Abstract
Background: It has been suggested that the cardiometabolic risk associated with excess adiposity is particularly related to central obesity.
Objective: The objective was to compare the associations between cardiometabolic risk of apparently healthy individuals and measures of central obesity [waist circumference (WC)] and overall obesity [body mass index (BMI)].
Design: In this cross-sectional, observational study, 492 subjects (306 women and 303 non-Hispanic whites) were classified by BMI (in kg/m2) as normal weight (BMI <25) or overweight/obese (BMI = 25.0–34.9) and as having an abnormal WC (≥80 cm in women and ≥94 cm in men) or a normal WC (<80 cm in women and <94 cm in men). Measurements were also made of the cardiometabolic risk factors age, systolic blood pressure (SBP), and fasting plasma glucose (FPG), triglyceride, and high-density lipoprotein (HDL)-cholesterol concentrations. Associations among cardiometabolic risk factors and BMI and WC were evaluated with Pearson correlations.
Results: There was a considerable overlap in the normal and abnormal categories of BMI and WC, and ∼81% of the subjects had both an abnormal BMI and WC. In women, BMI and WC correlated with SBP (r = 0.30 and 0.19, respectively), FPG (r = 0.25 and 0.22, respectively), triglycerides (r = 0.17 and 0.20, respectively), and HDL cholesterol (r = −0.23 and −0.20, respectively) (P < 0.01 for all). In men, BMI and WC also correlated with SBP (r = 0.22 and 0.22, respectively), FPG (r = 0.22 and 0.25, respectively), triglycerides (r = 0.21 and 0.18, respectively), and HDL cholesterol (r = −0.20 and −0.13, respectively) [P < 0.05 for all, except for the association of WC with HDL cholesterol (P = 0.08)].
Conclusions: Most individuals with an abnormal BMI also have an abnormal WC. Both indexes of excess adiposity are positively associated with SBP, FPG, and triglycerides and inversely associated with HDL cholesterol.
INTRODUCTION
Although the relation between obesity and cardiometabolic risk is well recognized, controversy continues about how best to identify those overweight/obese individuals who are at greatest risk. More recently, emphasis (1) has been placed on abdominal obesity, as measured by waist circumference (WC)4, as more reflective of such high-risk individuals than knowledge of BMI.
The superiority of using WC, rather than BMI, as an indicator of increased cardiometabolic risk is exemplified by its incorporation as 1 of the 5 criteria used to make a diagnosis of the metabolic syndrome (1). However, there is published evidence that the difference between abdominal obesity (WC) and overall obesity (BMI; in kg/m2) in predicting cardiometabolic risk is somewhat overstated (2–4). Furthermore, the elements that comprise the determination of BMI, height and weight, are routinely measured in physician-patient encounters, whereas WC is rarely measured. The goal of this study was to estimate the association between cardiometabolic risk factors and obesity by using 2 different measures of obesity.
SUBJECTS AND METHODS
Study subjects
The experimental observations were collected from 306 women and 186 men, approximately two-thirds of whom were of European ancestry. Participants had responded to newspaper advertisements from 1999 to 2010 describing our studies of the relation among obesity, insulin resistance, and cardiometabolic disease. Volunteers had normal findings on medical history, physical examination, and laboratory tests and had a BMI between 20.0 and 34.9. Individuals with a diagnosis of diabetes or a fasting plasma glucose (FPG) concentration ≥126 mg/dL were excluded. Stanford University's Human Subjects Committee approved the study protocols, and subjects gave written informed consent.
Experimental measurements
Height and weight were determined while subjects were wearing light clothing and no shoes, and BMI was calculated by dividing weight (kg) by height (m)2. Subjects with a BMI <25.0 were defined as normal weight and those with a BMI 25.0–34.9 as overweight/obese. WC was determined according to the NHANES III protocol during normal minimal respiration by placing a measuring tape around the waist just above the uppermost lateral border of the iliac crest (5). On the basis of the newly harmonized criteria for diagnosing the metabolic syndrome, women with a WC ≥80 cm and men with a WC ≥94 cm were classified as having an abnormal WC and women with a WC <80 cm and men with a WC <94 cm as having a normal WC (1). Blood pressure measurements were made with a Dinamap automatic blood pressure recorder (model 1846 SX), with an appropriate cuff size, while subjects sat quietly in a chair (6). Fasting lipid and lipoprotein concentrations were assayed in the core laboratory at Stanford University Medical Center by using standardized methods approved by the CDC; plasma glucose concentrations were measured as described previously (7, 8).
Statistical analysis
Summary statistics are presented as means ± SDs, means ± SEMs, or medians (IQRs). Linear associations of each cardiometabolic risk factor with BMI and WC were estimated with Pearson correlation coefficients, conducted separately for men and women because of possible sex differences in the association between cardiometabolic risk and obesity. Cardiometabolic risk factors—systolic blood pressure (SBP) and FPG, triglyceride, and HDL-cholesterol concentrations—were compared across the following 4 groups: 1) normal BMI and normal WC (n = 44), 2) normal BMI and abnormal WC (n = 26), 3) abnormal BMI and normal WC (n = 22), and 4) abnormal BMI and abnormal WC (n = 400). For each cardiometabolic risk factor, an omnibus 1-factor ANOVA was used to compare differences in group means. Follow-up pairwise comparisons were conducted by using least-significant difference tests. Triglyceride concentrations were log transformed to improve normality for parametric statistical tests. Statistical analyses were performed by using statistical software SPSS-IBM version 20.0.
RESULTS
The demographic and metabolic characteristic of all study participants (n = 492) are shown in Table 1. The mean (±SD) age of the participants was 50 ± 9 y. Most of the participants were women (62%) and of white non-Hispanic descent (61.6%) The average values for BMI and WC indicated that the study participants tended to be overweight/obese.
TABLE 1.
Clinical and metabolic characteristics of the study volunteers1
| Variable | Whole group(n = 492) | Women(n = 306) | Men(n = 186) |
| Age (y) | 50 ± 92 | 49 ± 9 | 51 ± 9 |
| Non-Hispanic white (n) | 303 | 176 | 127 |
| BMI (kg/m2) | 28.5 ± 3.5 | 28.3 ± 3.5 | 28.8 ± 3.5 |
| WC (cm) | 96 ± 11 | 93 ± 11 | 101 ± 9 |
| SBP (mm Hg) | 122 ± 16 | 119 ± 16 | 127 ± 15 |
| Triglycerides (mg/dL) | 135 ± 119107 (72, 162)3 | 117 ± 11494 (69, 140) | 165 ± 120129 (90, 199) |
| HDL cholesterol (mg/dL) | 48 ± 14 | 52 ± 13 | 40 ± 10 |
| FPG (mg/dL) | 96 ± 10 | 95 ± 10 | 98 ± 10 |
FPG, fasting plasma glucose; SBP, systolic blood pressure; WC, waist circumference.
Mean ± SD (all such values).
Median; IQR in parentheses (all such values).
The considerable overlap in the normal and abnormal categories of BMI and WC among the 492 individuals is shown in Table 2. Of the 426 volunteers with abnormal WC, 400 (94%) were also overweight/obese as defined by BMI criteria. Similarly, of the 422 volunteers classified as overweight/obese by their BMI, 400 (95%) were classified as abnormal by WC. The overlap in the number of individuals classified as abnormal by both criteria was consistent with the observed linear correlation between BMI and WC (r = 0.75, P < 0.001).
TABLE 2.
Overlap among the individuals (n = 492) classified as normal or abnormal by BMI and WC1
| Normal WC(n = 66) | Abnormal WC(n = 426) | |
| n | n | |
| Normal weight (n = 70) | 44 | 26 |
| Overweight/obese (n = 422) | 22 | 400 |
Individuals with a BMI (in kg/m2) <25.0 were defined as normal weight and those with a BMI of 25.0–34.9 as overweight/obese. Women with a WC <80 cm and men with a WC <94 cm were classified as having a normal WC and women with a WC ≥80 cm and men with a WC ≥94 cm as having an abnormal WC. WC, waist circumference.
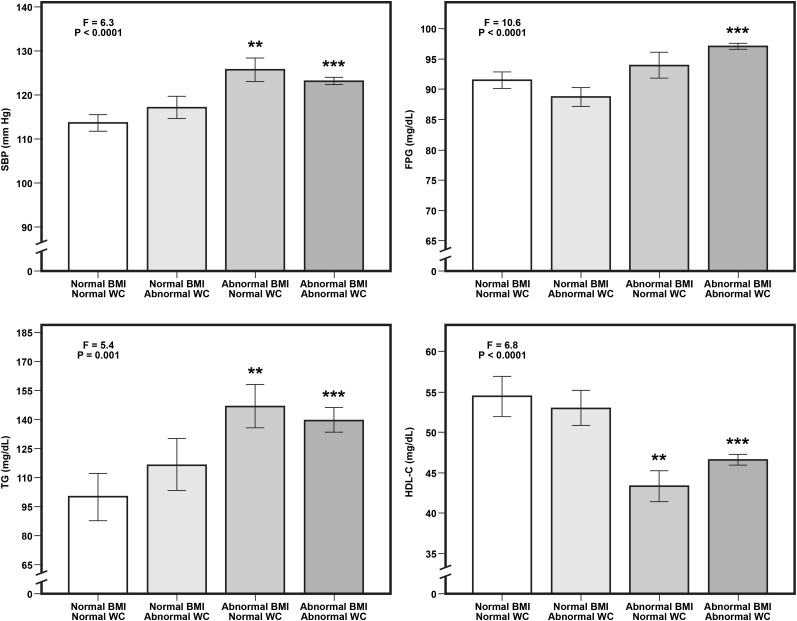
The mean (±SEM) cardiometabolic risk factor profiles of individuals who had both a normal BMI and WC (n = 44), only an abnormal WC (n = 26), only an abnormal BMI (n = 22), or both an abnormal BMI and WC (n = 400) are shown in Figure 1. These data are relevant to 2 issues. First, they emphasize the degree of overlap of the 2 indexes: 48 individuals had only one abnormality (26 with only an abnormal WC and 22 with only an elevated BMI). Second, they indicate that individuals with both abnormal BMI and abnormal WC had a more adverse cardiometabolic profile (P < 0.0001) than did those with neither of the indexes being elevated. Individuals with only one abnormality (abnormal BMI) had a significantly higher mean SBP (P = 0.003) and triglyceride concentration (P = 0.001) and lower mean HDL-cholesterol concentration (P = 0.001) than did those with both normal BMI and WC. On the other hand, subjects with only abnormal WC did not have a significantly higher mean SBP (P = 0.36), FPG concentration (P = 0.25), or triglyceride concentration (P = 0.12) or lower mean HDL-cholesterol concentration (P = 0.67) compared with those with both a normal BMI and WC.
FIGURE 1.
Mean (±SEM) values for cardiometabolic risk factors in individuals with normal BMI and normal WC (n = 44), normal BMI and abnormal WC (n = 26), abnormal BMI and normal WC (n = 22), and abnormal WC and abnormal BMI (n = 400). In each panel, the F statistic and the accompanying P value indicate the overall difference in means between the 4 groups (1-factor ANOVA). Significant differences in means between the groups: ***P < 0.0001 and **P < 0.01 for comparison with the normal BMI and normal WC group (least-significant difference pairwise comparison test). Normal BMI (in kg/m2), <25.0; abnormal BMI, 25.0–34.9; normal WC, <80 cm (women) and <94 cm (men); and abnormal WC, ≥80 cm (women) and ≥94 cm (men). C, cholesterol; FPG, fasting plasma glucose; SBP, systolic blood pressure; TG, triglycerides; WC, waist circumference.
The relations between the 2 indexes of obesity (ie, BMI and WC) and cardiometabolic risk were estimated for women and men (Table 3). In women, statistically significant correlations were found between each measure of obesity and SBP, FPG, triglycerides, and HDL cholesterol. In men, the results were essentially similar to those seen in women. Specifically, both BMI and WC significantly correlated with SBP, FPG, and triglycerides. However, in this instance, BMI, but not WC, was significantly related to HDL cholesterol.
TABLE 3.
Associations of cardiometabolic risk factors with BMI and WC in women and men1
| Women (n = 306) |
Men (n = 186) |
|||||||
| BMI |
WC |
BMI |
WC |
|||||
| Risk factor | r | P (2-tailed) | r | P (2-tailed) | r | P (2-tailed) | r | P (2-tailed) |
| Age | 0.06 | 0.31 | 0.19 | 0.001 | 0.06 | 0.46 | 0.17 | 0.02 |
| SBP | 0.30 | <0.001 | 0.19 | 0.001 | 0.22 | 0.003 | 0.22 | 0.003 |
| FPG | 0.25 | <0.001 | 0.22 | <0.001 | 0.22 | 0.003 | 0.25 | 0.001 |
| Triglycerides | 0.17 | 0.003 | 0.20 | <0.001 | 0.21 | 0.005 | 0.18 | 0.02 |
| HDL cholesterol | −0.23 | <0.001 | −0.20 | 0.001 | −0.20 | 0.007 | −0.13 | 0.08 |
Triglyceride concentrations were log transformed for statistical tests. FPG, fasting plasma glucose; SBP, systolic blood pressure; WC, waist circumference.
DISCUSSION
It seems essential before beginning the discussion of the findings of this study to distinguish between the following 2 basically different, but related issues: 1) why are overweight/obese individuals more likely to have the cardiometabolic risk factors associated with insulin resistance, and 2) what index of obesity provides the most useful clinical information in identifying enhanced cardiometabolic risk in apparently healthy individuals. It is obvious that the focus of our study was on the second question.
If the clinical goal is to identify individuals at increased cardiometabolic risk associated with excess adiposity, it is obvious from Table 2 that there were essentially as many individuals identified as being overweight/obese (n = 422) as abdominally obese (n = 426). Furthermore, most (95%) of the overweight/obese subjects were abdominally obese, and basically the same proportion (94%) of abdominally obese individuals was overweight/obese. This enormous degree of overlap, by itself, suggests that either index of excess adiposity will identify the same persons.
More specific evidence for the notion that BMI and WC both identify individuals whose excess adiposity puts them at increased cardiometabolic risk is provided in Table 3. Thus, in women, statistically significant associations were observed between WC and all the variables measured, and BMI correlated with all variables except age. The results were somewhat different in men in that WC was not significantly related to HDL cholesterol.
On the basis of the results presented, it seems justified to extrapolate to the clinical situation by concluding that the cardiometabolic risk profile of individuals whose BMI defines them as being overweight/obese will not differ substantially from that of subjects identified as being abdominally obese because of their enlarged WC. On the other hand, it must be acknowledged that our findings are only relevant to the goal of identifying individuals at increased cardiometabolic risk and may not apply to the index of excess adiposity best able to predict clinical outcome. We do not have outcome data, but this issue has been addressed in other studies (9–12), which showed that the 2 indexes of excess adiposity did not differ in their ability to predict cardiovascular disease, type 2 diabetes, or excess mortality. Furthermore, perhaps of greater relevance, is evidence that obesity, per se, may not be the crucial issue. Thus, Ninomiya et al (13), using data from NHANES III, concluded that obesity, as estimated from WC, was not an independent predictor of myocardial infarction, whereas insulin resistance, hypertension, low HDL cholesterol, and hypertriglyceridemia were “independently and significantly related.” Similarly, The Emerging Risk Factors Collaboration, based on prospective studies of 221,934 individuals from 17 countries (14), concluded that “BMI, waist circumference, and waist-to-hip ratio, whether assessed singly or in combination, do not importantly improve cardiovascular disease risk prediction in people in developed countries when additional information is available for systolic blood pressure, history of diabetes, and lipids.” Consequently, it could be argued that the central clinical question should be how to best identify the subset of those individuals who are at increased risk of developing many adverse clinical syndromes because of excess adiposity. We suggest that our findings show that documenting the presence of abdominal obesity by measuring WC offers no clinical advantage over using BMI to accomplish that goal.
Although our findings are straightforward, our experimental protocol suffers from ≥2 drawbacks. As indicated previously, our findings are relevant to risk of disease, not disease outcome. Furthermore, 61.6% of our population was of European ancestry; the remainder consisting of South Asians (13.8%), East Asians (10%), Hispanics (8.9%), and African Americans (5.9%). Thus, our findings may not apply to these other groups. On the other hand, we addressed these issues in a large number of subjects with a broad evaluation of cardiometabolic risk factors.
In conclusion, a similar number of individuals at increased cardiometabolic risk because of excess adiposity will be identified by having a BMI ≥25.0 rather than because of satisfying current WC criteria for abdominal obesity (1), and the ensuing risk profile will be of comparable clinical utility. Therefore, clinicians could continue to use BMI, and not substitute it with WC, to identify overweight/obese individuals who are potentially at increased cardiometabolic risk.
Acknowledgments
The authors’ responsibilities were as follows—FA: had full access to all of the data in the study, collected the data, and takes responsibility for the integrity of the data and the accuracy of the data analysis; FA and GMR: designed the study; FA and CB: analyzed the data; and FA, CB, and GMR: interpreted the results and wrote the manuscript. None of the authors had a potential conflict of interest.
Footnotes
Abbreviations used: FPG, fasting plasma glucose; SBP, systolic blood pressure; WC, waist circumference.
REFERENCES
- 1.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 2.Farin HM, Abbasi F, Reaven GM. Body mass index and waist circumference both contribute to differences in insulin-mediated glucose disposal in nondiabetic adults. Am J Clin Nutr 2006;83:47–51. [DOI] [PubMed] [Google Scholar]
- 3.Farin HM, Abbasi F, Reaven GM. Comparison of body mass index versus waist circumference with the metabolic changes that increase the risk of cardiovascular disease in insulin-resistant individuals. Am J Cardiol 2006;98:1053–6. [DOI] [PubMed] [Google Scholar]
- 4.Ryan MC, Fenster Farin HM, Abbasi F, Reaven GM. Comparison of waist circumference versus body mass index in diagnosing metabolic syndrome and identifying apparently healthy subjects at increased risk of cardiovascular disease. Am J Cardiol 2008;102:40–6. [DOI] [PubMed] [Google Scholar]
- 5.National Institutes of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. Obes Res 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 6.Williams RR, Rao DC, Ellison RC, Arnett DK, Heiss G, Oberman A, Eckfeldt JH, Leppert MF, Province MA, Mockrin SC, et al. NHLBI family blood pressure program: methodology and recruitment in the HyperGEN network. Hypertension genetic epidemiology network. Ann Epidemiol 2000;10:389–400. [DOI] [PubMed] [Google Scholar]
- 7.Abbasi F, Chu JW, McLaughlin T, Lamendola C, Leary ET, Reaven GM. Effect of metformin treatment on multiple cardiovascular disease risk factors in patients with type 2 diabetes mellitus. Metabolism 2004;53:159–64. [DOI] [PubMed] [Google Scholar]
- 8.Lamendola C, Abbasi F, Chu JW, Hutchinson H, Cain V, Leary E, McLaughlin T, Stein E, Reaven G. Comparative effects of rosuvastatin and gemfibrozil on glucose, insulin, and lipid metabolism in insulin-resistant, nondiabetic patients with combined dyslipidemia. Am J Cardiol 2005;95:189–93. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr 2009;89:1213–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore SC. Waist versus weight: which matters more for mortality? Am J Clin Nutr 2009;89:1003–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor AE, Ebrahim S, Ben-Shlomo Y, Martin RM, Whincup PH, Yarnell JW, Wannamethee SG, Lawlor DA. Comparison of the associations of body mass index and measures of central adiposity and fat mass with coronary heart disease, diabetes, and all-cause mortality: a study using data from 4 UK cohorts. Am J Clin Nutr 2010;91:547–56. [DOI] [PubMed] [Google Scholar]
- 12.van Dis I, Kromhout D, Geleijnse JM, Boer JM, Verschuren WM. Body mass index and waist circumference predict both 10-year nonfatal and fatal cardiovascular disease risk: study conducted in 20,000 Dutch men and women aged 20-65 years. Eur J Cardiovasc Prev Rehabil 2009;16:729–34. [DOI] [PubMed] [Google Scholar]
- 13.Ninomiya JK, L'Italien G, Criqui MH, Whyte JL, Gamst A, Chen RS. Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Circulation 2004;109:42–6. [DOI] [PubMed] [Google Scholar]
- 14.Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet 2011;377:1085–95. [DOI] [PMC free article] [PubMed] [Google Scholar]