Abstract
Numerous studies have pointed to histone deacetylase inhibitors as potential therapeutics for various neurodegenerative diseases, and clinical trials with several histone deacetylase inhibitors have been performed or are underway. However, histone deacetylase inhibitors tested to date are either highly cytotoxic or have very low specificities for different histone deacetylase enzymes. Our laboratories have identified a novel class of histone deacetylase inhibitors (2-aminobenzamides) that reverses heterochromatin-mediated silencing of the frataxin (FXN) gene in Friedreich ataxia. We have identified the histone deacetylase enzyme isotype target of these compounds and present evidence that compounds that target this enzyme selectively increase FXN expression from pathogenic alleles. Studies with model compounds show that these histone deacetylase inhibitors increase FXN messenger RNA levels in the brain in mouse models for Friedreich ataxia, relieve neurological symptoms observed in one mouse model, and support the notion that this class of molecules may serve as therapeutics for the human disease.
Keywords: chromatin immunoprecipitation, Friedreich ataxia, histone deacetylase inhibitor, heterochromatin, neurodegenerative disorder
Friedreich ataxia (OMIM 229300) is an autosomal recessive genetic disorder caused by a GAA•TTC triplet repeat expansion in the first intron of the nuclear FXN gene, encoding the essential mitochondrial protein frataxin (reviewed in 1). The vast majority of patients with Friedreich ataxia have 2 expanded FXN alleles, but a small number have one expanded allele and one allele with a coding region mutation. Unaffected individuals have 6 to 30 copies of the repeat, whereas affected people have as many as 1000 copies. The expanded repeats cause transcriptional repression of FXN through formation of heterochromatin2,3 and subsequent loss of frataxin protein. Frataxin insufficiency leads to neurodegeneration in the posterior columns of the spinal cord and the pyramidal tracts of the cerebellum, and in the dorsal root ganglia. In addition, cardiomyocytes and β-cells of the pancreas are also affected, leading to cardiac hypertrophy and diabetes in many affected individuals. Age of onset and disease severity correlate with the length of the GAA•TTC triplet repeat expansion (reviewed in 4). The average age of onset is in the second decade of life5 and the average age at death ranges from 30 to 40 years, with cardiac dysfunction being the most frequent cause of mortality.6 Currently there is no effective therapy for Friedreich ataxia.
Because frataxin is a mitochondrial protein involved in iron homeostasis, heme biosynthesis, and assembly and transfer of iron-sulfur clusters,7 several therapeutic approaches have been aimed at correction of mitochondrial dysfunction through the use of antioxidants (eg, idebenone and other mitochondrial targeted compounds8) or iron chelation.9 Although clinical trials are quite advanced with these approaches, no molecules have been reported as yet to show efficacy in slowing the progression of Friedreich ataxia or amelioration of neurological symptoms.1 Unlike many triplet-repeat diseases (eg, the polyglutamine expansion diseases), expanded GAA•TTC triplets in FXN are in an intron and do not alter the amino acid sequence of frataxin protein; thus, gene activation would be of therapeutic benefit. Several laboratories, including our own, have focused on therapies relying on activation of the silent gene (reviewed in 10). Other approaches include increasing levels of frataxin protein, with erythropoietin,11,12 with small molecules that stabilize frataxin against its normal turnover,13 or with protein replacement therapy.14 One other approach is gene therapy;15 however, current technology for delivery of a safe and effective expression vector to patients is not sufficiently advanced to envision success in this area in the immediate future. This review summarizes our efforts toward advancing a class of histone deacetylase inhibitors, the 2-aminobenzamides, as therapeutics for Friedreich ataxia. But first we summarize the evidence that Friedreich ataxia is a gene silencing disease with an epigenetic basis.
Friedreich Ataxia is a Transcription Defect Disease
A large body of evidence indicates that long GAA•TTC repeats within FXN intron 1 cause gene silencing through either unusual DNA structures or heterochromatin (reviewed in 10,16). Other lines of evidence show that the repeats do not affect RNA processing: that is, generation of the mature messenger RNA from the primary transcript is not affected by the repeats (17 and below). Although one publication using an artificial reporter construct did find an effect of the repeats on RNA splicing, this study did not extend their results to endogenous FXN in patient cells.18 There is also no evidence that long GAA-repeat intron 1 RNA is stable and could lead to an RNA-toxicity disease, such as found in myotonic dystrophy or fragile X-associated tremor/ataxia (reviewed in 19). In particular, we used intron 1 strand-specific primers for complementary DNA synthesis from RNA samples from control and FRDA Friedreich ataxia cells, followed by real-time polymerase chain reactionPCR, again using primers for FXN intron 1. We find that intron 1 RNA is at very low abundance in both cell types, suggesting rapid turn over after transcription (E Soragni, unpublished studies). Other laboratories have reported an FXN antisense transcript in both Friedreich ataxia cells and control cells.20 A tag corresponding to this antisense RNA is found in the human antisense transcriptome (position 71650344 on the “-” strand of chromosome 9, at the FXN exon 1/intron 1 boundary; UCSC Genome Browser 21), but given the location of the start-site for this RNA, it would not include the repeats. Another tag is found at position 71652938, 717bp downstream of the repeats. Although we were able to detect the corresponding antisense RNA, the levels of expression of such transcript were not different in affected versus unaffected lymphoblasts (E Soragni, unpublished results). Given the very low levels of intron 1 RNA (sense or antisense), it is highly unlikely that Friedreich ataxia is an RNA toxicity disease or that increases in FXN messenger RNA would lead to RNA toxicity, as found in other triplet repeat diseases.19
Extensive literature documents that expanded GAA•TTC repeats adopt unusual DNA structures in vitro, such as triplexes and “sticky” DNA (17,22,23, and additional references therein) and that such structures inhibit transcription both in vitro and in transfection assays in mammalian cells.24 Another model is that a DNA-RNA triplex is responsible for blocking transcription elongation.25,26 These biochemical results are consistent with the observed correlation between repeat length, triplex/”sticky” DNA formation and the age at onset and severity of disease. GAA•TTC repeat-mediated inhibition of replication in mammalian cells also provides supportive evidence for the formation of triplexes and/or sticky DNA in cells.27 However, confirmation of the role of such structures in Friedreich ataxia gene silencing must await experimental evidence that expanded GAA•TTC repeats exist in a non-B DNA structure at the chromosomal FXN in patient cells.
In contrast to a DNA structure-based mechanism for FXN transcriptional silencing, a growing literature documents that FXN alleles harboring expanded repeats have all the hallmarks of heterochromatin-mediated gene silencing. The first report that suggested a heterochromatin model for silencing was from Festenstein and colleagues,2 who showed that a transgene harboring GAA•TTC repeats induced silencing in vivo, in a manner reminiscent of position effect variegated gene silencing.2 Position effect variegated gene silencing occurs when a gene is located within or near regions of heterochromatin, and silent heterochromatin is characterized by the presence of particular types of histone modifications (for example, H3-K9 trimethylation and histone tail hypoacetylation), the presence of histone deacetylases, DNA methyltransferases, chromodomain proteins, such as members of the HP-1 family of repressors, and polycomb group proteins.28 In addition, GAA•TTC repeat-mediated repression was enhanced by co-expression of the heterochromatin protein HP1.2 It is certainly possible that an unusual non-B DNA structure, such the triplexes and/or the sticky DNA conformation adopted by GAA•TTC repeats, is the signaling mechanism that initiates heterochromatin silencing of genes harboring such repeats, such as FXN in Friedreich ataxia.
Subsequent to this pioneering study,2 our group and others have examined the histone modifications on endogenous FXN in Friedreich ataxia cells using chromatin immunoprecipitation methods, with antibodies to various histone modifications and cell lines derived from patients with Friedreich ataxia3,29-31 or in mouse models for the disease.32,33 In our study, no significant differences in the levels of histone acetylation were found on the FXN promoter in cell lines from a patient with Friedreich ataxia and those from unaffected individuals.3 However, the first intron of active FXN alleles in normal cell lines is enriched in acetylated histones H3 and H4, compared with the inactive alleles in Friedreich ataxia cells. Additionally, H3-K9 is highly trimethylated in the Friedreich ataxia cell line compared with the normal cell line. Along with hypoacetylation, trimethylation of H3-K9 is a hallmark of heterochromatin.
Importantly, although our studies were conducted in Friedreich ataxia lymphoid cells, the same epigenetic differences between active and inactive FXN alleles have also been found in Friedreich ataxia autopsy brain, cerebellum, and heart,32 the tissues affected in Friedreich ataxia. Thus, the histone postsynthetic modification state within the coding region of inactive FXN alleles is consistent with a chromatin-mediated mechanism as the cause of gene silencing in Friedreich ataxia.2 One study reports that compared with unaffected cells, the 5′ untranslated region of FXN in patient cells is depleted of the insulator protein CTCF, pointing to the involvement of CTCF in maintaining an open chromatin state on active FXN.20 Recent reports have also suggested that the chromatin changes associated with pathogenic FXN alleles prevent transcript elongation by RNA polymerase II through expanded GAA•TTC repeats,30,31,34 although one report suggested that both transcription initiation and elongation may be affected.30
Other studies have examined DNA methylation on active versus inactive FXN alleles in Friedreich ataxia patient cells and cell lines,29,35 in human Friedreich ataxia tissue samples, and in a mouse model,32 finding that DNA methylation at particular residues adjacent to the GAA•TTC repeats correlates with FXN silencing. Along with histone hypoacetylation and methylation (eg, H3-K9), DNA methylation is also a hallmark of gene repression. DNA methylation is a mark for recruitment of repressor complexes, containing histone deacetylases, mediated by methyl-CpG binding proteins.36 Alternatively, methylation could affect the binding of regulatory proteins required for active FXN transcription as suggested by Usdin and colleagues.29 Taken together, this body of literature points to Friedreich ataxia as an epigenetic silencing disease.
Histone Deacetylase Inhibitors to Correct Frataxin Deficiency in Friedreich Ataxia
Chromatin structural changes and histone acetylation and deacetylation are involved in various neurological and neuromotor diseases in addition to Friedreich ataxia, including spinal muscular atrophy, Huntington disease, fragile X syndrome, and others.37-42 Thus, inhibitors of the histone deacetylase enzymes may revert silent heterochromatin to an active chromatin conformation, and restore the normal function of genes that are silenced in these diseases.37,42 Eighteen histone deacetylase enzymes have been identified in the human genome, including the zinc-dependent (class I, class II, and class IV) and the NAD+-dependent enzymes (class III or sirtuins; for review, see 43). Histone deacetylase enzymes 1, 2, 3, and 8 belong to class I, showing homology to the yeast enzyme RPD3. Class II is further divided into class IIa (histone deacetylase enzymes 4, 5, 7, and 9) and IIb (histone deacetylase enzymes 6 and 10), according to their sequence homology and domain organization. Histone deacetylase enzyme 11 is the lone member of class IV. The sirtuins (class III) are related to the yeast silent information regulator 2 protein and are involved in regulation of metabolism and aging. A wide range of chemical entities have been identified as histone deacetylase inhibitors, including small carboxylates (such as sodium butyrate, valproic acid, and sodium phenylbutyrate), hydroxamic acids (such as trichostatin A and suberoylanilide hydroxamic acid), benzamides (such as MS-275), epoxyketones (trapoxins), and cyclic peptides (including apicidin and depsipeptide). Although clinical trials with several histone deacetylase inhibitors in various neurological and neuromotor diseases have been performed or are underway (see www.clinicaltrials.gov), those tested to date have very low specificities for the histone deacetylase enzymes, and as such no major successes have been reported.
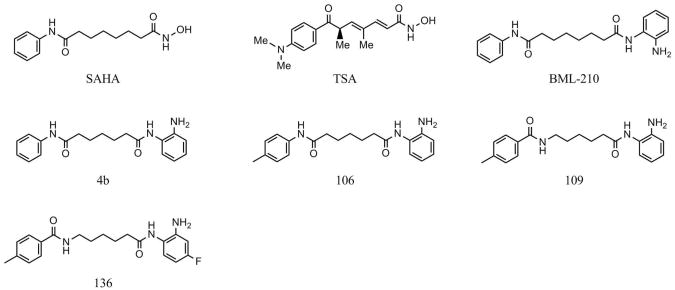
Based on the hypothesis that chromatin structure and the histone modification state of FXN are responsible for gene repression on alleles containing expanded GAA•TTC repeats, we asked whether histone deacetylase inhibitors might affect transcription of silenced FXN. Our results3 indicate that a commercially available histone deacetylase inhibitor (BML-210 from Enzo Life Sciences, Farmingdale, New York; Figure 1), and derivatives we have synthesized (Figure 1 and 3,33,44,45), relieve repression of FXN in lymphoid cell lines derived from patients with Friedreich ataxia, in primary lymphocytes from donor blood from patients with Friedreich ataxia, and in two mouse models.33,45 We also observe increases in frataxin protein that quantitatively parallel the observed changes in FXN messenger RNA. This finding is important because it demonstrates that expanded GAA•TTC repeats in the primary FXN RNA transcript do not interfere with RNA processing. Our compounds increased levels of FXN messenger RNA in lymphocytes from >100 patients with Friedreich ataxia, and the level of FXN messenger RNA in their lymphocytes was generally increased to at least that of lymphocytes from carrier siblings or parents. Independent confirmation of these results has been presented.44 Since heterozygous individuals do not exhibit symptoms of Friedreich ataxia, we believe our compounds have elicited a therapeutically useful increase in FXN messenger RNA in patient cells.
Figure 1.
Structures of the histone deacetylase inhibitors. Abbreviations: BML,; SAHA,; TSA,.
Surprisingly, we find that only members of the 2-aminobenzamide family of histone deacetylase inhibitors related to BML-210 reactivate silenced FXN in Friedreich ataxia cells (Figure 13). For example, the related hydroxamic acid suberoylanilide hydroxamic acid (Figure 1) is inactive as an activator of FXN transcription in Friedreich ataxia cells (at subcytotoxic concentrations), although suberoylanilide hydroxamic acid is a superior general histone deacetylase inhibitor to BML-210 and derivatives, as measured by IC50 values. Chromatin immunoprecipitation experiments also show that 4b increases acetylation at particular lysine residues of histones H3 and H4 within intron 1 of FXN (H3-K14, H4-K5, and H4-K123), while suberoylanilide hydroxamic acid and trichostatin A (Figure 1), 2 histone deacetylase inhibitors that have no effects on FXN messenger RNA levels, have no effect on histone acetylation on FXN. Taken together, our results suggest that a specific histone deacetylase, or histone deacetylase-protein complex, is involved in FXN silencing and 2-aminobenzamide histone deacetylase inhibitors selectively target this protein in cells. Alternatively, a different mechanism of action of these inhibitors could account for our results (see below).
Importantly, we find that the 2-aminobenzamides only increase transcription from pathogenic FXN alleles, both in human cells and in a mouse model (see below). Figure 2 shows results of an experiment where peripheral blood mononuclear cells from unaffected individuals and patients with Friedreich ataxia were incubated with histone deacetylase inhibitors 106 or 109 (Figure 1) at 10 μM for 48 hours, RNA isolated and FXN messenger RNA quantified by real-time quantitative reverse transcriptase PCR polymerase chain reaction(qRT-PCR). This experiment clearly shows only a very small effect of these compounds on wild-type alleles in cells from unaffected individuals compared with significant increases in FXN messenger RNA in cells from affected individuals, strongly suggesting that the compound is only acting on pathogenic alleles. Similar results have been presented for histone deacetylase inhibitor 4b.3,46 Moreover, chromatin immunoprecipitation experiments show no effects of the compounds on wild-type alleles in a mouse model for the disease (see below).33
Figure 2.
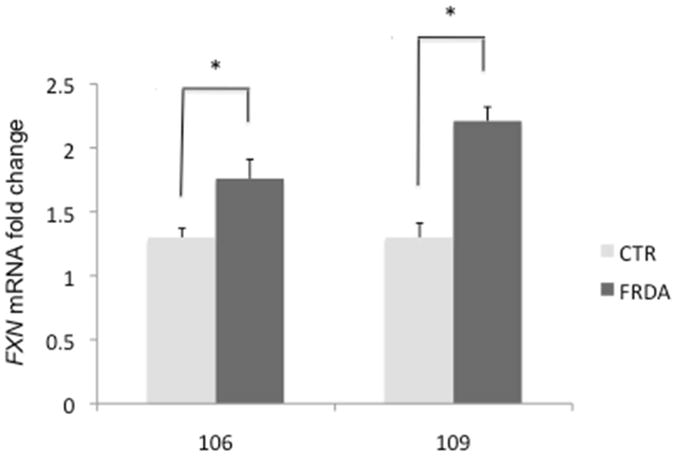
Effect of histone deacetylase inhibitors 106 and 109 on FXN messenger RNA levels in peripheral blood mononuclear cells isolated from unaffected individuals and patients with Friedreich ataxia. Cells were incubated in culture with 106/109 at 10 μM for 48 h prior to mRNA determinations by quantitative reverse transcriptase polymerase chain reaction, using cell number and input RNA concentration for normalization. The fold-change relative to a dimethyl sulfoxide vehicle control is shown for each data set, along with the standard error of the mean (SEM). The number of samples for each group is 15 for unaffected and 53 for patients in the 106-treated samples, and 7 for unaffected and 83 for patients in the 109-treated samples. Comparing histone deacetylase inhibitor-treated patient FXN levels to unaffected, P < .05 (*). Abbreviations: CTR,; FRDA, Friedreich ataxia.
Efficacy of Histone Deacetylase Inhibitors in Mouse Models for Friedreich Ataxia
In collaboration with the Pandolfo laboratory in Brussels, Belgium, we assessed the in vivo efficacy of our histone deacetylase inhibitors in a mouse model for Friedreich ataxia.33 The homozygous knock-in/knock-in (KIKI, FXN230GAA/230GAA) mouse exhibits ∼66% of wild-type FXN messenger RNA in the brain and other organs.47 Characteristic histone modifications occur at expanded alleles in the first intron of the mouse frataxin gene in the KIKI mouse as in cells from patients with Friedreich ataxia3 and Friedreich ataxia autopsy material,32 including increased H3-K9 trimethylation and hypoacetylation of histones H3 and H4. Treatment of KIKI mice with histone deacetylase inhibitor 106 (Figure 1) increased histone H3 and H4 acetylation in chromatin near the GAA•TTC repeat and restored frataxin levels in the nervous system and heart. Furthermore, microarray analysis indicated that most of the differentially expressed genes in KIKI mice, compared with wild-type mice of the same genetic background, reverted toward wild-type levels. We have thus demonstrated in vivo efficacy of our histone deacetylase inhibitors, at least with respect to increasing levels of FXN messenger RNA. As indicated above, the histone deacetylase inhibitors only increase FXN messenger RNA levels from the knock-in allele harboring GAA repeats; no effect of these compounds is found on wild-type alleles in the same mice.33,44 In addition, chromatin immunoprecipitation experiments in the mouse model show an effect on FXN intron 1 chromatin in only pathogenic alleles (no effect in wild-type alleles) and no affect at the promoter either in either pathogenic or wild-type alleles. These data, along with our results in peripheral blood mononuclear cells (above), strongly indicate that the compounds are acting at the mechanism of silencing associated with long GAA•TTC repeat in FXN intron 1.
Recently, Pook and colleagues have investigated the long-term effects of three 2-amiobenazmide HDAC inhibitors, 106, 109, and 136 (Figure 1), in a second GAA repeat expansion mouse model.45 The YG8R mouse model harbors a human Friedreich ataxia locus with expanded repeats and shows reduced levels of frataxin messenger RNA, protein, heterochromatin formation at the repeats, neuromotor deficits, and neuronal pathology.32 This group reported no overt toxicity during 5 months of treatment, and 2 compounds, 109 and 106, each produced an improvement of motor coordination, whereas 109 and 136 produced increased locomotor activity. All 3 compounds increased global histone H3 and H4 acetylation of brain tissue, but only 109 significantly increased acetylation of specific histone residues at the FXN locus. Histone deacetylase inhibitor 109 significantly increased frataxin protein expression in brain tissue and produced significant increases in brain aconitase enzyme activity, together with reduction of neuronal pathology of the dorsal root ganglia. Taken together, the results in mouse models support the use of 2-aminobenzamides as therapeutics for Friedreich ataxia.
Identification of the Histone Deacetylase Target of the 2-aminobenzamide Histone Deacetylase Inhibitors
Histone deacetylase inhibitor 106 (Figure 1) was screened against a panel of 10 class I and class II recombinant human histone deacetylase enzymes, expressed in baculovirus. We find that 106 is a class I histone deacetylase inhibitor, with a marked preference for histone deacetylase enzyme 3, with little or no activity against class II histone deacetylases.48 To elucidate any potential difference between the 2-aminobenzamides and the hydoxamates, exemplified by suberoylanilide hydroxamic acid and trichostatin A, we determined Kis for 106 and suberoylanilide hydroxamic acid with each of the class I histone deacetylase enzymes and explored the mechanisms for inhibition exhibited by these compounds.48 Strikingly, we find that suberoylanilide hydroxamic acid and trichostatin A are rapid-on/rapid-off, classical competitive inhibitors, but compound 106 inhibits histone deacetylase enzymes 1 and 3 through a slow-on/slow-off mechanism, with a ∼10-fold preference for histone deacetylase enzyme 3 over histone deacetylase enzyme 1, and much lower activity against either histone deacetylase enzyme 2 or 8 (see 48).
Previous studies have established that benzamide-type histone deacetylase inhibitors are selective for class I histone deacetylase enzymes, and, in particular, MS-275 and other o-aminobenzamides show a ∼4 to 10-fold preference for histone deacetylase enzyme 1 over histone deacetylase enzyme 3;49-51 thus, 106 is one of the first examples of a histone deacetylase inhibitor that shows selectivity for histone deacetylase enzyme 3 over all other class I histone deacetylases. We also examined the cellular histone deacetylase inhibition activities of suberoylanilide hydroxamic acid and 106 in the Friedreich ataxia lymphoblast cell line.48 Both compounds are highly active as general histone deacetylase inhibitors in this cell line, showing increased global acetylation of histone H3. However, after washing cells free of the compounds, acetylated histones are rapidly lost in the suberoylanilide hydroxamic acid-treated cells, but acetylation persists for several hours in the 106-treated cells, paralleling the in vitro activity described above. We also showed that 106 was a potent inducer of frataxin protein in these cells, but suberoylanilide hydroxamic acid showed no such activity.48 Thus, the active 2-aminobenzamides differ from hydroxamates in their mechanism of inhibition of class I histone deacetylases, and this difference could well account for the efficacy of this class of compounds in reactivation of silent FXN alleles in Friedreich ataxia cells and mouse models.
Proteomic Approaches for Target Identification
We synthesized an activity-profiling probe for proteomic studies aimed at identification of the histone deacetylase target of our compounds in cell extracts.52,53 This approach has recently been employed for the identification of the histone deacetylase targets of suberoylanilide hydroxamic acid,54 and histone deacetylases 1 and 2 were identified, as would be expected from previous studies with this compound.55 Our trifunctional probe (1-BP, Figure 3) consists of a benzophenone photolabeling group, which is attached through a flexible ethylene glycol linker to 4b/106,3 and an alkyne for subsequent attachment of a reporter dye or biotin for affinity capture by click chemistry. Importantly, compared with the parent compound 106, 1-BP retains comparable histone deacetylase inhibitory activity against recombinant histone deacetylases. For target identification, we incubated 1-BP with 6 different recombinant histone deacetylase enzymes (class I histone deacetylase 1, 2, 3, and 8; and 2 representative class II histone deacetylases 4 and 5), each expressed in baculovirus. Histone deacetylase 3 was expressed along with its required cofactor, N-CoR. After irradiation at 350 nm to effect photocrosslinking, a fluorescent dye (rhodamine)-azide was coupled to the probe by solution-phase Cu(I)-catalyzed “click” chemistry, and proteins were analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis and fluorescence imaging (see Figure 2 of 56). This experiment clearly showed that, at least among these 6 enzymes, 1-BP exhibits a clear preference for histone deacetylase 3/N-CoR, with little activity against other class I histone deacetylases (1, 2, or 8) or the class II histone deacetylases 4 and 5. Crosslinking to histone deacetylase 3 is competed by pre-incubation with the parent compound 106.56 Identification of histone deacetylase 3/N-CoR as a preferred target for 1-BP is in agreement with the Ki values measured for the parent compound 106 with recombinant histone deacetylase enzymes, as described above.48
Figure 3.
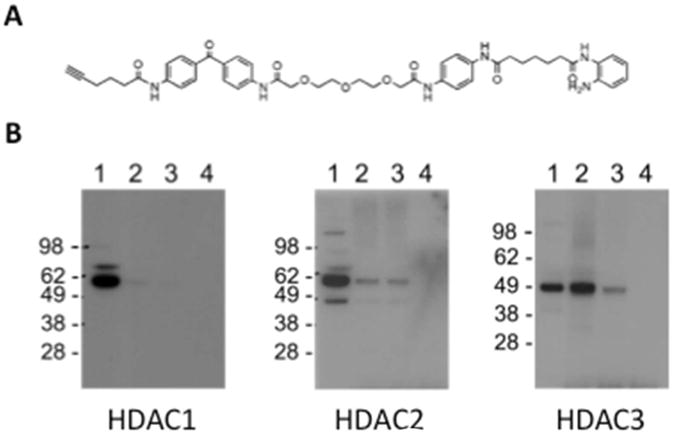
(A) Trifunctional probe for activity-profiling, 1-BP, containing an alkyne for click chemistry and a benzophenone for protein cross-linking. The histone deacetylase inhibitor is attached by an ethylene glycol linker. (B) Photoaffinity labeling of proteins in a nuclear extract from Friedreich ataxia lymphoblasts with 1-BP followed by addition of a biotin-azide by “click” chemistry, streptavidin capture, and Western blotting with antibody to the indicated histone deacetylase inhibitors. Lane 1, input (2% of total, relative to lanes 2 - 4); lane 2, proteins retained on streptavin beads; lane 3, same as lane 2 but with pre-incubation of a 20-fold excess of 106 prior to the addition of 106-BP to the extract; lane 4, no click chemistry control. Taken from Xu and colleagues,56 with permission. Abbreviation: HDAC, histone deacetylase.
We next sought to identify targets of 1-BP in cell extracts. After incubation of 1-BP in a nuclear extract derived from a Friedreich ataxia lymphoblastoid cell line and photocrosslinking, a biotin tag was appended to the inhibitor-photolabeling conjugate through Cu(I)-mediated “click” reaction of a biotin-azide. Streptavidin beads were then used for affinity capture of the histone deacetylase target, and Western blotting with antibodies to various histone deacetylase enzymes was used for target identification. Figure 3b shows that histone deacetylase 3 is indeed cross-linked by 1-BP and retained by the streptavidin beads. Western blotting with antibodies to the other class I histone deacetylases 1 and 2 fail to show strong cross-linking (Figure 3b), in agreement with results with recombinant histone deacetylases. Importantly, preincubation of the extract with the parent compound 106 abolishes the histone deacetylase 3 signal in this experiment (Figure 3b, lane 3), demonstrating the specificity of the reaction. Omission of the “click” reagent also abolished retention of histone deacetylase 3 on streptavidin beads (lane 4). Although these experiments were performed with a nuclear extract from Friedreich ataxia lymphoblasts, histone deacetylase 3 is known to be present in the brain, and in particular in the cerebellum (see Allen Brain Atlas: www.brain-map.org; and 57), attesting to the potential relevance of histone deacetylase 3 in Friedreich ataxia pathogenesis. Recent studies have demonstrated targeting of 1-BP to histone deacetylase 3 in the mouse brain in vivo (Xu and colleagues, in preparation).
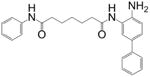
Testing Histone Deacetylase Inhibitors With Other Selectivity Profiles as FXN Gene Activators
While we find that potent histone deacetylase 3-selective inhibitors are the most active inducers of FXN expression in Friedreich ataxia patient lymphocytes, we recently identified potent and selective inhibitors of histone deacetylases 1 and 2, and tested whether these compounds would activate FXN expression in Friedreich ataxia cells.56 Our synthesis of these histone deacetylase 1/2 selective compounds stems from a recent study from the Merck group;58 on the basis of this work, we expected that appending a phenyl group at the 5-position of the “right” hand ring of 106 would generate a compound with specificity for histone deacetylase 1/2 over histone deacetylase 3. This notion was based on molecular modeling, where the 5-phenyl was predicted to clash with a tyrosine found in histone deacetylase 3, where a non-interfering serine would occupy a similar position in histone deacetylase 1/2.58
This expectation is fully borne out in Ki measurements (Table 1). This compound has a ∼350-fold preference for histone deacetylase 1 over histone deacetylase 3, is similarly active against histone deacetylase 2, and is active as a histone deacetylase inhibitor in Friedreich ataxia cells.56 We next assessed whether this histone deacetylase 1/2-selective compound would increase FXN messenger RNA in primary lymphocytes from patients with Friedreich ataxia. Our results showed that compared with histone deacetylase 3-selective compounds, this compound is only weakly active in lymphocytes from patients with Friedreich ataxia. In addition, we have synthesized a benzophenone activity-profiling probe and we find that this compound does indeed physically interact with histone deacetylase 1 in cell extracts.56 We also find that potent inhibitors of class II and class III (sirtuins) histone deacetylases fail to activate FXN in our cellular models (Table 1). Although our histone deacetylase inhibition and target identification experiments point to histone deacetylase 3 as the relevant histone deacetylase isotype involved in FXN silencing, additional studies will be needed to verify the role of this enzyme in Friedreich ataxia pathogenesis. We are currently pursuing this objective through chromatin immunoprecipitation and small interfering RNA approaches.
Table 1. Testing Various Selective HDAC Inhibitors as Activators of FXN Gene Transcription.
Refer to additional document
Quantitative reverse transcriptase polymerase chain reaction was used to measure FXN messenger RNA levels after treatment with 10 μM compound in Friedreich ataxia lymphoid cells. Abbreviations: HDAC, histone deacetylase; PCR, polymerase chain reaction
| Target/Class | Compound Structure | Ki or IC50 | FXN transcription |
|---|---|---|---|
| HDAC1/2 |
|
Ki = 7 nM HDAC1 Ki = 2.5 μM HDAC3 |
Weakly active |
| HDAC3 |
|
Ki = 14 nM HDAC3 Ki = 148 nM HDAC1 |
Highly active |
| Class II |
|
IC50 ∼ 1 μM class II HDACs | Inactive |
| Sirtuins |
|
IC50 = 100 nM Sirt1 IC50 = 20 μM Sirt2 IC50 = 50 μM Sirt3 |
Inactive |
Generation of Compounds with Improved Pharmacological Properties
The 2-aminobenzamides discussed above suffer from 2 liabilities that limit their potential for actual use as human therapeutics for Friedreich ataxia; namely, less than optimal brain penetration and conversion of the active molecule into an inactive metabolic product under the acidic conditions of the stomach and in serum. For example, on subcutaneous injection of histone deacetylase inhibitor 109 in rodents, this molecule has only a 10% to 15% brain concentration compared with serum. In addition, the 2-aminobenzamides are converted to an inactive benzimidazole in vivo. Through a medicinal chemistry effort at Repligen, two structural features that individually improve brain distribution and metabolic stability have been identified; namely, replacement of the “left” amide with an ether, olefin, or ketone to improve brain penetration and introduction of an unsaturated linkage adjacent to the “right” amide to prevent formation of a benzimidazole metabolic byproduct (Figure 4a). On the basis of these results, we devised and synthesized a new lead compound click-1 using Cu(I)-catalyzed click chemistry (Figure 4b). This synthetic route allows for the generation of compounds containing both modifications mentioned above, but introduces a triazole into the aliphatic linker region of the standard pimelic 2-aminobenzamide scaffold. Initially, we did not know whether a heterocycle in the linker would retain activity compared to the active parent molecules, exemplified by 106, etc. (Figure 1).
Figure 4.
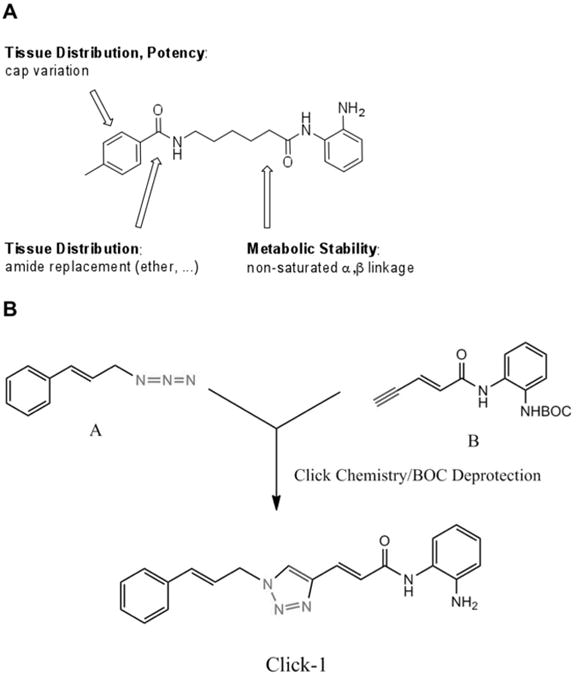
Compounds with improved pharmacological properties. (A) Brain penetration can be improved by elimination of the left amide, and replacement with an ether, olefin, or ketone. Metabolic stability can be improved by introducing a non-saturated α/β linkage adjacent to the right amide, which prevents formation of a benzimidazole. (B) Synthetic route to compounds with these replacements using Cu(I)-catalyzed click chemistry, where azide A is reacted with alkyne B, and after Boc deprotection, a triazole is generated in the linker region of the histone deacetylase inhibitor.59
We therefore monitored click-1 for its activity against recombinant histone deacetylases (histone deacetylase 1, 2, and 3) in vitro, in-cell histone deacetylase activity, and activity in restoring FXN transcription in patient cells. We find that click-1 has comparable activity to histone deacetylase inhibitor 106 or 109 in these assays.59 Blood-brain barrier penetration was measured in the rat for compound 109 and click-1. Brain penetration (as measured by brain/plasma ratio at tmax) was determined to be 0.15 for 109 and 0.33 for click-1 (Cmax: 800 ng/g in the brain at Tmax = 5 min post-dose [5 mg/kg IV rat]), representing a significant increase in brain penetration for click-1 compared with the standard 2-aminobenzamide 109. The half-life of the compounds in acidic conditions was used to quantify their relative stability. At pH = 2 and 50 °C, t1/2; = 6 hours for 109 versus t1/2 = 33 hours for click-1, representing a 5.5-fold improvement relative to histone deacetylase inhibitor 109. These results demonstrate that click-1 has improved acid stability and better brain penetration, through placing a double bond next to the right amide bond and removing the left amide. These modifications may therefore lead to a new generation of compounds for clinical use.
Future Directions and Clinical Studies
Full preclinical assessment of a lead clinical compound (109/RG2833; Repligen Corporation, Waltham, Massachusetts) has been accomplished and an Investigational New Drug application has been filed with the US Food and Drug Administration for initiation of a phase I clinical trial of RG2833 in man. Additionally, Repligen has received Orphan Drug status for its clinical candidate. Clinical studies will determine both safety and in vivo efficacy, at least in terms of increases in frataxin expression in peripheral blood mononuclear cells taken from patients after dosing. Such information will provide a proof of principle for initiating the clinical efficacy stage of clinical studies. If oral delivery of a histone deacetylase inhibitor can be effective at drug exposures that are well-tolerated, it will provide impetus to further advance the 2-aminobenzamide class of compounds to target histone deacetylase inhibition as a viable therapeutic strategy for this devastating disease.
Acknowledgments
This paper is based in part on a presentation given at the Neurobiology of Disease in Children Symposium: Childhood Ataxia, in conjunction with the 40th Annual Meeting of the Child Neurology Society, Savannah, Georgia, October 26, 2011. Supported by grants from the National Institutes of Health (2R13NS040925-14 Revised), the National Institutes of Health Office of Rare Diseases Research, the Child Neurology Society, and the National Ataxia Foundation. We thank Melanie Fridl Ross, MSJ, ELS, for editing assistance.
Funding: Studies in our laboratories have been supported by grants from the National Institute of Neurological Disorders and Stroke, National Institutes of Health (to Dr Gottesfeld), the Friedreich's Ataxia Research Alliance (Dr Xu and Repligen), GoFAR (Dr Soragni and Repligen), Ataxia UK (Dr Soragni), Friedreich's Ataxia Society Ireland (Dr Soragni), and the Muscular Dystrophy Association (Repligen Corporation).
Footnotes
Declaration of Conflicting Interests: Drs Plasterer, Jacques, and Rusche are employees of Repligen Corporation and Dr Gottesfeld serves as a consultant to Repligen.
References
- 1.Schmucker S, Puccio H. Understanding the molecular mechanisms of Friedreich's ataxia to develop therapeutic approaches. Hum Mol Genet. 2010;19(R1):R103–R110. doi: 10.1093/hmg/ddq165. [DOI] [PubMed] [Google Scholar]
- 2.Saveliev A, Everett C, Sharpe T, et al. DNA triplet repeats mediate heterochromatinprotein-1-sensitive variegated gene silencing. Nature. 2003;422(6934):909–913. doi: 10.1038/nature01596. [DOI] [PubMed] [Google Scholar]
- 3.Herman D, Jenssen K, Burnett R, et al. Histone deacetylase inhibitors reverse gene silencing in Friedreich's ataxia. Nature Chem Biol. 2006;2:551–558. doi: 10.1038/nchembio815. [DOI] [PubMed] [Google Scholar]
- 4.Pandolfo M. Friedreich ataxia. Semin Pediatr Neurol. 2003;10(3):163–172. doi: 10.1016/s1071-9091(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 5.Delatycki MB, Williamson R, Forrest SM. Friedreich ataxia: an overview. J Med Genet. 2000;37(1):1–8. doi: 10.1136/jmg.37.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsou AY, Paulsen EK, Lagedrost SJ, et al. Mortality in Friedreich ataxia. J Neurol Sci. 2011;307(1-2):46–49. doi: 10.1016/j.jns.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 7.Ye H, Rouault TA. Human iron-sulfur cluster assembly, cellular iron homeostasis, and disease. Biochemistry. 2010;49(24):4945–4956. doi: 10.1021/bi1004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meier T, Perlman SL, Rummey C, et al. Assessment of neurological efficacy of idebenone in pediatric patients with Friedreich's ataxia: data from a 6-month controlled study followed by a 12-month open-label extension study. J Neurol. 2012;259(2):284–291. doi: 10.1007/s00415-011-6174-y. Epub 2011 July 22. [DOI] [PubMed] [Google Scholar]
- 9.Velasco-Sanchez D, Aracil A, Montero R, et al. Combined therapy with idebenone and deferiprone in patients with Friedreich's ataxia. Cerebellum. 2011;10(1):1–8. doi: 10.1007/s12311-010-0212-7. [DOI] [PubMed] [Google Scholar]
- 10.Gottesfeld JM. Small molecules affecting transcription in Friedreich ataxia. Pharmacol Ther. 2007 Nov;116(2):236–248. doi: 10.1016/j.pharmthera.2007.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sturm B, Stupphann D, Kaun C, et al. Recombinant human erythropoietin: effects on frataxin expression in vitro. Eur J Clin Invest. 2005;35(11):711–717. doi: 10.1111/j.1365-2362.2005.01568.x. [DOI] [PubMed] [Google Scholar]
- 12.Acquaviva F, Castaldo I, Filla A, et al. Recombinant human erythropoietin increases frataxin protein expression without increasing mRNA expression. Cerebellum. 2008;7(3):360–365. doi: 10.1007/s12311-008-0036-x. [DOI] [PubMed] [Google Scholar]
- 13.Rufini A, Fortuni S, Arcuri G, et al. Preventing the ubiquitin-proteasome-dependent degradation of frataxin, the protein defective in Friedreich's ataxia. Hum Mol Genet. 2011;20(7):1253–1261. doi: 10.1093/hmg/ddq566. [DOI] [PubMed] [Google Scholar]
- 14.Vyas PM, Tomamichel WJ, Pride PM, et al. A TAT-Frataxin fusion protein increases lifespan and cardiac function in a conditional Friedreich's ataxia mouse model. Hum Mol Genet. 2012;21(6):1230–1247. doi: 10.1093/hmg/ddr554. Epub 2011 Nov 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim F, Palomo GM, Mauritz C, et al. Functional recovery in a Friedreich's ataxia mouse model by frataxin gene transfer using an HSV-1 amplicon vector. Mol Ther. 2007;15:1072–1078. doi: 10.1038/sj.mt.6300143. [DOI] [PubMed] [Google Scholar]
- 16.Kumari D, Usdin K. Chromatin remodeling in the noncoding repeat expansion diseases. J Biol Chem. 2009;284(12):7413–7417. doi: 10.1074/jbc.R800026200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bidichandani SI, Ashizawa T, Patel PI. The GAA triplet-repeat expansion in Friedreich ataxia interferes with transcription and may be associated with an unusual DNA structure. Am J Hum Genet. 1998;62(1):111–121. doi: 10.1086/301680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baralle M, Pastor T, Bussani E, Pagani F. Influence of Friedreich ataxia GAA noncoding repeat expansions on pre-mRNA processing. Am J Hum Genet. 2008;83(1):77–88. doi: 10.1016/j.ajhg.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zoghbi HY, Orr HT. Trinucleotide repeat disorders. Ann Rev Neurosci. 2007;30:575–621. doi: 10.1146/annurev.neuro.29.051605.113042. [DOI] [PubMed] [Google Scholar]
- 20.De Biase I, Chutake YK, Rindler PM, Bidichandani SI. Epigenetic silencing in Friedreich ataxia is associated with depletion of CTCF (CCCTC-binding factor) and antisense transcription. PLoS One. 2009;4(11):e7914. doi: 10.1371/journal.pone.0007914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He Y, Vogelstein B, Velculescu VE, et al. The antisense transcriptomes of human cells. Science. 2008;322:1855–1857. doi: 10.1126/science.1163853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakamoto N, Chastain PD, Parniewski P, et al. Sticky DNA: self-association properties of long GAA.TTC repeats in R.R.Y triplex structures from Friedreich's ataxia. Mol Cell. 1999;3(4):465–475. doi: 10.1016/s1097-2765(00)80474-8. [DOI] [PubMed] [Google Scholar]
- 23.Ohshima K, Montermini L, Wells RD, Pandolfo M. Inhibitory effects of expanded GAA.TTC triplet repeats from intron I of the Friedreich ataxia gene on transcription and replication in vivo. J Biol Chem. 1998;273(23):14588–14595. doi: 10.1074/jbc.273.23.14588. [DOI] [PubMed] [Google Scholar]
- 24.Sakamoto N, Ohshima K, Montermini L, et al. Sticky DNA, a self-associated complex formed at long GAA*TTC repeats in intron 1 of the frataxin gene, inhibits transcription. J Biol Chem. 2001;276(29):27171–27177. doi: 10.1074/jbc.M101879200. [DOI] [PubMed] [Google Scholar]
- 25.Grabczyk E, Usdin K. Alleviating transcript insufficiency caused by Friedreich's ataxia triplet repeats. Nucleic Acids Res. 2000;28(24):4930–4937. doi: 10.1093/nar/28.24.4930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grabczyk E, Usdin K. The GAA*TTC triplet repeat expanded in Friedreich's ataxia impedes transcription elongation by T7 RNA polymerase in a length and supercoil dependent manner. Nucleic Acids Res. 2000;28(14):2815–2822. doi: 10.1093/nar/28.14.2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krasilnikova MM, Kireeva ML, Petrovic V, et al. Effects of Friedreich's ataxia (GAA)n*(TTC)n repeats on RNA synthesis and stability. Nuc Acids Res. 2007;35:1075–1084. doi: 10.1093/nar/gkl1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elgin SC, Grewal SI. Heterochromatin: silence is golden. Curr Biol. 2003;13(23):R895–R898. doi: 10.1016/j.cub.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Greene E, Mahishi L, Entezam A, et al. Repeat-induced epigenetic changes in intron 1 of the frataxin gene and its consequences in Friedreich ataxia. Nucl Acids Res. 2007;35:3383–3390. doi: 10.1093/nar/gkm271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumari D, Biacsi RE, Usdin K. Repeat expansion affects both transcription initiation and elongation in friedreich ataxia cells. J Biol Chem. 2011;286(6):4209–4215. doi: 10.1074/jbc.M110.194035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim E, Napierala M, Dent SY. Hyperexpansion of GAA repeats affects post-initiation steps of FXN transcription in Friedreich's ataxia. Nucleic Acids Res. 2011;39(19):8366–8377. doi: 10.1093/nar/gkr542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Mahdawi S, Pinto RM, Ismail O, et al. The Friedreich ataxia GAA repeat expansion mutation induces comparable epigenetic changes in human and transgenic mouse brain and heart tissues. Hum Mol Genet. 2008;17(5):735–746. doi: 10.1093/hmg/ddm346. [DOI] [PubMed] [Google Scholar]
- 33.Rai M, Soragni E, Jenssen K, et al. HDAC inhibitors correct frataxin deficiency in a Friedreich ataxia mouse model. PLoS ONE. 2008;3:e1958. doi: 10.1371/journal.pone.0001958. doi:1910.1371/journal.pone.0001958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Punga T, Buhler M. Long intronic GAA repeats causing Friedreich ataxia impede transcription elongation. EMBO Mol Med. 2010;2(4):120–129. doi: 10.1002/emmm.201000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castaldo I, Pinelli M, Monticelli A, et al. DNA methylation in intron 1 of the frataxin gene is related to GAA repeat length and age of onset in Friedreich ataxia patients. J Med Genet. 2008;45(12):808–812. doi: 10.1136/jmg.2008.058594. [DOI] [PubMed] [Google Scholar]
- 36.El-Osta A, Wolffe AP. DNA methylation and histone deacetylation in the control of gene expression: basic biochemistry to human development and disease. Gene Expr. 2000;9:63–75. doi: 10.3727/000000001783992731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Di Prospero NA, Fischbeck KH. Therapeutics development for triplet repeat expansion diseases. Nat Rev Genet. 2005;6(10):756–765. doi: 10.1038/nrg1690. [DOI] [PubMed] [Google Scholar]
- 38.Langley B, Gensert JM, Beal MF, Ratan RR. Remodeling chromatin and stress resistance in the central nervous system: histone deacetylase inhibitors as novel and broadly effective neuroprotective agents. Curr Drug Targets CNS Neurol Disord. 2005;4(1):41–50. doi: 10.2174/1568007053005091. [DOI] [PubMed] [Google Scholar]
- 39.Kernochan LE, Russo ML, Woodling NS, et al. The role of histone acetylation in SMN gene expression. Hum Mol Genet. 2005;14(9):1171–1182. doi: 10.1093/hmg/ddi130. [DOI] [PubMed] [Google Scholar]
- 40.Tapscott SJ, Klesert TR, Widrow RJ, et al. Fragile-X syndrome and myotonic dystrophy: parallels and paradoxes. Curr Opin Genet Dev. 1998;8(2):245–253. doi: 10.1016/s0959-437x(98)80148-2. [DOI] [PubMed] [Google Scholar]
- 41.Cho DH, Thienes CP, Mahoney SE, et al. Antisense transcription and heterochromatin at the DM1 CTG repeats are constrained by CTCF. Mol Cell. 2005;20(3):483–489. doi: 10.1016/j.molcel.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 42.Kazantsev AG, Thompson LM. Therapeutic application of histone deacetylase inhibitors for central nervous system disorders. Nat Rev Drug Discov. 2008;7:854–868. doi: 10.1038/nrd2681. [DOI] [PubMed] [Google Scholar]
- 43.Drummond DC, Noble CO, Kirpotin DB, et al. Clinical development of histone deacetylase inhibitors as anticancer agents. Ann Rev Pharmacol Toxicol. 2005;45:495–528. doi: 10.1146/annurev.pharmtox.45.120403.095825. [DOI] [PubMed] [Google Scholar]
- 44.Rai M, Soragni E, Chou CJ, et al. Two new pimelic diphenylamide HDAC inhibitors induce sustained frataxin upregulation in cells from Friedreich's ataxia patients and in a mouse model. PLoS One. 2010;5(1):e8825. doi: 10.1371/journal.pone.0008825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sandi C, Pinto RM, Al-Mahdawi S, et al. Prolonged treatment with pimelic o-aminobenzamide HDAC inhibitors ameliorates the disease phenotype of a Friedreich ataxia mouse model. Neurobiol Dis. 2011;42(3):496–505. doi: 10.1016/j.nbd.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Soragni E, Xu C, Cooper A, Plasterer HL, et al. Evaluation of histone deacetylase inhibitors as therapeutics for neurodegenerative diseases. Methods Mol Biol. 2011;793:495–508. doi: 10.1007/978-1-61779-328-8_32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miranda CJ, Santos MM, Ohshima K, et al. Frataxin knockin mouse. FEBS Lett. 2002;512(1-3):291–297. doi: 10.1016/s0014-5793(02)02251-2. [DOI] [PubMed] [Google Scholar]
- 48.Chou CJ, Herman D, Gottesfeld JM. Pimelic diphenylamide 106 is a slow, tight-binding inhibitor of class I histone deacetylases. J Biol Chem. 2008;283:35402–35409. doi: 10.1074/jbc.M807045200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beckers T, Burkhardt C, Wieland H, et al. Distinct pharmacological properties of second generation HDAC inhibitors with the benzamide or hydroxamate head group. Int J Cancer. 2007;121:1138–1148. doi: 10.1002/ijc.22751. [DOI] [PubMed] [Google Scholar]
- 50.Hu E, Dul E, Sung CM, et al. Identification of novel isoform-selective inhibitors within class I histone deacetylases. J Pharmacol Exp Ther. 2003;307(2):720–728. doi: 10.1124/jpet.103.055541. [DOI] [PubMed] [Google Scholar]
- 51.Siliphaivanh P, Harrington P, Witter DJ, et al. Design of novel histone deacetylase inhibitors. Bioorg Med Chem Lett. 2007;17(16):4619–4624. doi: 10.1016/j.bmcl.2007.05.080. [DOI] [PubMed] [Google Scholar]
- 52.Evans MJ, Cravatt BF. Mechanism-based profiling of enzyme families. Chem Rev. 2006;106(8):3279–3301. doi: 10.1021/cr050288g. [DOI] [PubMed] [Google Scholar]
- 53.Hagenstein MC, Sewald N. Chemical tools for activity-based proteomics. J Biotechnol. 2006;124(1):56–73. doi: 10.1016/j.jbiotec.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 54.Salisbury CM, Cravatt BF. Activity-based probes for proteomic profiling of histone deacetylase complexes. Proc Natl Acad Sci USA. 2007;104(4):1171–1176. doi: 10.1073/pnas.0608659104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marks P, Rifkind RA, Richon VM, et al. Histone deacetylases and cancer: causes and therapies. Nat Rev Cancer. 2001;1(3):194–202. doi: 10.1038/35106079. [DOI] [PubMed] [Google Scholar]
- 56.Xu C, Soragni E, Chou CJ, et al. Chemical probes identify a role for histone deacetylase 3 in Friedreich's ataxia gene silencing. Chem Biol. 2009;16:980–989. doi: 10.1016/j.chembiol.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Broide RS, Redwine JM, Aftahi N, et al. Distribution of histone deacetylases 1-11 in the rat brain. J Mol Neurosci. 2007;31(1):47–58. doi: 10.1007/BF02686117. [DOI] [PubMed] [Google Scholar]
- 58.Methot JL, Chakravarty PK, Chenard M, et al. Exploration of the internal cavity of histon deacetylase (HDAC) with selective HDAC1/HDAC2 inhibitors (SHI-1:2) Bioorg Med Chem Lett. 2008;18(3):973–978. doi: 10.1016/j.bmcl.2007.12.031. [DOI] [PubMed] [Google Scholar]
- 59.Xu C, Soragni E, Jacques V, et al. Improved histone deacetylase inhibitors as therapeutics for the neurodegenerative disease Friedreich's ataxia: a new synthetic route. Pharmaceuticals. 2011;4(12):1578–1590. doi: 10.3390/ph4121578. [DOI] [PMC free article] [PubMed] [Google Scholar]