Abstract
Purpose: To identify the degree of perceived social support by mothers of infants hospitalized in neonatal intensive care unit (NICU) and to investigate effects depression and anxiety levels on the perceived social support.
Method: The study included 50 mothers of infants hospitalized in NICU. Demographic and clinical characteristics of the mothers were collected using a personal data form designed by the study researchers via face-to-face interviews. The Multidimensional Scale of Perceived Social Support Scale (MSPSS) was used to evaluate the degree of perceived social support by the mothers and Hospital Anxiety and Depression (HAD) Scale was used to assess their anxiety and depression levels.
Results: The mean age of the mothers was 29.1 ± 4.2 years. There was a significant correlation between the scores of the anxiety and depression subscales (r=0.772; p<0.001), whereas these scores were not significantly correlated with MSPSS total score. The scores MSPSS subscales were significantly correlated with each other, as well as with MSPSS total score. Friend subscale score and depression subscale score were positively correlated with education level (r=0.295, p=0.038 and r=0.407, p=0.003, respectively). The family and spouse subscale scores and MSPSS total score were significantly higher assisted conception technique group compared with the spontaneous conception group (p=0.020, p=0.010 and p=0.016, respectively). The family and spouse subscale scores and MSPSS total score were significantly lower in the mothers with depression subscale score of ≥7 than in the mothers with depression subscale score of <7 (p=0.010, p=0.038 and p=0.018, respectively). In the linear regression model, only education level was found to be a significant factor affecting depression level (p=0.006).
Conclusion: The mothers of infants hospitalized in the NICU with higher education levels had higher depression level and perceived social support from friends. Informing the family members and providing psychological support independent from the duration of gestation are of paramount importance.
Keywords: Newborn, social support, depression, anxiety
Introduction
Having premature or severely ill infants may lead parents to experience negative feelings such as shock, grief, anxiety or guilt1-3. Anxiety constitutes one of the negative feelings most frequently experienced by the parents. Pregnancy, delivery, becoming parent, disease states, hospitalization, emotional loss, and economic problems are among the anxiety-provoking factors4. In addition, other anxiety-provoking factors include disease course of the babies, likelihood of losing the babies, strange hospital environment, and feeling loss of control4. The technological devices, and different sounds, and smells in neonatal intensive care units (NICUs) are likely to be perceived by parents as scary or even horrifying1,5. Parents of infants hospitalized in NICUs have a number of higher priority requirements compared with those of infants hospitalized in other units, including physiological requirements (eating, drinking, sleeping), communication, social support, trust, participation in the care of their infant, and being informed about health status of their infants, equipments used, routines of the unit, and their own roles6,7. Thus, parents are in need of support both from their social environment and from healthcare providers8.
Social support can be described as tangible and intangible benefits commonly provided upon a stressful condition on an individual by others9. People need relying on the other family members and friends in case of crisis and emotional stress. Release of information about health status of the infants, encouragement of participation in the care of the infants, and provision of emotional support by healthcare providers promote parents’ ability to cope with anxiety3,5. Bialoskurski et al8 stated that meeting all the requirements of mothers of infants hospitalized in NICUs was a prerequisite for achieving their well-being. Although there have been several studies conducted on the requirements of mothers of infants hospitalized in NICUs2,6,10, to the best of our knowledge, there are limited number of studies on this issue in Turkey. Accordingly, the aim of the present study was to identify the degree of perceived social support by mothers of infants hospitalized in NICU and to investigate effects depression and anxiety levels on the perceived social support.
Materials and methods
The present study included the mothers of infants hospitalized in the neonatal intensive care unit of Zekai Tahir Burak Women’s Health Training and Research Hospital between June 2010 and December 2010 due to some reasons including prematurity, sepsis, pneumonia, and multiple pregnancy. Demographic and clinical characteristics of the mothers were collected using a personal data form designed by the study researchers via face-to-face interviews.
Multidimensional Scale of Perceived Social Support (MSPSS)
MSPSS, which was developed by Zimet et al11 in 1988, is a straightforward and brief scale with 12 items designed to subjectively assess the sufficiency of perceptions about social support. The adaptation and validation of MSPSS in Turkish was performed by Eker et al12. The scale consists of 3 subscales, each composed of 4 items rated on a 7-point Likert-type scale. The subscales are family (3rd, 4th, 8th and 11th items), friends (6th, 7th, 9th and 12th items) and significant others (such as, spouses) (1st, 2nd, 5th and 10th items). The total score is obtained by simply summing all subscale scores; the possible range for total is 12 to 84. Higher total scores indicate higher levels of perceived social support, whereas lower total scores indicate either the support is not perceived, or a lack or scarcity of support.
Hospital Anxiety and Depression Scale (HAD)
HAD is a self-report scale designed to briefly measure anxiety and depression and widely used in hospital settings13. The scale is also used to address the anxiety and depression risks and to measure the level and severity of anxiety and depression. The scale was adapted and validated in Turkish by Aydemir et al14. In the present study, mothers with the anxiety subscale score of ≥10 were considered to have definite anxiety and with the depression subscale score of ≥7 were considered to have definite depression.
Statistical Analysis
Data analysis was performed using the MS Excel 2003 (Microsoft Corp., Redmond, WA) and the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL, USA) version 15.0. The normality of continuous variables was tested using the Shapiro-Wilk test. Descriptive statistics were expressed as numbers and percentages for categorical variables and as mean±standard deviation or median (minimum and maximum) for continuous variables. Spearman’s rank correlation coefficient was used to assess correlations between demographic characteristics and HAD and MSPSS subscale scores, between each subscale score of HAD or MSPSS scale, and between each subscale score of both scales and MSPSS total score. Kruskal-Wallis variance analysis was performed to compare HAD and MSPSS subscale scores in mothers grouped according to the birth weights of infants and to their education levels. Group differences were tested using the Mann-Whitney U test with Bonferroni correction. Comparison of the groups formed based on type of delivery and gestational duration were performed using the Mann-Whitney U test. Linear regression analysis was used to determine the factors affecting depression and anxiety levels of the mothers. A p value <0.05 was considered statistically significant.
Results
The present study included 50 mothers of infants hospitalized in the neonatal intensive care unit. The mean age of the mothers was 29.1 ± 4.2 years (range 20-38 years). Demographic and clinical characteristics of mothers and infants are presented in Table 1. The median anxiety subscale score (8, range 0-17) was lower than the cutoff value of 10, whereas the median depression subscale score (10, range 1-17) was higher than the cutoff value of 7. No significant correlation was found between the scores of HAD and MSPSS subscales. There was a significant correlation between the scores of the anxiety and depression subscales (r=0.772; p<0.001), whereas these scores were not significantly correlated with MSPSS total score. The scores MSPSS subscales were significantly correlated with each other, as well as with MSPSS total score (Table 2).
Table 1. Demographic and clinical characteristics of the mothers.
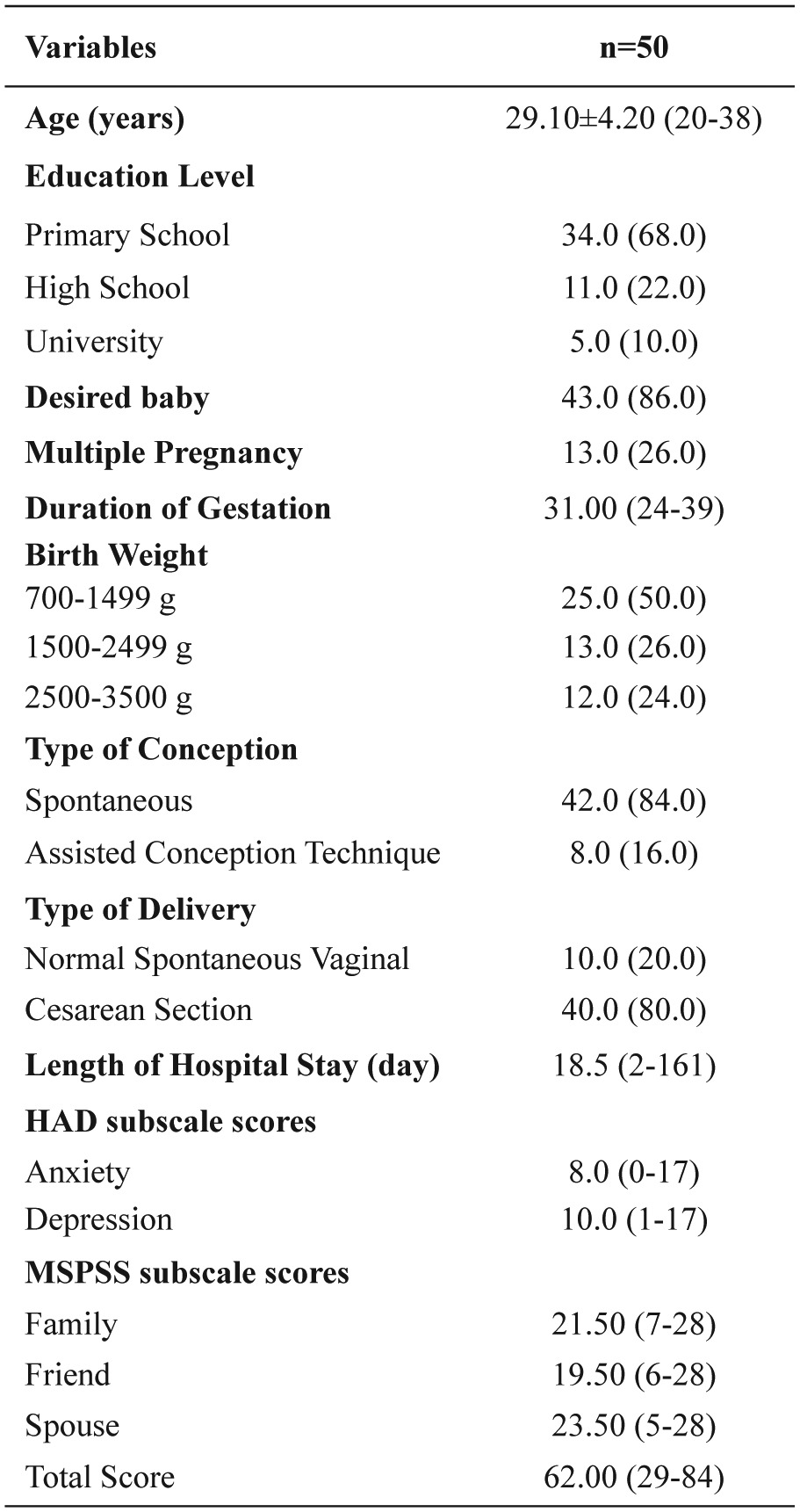
Data are presented as mean ± standard deviation, number (%) or median (minimum-maximum), where appropriate. HAD: Hospital Anxiety and Depression, MSPSS: Multidimensional Scale of Perceived Social Support
Table 2. Correlation between the scores of Hospital Anxiety and Depression (HAD) and Multidimensional Scale of Perceived Social Support (MSPSS) subscales, between each subscale score of HAD or MSPSS scale, and between each subscale score of both scales and MSPSS total score.
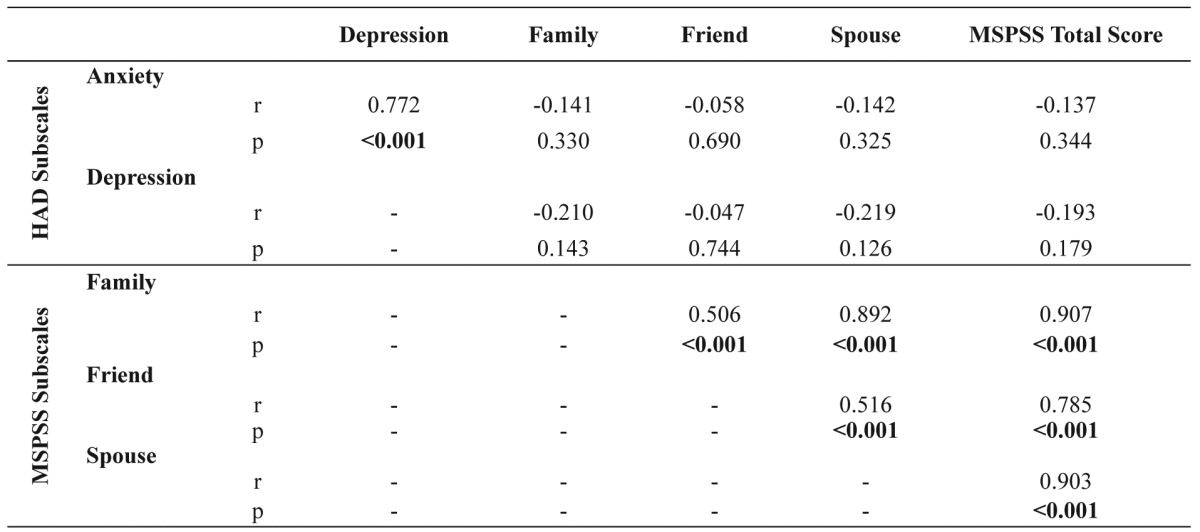
HAD: Hospital Anxiety and Depression, MSPSS: Multidimensional Scale of Perceived Social Support
Table 3 presents the correlation between the subscale scores of HAD and MSPSS, and MSPSS total score and age, education level, duration of gestation, birth weight and length of hospital stay. Friend subscale score was positively correlated with education level (r=0.295, p=0.038), whereas it was negatively correlated with duration of gestation (r=-0.321, p=0.023) and birth weight (r=-0.479, p<0.001). There was also a negative correlation between MSPSS total score and birth weight (r=-0.364, p=0.009). A positive significant correlation was determined between depression subscale score and education level (r=0.407, p=0.003). Moreover, depression subscale scores were significantly higher in the mothers graduated from high school and university as compared to those graduated from primary school (p=0.009 and p=0.005, respectively).
Table 3. Correlation between the scores of Hospital Anxiety and Depression subscale, Multidimensional Scale of Perceived Social Support (MSPSS) subscales, and MSPSS total score and age, education level, duration of gestation, birth weight and length of hospital stay.
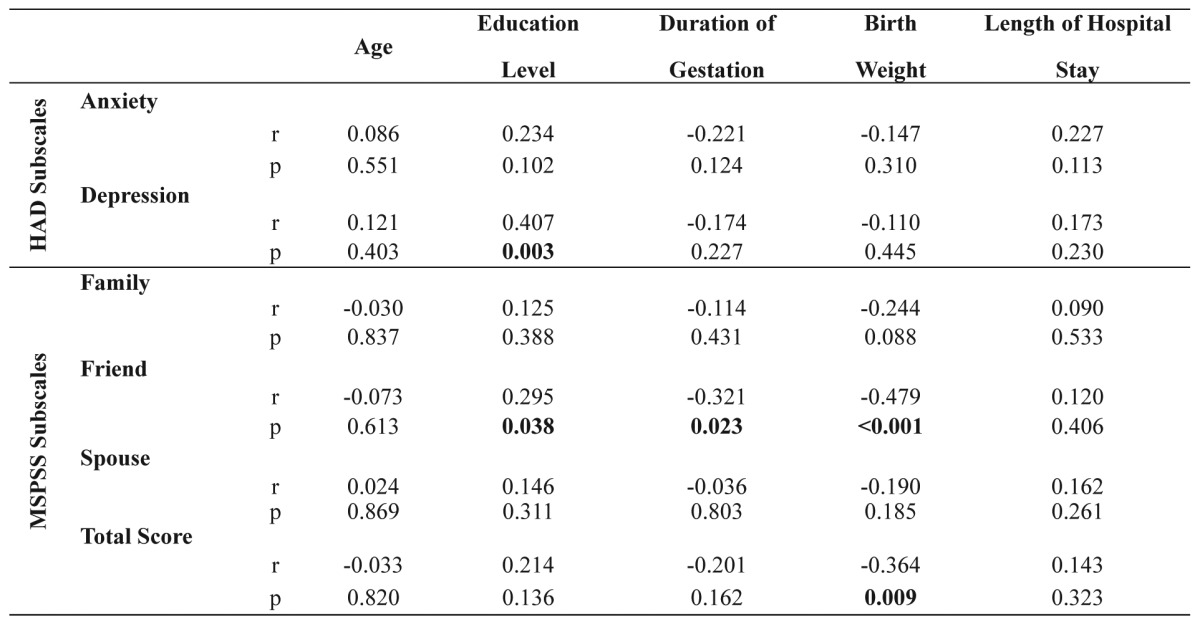
HAD, Hospital Anxiety and Depression; MSPSS, Multidimensional Scale of Perceived Social Support
When the mothers were grouped according to the birth weights of their infants, 12 of 25 (48.0%) in 700-1499 g group, 6 of 13 (46.2%) in 1500-2499 g group, and 3 of 12 (25.0%) in 2500-3500 g group had an anxiety level of ≥10, with no significant difference (p=0.390). Eighteen mothers (72.0%) in 700-1499 g group, 8 mothers (61.5%) in 1500-2499 g group, and 10 mothers (83.3%) in 2500-3500 g group had a depression level of ≥7, with no significant difference (p=0.470). The distribution of subscale scores of HAD and MSPSS in mothers grouped according to the birth weights of infants is presented in Table 4. There were significant differences among birth weight groups in terms of the friend subscale and MSPSS total scores (p=0.004 and p=0.037, respectively). The friend subscale and MSPSS total scores were significantly higher in the 700-1499 g group than in the 1500-2499 g and 2500-3500 g groups (p=0.022 and p<0.001 respectively for friend subscale; p=0.025 and p=0.004 respectively for MSPSS total score).
Table 4. Distribution of subscale scores of Hospital Anxiety and Depression scale and Multidimensional Scale of Perceived Social Support in mothers grouped according to the birth weights of infants.
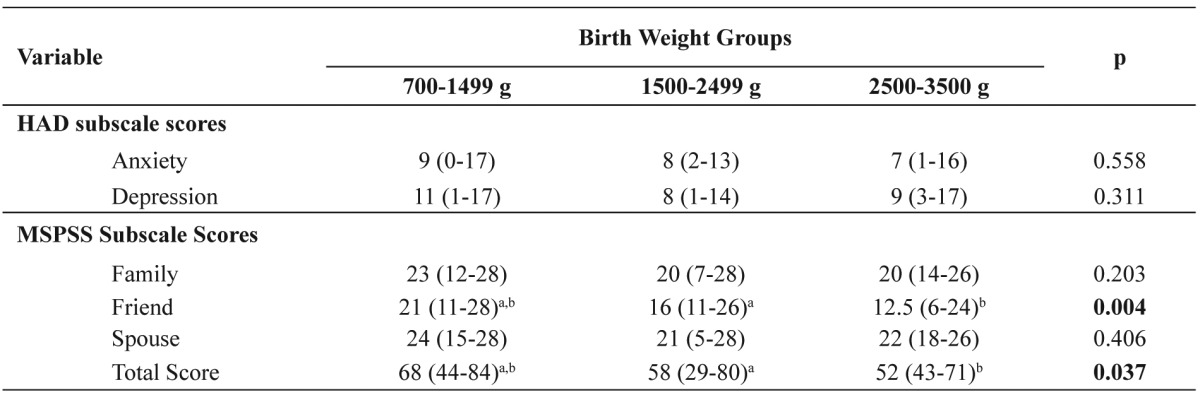
a p<0.05 for 700-1499 g group vs. 1500-2499 g group
b pp<0.01 for 700-1499 g group vs. 2500-3500 g group, HAD: Hospital Anxiety and Depression, MSPSS: Multidimensional Scale of Perceived Social Support
When the mothers were grouped according to the type of conception, the family and spouse subscale scores and MSPSS total score were significantly higher in the assisted conception technique group compared with the spontaneous conception group (p=0.020, p=0.010 and p=0.016, respectively). The duration of gestation was longer in the mothers with anxiety subscale score of <10 than in the mothers with anxiety subscale score of ≥10 (p=0.047). The family and spouse subscale scores and MSPSS total score were significantly lower in the mothers with depression subscale score of ≥7 than in the mothers with depression subscale score of <7 (p=0.010, p=0.038 and p=0.018, respectively).
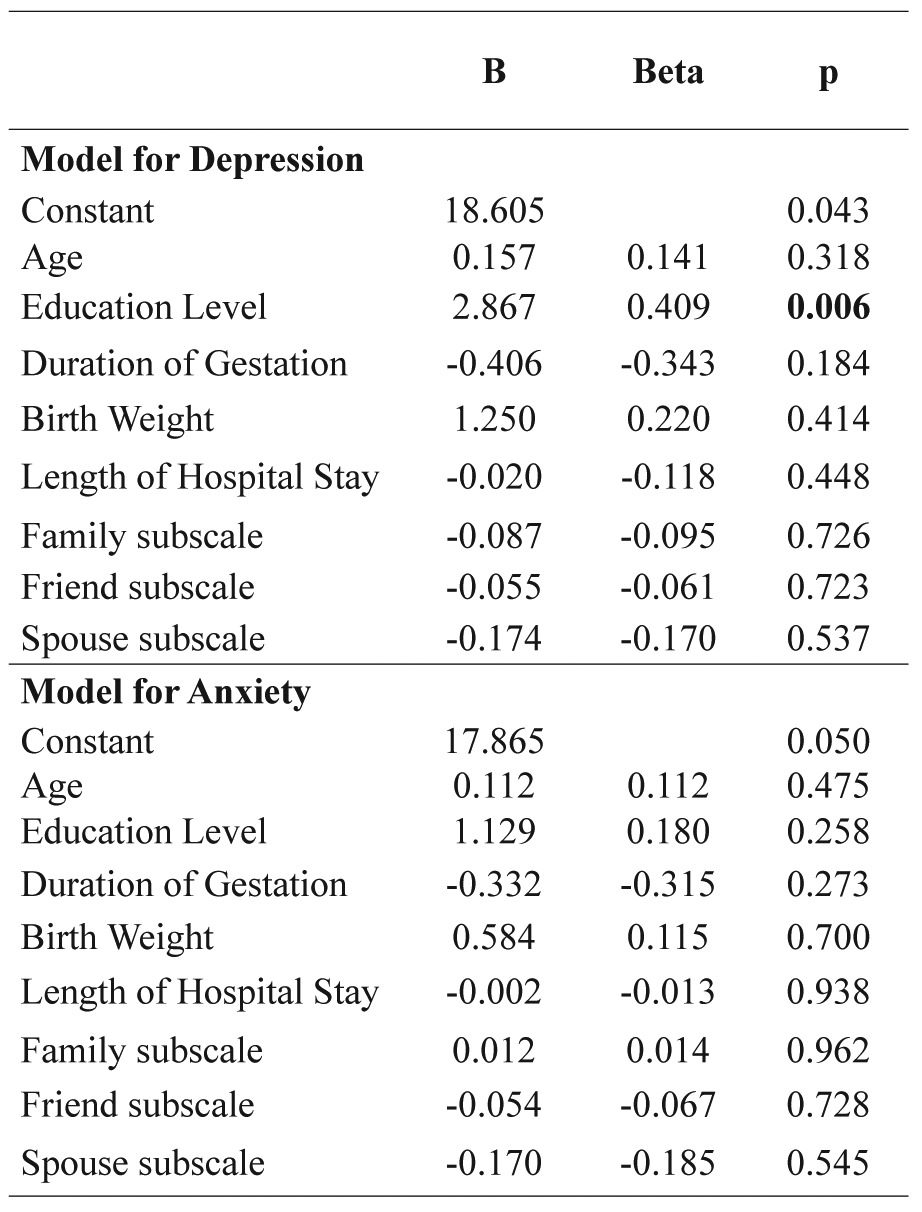
A model was developed to determine the factors including age, education level, duration of gestation, birth weight, length of hospital stay, and family, friend, and spouse subscales that could affect the depression level. Education level was found to be a significant factor (p=0.006). Another model was also developed to determine the factors including age, education level, duration of gestation, birth weight, length of hospital stay, and family, friend, and spouse subscales that could affect the anxiety level. None of these factors was found to be significant factor (Table 5).
Table 5. Linear regression analysis.
Discussion
Major or minor disorders of children have been considered as stress-provoking events in mothers. Families face with various stressors especially following hospitalization of risky infants, which are likely to initiate major psychosocial changes in families15,16.
Keeping mothers out of NICUs during treatment and follow-up of their infants or not allowing mothers’ companion to their infants is considered quite stressful. There exist studies reporting high levels of state and unceasing anxiety experienced by mothers of babies received treatment in NICUs and clinical levels of emotional symptoms such as anxiety, depression, and dysphoria17,18. Previous studies also addressed that separation of a mother from especially a newborn provokes anxiety and despair in mothers19-21. In the present study, depression and anxiety levels of mothers of infants hospitalized in the NICU were investigated. The length of hospital stay of infants was 18.5 days (2-161 days), which did not correlate with the depression and anxiety levels of mothers.
Contrary to our expectation, a positive significant correlation was observed between the depression subscale scores and education level of the mothers. It was also noteworthy that the higher the educational level, the more support one received from her friends. This result contradicts with the finding implying that mothers more easily cope with the negative effects due to having a troubled child, showing less signs of stress22.
In the present study, the family and spouse subscale scores and MSPSS total score were significantly lower in the mothers with depression subscale score of ≥7 than in the mothers with depression subscale score of <7. A mutual and cyclic relationship is present between the perceived social support and depression. It is well known that lack of social support is likely to cause depression, and depression may further deteriorate the social relations of an individual, thus leading to reduction in social supports23. In the present study, the duration of gestation was lower in the mothers with anxiety subscale score of ≥10. Similarly, studies have stated that families of premature infants experience higher levels of depression secondary to increasing stress and anxiety during early postpartum period24-25. In studies from different countries, insufficiency in social support has been reported as one of the substantial factors increasing the risk for postpartum depression26-29. Particularly, weak family bonds have been identified as a significant factor increasing the risk for postpartum depression30,31.
In the present study, the friend subscale and MSPSS total scores were determined to be higher in the mothers of infants with low birth weights. Moreover, the family and spouse subscale scores and MSPSS total score were significantly higher in the mothers undergoing assisted conception, although their number was low, than those who conceived spontaneously, These results indicated that the social support was insufficiently provided to the mothers who conceived spontaneously or those of infants with normal birth weight. We are in the opinion that, enhanced perception of the problem by spouses and friends also promotes their sensitivities towards mothers, thus increasing the level of perceived social support in mothers. The literature has highlighted that insufficiency in the psychosocial and emotional supports during pregnancy are predictive for development of depression during both pregnancy and postpartum periods32,33. Moreover, depression and anxiety have been reported to increase the pregnancy and delivery complications, to exert detrimental effects on newborn health, and to cause premature birth, low birth weight and intrauterine growth retardation34.
Vital events, state anxiety and high levels of perceived stress have been reported to significantly shorten duration of gestation35,36. In the present study, as well, the duration of gestation was determined to be longer in the mothers experienced low level of anxiety. A study conducted in a similar manner concluded that vital events experienced throughout the pregnancy were associated with lower birth weight and that one unit increase in the pregnancy-associated anxiety level shortened the duration of gestation by three days37.
Previous studies have implied that the perceived social support from families and the environment promotes the quality of life and the well-being of patients38,39 and concluded that social support provided especially by families, spouses and healthcare providers has a significant effect on the prevention of postpartum depression40-42. The results of the present study conducted on the mothers of infants hospitalized in the NICU revealed that depression level and perceived social support from friends were higher in those with higher education levels. We are in the opinion that informing the family members and providing psychological support independent from the duration of gestation are of paramount importance.
Conflict of Interest
Authors declare no conflict of interest.
References
- 1.Boxwel G. Neonatal Intensive Care Nursing. 2nd ed. Taylor and Francis, London, e-Library. 2002:392–400. [Google Scholar]
- 2.Ward K. Perceived needs of parents of critically ill infants in a neonatal intensive care unit. Pediatr Nurs. 2001;27:281–286. [PubMed] [Google Scholar]
- 3.Wigert H, Johansson R, Berg M, Hellström AL. Mothers’ experiences of having their newborn child in a neonatal intensive care unit. Scand J Caring Sci. 2006;20:35–41. doi: 10.1111/j.1471-6712.2006.00377.x. [DOI] [PubMed] [Google Scholar]
- 4.Öz F. Sağlık Alanında Temel Kavramlar. İmaj İç ve Dış Ticaret AS, 1. Baskı, Ankara. 2004:157–173. [Google Scholar]
- 5.Franklin C. The neonatal nurse’s role in parental attachment in the NICU. Crit Care Nurs Q. 2006;29:81–85. doi: 10.1097/00002727-200601000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Bass LS. What do parents need when their infant is a patient in the NICU? Neonatal Netw. 1991;10:25–33. [PubMed] [Google Scholar]
- 7.Fisher MD. Identified needs of parents in a pediatric intensive care unit. Crit Care Nurse. 1994;14:82–90. [PubMed] [Google Scholar]
- 8.Bialoskurski MM, Cox CL, Wiggins RD. The relationship between maternal needs and priorities in a neonatal intensive care environment. J Adv Nurs. 2002;37:62–69. doi: 10.1046/j.1365-2648.2002.02057.x. [DOI] [PubMed] [Google Scholar]
- 9.Aksüllü N, Doğan S. Huzurevinde ve evde yaşayan yaşlılarda algılanan sosyal destek etkenleri ile depresyon arasındaki ilişki. Anadolu Psikiyatri Derg. 2004;5:76–84. [Google Scholar]
- 10.Miles MS, Carlson J, Funk SG. Sources of support reported by mothers and fathers of infants hospitalized in a neonatal intensive care unit. Neonatal Netw. 1996;15:45–52. [PubMed] [Google Scholar]
- 11.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 12.Eker D, Arkar H, Yaldız H. Çok boyutlu algılanan sosyal destek ölçeğinin gözden geçirilmiş formunun faktör yapısı, geçerlik ve güvenirliği. Turk Psikiyatri Derg. 2001;12:17–25. [Google Scholar]
- 13.Zigmund AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Aydemir Ö, Güvenir T, Küey L. Hastane anksiyete ve depresyon ölçeği Türkçe formunun geçerlilik ve güvenilirliği. Turk Psikiyatri Derg. 1977;8:280–287. [Google Scholar]
- 15.Karaman H. G.Ü.T.F YDYBÜ’de yatan bebeklerin ailelerine uygulanan aile memnuniyeti anketinin sonuçları. X. Ulusal Neonatoloji Kongresi Kitabı. Antalya. 26-30 Mart 2000;157 [Google Scholar]
- 16.Miles MS, Carlson J, Brunssen S. Nurse parent support tool. J Pediatric Nurs. 2001;14:44–50. doi: 10.1016/S0882-5963(99)80059-1. [DOI] [PubMed] [Google Scholar]
- 17.Padovani FH, Linhares MB, Carvalho AE, Duarte G, Martinez FE. [Anxiety and depression symptoms assessment in pre-term neonates’ mothers during and after hospitalization in neonatal intensive care unit] Rev Bras Psiquiatr. 2004;26:251–254. doi: 10.1590/s1516-44462004000400009. [DOI] [PubMed] [Google Scholar]
- 18.Ergin D, Şen N, Demet M. Yenidoğan ünitesinde tedavi gören bebeklerin ebeveynlerinin anksiyete ve kaygı düzeyleri ve bunları etkileyen etmenler. 1. Ulusal Pediatri Hemşireliği Kongresi. Kongre Özet Kitabı, İzmir. Sayfa. 21-23 Haziran 2007;55 [Google Scholar]
- 19.Nyström K, Axelsson K. Mothers’ experience of being separated from their newborns. J Obstet Gynecol Neonatal Nurs. 2002;31:275–282. doi: 10.1111/j.1552-6909.2002.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 20.Fowlie PW, McHaffie H. Supporting parents in the neonatal unit. BMJ. 2004;329:1336–1338. doi: 10.1136/bmj.329.7478.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall EO. Being in an alien world: Danish parents’ lived experiences when a newborn or small child is critically ill. Scand J Caring Sci. 2005;19:179–185. doi: 10.1111/j.1471-6712.2005.00352.x. [DOI] [PubMed] [Google Scholar]
- 22.Quine L, Pahl J. Stress and coping in mothers caring for a child with severe learning dfficulties: A test of Lazarus transitional model of coping. J Comm Appl Soc Psych. 1991;1:57–70. [Google Scholar]
- 23.Ralpmund V, Moore C. Women’s stories of depression: A constructivist approach. S Afr J Psychol. 2000;30:20–31. [Google Scholar]
- 24.Ekuklu G, Tokuc B, Eskiocak M, Berberoglu U, Saltik A. Prevalence of postpartum depression in Edirne, Turkey and related factors. J Reprod Med. 2004;49:908–914. [PubMed] [Google Scholar]
- 25.Lee SK, Penner PL, Cox M. Impact of very low birth weight infants on the family and its relationship to parental attitudes. Pediatrics. 1991;88:105–109. [PubMed] [Google Scholar]
- 26.Dilbaz N, Enez A. Kadın ve depresyon: Doğum sonrası görülen duygudurum bozuklukları. J Int Med Sci. 2007;3:32–40. [Google Scholar]
- 27.Yıldırım GS, Kısa C, Aydemir Ç. Postpartum depresyon. Psikiyatri Psikoloji Psikofarmakoloji Dergisi. 2004;4:12–20. [Google Scholar]
- 28.Glasser S, Barell V, Boyko V, Ziv A, Lusky A, Shoham A, et al. Postpartum depression in an Israeli cohort: demographic, psychosocial and medical risk factors. J Psychosom Obstet Gynaecol. 2000;21:99–108. doi: 10.3109/01674820009075615. [DOI] [PubMed] [Google Scholar]
- 29.Mills EP, Finchilescu G, Lea SJ. Postnatal depression--an examination of psychological factors. S Afr Med J. 1995;85:99–105. [PubMed] [Google Scholar]
- 30.Zhang R, Chen Q, Li Y. [Study for the factors related to postpartum depression] Zhonghua Fu Chan Ke Za Zhi. 1999;34:231–233. [PubMed] [Google Scholar]
- 31.Stuchbery M, Matthey S, Barnett B. Postnatal depression and social supports in Vietnamese, Arabic and Anglo-Celtic mothers. Soc Psychiatry Psychiatr Epidemiology. 1998;33:483–490. doi: 10.1007/s001270050083. [DOI] [PubMed] [Google Scholar]
- 32.Neter E, Collins NL, Lobel M, Dunkel-Schetter C. Psychosocial predictors of postpartum depressed mood in socioeconomically disadvantaged women. Womens Health. 1995;1:51–57. [PubMed] [Google Scholar]
- 33.Da Costa D, Larouche J, Dritsa M, Brender W. Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord. 2000;59:31–40. doi: 10.1016/s0165-0327(99)00128-7. [DOI] [PubMed] [Google Scholar]
- 34.Pagel MD, Smilkstein G, Regen H, Montano D. Psychosocial influences on new born outcomes: a controlled prospective study. Soc Sci Med. 1990;30:597–604. doi: 10.1016/0277-9536(90)90158-o. [DOI] [PubMed] [Google Scholar]
- 35.Lobel M, Dunkel-Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: a prospective study of socioeconomically disadvantaged women. Health Psychol. 1992;11:32–40. doi: 10.1037//0278-6133.11.1.32. [DOI] [PubMed] [Google Scholar]
- 36.Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18:333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- 37.Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Gaite TJ. The association between prenatal stress and infant birth weight and gestational age at birth: a prospective investigation. Am J Obstet Gynecol. 1993;169:858–865. doi: 10.1016/0002-9378(93)90016-c. [DOI] [PubMed] [Google Scholar]
- 38.Hewitt J. Critical evaluation of the use of research tools in evaluating quality of life for people with schizophrenia. Int J Ment Health Nurs. 2007;16:2–14. doi: 10.1111/j.1447-0349.2006.00438.x. [DOI] [PubMed] [Google Scholar]
- 39.Kaiser SL, Snyder JA, Corcoran R, Drake RJ. The relationship among insight, social support, and depression in psychosis. J Nerv Ment Dis. 2006;194:905–908. doi: 10.1097/01.nmd.0000242975.96932.4c. [DOI] [PubMed] [Google Scholar]
- 40.Heh SS, Coombes L, Barlett H. The association between depressive symptoms and social support in Taiwanese women during the month. Int J Nurs Stud. 2004;41:573–579. doi: 10.1016/j.ijnurstu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Kuscu MK, Akman I, Karabekiroglu A, Yurdakul Z, Orhan L, Ozdemir N, et al. Early adverse emotional response to childbirth in Turkey: the impact of maternal attachment styles and family support. J Psychosom Obstet Gynaecol. 2008;29:33–38. doi: 10.1080/01674820701535480. [DOI] [PubMed] [Google Scholar]
- 42.Chen CM, Kuo SF, Chou YH, Chen HC. Postpartum Taiwanese women: their postpartum depression, social support and health-promoting lifestyle profiles. J Clin Nurs. 2007;16:1550–1560. doi: 10.1111/j.1365-2702.2006.01837.x. [DOI] [PubMed] [Google Scholar]


