Abstract
Severe hypoglycemia in patients with diabetes is associated with increased risk of adverse cardiovascular events and death. Recent large randomized clinical trials in individuals with type 2 diabetes have shown that intensive glycemic control may result in increased mortality and hypoglycemia has been investigated as a possible cause. Acute hypoglycemia is a pro-arrhythmic, pro-inflammatory and pro-thrombotic state and several mechanisms have been proposed to explain how hypoglycemia might increase cardiovascular morbidity and mortality. However, data from large clinical trials do not provide strong evidence to establish hypoglycemia as cause of increase mortality. Severe hypoglycemia is also a marker of frailty and predictor of adverse outcomes in patients with diabetes. Individualized therapy should be the goal in patients with diabetes to avoid severe hypoglycemia and any related adverse outcomes.
Keywords: Hypoglycemia, diabetes mellitus, cardiovascular risk, HAAF, mortality, type 2 diabetes mellitus, type 1 diabetes mellitus, severe hypoglycemia
Introduction
Cardiovascular disease is the leading cause of morbidity and mortality in individuals with diabetes mellitus. Intensive glycemic control has been shown to decrease risk of microvascular complications of diabetes but its effect on the risk of macrovascular complications is less clear. While a significant relationship between glycemic control and cardiovascular outcomes has been repeatedly demonstrated in epidemiological analyses (1), it is only recently that the question has been evaluated in large randomized trials. ACCORD (Action to Control Cardiovascular Risk in Diabetes)(2), ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) (3) and VADT (Veterans Affairs Diabetes Trial) (4) all examined the impact of intensifying glycemic control on cardiovascular outcomes, but failed to demonstrate benefit on the primary outcome measures of cardiovascular disease. However, participants randomized to the intensive glucose arm in ACCORD study where hemoglobin A1c was targeted at < 6.0% had 22% more mortality than those randomized to the standard glucose arm with a hemoglobin A1c target of 7.1-7.9%; largely due to cardiovascular disease. A similar finding of increased mortality risk in participants randomized to intensive glucose control was also found in the NICE-SUGAR (Normoglycemia in Intensive Care Evaluation–Survival Using Glucose Algorithm Regulation) (5) trial that examined the impact of intensive glycemic control in critically ill patients with type 2 diabetes. In the NICE-SUGAR trial target blood glucose ranged between 81 to 108 mg/dl in the intensive control group as compared to a target of 180 mg/dl or less in the conventional group. Reasons for the increased mortality in participants randomized to intensive glycemic control in these trials is not well understood, but hypoglycemia has been implicated as a possible cause. Individuals in the intensively treated arms in these trials all had significantly higher rates of hypoglycemia than their controls.
In this paper we will review the results of recent post hoc analysis of ACCORD and ADVANCE done to examine the relationship between hypoglycemia and mortality, as well as review the epidemiological data that links hypoglycemia, mortality and cardiovascular disease. We will also discuss what is known about how hypoglycemia might increase cardiovascular morbidity and mortality.
Insights from recent large clinical trials
The ACCORD trial (2) was designed to study whether a strategy of intensive glycemic control with target glycated hemoglobin level of < 6% would reduce risk of serious cardiovascular events in patients with advanced type 2 diabetes and additional cardiovascular risk factors. The study was stopped early (mean of 3.7 years of followup) because of a 22% increased risk of death in the intensive therapy group. While the causes of death were highly variable, most of them were believed to be due to cardiovascular causes. Interestingly, the incidence of severe hypoglycemia was three times higher in the intensive group as compared to the standard group, and there was immediate discussion that hypoglycemia must have been contributing to the increased risk of death (6). However, at the conclusion of the glucose arm of the study, all participants were transitioned to the standard treatment that targeted a glycated hemoglobin of 7.1-7.9% so that the blood pressure and lipid arms of the trial could be completed. At five years of followup (•7), the risk of mortality continued to be greater in those who had been randomized to the intensive glycemic arm, even though the rate of hypoglycemia after transition dropped. Because the rate of hypoglycemia was similar in both groups in the post transition period, it seems unlikely that hypoglycemia was the cause of the continued increase in mortality in the participants who had originally been randomized to the intensive glucose arm.
The ACCORD investigators have performed post hoc analyses to understand the link between hypoglycemia and mortality in their cohort. In 2010, Bonds et al (•8) reported that mortality risk was increased in those participants who experienced severe hypoglycemia, which was defined as hypoglycemia that required the assistance of another to treat. Interestingly, this relationship was seen in participants randomized to both the intensive and standard glycemia treatment strategies. For those participants who experienced more than one episode of severe hypoglycemia, the risk of mortality was greater in those participants in the standard group than in the intensive group. In this analysis no temporal relation was seen between hypoglycemia and death, and only one death was adjudicated as definitely related to hypoglycemia. The authors concluded that severe hypoglycemia did not account for the difference in mortality between the two study arms.
In another post-hoc analysis of ACCORD study cohort, Seaquist et al (•9) examined the relationship between frequent and unrecognized hypoglycemia as a surrogate for recurrent hypoglycemia and mortality risk. Analysis from this study showed a lower risk of death in ACCORD study subjects assigned to the intensive treatment group who experienced more episodes of hypoglycemia. Such a relationship was not seen in the standard group. One explanation for these findings could be that individuals with diabetes who are exposed to frequent hypoglycemia develop blunted counterregulatory response to hypoglycemia, which could potentially reduce the impact of hypoglycemia to cardiovascular function.
ADVANCE (3) and VADT (4) trials also randomized patients with type 2 diabetes to intensive vs. standard glucose control. No significant effects of intensive glycemic control was seen on rates of major cardiovascular events or death in these trials. As with the ACCORD study, the rate of hypoglycemia was higher in the intensive control arms. In a retrospective analysis of ADVANCE study, Zoungas et al (•10) examined the associations between severe hypoglycemia and the risks of vascular complications and death among 11,140 patients with type 2 diabetes. During a median follow-up of 5 years, severe hypoglycemia was found to be associated with increased risks of macrovascular events, microvascular events, and death from both cardiovascular and noncardiovascular causes. The relationship was highly significant, but no temporal relationship or a dose–response relationship was observed. Analysis from VADT trial showed that severe hypoglycemia within the past 90 days was associated with increased cardiovascular events and death (11).
Association between hypoglycemia and cardiovascular events in epidemiological studies
Several epidemiological studies have shown that hypoglycemia is associated with increased risk of death in patients with diabetes. In a large-scale retrospective study Johnston et al (12) examined the association between outpatient hypoglycemic events and acute cardiovascular events in patients with type 2 diabetes. Acute cardiovascular events included acute myocardial infarction, coronary artery bypass grafting, revascularization, percutaneous coronary intervention, and incident unstable angina. In this analysis 27,065 patients had hypoglycemic events during the evaluation period. Outpatient hypoglycemic events in this study were independently associated with an increased risk of acute cardiovascular events. In a prospective study, McCoy et al (13) examined the relationship between a history of severe hypoglycemia with mortality risk during the subsequent five years in more than 1000 adult patients with diabetes. They found that the odds ratio for mortality was 3.38 in those with a history of severe hypoglycemia; a significantly higher ratio than for patients without such a history.
Recently, Hsu et al (14) investigated the relationship between hypoglycemia with total mortality and cardiovascular events, including stroke, cardiovascular diseases, and all-cause hospitalization in a population of more than 77,000 Taiwanese with newly diagnosed type 2 diabetes. Between 1998-2009, there were 1,844 hypoglycemic events (500 inpatients and 1,344 outpatients) among the 77,611 patients. Symptomatic hypoglycemia in patients with diabetes was associated with an increased risk of cardiovascular events, all-cause hospitalization, and all-cause mortality. Similar association between hypoglycemia and higher risk of cardiovascular events in patients with type 2 diabetes has been shown in other studies as well (15).
While most work in this area has examined risk in patients with type 2 diabetes, a recent study by Gruden et al (16) evaluated risk in a population with type 1 diabetes. They determined the relationship between severe hypoglycemia at baseline and incident cardiovascular disease up to 8 years in the future in a population of more than 3000 Europeans. They found that the frequency of severe hypoglycemia at baseline was not a predictor of subsequent cardiovascular events and that hypoglycemic episodes were not cross-sectionally associated with increase in markers of inflammation and endothelial injury.
Impact of hypoglycemia in hospitalized patients
Investigators have also looked at impact of tight glycemic control and hypoglycemia on mortality in hospitalized patients. Trials of tight glycemic control in critically ill individuals have shown conflicting results, with one trial showing decreased mortality (17), another showing no benefit (18), and the most recent (5) showed an increase in mortality. As shown in studies done in the out patient setting, intensive control also increases the risk of hypoglycemia in hospitalized patients (18, 19). A meta analysis which included results from twenty-nine randomized control trials in critically ill patients did not show reduced hospital mortality with tight glucose control but tight glucose control resulted in significantly higher risk of hypoglycemia (19). Multiple studies have demonstrated that hypoglycemia in hospitalized patients is associated with increased mortality (20, 21).
Very little work has been done to determine the impact of hypoglycemia on outcomes in non-critically ill hospitalized patients. In a retrospective cohort study, Boucai et al (22) compared in-hospital mortality risk of in patients with hypoglycemia (defined as at least 1 blood glucose ≤ 70 mg/dL) relative to patients with normoglycemia. They found that hypoglycemia was associated with greater risk of in-hospital mortality, but this association was seen only in patients who developed hypoglycemia spontaneously. Hypoglycemia that occurred with initiation of antidiabetic medications was not associated with higher in-hospital mortality. The authors concluded that these findings suggest that hypoglycemia in hospitalized patients is likely a marker of disease rather then a direct cause of death.
How might hypoglycemia increase mortality and cardiovascular disease?
The mechanisms by which hypoglycemia may increase cardiovascular events and mortality are not fully understood. Proposed pathways include sympathoadrenal activation, abnormal cardiac repolarization, induction of cardiac and cerebral ischemia, development of cardiac autonomic neuropathy, increased thrombogenesis and enhanced inflammation all of which could cause sudden death (Figure 1).
Figure 1.
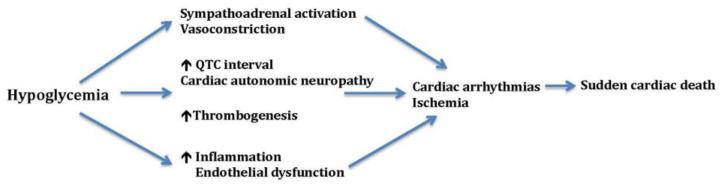
Potential mechanism underlying hypoglycemia related cardiovascular disease or death
Landstedt-Hallin and colleagues (23) were among the first to study the effects of insulin-induced hypoglycemia on cardiac repolarization using QT interval measurements in individuals with type 2 diabetes. In their investigation, participants were studied under euglycemic and hypoglycemic clamps in which plasma concentration of glucose and insulin were carefully controlled. Mean QT intervals and QT dispersion increased significantly during hypoglycemia, indicating that hypoglycemia led to changes in cardiac repolarization that could increase risk of arrhythmia in patients with diabetes. Sympathoadrenal stimulation in response to hypoglycemia is thought to drive these ECG changes. Hypokalemia may be another contributing factor; hypoglycemia can decrease serum potassium through activation of of sympathoadrenal system along with direct effects of insulin (•24). Increases in QT interval (QTc) and QT dispersion (QTd) during acute experimental hypoglycemia is prevented with β adrenoceptor blockade, whereas potassium replacement prevented the increase in QT dispersion only (25).
In real life settings, hypoglycemia has been found to be associated with cardiac ischemia. Desouza et al (26) carried out 72-hour continuous glucose monitoring along with simultaneous cardiac Holter monitoring in 21 patients with coronary artery disease and insulin treated type 2 diabetes. Participants in this study also recorded symptoms of cardiac ischemia and symptoms of hypoglycemia while they were monitored. The investigators found that some but not all participants had definite ECG abnormalities during hypoglycemia that were suggestive of cardiac ischemia. Such ECG changes were seen much more often during hypoglycemia than during normoglycemia and hyperglycemia and participants reported more cardiac symptoms during hypoglycemia than at other levels of glycemia.
Cardiovascular autonomic neuropathy has been associated with increased risk of mortality in patients with diabetes (27, 28). Recurrent antecedent hypoglycemia in patient with diabetes can lead to development of syndrome of hypoglycemia associated autonomic failure (HAAF), which includes defective glucose counterregulation and hypoglycemia unawareness (29). In addition to hypoglycemia, antecedent hypoglycemia can also impair autonomic responses to other physiologic stresses. Davis et al showed that in healthy individuals antecedent hypoglycemia attenuates normal exercise induced rise in catecholamines, cortisol and growth hormone (30). Recent antecedent hypoglycemia has been shown to impair autonomic cardiovascular function with reduced baroreflex sensitivity and sympathetic response to a hypotensive stress. Impaired autonomic cardiovascular function, including decreased cardiac vagal baroreflex sensitivity, can potentially increase vulnerability to a ventricular arrhythmia (31).
More recently, the impact of hypoglycemia on the risk of thrombosis has been examined. In a study of subjects with type 1 diabetes and healthy controls, Wright et al (32) showed that markers of inflammation and platelet activation including P-selectin, expression of CD40 on monocytes and hsCRP were significantly higher during acute insulin-induced hypoglycemia. Another study looked at the effects of 2 hours of clamped hyperinsulinemic euglycemia and moderate hypoglycemia on markers of inflammation and fibrinolytic balance in individuals with type 1 diabetes and healthy individuals (33). Results from this study demonstrated that hypoglycemia had acute and widespread effects including activation of proinflammatory mechanisms (ICAM, VCAM, E-selectin, VEGF, IL-6), increase in platelet activation (P-selectin), and decrease in systemic fibrinolytic balance (increase in PAI-1, no change in tPA) in both individuals with type 1 diabetes and healthy controls.
Hypoglycemia predictor vs cause of cardiovascular events
As discussed earlier in this review, recent large clinical trials in patients with type 2 diabetes have shown that hypoglycemia is associated adverse cardiovascular outcomes and death. Similarly, several epidemiological studies have shown a strong association between hypoglycemia and increased cardiovascular events and mortality. However, none of these data establish a direct causal relationship between severe hypoglycemia and increased mortality. None have found a close temporal or a dose response relationship between hypoglycemia and adverse outcomes. Study participants who have higher rates of severe hypoglycemia usually have more comorbidities and are on more glucose-lowering medications than participants without severe hypoglycemia. Acute hypoglycemia induces physiological changes that can lead to a pro arrhythmic and pro thrombotic state and it is plausible that these changes can lead to acute cardiac ischemia or ventricular arrhythmias. Evidence from these studies also suggest that severe hypoglycemia may be a marker of frailty. In patients with diabetes severe hypoglycemia may be prognostic tool identifying susceptible patients who may be at increased risk of cardiovascular event and death.
Conclusion
Over the last several years, a significant body of evidence has appeared that indicates severe hypoglycemia in patients with diabetes is associated with an increased risk of adverse cardiovascular events and death. Several possible mechanisms has been proposed to explain the increase risk of cardiovascular events with hypoglycemia but direct evidence linking hypoglycemia to adverse cardiovascular outcomes is lacking. Investigation to date also suggests that severe hypoglycemia is a marker of frailty and predictor of adverse outcomes in patients with diabetes. Providers should routinely evaluate patients regarding risk and history of hypoglycemia. Patients should receive education on how recognize, treat and prevent hypoglycemia. Diabetic patients with history of severe hypoglycemia should receive close attention and providers should individualize treatment plans based patient’s age, duration of diabetes and other comorbidities and adjust glycemic goals to avoid severe hypoglycemia and any related morbidity and mortality.
Footnotes
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Riddle MC. Glycemic control and cardiovascular mortality. Current Opinion in Endocrinology Diabetes and Obesity. 2011;18(2):104–9. doi: 10.1097/MED.0b013e3283446b7e. [DOI] [PubMed] [Google Scholar]
- 2.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 4.Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–U62. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 5.Finfer S, Blair D, Bellomo R, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–97. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 6.Riddle MC. Counterpoint: Intensive glucose control and mortality in ACCORD-still looking for clues. Diabetes Care. 2010;33(12):2722–4. doi: 10.2337/dc10-1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •7.Gerstein HC, Miller ME, Genuth S, et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011;364(9):818–2. doi: 10.1056/NEJMoa1006524. This report describes the 5-year outcomes on mortality and cardiovascular events in participants of ACCROD trial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •8.Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. Br Med J. 2010;340:b4909. doi: 10.1136/bmj.b4909. Post hoc analyses of ACCORD study suggesting that severe hypoglycemia was likely not the cause of difference in mortality between the intensive and control arms. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •9.Seaquist ER, Miller ME, Bonds DE, et al. The impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study. Diabetes Care. 2012;35(2):409–14. doi: 10.2337/dc11-0996. This post hoc analyses of ACCORD study showed that subjects in the intensive control group who experienced more episodes of hypoglycemia had a lower risk of death. One explanation for this interesting finding is that individuals with diabetes who are exposed to frequent hypoglycemia can develop blunted counterregulatory response to hypoglycemia which could reduce impact of hypoglycemia on cardiovascular function. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •10.Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010;363(15):1410–8. doi: 10.1056/NEJMoa1003795. This retrospective analysis of ADVANCE study showed severe hypoglycemia was associated with increased risks of cardiovascular events and death. [DOI] [PubMed] [Google Scholar]
- 11.Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA diabetes trials: A position statement of the american diabetes association and a scientific statement of the american college of cardiology foundation and the american heart association (vol 32, pg 187, 2009) Diabetes Care. 2009;32(4):754. doi: 10.2337/dc08-9026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnston SS, Conner C, Aagren M, et al. Evidence linking hypoglycemic events to an increased risk of acute cardiovascular events in patients with type 2 diabetes. Diabetes Care. 2011;34(5):1164–70. doi: 10.2337/dc10-1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCoy RG, Van Houten HK, Ziegenfuss JY, et al. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–901. doi: 10.2337/dc11-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsu P, Sung S, Cheng H, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes A nationwide population-based study. Diabetes Care. 2013;36(4):894–900. doi: 10.2337/dc12-0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao Y, Campbell CR, Fonseca V, Shi L. Impact of hypoglycemia associated with antihyperglycemic medications on vascular risks in veterans with type 2 diabetes. Diabetes Care. 2012;35(5):1126–32. doi: 10.2337/dc11-2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gruden G, Barutta F, Chaturvedi N, et al. Severe hypoglycemia and cardiovascular disease incidence in type 1 diabetes the EURODIAB prospective complications study. Diabetes Care. 2012;35(7):1598–604. doi: 10.2337/dc11-1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–67. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 18.Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–61. doi: 10.1056/NEJMoa052521. [DOI] [PubMed] [Google Scholar]
- 19.Soylemez Wiener R, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults - A meta-analysis. JAMA-J Am Med Assoc. 2008;300(8):933–44. doi: 10.1001/jama.300.8.933. [DOI] [PubMed] [Google Scholar]
- 20.Svensson A, McGuire D, Abrahamsson P, Dellborg M. Association between hyper- and hypoglycaemia and 2 year all-cause mortality risk in diabetic patients with acute coronary events. Eur Heart J. 2005;26(13):1255–61. doi: 10.1093/eurheartj/ehi230. [DOI] [PubMed] [Google Scholar]
- 21.Kagansky N, Levy S, Rimon E, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003;163(15):1825–9. doi: 10.1001/archinte.163.15.1825. [DOI] [PubMed] [Google Scholar]
- 22.Boucai L, Southern WN, Zonszein J. Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med. 2011;124(11):1028–35. doi: 10.1016/j.amjmed.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Landstedt-Hallin L, Englund A, Adamson U, Lins P. Increased QT dispersion during hypoglycaemia in patients with type 2 diabetes mellitus. J Intern Med. 1999;246(3):299–307. doi: 10.1046/j.1365-2796.1999.00528.x. [DOI] [PubMed] [Google Scholar]
- •24.Frier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care. 2011;34:S132–7. doi: 10.2337/dc11-s220. Review article on effects of hypoglycemia on cardiovascular system. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson R, Harris N, Ireland R, Lee S, Newman C, Heller S. Mechanisms of abnormal cardiac repolarization during insulin-induced hypoglycemia. Diabetes. 2003;52(6):1469–74. doi: 10.2337/diabetes.52.6.1469. [DOI] [PubMed] [Google Scholar]
- 26.Desouza C, Salazar H, Cheong B, et al. Association of hypoglycemia and cardiac ischemia - A study based on continuous monitoring. Diabetes Care. 2003;26(5):1485–9. doi: 10.2337/diacare.26.5.1485. [DOI] [PubMed] [Google Scholar]
- 27.Gerritsen J, Dekker J, TenVoorde B, et al. Impaired autonomic function is associated with increased mortality, especially in subjects with diabetes, hypertension, or a history of cardiovascular disease - the hoorn study. Diabetes Care. 2001;24(10):1793–8. doi: 10.2337/diacare.24.10.1793. [DOI] [PubMed] [Google Scholar]
- 28.Maser R, Mitchell B, Vinik A, Freeman R. The association between cardiovascular autonomic neuropathy and mortality in individuals with diabetes - A meta-analysis. Diabetes Care. 2003;26(6):1895–901. doi: 10.2337/diacare.26.6.1895. [DOI] [PubMed] [Google Scholar]
- 29.Cryer P. Mechanisms of hypoglycemia-associated autonomic failure and its component syndromes in diabetes. Diabetes. 2005;54(12):3592–601. doi: 10.2337/diabetes.54.12.3592. [DOI] [PubMed] [Google Scholar]
- 30.Davis S, Galassetti P, Wasserman D, Tate D. Effects of antecedent hypoglycemia on subsequent counterregulatory responses to exercise. Diabetes. 2000;49(1):73–81. doi: 10.2337/diabetes.49.1.73. [DOI] [PubMed] [Google Scholar]
- 31.Adler GK, Bonyhay I, Fainng H, et al. Antecedent hypoglycemia impairs autonomic cardiovascular function implications for rigorous glycemic control. Diabetes. 2009;58(2):360–6. doi: 10.2337/db08-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright RJ, Newby DE, Stirling D, et al. Effects of acute insulin-induced hypoglycemia on indices of inflammation putative mechanism for aggravating vascular disease in diabetes. Diabetes Care. 2010 Jul;33(7):1591–7. doi: 10.2337/dc10-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joy NG, Hedrington MS, Briscoe VJ, et al. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes Care. 2010;33(7):1529–35. doi: 10.2337/dc09-0354. [DOI] [PMC free article] [PubMed] [Google Scholar]


