Use Codebook. SAMHSA; Rockville, MD: 2011. Available at http://www.icpsr.umich.edu/icpsrweb/SAMHDA/; accessed May 16, 2012. [Google Scholar]
- 32.American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4 American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 33.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 34.Hosmer DW, Jr., Lemeshow S. Applied Logistic Regression. Wiley; New York: 1989. [Google Scholar]
- 35.Kessler RC, Berglund PA, Bruce ML, et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36(6):987–1007. [PMC free article] [PubMed] [Google Scholar]
- 36.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 37.Substance Abuse and Mental Health Services Administration . 2009 National Survey on Drug Use and Health: Cai Specifications for Programming. SAMHSA; Rockville, MD: 2008. Available at http://www.samhsa.gov/data/NSDUH.aspx; accessed March 16, 2012. [Google Scholar]


