Abstract
Objective
To survey current practices among different types of medical practitioners in Ontario to assess if national guidelines for screening and management of neonatal hyperbilirubinemia were being followed.
Design
An anonymized, cross-sectional survey distributed by mail and e-mail.
Setting
Ontario.
Participants
From each group (general practitioners, family medicine practitioners, and pediatricians), 500 participants were randomly selected, and all 390 registered midwives were selected.
Main outcome measures
Compliance with national guidelines for screening, postdischarge follow-up, and management of newborns with hyperbilirubinemia.
Results
Of the 1890 potential respondents, 321 (17%) completed the survey. Only 41% of family physicians reported using national guidelines, compared with 75% and 69% of pediatricians and midwives, respectively (P < .001). Bilirubin was routinely measured for all newborns before discharge by 42% of family physicians, 63% of pediatricians, and 22% of midwives (P < .001). Newborn follow-up was completed within 72 hours after discharge by 60% of family physicians, 89% of pediatricians, and 100% of midwives. Management of neonatal hyperbilirubinemia differed significantly (P < .001), with 91% of family physicians, 99% of pediatricians, and 79% of midwives correctly managing a case scenario according to the guidelines.
Conclusion
The management of jaundice varied considerably among the different practitioner types, with pediatricians both most aware of the guidelines and most likely to follow them. Increased knowledge translation efforts are required to promote adherence to the jaundice management guidelines across all practitioner types, but particularly among family physicians.
Résumé
Objectif
Vérifier comment différents types de praticiens médicaux de l’Ontario traitent actuellement l’hyperbilirubinémie néonatale afin d’établir si les directives de pratique nationales pour le dépistage et le traitement sont respectées.
Type d’étude
Enquête transversale anonyme distribuée par la poste ou par courriel.
Contexte
L’Ontario.
Participants
On a choisi au hasard 500 omnipraticiens, 500 médecins de famille et 500 pédiatres ainsi que toutes les sages-femmes licenciées (N = 390).
Principaux paramètres à l’étude
Respect des directives nationales pour le dépistage, suivi post congé et traitement de l’hyperbilirubinémie néonatale.
Résultats
Sur les 1890 répondants potentiels, 321 (17 %) ont complété l’enquête. Seulement 41 % des médecins de famille ont déclaré suivre les directives nationales, contre de 75 % des pédiatres et 69 % des sages-femmes (P < ,001). Les médecins de famille ont mesuré la bilirubine chez tous les nourrissons avant le congé dans une proportion de 42 %, contre 63 % des pédiatres et 22 % des sages-femmes (P < ,001). Le suivi des nouveau-nés a été complété en moins de 72 heures après le congé par 60 % des médecins de famille, par 89 % des pédiatres et par 100 % des sages-femmes. Il y avait des différences significatives (P < ,001) dans le traitement de l’ictère néonatal, 91 % des médecins de famille, 99 % des pédiatres et 79 % des sages-femmes ayant correctement appliqué les directives lorsque confrontés à un cas type.
Conclusion
La façon de traiter l’ictère néonatal varie considérablement entre les différents type de praticiens, les pédiatres étant les plus au fait des directives et les plus susceptibles de s’y conformer. Une meilleure formation est souhaitée pour tous les types de praticiens, en particulier pour les médecins de famille, afin d’améliorer l’adhésion aux directives concernant le traitement de cet ictère.
Hyperbilirubinemia continues to be the most common cause of neonatal readmission to hospitals in North America.1–5 If not treated rapidly and effectively, severe hyperbilirubinemia can have devastating long-term consequences of varying severity (eg, kernicterus).6 Although severe hyperbilirubinemia is largely a preventable disease, cases continue to occur at an alarming rate, with 258 infants in Canada presenting with severe hyperbilirubinemia during a 2-year period according to data from the Canadian Paediatric Surveillance Program.7 The morbidity continues to occur despite attempts to identify at-risk newborns before discharge from the hospital,8–11 and despite the publication of guidelines by the American Academy of Pediatrics (AAP) in 200412 and the Canadian Paediatric Society (CPS) in 200713 to promote good practices in the screening and management of hyperbilirubinemia. In addition, the importance of screening all newborns, including those without apparent risk factors, has been highlighted by reports of kernicterus in healthy near-term and term infants with no evidence of hemolytic disease or risk factors.14,15
Based on these concerning findings, it is important to assess knowledge translation and the extent to which national guidelines are known and practised, as management according to national guidelines might minimize morbidity in hyperbilirubinemia. The objective of this study was to determine current practices among medical practitioners in Ontario in the screening for, and management of, neonatal hyperbilirubinemia. Through assessment of the level of knowledge and practice patterns that are reported by the different medical practitioner types, this study will help to direct future knowledge translation efforts.
METHODS
Study population
A cross-sectional survey of randomly selected medical practitioners involved in the care of newborns was conducted in Ontario. The Scott’s Directories Medical Directories Database was used to identify medical practitioners. The Medical Directories Database contains the Canadian Medical Directory, which captures almost 99% of all the medical practitioners in Canada. The Canadian Medical Directory includes registered physicians from the Royal College of Physicians and Surgeons of Canada and the College of Family Physicians of Canada (CFPC) and maintains a current list of contact information through reminders sent to the physicians twice a year.
Based on the 2008 Canadian Medical Directory, there were 4844 general practitioners, 5716 family medicine practitioners, and 1042 pediatricians across Ontario.16 A priori, we hypothesized that there would be differences in jaundice management practices among the various practitioner types. Although it would have been ideal to survey all practitioners, it was not feasible owing to resource constraints and the large sample size of 11 992 practitioners in Ontario; thus, a sampling frame was devised. Our sample-size calculation was based on defining a 20% difference in responses to key practice questions among practitioner types as clinically meaningful. There were no published data on jaundice management practices by practitioner type to use for baseline rates. Thus, we estimated the proportion of family physicians and pediatricians ordering serum bilirubin tests before discharge to be 30% and 50%, respectively. For an α of .05 and a power of 80%, a total of 93 responses per practitioner type would be required. Community-based mail and e-mail surveys have reported response rates of 20% to 30%.17 It was anticipated that sending 500 surveys to each practitioner type with a response rate of 20% would yield 100 responses from each practitioner type. Owing to the small number of midwives, all 390 midwives registered with the Association of Ontario Midwives were surveyed to attempt to obtain a sufficient sample size of 100 responses. Using an electronic randomization program, the Canadian Medical Directory randomly selected 500 participants from each of the general practitioner, family medicine practitioner, and pediatrician groups. In addition to the 390 midwives, this gave us a pool of 1890 potential respondents.
Questionnaire development and distribution
An anonymized questionnaire was developed, with questions chosen to specifically assess the practitioners’ awareness of and adherence to published CPS and AAP guidelines for the screening and management of hyperbilirubinemia. One of the questions was a case scenario to assess jaundice management practices (Box 1).
Box 1. Case scenario.
A 32-year-old mother with blood group O Rh+ gave birth to a 3.5-kg male infant after 39 weeks’ gestation. Before discharge, at 48 hours of age, the infant appeared jaundiced. I would
discharge the baby with follow-up as an outpatient;
request Coombs testing, Rh blood typing, and bilirubin level measurement;
cancel discharge and start phototherapy; or
request a consultation
Demographic characteristics of respondents were collected based on the variables used in a previous survey on jaundice.18
The questionnaire was pilot-tested on a sample of 57 practitioners, which included 5 general and family medicine practitioners, 26 pediatricians, and 16 midwives to assess for clarity and ease of completion. Sixty-two percent of the midwives and 100% of the general and family medicine practitioners and pediatricians reported that the instructions were clear. Some questions were modified to improve clarity, and the final questionnaire was considered easy to complete by those who participated in the pilot testing.
A total of 1890 questionnaires were then distributed by postal service and electronic mail using SurveyMonkey (www.surveymonkey.com) in July 2009. E-mail reminders were sent 1, 2, and 3 weeks after the start of the study for nonresponders who had not declined participation in the survey. The survey was officially closed 6 months after the last mailing. The survey was voluntary and no incentives were provided. The Research and Ethics Board of St Michael’s Hospital in Toronto, Ont, approved the study.
Statistical analysis
Completed forms from the respondents were encoded. Data were entered into a Microsoft Excel spreadsheet and then exported for analysis with SPSS software, version 15.0. Because of low response rates and similarities in their scopes of practice, the general practitioners and family medicine practitioners were grouped together and labeled as family physicians. Family medicine practitioners were defined as physicians who had completed 2 to 3 years of an accredited family medicine residency program and successfully completed examination for Certification by the CFPC. General practitioners were defined as physicians who might not have completed an accredited family medicine residency program, and did not have Certification by the CFPC. General practitioners in Canada typically operate in private practices and either own their practices or work for privately owned practices.
Data were summarized and analyzed with descriptive statistics using the SPSS software. For descriptive data, proportions, means, and medians were recorded. Comparisons were made using t tests, χ2 tests, Fisher exact tests, or Mann-Whitney tests as appropriate. The level of statistical significance was taken at P < .05.
RESULTS
We distributed surveys to 500 of 4844 (10%) general practitioners, 500 of 5716 (9%) family medicine practitioners, 500 of 1042 (48%) pediatricians, and 390 of 390 (100%) of midwives (Figure 1). Response rates as a proportion of the total pool of practitioners in Ontario were 5 of 4844 general practitioners (0.1%), 76 of 5716 family medicine practitioners (1%), 152 of 1042 pediatricians (15%), and 88 of 390 midwives (23%). Among those surveyed, the response rate was 17% (321 of 1890), and the response rates differed by practitioner type, with responses from 1% of general practitioners, 15% of family medicine practitioners, 30% of pediatricians, and 23% of midwives.
Figure 1.
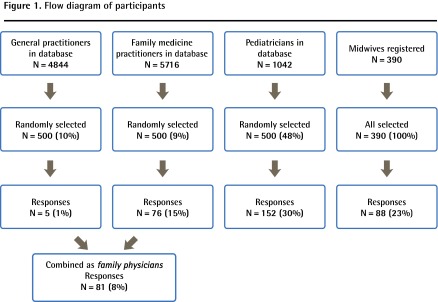
Flow diagram of participants
Most respondents in the family physician and pediatrician groups were men (Table 1). The respondents in both these groups were older and had more years of practice than the respondents from the midwife group, with most being 50 to 59 years old and having more than 10 years of practice experience. For practice settings, 45% were in community practice, and 52% had only level I nurseries in their hospital-based practices. Only 10% of family physicians saw more than 5 neonates per month compared with 91% of pediatricians and 57% of midwives.
Table 1.
Demographic characteristics of respondents
| CHARACTERISTIC |
PRACTITIONER TYPE, %
|
ALL PRACTITIONERS (N = 321), % | P VALUE* | ||
|---|---|---|---|---|---|
| FAMILY PHYSICIANS (N = 81) | PEDIATRICIANS (N = 152) | MIDWIVES (N = 88) | |||
| Sex | |||||
| • Male | 60 | 55 | 0 | 41 | < .001 |
| Age, y | < .001 | ||||
| • ≤ 30 | 1 | 1 | 12 | 4 | |
| • 31–39 | 17 | 19 | 36 | 23 | |
| • 40–49 | 25 | 24 | 22 | 24 | |
| • 50–59 | 38 | 36 | 25 | 33 | |
| • ≥ 60 | 19 | 20 | 5 | 15 | |
| Years of practice | < .001 | ||||
| • < 5 | 6 | 9 | 34 | 15 | |
| • 5–10 | 13 | 18 | 27 | 19 | |
| • > 10 | 81 | 73 | 39 | 65 | |
| No. of neonates seen per month | < .001 | ||||
| • ≤ 1 | 26 | 5 | 0 | 9 | |
| • 2–5 | 64 | 5 | 43 | 30 | |
| • > 5 | 10 | 91 | 57 | 61 | |
| Highest level of NICU in hospital practice | < .001 | ||||
| • Level I | 89 | 42 | 36 | 52 | |
| • Level II | 11 | 49 | 56 | 41 | |
| • Level III | 0 | 9 | 8 | 6 | |
NICU—neonatal intensive care unit.
P value for χ2 tests for differences in proportions between groups.
The use of AAP or CPS guidelines as a resource to guide jaundice management was reported by 41% of family physicians, 75% of pediatricians, and 69% of midwives (Table 2). Fewer family physicians reported that AAP or CPS guidelines were accessible or easy to use compared with midwives and pediatricians. Significant variations were found in predischarge and follow-up management of jaundice among the different practitioner types. Routine bilirubin tests were ordered before discharge by 42% of family physicians, 63% of pediatricians, and 22% of midwives (P < .001). Routine postdischarge follow-up within 72 hours was planned by 60% of family physicians, 89% of pediatricians, and 100% of midwives (P < .001). In response to the case scenario describing a jaundiced neonate with probable ABO incompatibility before hospital discharge, 91% of family physicians, 99% of pediatricians, and 79% of midwives indicated practices that were consistent with AAP or CPS guidelines (P < .001).
Table 2.
Practice patterns by practitioner type
| PATTERN |
PRACTITIONER TYPE, %
|
ALL PRACTITIONERS (N = 321), % | P VALUE* | ||
|---|---|---|---|---|---|
| FAMILY PHYSICIANS (N = 81) | PEDIATRICIANS (N = 152) | MIDWIVES (N = 88) | |||
| LOS after vaginal delivery, h | < .001 | ||||
| • ≤ 24 | 7 | 1 | 81 | 26 | |
| • 25–48 | 88 | 89 | 19 | 68 | |
| • > 48 | 5 | 9 | 0 | 6 | |
| Predischarge bilirubin level test | 42 | 63 | 22 | 46 | < .001 |
| Time of postdischarge follow-up, h | < .001 | ||||
| • ≤ 24 | 1 | 6 | 91 | 29 | |
| • 48–72 | 59 | 81 | 9 | 55 | |
| • ≤ 72 | 60 | 89 | 100 | 85 | |
| • > 72 | 40 | 11 | 0 | 15 | |
| Correct response to jaundice case scenario | 91 | 99 | 79 | 91 | < .001 |
| AAP or CPS guidelines used | 41 | 75 | 69 | 65 | < .001 |
| Agree or strongly agree that guidelines are accessible | 67 | 87 | 80 | 81 | .002 |
| Agree or strongly agree that guidelines are easy to use | 59 | 78 | 70 | 71 | .01 |
AAP—American Academy of Pediatrics, CPS—Canadian Paediatric Society, LOS—length of stay.
P value for χ2 test for differences in proportions between groups.
DISCUSSION
In this study of the knowledge translation of national guidelines for the management of neonatal hyperbilirubinemia in Ontario, we found substantial variation in adherence to the guidelines by practitioner type. An important goal of the CPS and AAP guidelines for management of hyperbilirubinemia is to minimize the risks of hyperbilirubinemia through early identification. At-risk infants are identified through routine monitoring of either serum bilirubin or transcutaneous bilirubin levels measured at discharge, or if not yet discharged, during the first 72 hours of life.13 Follow-up should occur at 3 to 5 days of age12 or every 24 to 48 hours for all newborns until feeding is established.13 Routine monitoring of bilirubin levels at or before discharge was reported by only 42% of family physicians compared with 63% of pediatricians. The low rate of bilirubin screening before hospital discharge by midwives is most likely owing to the typical timing of discharge for midwife deliveries at 24 hours of birth, rather than noncompliance with the guidelines. In routine midwifery practice, all newborns are seen by midwives within 72 hours of discharge and bilirubin screening would then likely occur after discharge during the follow-up visit.19,20 Timely postdischarge follow-up within 72 hours was reported by most pediatricians but by only 60% of family physicians.
Our finding of variability in the use of guidelines for hyperbilirubinemia is consistent with previous studies from the United States that demonstrate that the general uptake of guidelines is variable.21–23 There are reports of clinicians providing phototherapy as per the guidelines only 54% of the time,22 and only 37% of newborns are being followed as per AAP guidelines.21 Barriers to adherence to guidelines are multifactorial and might include lack of awareness, lack of agreement, and inertia of previous practices.24 Lack of awareness might partially explain the low adherence to guidelines by family physicians compared with pediatricians. The CPS or AAP guidelines were used by only 41% of family physicians, and were reported as easy to access by only 67% of family physicians compared with most of the pediatricians and midwives. Hospital affiliation of health care providers has been shown to be one of the strongest predictors of adherence to practice guidelines,18 and notably most family physicians had affiliations with hospitals with level I newborn care. The guidelines for hyperbilirubinemia have been widely disseminated among pediatricians through publication in Paediatrics & Child Health13 and are readily accessible on the CPS website,25 but these guidelines do not appear on the website for the Ontario College of Family Physicians26 nor the website for the Association of Ontario Midwives.27 Although individual family physicians might not see newborns frequently, most (69%) Ontario children younger than 1 year of age had general practitioners or family medicine practitioners as their regular primary care providers.28 Therefore, there is a need for national pediatric societies to focus their efforts on ensuring that jaundice guidelines are effectively disseminated to all newborn care practitioners, and not just pediatricians, as well as to level I newborn care hospitals, where most family physicians are practising. Another barrier to the use of guidelines might have been that they were not easy to use, as reported by 41% of family physicians.
Interestingly, most respondents across all practitioner types responded correctly to the jaundice case scenario of a newborn before hospital discharge with likely ABO incompatibility. (The correct response is b or d; Box 1.) This result supports the concept that once jaundice and its risk factors are recognized, practitioners will respond appropriately. Unfortunately, many cases of severe hyperbilirubinemia can occur in newborns with no recognized risk factors, and patients might not present to health care providers until it is too late to minimize the risks of excessive bilirubin exposure.14 This underscores the importance of appropriate surveillance and timely follow-up after discharge of all newborns, not just those at high risk.
Our study is unique in that family physicians and midwives were included, whereas most previous studies included mostly pediatricians and neonatologists.18,21,22 Another strength of the study was the random and unbiased sampling of caregivers and our ability to obtain demographic information on the respondents. Although only a small proportion of the total provincial practitioner pool was represented by those surveyed and by those who responded to the survey, our random sampling strategy should have minimized sampling bias; thus, the results might be somewhat representative of the work pool.
Limitations
An important limitation of our study was the low response rate, particularly by the family physician group. Community-based mail or electronic surveys have reported 20% to 30% response rates.29 We were able to attain comparable response rates from pediatricians and midwives, but the low response rate from family physicians might be owing to several factors. Reasons for the lack of response from physicians include lack of time, perceived salience of the study, and private office settings that have administrative assistants who act as gatekeepers to direct physician access.30 Family physicians who see newborns infrequently might not perceive the study to be salient. From the Canadian Medical Directory, we were unable to identify those family physicians who provided well-baby care. Rourke et al found that only 48% of family physicians in the Canadian Medical Directory in 2 regions in Ontario performed office-based well-baby care.31 Thus, it is likely that most of our random sample of family physicians did not provide newborn care and thus were not likely to respond to the survey. Of note, most respondents (94%) in the family physician group were family medicine practitioners rather than general practitioners which supports the hypothesis that family medicine practitioners were more likely to provide newborn care than general practitioners.
Demographic characteristics of the family physician respondents in our survey showed a higher proportion of men and older respondents compared with family physicians in the National Physician Survey32 and the Rourke et al survey.31 These differences in demographic characteristics might have introduced bias and lent uncertainty to the conclusions. Despite the possibility that family physicians did not find the topic salient to their practices, it is important for family physicians who see any newborns in their practices, albeit infrequently, to be aware of the guidelines if the risks of severe hyperbilirubinemia are to be minimized for all newborns.
Another limitation of our study was that the results represent self-reports of practices rather than an objective assessment of actual practices. Respondents might report what they believe to be acceptable or recommended practices rather than what they actually do; thus, the results might be more representative of their knowledge than their practices.18,33
Conclusion
Our survey demonstrated that the management of jaundice varied considerably among the various practitioner types, with pediatricians both most aware of the guidelines and most likely to follow them. Increased knowledge translation efforts are required to promote adherence to the jaundice management guidelines for all newborn practitioner types, but particularly among family physicians. Future studies are recommended to accurately determine the actual practices in the follow-up of newborn infants after discharge among different health care practitioners. This might be possible to assess through the use of available databases such as the Canadian Institute for Health Information database, which contains newborn delivery and length-of-stay data that can be linked to the Ontario Health Insurance Plan database, which can be used to assess timing of outpatient follow-up.
Acknowledgments
We thank Dr Sarah De La Rue from the MiCare Research Center (funded by the Ontario Ministry of Health and Long-Term Care) for editorial assistance with this manuscript. The study was funded by the Ontario Federation for Cerebral Palsy and the Canadian Medical Protective Association. This article was presented at the Annual Conference of the Canadian Paediatric Society in Vancouver, BC, in June 2010.
EDITOR’S KEY POINTS
Hyperbilirubinemia continues to be the most common cause of neonatal readmission to hospitals in North America. If not treated rapidly and effectively, severe hyperbilirubinemia can have devastating consequences such as kernicterus. Morbidity continues to occur despite attempts to identify at-risk newborns before discharge from the hospital, and despite the publication of guidelines to promote good practice in the screening and management of hyperbilirubinemia.
Significant variation was found in adherence to the guidelines by practitioner type. Routine monitoring of bilirubin at or before discharge was reported by only 42% of family physicians, compared with 63% of pediatricians and 22% of midwives (P < .001).
Barriers to adherence to guidelines are multifactorial and might include lack of awareness, lack of agreement, and inertia of previous practices. Lack of awareness might partially explain the low adherence to guidelines by family physicians compared with pediatricians. The Canadian Paediatric Society or American Academy of Pediatrics guidelines were used by only 41% of family physicians, and were described as easy to access by only 67% of family physicians compared with most pediatricians and midwives.
POINTS DE RÈPERE DU RÉDACTEUR
L’hyperbilirubinémie continue d’être la plus grande cause de réadmission néonatale à l’hôpital en Amérique du Nord. Faute d’un traitement rapide et efficace, cette condition peut avoir des conséquences aussi graves que le kernictère. Des problèmes de santé continuent de survenir malgré les efforts pour identifier les nouveau-nés à risque avant leur départ de l’hôpital et malgré la publication de directives sur la meilleure façon de dépister et de traiter l’hyperbilirubinémie.
On a observé que l’adhésion aux directives différait de façon significative selon les types de praticiens. Seulement 42 % des médecins de famille ont déclaré mesurer la bilirubine de façon routinière avant le congé ou au moment du congé, contre 63 % des pédiatres et 22 % des sages-femmes (P < ,001).
Les obstacles au respect des directives sont de plusieurs ordres, incluant notamment des connaissances insuffisantes, un désaccord avec les directives et la poursuite des anciennes habitudes de pratique. Le manque de connaissances pourrait partiellement expliquer que les médecins de famille respectent moins les directives que les pédiatres. Les directives de pratique de la Société canadienne de pédiatrie et de l’American Academy of Pediatrics ont été suivies par seulement 41 % des médecins de famille et elles ont été décrites comme facilement accessibles par seulement 67 % des médecins de famille, comparativement à la majorité des pédiatres et des sages-femmes.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the conception and analysis of the study and approved the contents of the manuscript.
Competing interests
None declared
References
- 1.Tan-Dy CM, Moore A, Satodia P, Blaser S, Fallagh S. Predicting kernicterus in severe unconjugated hyperbilirubinemia [Abst 7] Paediatr Child Health (Oxford) 2004;9(Suppl A) [Google Scholar]
- 2.Lee KS, Perlman M. The impact of early obstetric discharge on newborn health care. Curr Opin Pediatr. 1996;8(2):96–101. doi: 10.1097/00008480-199604000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Lee KS, Perlman M, Ballantyne M, Elliott I, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatr. 1995;127(5):758–66. doi: 10.1016/s0022-3476(95)70170-2. [DOI] [PubMed] [Google Scholar]
- 4.Liu S, Wen SW, McMillan D, Trouton K, Fowler D, McCourt C. Increased neonatal readmission rate associated with decreased length of hospital stay at birth in Canada. Can J Public Health. 2000;91(1):46–50. doi: 10.1007/BF03404253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown AK, Damus K, Kim MH, King K, Harper R, Campbell D, et al. Factors relating to readmission of term and near-term neonates in the first two weeks of life. Early Discharge Survey Group of the Health Professional Advisory Board of the Greater New York Chapter of the March of Dimes. J Perinat Med. 1999;27(4):263–75. doi: 10.1515/JPM.1999.037. [DOI] [PubMed] [Google Scholar]
- 6.Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA Kernicterus Registry (1992 to 2004) J Perinatol. 2009;29(Suppl 1):S25–45. doi: 10.1038/jp.2008.211. [DOI] [PubMed] [Google Scholar]
- 7.Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. CMAJ. 2006;175(6):587–90. doi: 10.1503/cmaj.060328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhutani VK, Johnson LH. Urgent clinical need for accurate and precise bilirubin measurements in the United States to prevent kernicterus. Clin Chem. 2004;50(3):477–80. doi: 10.1373/clinchem.2003.024489. Epub 2004 Jan 15. [DOI] [PubMed] [Google Scholar]
- 9.Bhutani VK, Johnson LH, Keren R. Diagnosis and management of hyperbilirubinemia in the term neonate: for a safer first week. Pediatr Clin North Am. 2004;51(4):843–61. vii. doi: 10.1016/j.pcl.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Johnson LH, Bhutani VK, Brown AK. System-based approach to management of neonatal jaundice and prevention of kernicterus. J Pediatr. 2002;140(4):396–403. doi: 10.1067/mpd.2002.123098. [DOI] [PubMed] [Google Scholar]
- 11.Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103(1):6–14. doi: 10.1542/peds.103.1.6. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics Subcommittee on Hyperbilirubinemia Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114(1):297–316. doi: 10.1542/peds.114.1.297. [DOI] [PubMed] [Google Scholar]
- 13.Barrington KJ, Sankaran K. Canadian Paediatric Society Fetus and Newborn Committee. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants. Paediatr Child Health (Oxford) 2007;12(Suppl B):1B–12B. [Google Scholar]
- 14.Maisels MJ, Newman TB. Kernicterus in otherwise healthy, breast-fed term newborns. Pediatrics. 1995;96(4 Pt 1):730–3. [PubMed] [Google Scholar]
- 15.Penn AA, Enzmann DR, Hahn JS, Stevenson DK. Kernicterus in a full term infant. Pediatrics. 1994;93(6 Pt 1):1003–6. [PubMed] [Google Scholar]
- 16.Scott’s Directories [website] Canadian medical directory. Toronto, ON: Scott’s Directories; 2008. Available from: www.mdselect.ca. Accessed 2010 Oct 13. [Google Scholar]
- 17.Kaplowitz MD, Hadlock TD, Levine R. A comparison of web and mail survey response rates. Public Opin Q. 2004;68(1):94–101. [Google Scholar]
- 18.Gartner LM, Herrarias CT, Sebring RH. Practice patterns in neonatal hyperbilirubinemia. Pediatrics. 1998;101(1 Pt 1):25–31. doi: 10.1542/peds.101.1.25. [DOI] [PubMed] [Google Scholar]
- 19.Association of Ontario Midwives . Clinical practice guidelines for midwives. No. 1—physical assessment of the newborn. Toronto, ON: Association of Ontario Midwives; 1999. Available from: www.aom.on.ca/files/Health_Care_Professionals/Clinical_Practice_Guidelines/No_1_-_Physical_Assessment_of_the_Newborn.pdf. Accessed 2013 Jul 15. [Google Scholar]
- 20.Association of Ontario Midwives . Clinical practice guidelines for midwives. No. 2—physical assessment of the well woman. Toronto, ON: Association of Ontario Midwives; 1999. Available from: www.aom.on.ca/files/Health_Care_Professionals/Clinical_Practice_Guidelines/No_2_-_Physical_Assessment_of_the_Well_Woman.pdf. Accessed 2013 Jul 15. [Google Scholar]
- 21.Profit J, Cambric-Hargrove AJ, Tittle KO, Pietz K, Stark AR. Delayed pediatric office follow-up of newborns after birth hospitalization. Pediatrics. 2009;124(2):548–54. doi: 10.1542/peds.2008-2926. Epub 2009 Jul 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atkinson LR, Escobar GJ, Takayama JI, Newman TB. Phototherapy use in jaundiced newborns in a large managed care organization: do clinicians adhere to the guideline? Pediatrics. 2003;111(5 Pt 1):e555–61. doi: 10.1542/peds.111.5.e555. [DOI] [PubMed] [Google Scholar]
- 23.Mol F, van den Boogaard E, van Mello NM, van der Veen F, Mol BW, Ankum WM, et al. Guideline adherence in ectopic pregnancy management. Hum Reprod. 2011;26(2):307–15. doi: 10.1093/humrep/deq329. Epub 2010 Dec 2. [DOI] [PubMed] [Google Scholar]
- 24.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 25.Canadian Paediatric Society [website] Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants. Ottawa, ON: Canadian Paediatric Society; 2007. Available from: www.cps.ca/english/statements/FN/fn07-02.htm. Accessed 2010 Sep 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ontario College of Family Physicians [website] Toronto, ON: Ontario College of Family Physicians; Available from: www.ocfp.on.ca. Accessed 2010 Jul 5. [Google Scholar]
- 27.Association of Ontario Midwives [website] Toronto, ON: Association of Ontario Midwives; Available from: www.aom.on.ca. Accessed 2010 Aug 15. [Google Scholar]
- 28.Guttman A, Schultz SE, Jaakkimainen L. Primary care for children. In: Jaakkimainen L, Upshur R, Klein-Geltink JE, Leong A, Maaten S, Schultz SE, et al., editors. Primary care in Ontario: ICES atlas. Toronto, ON: Institute for Clinical Evaluative Sciences; 2006. Available from: www.ices.on.ca/file/PC_atlas_prelims_complete.pdf. Accessed 2013 Jul 16. [Google Scholar]
- 29.Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev. 2007;(2):MR000008. doi: 10.1002/14651858.MR000008.pub3. [DOI] [PubMed] [Google Scholar]
- 30.VanGeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: a systematic review. Eval Health Prof. 2007;30(4):303–21. doi: 10.1177/0163278707307899. [DOI] [PubMed] [Google Scholar]
- 31.Rourke L, Godwin M, Rourke J, Pearce S, Bean J. The Rourke Baby Record Infant/Child Maintenance Guide: do doctors use it, do they find it useful, and does using it improve their well-baby visit records? BMC Fam Pract. 2009;10:28. doi: 10.1186/1471-2296-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . 2007 National Physician Survey. Mississauga, ON: College of Family Physicians of Canada; 2007. Available from: www.nationalphysiciansurvey.ca. Accessed 2010 Sep 10. [Google Scholar]
- 33.Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics. 1999;104(6):1251–7. doi: 10.1542/peds.104.6.1251. [DOI] [PubMed] [Google Scholar]


