Abstract
Petrous apex cholesterol granulomas (PACG) are uncommon lesions. Recurrence following transcranial or endonasal approaches to aerate the cyst occurs in up to 60% of cases. We describe the technical nuances pertinent to the endonasal endoscopic management of a recurrent symptomatic PACG and review the literature. A 19-year-old woman presented with a recurrent right abducens nerve paresis. Four months prior, she underwent an endonasal transsphenoidal surgery (TSS) for drainage of a symptomatic PACG. Current imaging documented recurrence of the right PACG. Transsphenoidal and infrapetrous approaches were performed to obtain a wider bony opening along the petrous apex and drain the cyst. A Doyle splint was inserted into the cyst's cavity and extended out into the sphenoid, maintaining patency during the healing process. Three months after surgery, the splint was removed endoscopically, allowing visualization of a patent cylindrical communication between both aerated cavities. The patient remains symptom- and recurrence-free. Endoscopic endonasal surgery must be adapted to manage recurrent PACG. A TSS may not be sufficient. An infrapetrous approach with wider bony opening, extensive removal of the cyst's anterior wall, and use of a stent are indicated for the treatment of recurrent PACG and to prevent recurrences.
Keywords: Cholesterol granuloma, petrous apex, endoscopy, transsphenoidal approach, expanded endonasal approach
Cholesterol granulomas are inflammatory lesions that occur rarely in the petrous apex.1 Initially, these lesions tend to remain asymptomatic. As they expand, headaches and cranial neuropathies may arise.1,2 The treatment of symptomatic petrous apex cholesterol granuloma (PACG) is surgical drainage of the cyst and permanent aeration of petrous apex air cells to prevent recurrence.1,3 Several transcranial approaches have been used to treat these lesions, the choice of which depends on the patient's preoperative hearing status and the lesion's location in relation to critical neurovascular structures.2,3,4,5 These traditional lateral skull base approaches expose the inner ear and facial nerve to potential structural damage as well as add morbidities of any intracranial procedure.4 They also have the shortcoming of often producing a relatively narrow bony opening, potentially compromising long-term drainage and preventing the use of stents between the aerated cavity and the sphenoid sinus. In addition to having recurrence rates as high as 60%, repeat transcranial surgeries for recurrent lesions may be associated with significant morbidities.2,3 Recently, the endoscopic endonasal approach has gained popularity in the neurosurgical community. This less invasive approach is attractive for the initial surgical management of symptomatic PACG and possibly even more so for symptomatic recurrent PACG.
In this report, we describe a case of recurrent symptomatic PACG treated by an expanded endonasal approach. We review all reported cases treated by an endoscopic endonasal approach and attempt to establish management pearls regarding the endoscopic endonasal management of PACG.
Case Report and Technique Description
A 19-year-old woman presented with an ongoing severe headache of subacute onset and 3-day history of diplopia. Physical examination was unremarkable except for right abducens nerve palsy. Head computed tomography scan demonstrated expansion of the right petrous apex. Magnetic resonance imaging showed a right petrous apex mass measuring 25 × 14 × 14 mm abutting the posterior wall of the sphenoid sinus. The lesion was hyperintense on both T1- and T2-weighted images and did not enhance following gadolinium administration (Fig. 1). Given her rapid onset of symptoms, surgical drainage was recommended.
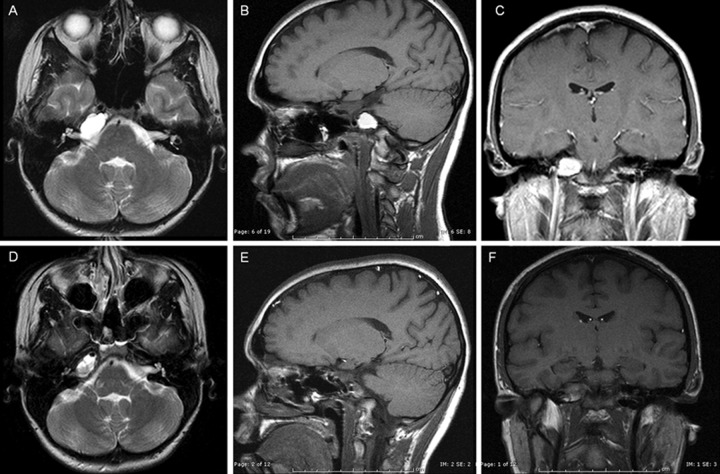
Figure 1.
Preoperative and postoperative magnetic resonance T2-weighted axial images (A, D), T1-weighted sagittal images (B, E), and T1-weighted postgadolinium coronal images (C, F).
The patient underwent an endonasal transsphenoidal approach using intermittently the operating microscope and the endoscope for visualization. The location of the lesion was confirmed in the lower inferior right aspect of the sphenoid sinus with intraoperative neuronavigation. After creating a wide bony opening to the face of the cholesterol granuloma, its capsule was incised. Characteristic greenish fluid with cholesterol crystals poured forth. After satisfactory drainage, the bony opening was widened and multiple fragments of the capsule were removed. Final inspection of the cyst's cavity showed complete drainage of the lesion. Postoperatively, symptoms progressively resolved.
Four months after initial surgery, clinicoradiological recurrence occurred and mandated a repeat transsphenoidal and infrapetrous approach (Fig. 2). After removing scar tissue from the prior bony opening in the sphenoid floor, care was taken to identify the vertical and horizontal segments of the internal carotid artery. The high-speed drill was used to widen the bony opening inferior to the petrous carotid into the petrous apex in a medial and inferior direction. Once exposed on a large surface, the anterior wall of the cyst was removed, the content of the cyst was drained, and its lining partly removed. A 45-degree endoscope allowed visualization of the empty cavity (Fig. 3). A Doyle splint was inserted into the cyst's cavity on ∼1 cm and extended out into the sphenoid sinus, maintaining patency during the healing process. At 3 months after surgery, the Doyle splint was removed under endoscopic visualization. A healed cylindrical communication between the involved petrous apex cells and the sphenoid sinus was appreciated (Fig. 4). A rubber catheter was used to irrigate the aerated cavity. The patient currently remains symptom- and recurrence-free 15 months postoperatively.
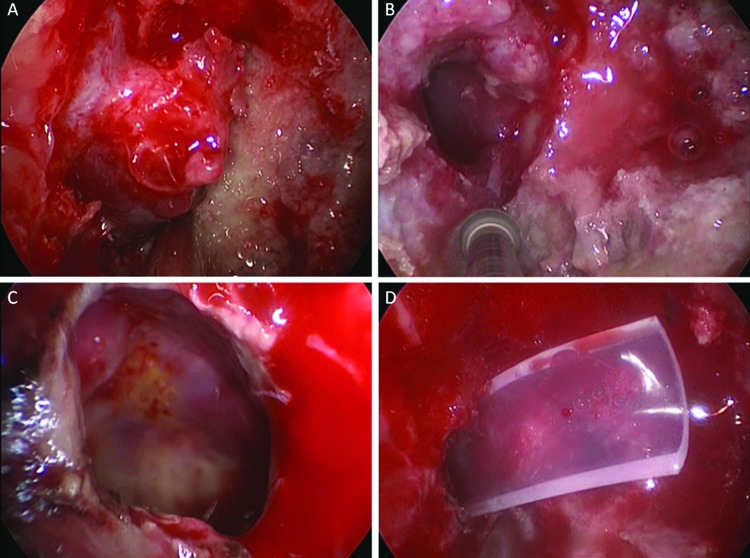
Figure 2.

Magnetic resonance images at clinical recurrence: T2-weighted axial image (A), T1-weighted sagittal image (B), and T1-weighted postgadolinium coronal image (C).
Figure 3.
Intraoperative view of the repeat transsphenoidal and infrapetrous approach. (A) Exposure of the petrous apex and cyst on a large surface. (B) Widening of the bony opening inferior to the petrous carotid into the petrous apex in a medial and inferior direction. (C) Visualization of the emptied cavity with a 45-degree endoscope. (D) Insertion of a Doyle splint into the cyst's cavity.
Figure 4.
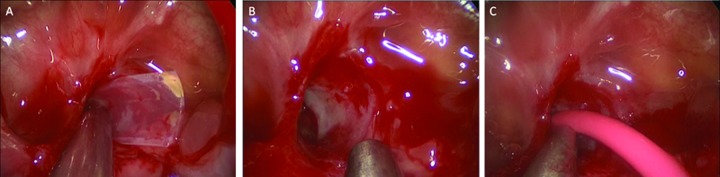
Intraoperative view of the removal of the Doyle splint with irrigation of the cavity.
Discussion
Cholesterol granulomas rarely occur in the petrous apex because the petrous apex is pneumatized in only 30% of temporal bones.6 They result from obstruction of the normal aeration of petrous apex air cells. This obstruction is believed to lead to negative pressure within the air cells, eventually causing mucosal edema, tissue breakdown, and hemorrhage and accumulation of breakdown products such as cholesterol.1,2 The cholesterol crystals induce a granulomatous inflammatory reaction resulting in the typical cholesterol granuloma.
For symptomatic patients, surgery is presently the only treatment option available. Surgical treatment implies cyst drainage, with or without removal of its lining, and restoration of air cell aeration. Some authors have also proposed complete excision of the lesion followed by obliteration of the cavity with vascularized tissue.2 Numerous transcranial approaches have been performed to treat PACG such as middle cranial fossa approaches and lateral skull base approaches including the translabyrinthine, infratrochlear, infralabyrinthine, transcochlear approaches.2,3,4,5 The specific approach recommended depends on the patient's hearing status and the cyst's location. Given the lateral trajectory of transcranial skull base approaches, they inevitably expose the inner ear and facial nerve to potential structural damage as well as add morbidities of any intracranial procedure.4,7
In addition, although satisfactory cyst drainage may be accomplished through these external routes, the bony opening obtained is often relatively narrow, rendering difficult intraoperative splinting techniques and potentially putting at risk chronic drainage. Indeed, recurrences have been reported to be as high as 60% irrespective of the transcranial approach used and degree of completeness of removal.2,3 Stenosis of the opening used to exteriorize the cyst may result in reaccumulation of its contents and recurrence of symptoms. Just as for initial procedures, revision transcranial surgeries for recurrent lesions may also be associated with significant morbidities.
Contemporary progresses in endoscopic surgery as well as in image-guidance technology have allowed treatment of PACG through a less invasive route. Petrous lesions located medial to the internal carotid artery (ICA) and that abut, protrude, or invade the sphenoid sinus may be safely approached through a transsphenoidal approach3,7,8,9,10,11,12,13 (Table 1). The use of the endoscope as visualization technique has enabled a more complete drainage of the cyst.14 The cyst cavity may be closely inspected under endoscopic visualization to remove septations between separate fluid loculations or any remote debris.14
Table 1. Summary of Reported Cases of Petrous Apex Cholesterol Granuloma Treated via the Endonasal Endoscopic Approach.
| Author | Age, Sex | Preoperative Symptoms | Location of CG in Relation to Sphenoid Sinus (SS) | Symptoms on Follow-Up (Length of Follow-Up, mo) | Procedure | Complication | Symptomatic Recurrence |
|---|---|---|---|---|---|---|---|
| Griffith and Terrell (1996)3 | 34, M | Disequilibrium | Protruding into the posterior SS, bony erosion | Asymptomatic (18) | TS drainage of cyst; wide opening of the cyst cavity | Transient epistaxis | None |
| 24, M | Hearing loss, V3 hypesthesia | Protruding into SS | Asymptomatic after 3rd OR (12) | 1st: subtemporal transzygomatic approach; 2nd: TS drainage of cyst; 3rd: TS drainage of cyst and wide opening of the cyst cavity | None | Recurrence 2 mo after 1st OR; recurrence 2 mo follow-up after 2nd OR; no recurrence after 3RD OR | |
| Michaelson et al (2001)8 | 13, F | H/A, VIth nerve palsy | Abutting the posterior SS | Asymptomatic (6) | TS drainage of cyst; wide opening of the cyst cavity; marsupialization | None | None |
| DiNardo et al (2003)9 | 62, F | Disequilibrium | Abutting the posterior SS, separated by a thin layer of bone | Asymptomatic (12) | TS drainage of cyst; wide opening of the cyst cavity | None | None |
| Presutti et al (2006)10 | 38, M | H/A, VIth nerve palsy, increasing vertigo | Abutting the posterolateral wall of the SS | Asymptomatic (3) | TS drainage of cyst; wide opening of the cyst cavity; placement of T-shaped stent | None | None |
| Oyama et al (2007)11 | 28, F | Hemifacial pain | Protruding in the posterior SS, separated by a thin layer of bone | Asymptomatic (24) | TS drainage of cyst; wide opening of the cyst cavity | None | None |
| Georgalas et al (2008)7 | 30, M | Facial palsy, sensorineural hearing loss, vertigo | Abutting the posterolateral SS | Asymptomatic (120) | TS drainage of cyst; wide opening of the cyst cavity; marsupialization | None | None |
| 13, M | H/A, VIth nerve palsy | Sphenopetrous lesion, almost completely obliterating SS | Asymptomatic (72) | 1st: middle fossa approach; 2nd: TS drainage of cyst; wide opening of the cyst cavity; marsupialization | None | Recurrence after 1st OR (time to recurrence not specified); no recurrence after 2nd OR | |
| 44, F | H/A | Protruding into the posterior SS | Asymptomatic (24) | TS drainage of cyst; wide opening of the cyst cavity; marsupialization | None | None | |
| Samadian et al (2009)12 | 28, F | H/A, VIth nerve palsy, hearing loss | Protruding in the posterior SS, separated by a thin layer of bone | Asymptomatic (48) | TS drainage of cyst; wide opening of the cyst cavity; marsupialization; placement of a Silicone tube drain | None | None |
| Zanation et al (2009)13 | 8 patients | All had H/A; 2 had occasional vertigo | No detail | No detail | TS: 2; TS with carotid lateralization: 3; IP approach: 3; drainage of cyst and stenting | None | One recurrence at 2.5 y after 1st OR |
| Present case | 19, F | H/A, VIth nerve palsy | Abutting the posterior SS | Asymptomatic to date (15) | 1st: TS drainage of cyst; wide opening of the cyst cavity; partial marsupialization; 2nd: TS and IP for drainage of cyst; very wide opening of the cyst cavity; marsupialization; placement of a Doyle stent | After 1st OR: delayed epistaxis | Recurrence 4 mo after 1st OR; no recurrence yet after 2nd OR |
CG, cholesterol granuloma; H/A, headache; IP, infrapetrous; mo, months; OR, operation; SS, sphenoid sinus; TS, transsphenoidal.
Including the present case, 19 cases of PACG have been treated through an endoscopic endonasal approach (Table 1).3,7,8,9,10,11,12,13 Sixteen of the 19 patients have been drained initially through a medial transsphenoidal approach (with or without lateralization of the ICA). Three of these 16 patients developed a symptomatic recurrence that required repeat surgery. The remaining three patients had been drained initially via an intrapetrous approach and did not develop a recurrence.13 Accordingly, 3 of 19 patients (15.7%) with PACG treated via an endonasal route presented a postoperative recurrence at 2, 4, and 30 months. This recurrence rate (15.7%) is significantly lower than that reported following other approaches (up to 60%). Several factors may contribute to this lower recurrence rate including a wider bony opening and, consequently, a more extensive removal of the cyst's anterior or medial wall, afforded by the endonasal endoscopic approaches (especially with the infrapetrous approach). In addition, the superior visualization of the cavity using angled endoscopes enables to assess and address remaining septations and/or debris and therefore optimizing the drainage.14 Furthermore, the use of a stent to preserve a drainage pathway throughout the healing process may contribute to reducing recurrences. This is especially important with the infrapetrous approach because the path of dissection is deeper than that performed in the medial transsphenoidal approach and therefore may be at greater risk of scarring.13 All of these considerations are of utmost importance when treating a recurrent PACG. We favor the endonasal endoscopic infrapetrous approach for recurrent PACG regardless of the initial surgical approach. In comparison to a transcranial surgery that may be associated with significant morbidity, no complications have yet occurred following endonasal endoscopic treatment for recurrent PACG.
Conclusion
Overall, the endoscopic endonasal route enables treatment of PACG through an anterior trajectory, preserving hearing and vestibular and facial function. This approach is significantly less invasive than traditional transcranial procedures with overall reduced morbidity, shortened procedure time, reduced hospital stay, better cosmetic results, and lower recurrence rates. It should be considered as the preferred surgical alternative for initial treatment of symptomatic PACG but also for the treatment of symptomatic recurrence, independently of the initial surgical route. Repeat endoscopic endonasal surgery must be adapted to recurrent PACG. The infrapetrous approach with wider bony opening, extensive anterior cyst wall removal, and use of a stent should be the treatment of choice for recurrent PACG.
References
- 1.Sincoff E H, Liu J K, Matsen L. et al. A novel treatment approach to cholesterol granulomas. Technical note. J Neurosurg. 2007;107:446–450. doi: 10.3171/JNS-07/08/0446. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg M B, Haddad G, Al-Mefty O. Petrous apex cholesterol granulomas: evolution and management. J Neurosurg. 1997;86:822–829. doi: 10.3171/jns.1997.86.5.0822. [DOI] [PubMed] [Google Scholar]
- 3.Griffith A J, Terrell J E. Transsphenoid endoscopic management of petrous apex cholesterol granuloma. Otolaryngol Head Neck Surg. 1996;114:91–94. doi: 10.1016/S0194-59989670289-9. [DOI] [PubMed] [Google Scholar]
- 4.Brackmann D E, Toh E H. Surgical management of petrous apex cholesterol granulomas. Otol Neurotol. 2002;23:529–533. doi: 10.1097/00129492-200207000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Terao T, Onoue H, Hashimoto T, Ishibashi T, Kogure T, Abe T. Cholesterol granuloma in the petrous apex: case report and review. Acta Neurochir (Wien) 2001;143:947–952. doi: 10.1007/s007010170026. [DOI] [PubMed] [Google Scholar]
- 6.Thedinger B A, Nadol J B Jr, Montgomery W W, Thedinger B S, Greenberg J J. Radiographic diagnosis, surgical treatment, and long-term follow-up of cholesterol granulomas of the petrous apex. Laryngoscope. 1989;99:896–907. doi: 10.1288/00005537-198909000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Georgalas C, Kania R, Guichard J P, Sauvaget E, Tran Ba Huy P, Herman P. Endoscopic transsphenoidal surgery for cholesterol granulomas involving the petrous apex. Clin Otolaryngol. 2008;33:38–42. doi: 10.1111/j.1749-4486.2007.01589.x. [DOI] [PubMed] [Google Scholar]
- 8.Michaelson P G, Cable B B, Mair E A. Image-guided transphenoidal drainage of a cholesterol granuloma of the petrous apex in a child. Int J Pediatr Otorhinolaryngol. 2001;57:165–169. doi: 10.1016/s0165-5876(00)00456-0. [DOI] [PubMed] [Google Scholar]
- 9.DiNardo L J, Pippin G W, Sismanis A. Image-guided endoscopic transsphenoidal drainage of select petrous apex cholesterol granulomas. Otol Neurotol. 2003;24:939–941. doi: 10.1097/00129492-200311000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Presutti L, Villari D, Marchioni D. Petrous apex cholesterol granuloma: transsphenoid endoscopic approach. J Laryngol Otol. 2006;120:e20. doi: 10.1017/S0022215106009121. [DOI] [PubMed] [Google Scholar]
- 11.Oyama K Ikezono T Tahara S Shindo S Kitamura T Teramoto A Petrous apex cholesterol granuloma treated via the endoscopic transsphenoidal approach Acta Neurochir (Wien) 2007149299–302., discussion 302 [DOI] [PubMed] [Google Scholar]
- 12.Samadian M, Vazirnezami M, Moqaddasi H, Rakhshan M, Khormaee F, Ashraf H. Endoscopic transrostral-transsphenoidal approach to petrous apex cholesterol granuloma: case report. Turk Neurosurg. 2009;19:106–111. [PubMed] [Google Scholar]
- 13.Zanation A M, Snyderman C H, Carrau R L, Gardner P A, Prevedello D M, Kassam A B. Endoscopic endonasal surgery for petrous apex lesions. Laryngoscope. 2009;119:19–25. doi: 10.1002/lary.20027. [DOI] [PubMed] [Google Scholar]
- 14.Mattox D E. Endoscopy-assisted surgery of the petrous apex. Otolaryngol Head Neck Surg. 2004;130:229–241. doi: 10.1016/j.otohns.2003.11.002. [DOI] [PubMed] [Google Scholar]