Abstract
Background
The use of larval source management is not prioritized by contemporary malaria control programs in sub-Saharan Africa despite historical success. Larviciding, in particular, could be effective in urban areas where transmission is focal and accessibility to Anopheles breeding habitats is generally easier than in rural settings. The objective of this study is to assess the effectiveness of a community-based microbial larviciding intervention to reduce the prevalence of malaria infection in Dar es Salaam, United Republic of Tanzania.
Methods and Findings
Larviciding was implemented in 3 out of 15 targeted wards of Dar es Salaam in 2006 after two years of baseline data collection. This intervention was subsequently scaled up to 9 wards a year later, and to all 15 targeted wards in 2008. Continuous randomized cluster sampling of malaria prevalence and socio-demographic characteristics was carried out during 6 survey rounds (2004–2008), which included both cross-sectional and longitudinal data (N = 64,537). Bayesian random effects logistic regression models were used to quantify the effect of the intervention on malaria prevalence at the individual level. Effect size estimates suggest a significant protective effect of the larviciding intervention. After adjustment for confounders, the odds of individuals living in areas treated with larviciding being infected with malaria were 21% lower (Odds Ratio = 0.79; 95% Credible Intervals: 0.66–0.93) than those who lived in areas not treated. The larviciding intervention was most effective during dry seasons and had synergistic effects with other protective measures such as use of insecticide-treated bed nets and house proofing (i.e., complete ceiling or window screens).
Conclusion
A large-scale community-based larviciding intervention significantly reduced the prevalence of malaria infection in urban Dar es Salaam.
Introduction
The Ross-Macdonald model of malaria transmission suggests that control methods that reduce adult mosquitoes’ longevity can achieve greater malaria reduction than strategies that target larval stages. Yet, Larval Source Management (LSM), such as the use of larvicides and the draining of breeding habitats, has historically been a very successful tool to reduce mosquito density [1] – examples include the elimination of Anopheles arabiensis from Egypt [2] and Brazil [3], malaria control in the Zambian copperbelt (1930–1950) [4], Dr. Gorga’s work during the construction of the Panama canal [5], and the vector control program of the Tennessee Valley Authority [6]. With the discovery of DDT, however, such approaches where disfavored as exemplified by the almost exclusive use of this potent insecticide during the Global Malaria Eradication Program (1955–1969) [7]. In addition, LSM programs were often associated with vertical, authoritarian management. Currently, there are few examples of LSM initiatives in post-colonial Africa [8]–[10]. LSM is often perceived as a secondary malaria control strategy, labor-intensive, requiring strong managerial support and oversight for monitoring and evaluation [11], [12], and often beyond the financial and operational capabilities of most malaria endemic areas in sub-Saharan Africa [13].
Such considerations might explain the insufficient evidence-base of LSM in post-colonial Africa, and the contemporary prioritization of malaria control programs that rely on Insecticide-Treated Nets (ITNs) and Insecticide Residual Spraying (IRS) as the main vector control measures. Nevertheless, a renewal of interest in applications of LSM within the sub-Saharan context has been observed recently [14]–[18]. In fact, in April of 2012, the World Health Organization (WHO) released an interim position statement [19] on the use of larvicides for malaria control in sub-Saharan Africa, recognizing that larviciding should be considered for malaria control but only in areas where breeding sites are ‘few, fixed and findable’ [19]. Larval control is regarded as being of secondary importance in comparison with IRS and ITNs. Although the WHO acknowledges that larvicides could be effective as one of the leading methods of vector control in urban areas of sub-Saharan Africa, it highlights the lack of recent and sound evidence of its effectiveness. Few contemporary studies have assessed the effectiveness of larvicides on malaria infection. Studies in highland valley communities of Kenya [20] and urban Tanzania [21] demonstrated substantial reduction in malaria prevalence, while no reductions were observed in a study conducted in a rural setting in The Gambia [22]. Strong empirical evidence on the causal effect of larviciding on malaria infection is difficult to obtain since larviciding interventions need to be implemented and scaled-up over large areas, appropriate control groups with similar malaria ecology are difficult to find, and the cost of such trials can be prohibitively expensive [14].
The rationale for adding larvicides to the arsenal of malaria control tools in urban areas is manifold. First, in contrast to rural areas, vector breeding habitats are generally fewer and much easier to reach in highly densely populated areas [10]. Second, the most potent malaria vector in Africa, An. gambiae, has been shown to exhibit exophagic behavior in some urban areas - although the majority of bites still take place indoors [23]. If this behavior intensifies over time, and therefore more biting and resting start to occur outside of homes, the efficacy of both IRS and ITNs would be reduced. Mathematical models have provided evidence that the outdoor biting rate defines what is achievable in terms of malaria reduction with IRS and ITNs [24]. LSM is one of the few strategies that could contribute to further reduce malaria when Anopheles are partially exophagic [14]. Third, insecticide resistance has emerged for the primary malaria vectors in many areas of the African continent [25]–[28] and combining IRS and ITN with larviciding could become more desirable in such settings. Finally, relying solely on IRS and ITNs may be insufficient to achieve malaria elimination in much of sub-Saharan Africa [29], [30]. As such, larviciding may be part of an integrated vector management (IVM) approach [31] that could help hinder malaria transmission [18]. Such informed use of larvicides, based on local malaria ecology, is in line with WHO’s current position on IVM [31], [32].
Africa is the fastest urbanizing continent in the world and its share of urban population is expected to double between 2000 and 2030 [33]. Malaria intensity is generally much lower in urban areas and transmission is highly focal [34], [35]. A corollary of this reduced endemicity is that urban dwellers will develop lower levels of clinical immunity to the disease, which can pose public health challenges. It has been estimated that about 28% of the malaria burden in sub-Saharan Africa is attributable to urban malaria [34]. Malaria control in urban settings offers more options than for rural areas because logistical constraints are alleviated by relatively good transportation, education, communication, and health infrastructures [36].
Following this rationale, the Dar es Salaam Urban Malaria Control Program (UMCP) was launched in 2004, targeting 15 of the city’s 73 wards, covering 56 km2 of the city, and a population of more than 610,000 residents [36]. The goal was to develop a sustainable larval control intervention as one of the main components of a malaria control strategy. Regular application of microbial larvicides was initiated in 2006 through vertically managed community-based delivery systems [36]. Initial results, restricted to children under five years of age and comprising data from the first period of larviciding (2006–2007) in three wards of the city (N = 4,450), demonstrated that this intervention reduced by 72% the odds of malaria infection [21]. In addition, rigorous monitoring of larval population in the same period showed that larviciding reduced anopheline larval abundance by 96% [36]. The larviciding intervention was scaled-up to 9 wards in 2007 and to all 15 wards in 2008.
In this paper, we will comprehensively investigate the effectiveness of the larviciding intervention on reducing malaria prevalence using 4.6 years of data, including individuals of all ages, and combining both cross-sectional and longitudinal data (N = 64,537). This will provide crucial evidence on the potential contribution of larvicide use for reducing population-level malaria burden in urban areas of sub-Saharan Africa.
Materials and Methods
Study site
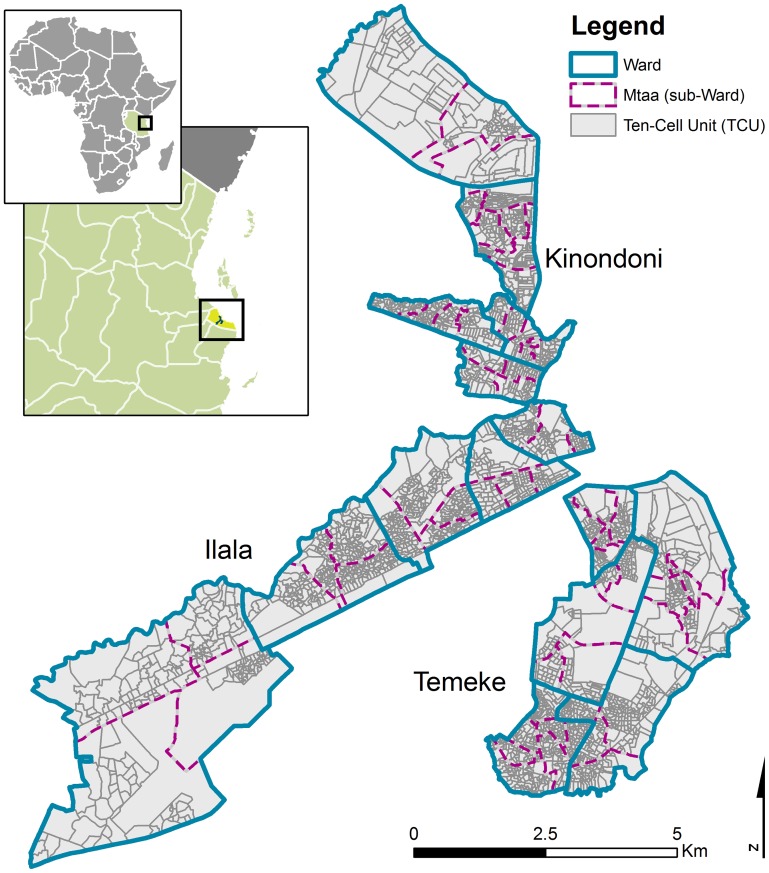
Dar es Salaam is the largest city and economic capital of the United Republic of Tanzania with an estimated population of 2.7 million in 2005 [37]. The climate is tropical humid with two rainy seasons – the long rains during the months of April and May and the short rains of October and November. Malaria transmission is year-round [38] with peaks in incidence after the two rainy seasons. Plasmodium falciparum accounts for more than 90% of cases and the principal vectors involved in malaria transmission are An. gambiae s.s. and An. funestus [10]. An. coustani’s contribution to malaria transmission is believed to be marginal [21]. Dar es Salaam is composed of three municipalities: Illala, Temeke, and Kinondoni. These municipalities are further divided in 73 wards (Figure 1). Each ward is comprised of administrative sub-units called mtaa (plural mitaa) which are further divided in ten-cell units (TCU) – the smallest administrative unit that contains approximately 10–20 houses, but may also contain as many as 100 [10].
Figure 1. Map of the study area and administrative units.
The northern portion belongs to the municipality of Kinondoni, the south-eastern portion to Temeke, and the south-western part to Ilala.
Design of the larviciding intervention
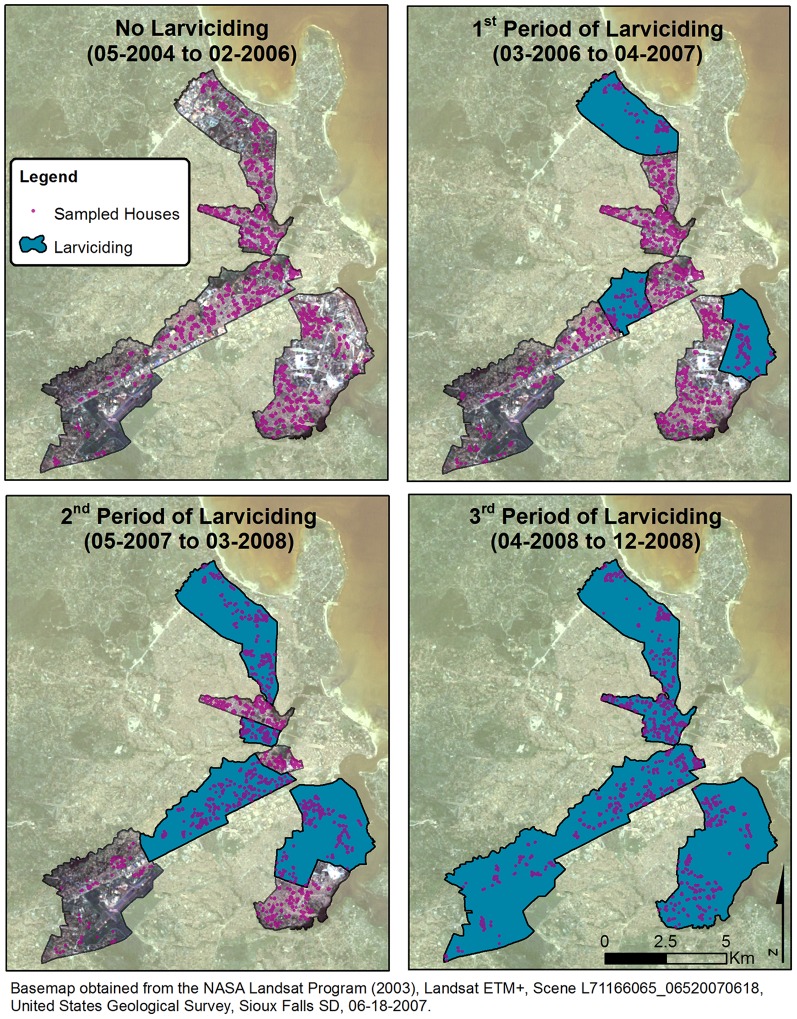
The Dar es Salaam’s UMCP was launched in 2004, and targeted 15 wards, five in each of the three municipalities, totaling 67 mitaa. During the first phase of the project (May 2004 to February 2006), systems for extensive mapping [39], [40] and surveillance of potential mosquito breeding sites were developed [36]. In 2005, routine surveillance of immature and adult mosquitoes was fully operationalized. Comprehensive larviciding of the identified breeding habitats debuted in March 2006 in three wards (Figure 2). The program was community-based but the UMCP remained responsible for vertical management and supervision. This entailed that responsibility for routine mosquito control and surveillance was delegated to modestly paid community members referred to as Community-Owned Resource Person (CORP) [11], [12], [41]. After 13 months of larviciding in these three wards, operations were extended to six additional wards: two in each municipality, totaling 9 wards covered by larviciding activities. Finally, about 12 months later, in April of 2008, the intervention was scaled-up to all 15 wards of the UMCP. The order in which wards were chosen to receive the larviciding intervention was not randomly allocated. Rather, the choice was the result of careful consideration of the following two criteria: (i) the availability of comprehensive and detailed maps of the ward, and (ii) the proven ability of the ward supervisor and CORPs to efficiently undertake the required tasks.
Figure 2. Map control and intervention wards and location of sampled households for each larviciding period.
The biological agents Bacillus thuringiensis var. israelensis (Bti; VectoBac® Valent BioSciences Corporation, VBC, USA) and Bacillus sphaericus (Bs; VectoLex®, VBC, USA) were used to control the aquatic stages of anopheline mosquitoes. Each mtaa, or portion of a mtaa, was under the responsibility of a designated CORP who was instructed to treat breeding habitats on a weekly basis. The dosage was 0.04 grams per m2 and 1 gram per m2 for Bti and Bs, respectively. Closed habitats that mainly breed Culex quinquefaciatus were treated with Bs every three months by a separate team of CORPs (although Culex mosquitoes play no role in malaria transmission, this was a programmatic decision to gain support from the community).
UMCP Data collection
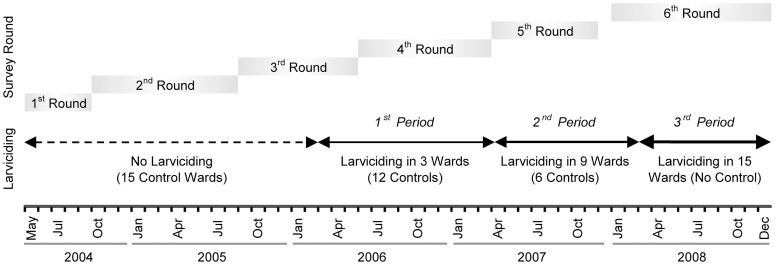
During the study period, a total of six randomized cluster-sampled household surveys were carried out (Figure 3). A list of TCUs was assembled for each ward before March of 2004 and was regularly updated throughout the study duration. During the first round of the survey, ten TCUs were randomly sampled from each of the 15 wards. All households located in the sampled TCUs were invited to participate in the survey. From the second round onwards, the TCUs sampled in the first round were followed-up longitudinally, and another ten TCUs per ward were selected for cross-section surveys. Since loss to follow-up is non-negligible in urban areas, starting from the 3rd survey round, the list of subjects to be followed-up also included randomly selected subjects interviewed in previous cross-section surveys. This was implemented in order to guarantee that the minimum required sample size would be met. Sample size calculations used a significance level of 5% and 80% power to detect a 5% absolute difference in malaria prevalence from 10% baseline prevalence. This is equivalent to a ±50% relative risk of infection. Calculations were based on mean TCU population size [21].
Figure 3. Timeline of data collection activities and larviciding intervention.
The first survey round was conducted form 05/2004 to 09/2004, the second from 10/2004 to 08/2005, the third from 09/2005 to 05/2006, the fourth from 06/2006 to 03/2007, the fifth from 04/2007 to 11/2007, and the sixth and last survey round from 01/2008 to 12/2008. The first period of the intervention started on March 1st 2006, the second period of larviciding on May 1st 2007, and the last period of larviciding on April 1st 2008.
Upon consenting to the interview, each household was geo-referenced using a hand-held global positioning system (GPS) device. A detailed questionnaire was administered, collecting information grouped in four modules: (i) house characteristics (e.g., location, conditions, number of habitants); (ii) head of the household (e.g., occupation, education, knowledge of malaria transmission and disease symptoms, assets, agricultural practices); (iii) use of preventive measures (e.g., bednet, mosquito repellent, coil); and (iv) individual characteristics (e.g., age and sex of all household members, occurrence of fever in the past two weeks, treatment-seeking behavior, use of antimalarial drug, sleeping habits, travel history). A proxy for socio-economic status was constructed using an asset-based index calculated by performing Principal Component Analysis [42] of the households’ possession, excluding protective assets such as bednets and window screenings. Table 1 describes the variables selected for this study, their type and, if appropriate, the way they were categorized.
Table 1. Characteristics of study participants stratified by survey round and intervention group (lagged by 5 weeks).
| Variables | Survey round #1 | Survey round #2 | Survey round #3 | Survey round #4 | Survey round #5 | Survey round #6 | |||||
| Control | Control | Control | Larvicide | Control | Larvicide | Control | Larvicide | Control | Larvicide | ||
| Outcome: Prevalence of malaria infection | 20.8% | 16.9% | 10.2% | 13.1% | 7.1% | 4.6% | 5.2% | 4.4% | 2.3% | 1.7% | |
| Individual-Level Variables | n = 5,809 | n = 11,149 | n = 10,791 | n = 697 | n = 9,951 | n = 2,385 | n = 6,461 | n = 5,663 | n = 744 | n = 10,887 | |
| Age | |||||||||||
| 0 to <5 years of age | 16.0% | 14.9% | 15.3% | 15.1% | 13.5% | 12.7% | 12.3% | 11.5% | 18.4% | 10.3% | |
| 5 to <15 years of age | 27.7% | 27.7% | 27.2% | 30.1% | 28.3% | 28.9% | 28.0% | 31.0% | 26.7% | 30.3% | |
| 15 to <30 years of age | 28.5% | 29.2% | 28.4% | 29.1% | 29.0% | 29.3% | 28.6% | 28.6% | 30.4% | 29.3% | |
| 30 to <45 years of age | 15.8% | 16.3% | 16.8% | 14.5% | 17.0% | 16.6% | 19.2% | 18.7% | 14.7% | 18.4% | |
| 45 to <60 years of age | 7.1% | 7.2% | 7.2% | 8.3% | 7.3% | 7.6% | 7.8% | 6.6% | 5.2% | 7.5% | |
| ≥ 60 years of age | 4.9% | 4.7% | 5.1% | 2.9% | 4.8% | 4.9% | 4.2% | 3.7% | 4.6% | 4.2% | |
| Missing | 0.2% | 0.2% | 0.1% | 0% | 0.1% | 0% | 0% | 0% | 0% | 0% | |
| Place slept in previous two weeks | |||||||||||
| Outside the ward | 2.9% | 2.1% | 6.2% | 12.1% | 8.4% | 9.3% | 4.7% | 8.5% | 29.2% | 5.1% | |
| Missing | 0.1% | 0.1% | 0.1% | 0% | 0.2% | 0.1% | 0% | 0% | 0% | 0.1% | |
| Male sex | 36.7% | 35.0% | 34.5% | 35.4% | 35.3% | 37.0% | 36.2% | 38.4% | 35.2% | 39.0% | |
| Slept under a bed net the night before | 78.7% | 88.9% | 85.3% | 97.6% | 87.8% | 78.9% | 86.0% | 82.2% | 94.2% | 91.5% | |
| Slept under an ITN the night before | 20.5% | 23.4% | 27.8% | 23.7% | 24.8% | 20.5% | 20.9% | 20.7% | 14.2% | 29.3% | |
| Use of coil the night before | 4.9% | 5.8% | 6.6% | 8.9% | 7.4% | 5.1% | 8.6% | 8.0% | 2.2% | 5.7% | |
| Use of repellent the night before | 0.3% | 1.3% | 1.6% | 4.9% | 5.0% | 3.4% | 3.0% | 3.0% | 0.5% | 3.3% | |
| Use of spray the night before | 8.4% | 10.5% | 15.8% | 16.8% | 21.0% | 18.2% | 30.8% | 30.6% | 6.6% | 29.2% | |
| Took malaria drug in previous two weeks | 7.4% | 3.7% | 5.4% | 3.0% | 8.2% | 3.9% | 4.9% | 6.9% | 6.3% | 2.0% | |
| Interviewed during wet season | 10.7% | 49.7% | 56.2% | 100.0% | 27.4% | 37.5% | 64.2% | 12.8% | 99.5% | 46.5% | |
| Follow-up observation | 0% | 17.0% | 26.5% | 24.1% | 31.2% | 32.1% | 35.2% | 32.8% | 17.2% | 27.2% | |
| Household-Level Covariates | N = 1,240 | N = 2,107 | N = 2,038 | N = 124 | N = 1,824 | N = 396 | N = 1,046 | N = 827 | N = 103 | N = 1,549 | |
| Occupation of household head/designated | |||||||||||
| Business / Government / Formal sector | 63.1% | 58.2% | 59.8% | 67.7% | 67.0% | 64.4% | 60.7% | 68.0% | 37.9% | 76.7% | |
| Farmer / Fisherman | 3.3% | 1.6% | 2.1% | 0.0% | 0.9% | 2.0% | 1.4% | 0.7% | 0% | 0.8% | |
| Informal sector | 16.9% | 17.8% | 21.1% | 22.6% | 19.7% | 16.7% | 22.8% | 17.9% | 53.4% | 12.5% | |
| Retired / No job / Domestic | 15.2% | 20.5% | 16.3% | 9.7% | 11.3% | 15.2% | 13.3% | 12.9% | 7.8% | 9.0% | |
| Missing | 1.5% | 1.9% | 0.8% | 0% | 1.0% | 0.8% | 1.7% | 0.5% | 1.0% | 1.0% | |
| Socio-Economic Status | |||||||||||
| Lowest quintile | 32.0% | 32.3% | 29.7% | 12.9% | 20.4% | 24.0% | 7.3% | 7.3% | 3.9% | 8.4% | |
| Second quintile | 29.4% | 28.7% | 26.2% | 20.2% | 23.6% | 15.4% | 20.9% | 16.3% | 11.7% | 15.0% | |
| Third quintile | 13.6% | 12.1% | 16.0% | 20.2% | 19.9% | 18.9% | 14.1% | 15.7% | 57.3% | 18.1% | |
| Fourth quintile | 12.1% | 11.2% | 12.5% | 21.8% | 19.7% | 19.9% | 29.2% | 30.7% | 23.3% | 29.1% | |
| Highest quintile | 12.9% | 15.7% | 15.5% | 25.0% | 16.3% | 21.7% | 28.5% | 30.0% | 3.9% | 29.4% | |
| Education of Household Head/Designated | |||||||||||
| Illiterate | 6.0% | 4.5% | 9.4% | 0.8% | 6.4% | 5.3% | 2.6% | 2.7% | 13.6% | 1.6% | |
| Primary | 64.4% | 60.6% | 51.0% | 50.0% | 46.2% | 48.0% | 35.9% | 30.8% | 48.5% | 35.6% | |
| Secondary | 26.9% | 28.2% | 33.3% | 37.9% | 42.0% | 39.6% | 57.4% | 60.2% | 37.9% | 59.3% | |
| Tertiary | 1.7% | 3.6% | 4.9% | 11.3% | 4.5% | 5.8% | 3.4% | 5.4% | 0% | 2.9% | |
| Other | 0.2% | 0.2% | 0.4% | 0% | 0.1% | 0.5% | 0% | 0% | 0% | 0.1% | |
| Missing | 1.0% | 2.9% | 1.0% | 0% | 0.9% | 0.8% | 0.7% | 0.8% | 0% | 0.6% | |
| Know how malaria is transmitted | 68.7% | 62.4% | 78.4% | 83.9% | 82.9% | 84.3% | 90.2% | 90.1% | 81.6% | 88.6% | |
| House has window screening | 22.0% | 19.7% | 29.5% | 37.9% | 23.7% | 48.0% | 21.5% | 28.3% | 31.1% | 39.1% | |
| House has complete ceiling | 27.6% | 24.8% | 24.1% | 35.5% | 29.4% | 36.4% | 42.4% | 46.8% | 14.6% | 33.2% | |
| Own house | 51.9% | 63.1% | 72.4% | 66.1% | 76.4% | 80.3% | 81.2% | 80.2% | 85.4% | 85.7% | |
| Household cultivates crops | 19.4% | 11.0% | 10.3% | 12.1% | 8.7% | 11.4% | 5.8% | 6.8% | 13.6% | 5.6% | |
Malaria infection status was ascertained for all household members for whom written informed consent was provided. Finger-pricked blood samples were analyzed using Giemsa-stained thick smear microscopy. Quality check was conducted on a 10% sample of blood slides at the Muhimbili University of Health and Allied Sciences – MUHAS (a center of excellence in laboratory analysis), indicating a 94.5% specificity rate and 95.7% sensitivity rate [43]. Individuals found to be infected with malaria were treated with appropriate front-line regimens (sulphadoxine-pyrimethamine until August 2006, after which it was replaced with artesunate-amodiaquine). In order to minimize selection bias and achieve full coverage for each house and TCU, up to three attempts were made to enroll subjects.
Information was collected from a total of 48,525 unique individuals and the great majority of them (39,146) were interviewed once. A total of 5,223 participants were followed up twice, 2,349 three times, 1,236 four times, 472 five times, and 99 subjects participated in every round of the survey. Including follow-up data, our sample is thus composed of 64,537 observations, which were drawn from 913 unique TCU and 6,796 households. The small number of subjects who participated in more than two rounds results from two main factors. First, the high mobility observed among urban dwellers; in the second survey round 25.6% of the subjects had moved or were travelling. Second, 13.9% of those interviewed in round 1 declined to participate in the second survey round. Reasons for refusal included pain inflicted by the finger prick, misconceptions about malaria transmission, and the mistrust of the malaria counts provided in the precedent survey round. Sensitization efforts addressed these issues and refusal decreased in subsequent survey rounds.
Rainfall data
Rainfall estimates were obtained from the National Oceanic and Atmospheric climate prediction center. This data source combines modeling of satellite-based infrared data collected each 30-minute and station rainfall data to estimate the quantity of daily precipitation over the African continent, and has a spatial resolution of 8 kilometers [44]. Given the biology of the Anopheles mosquito and of the Plasmodium parasite, the effect of rainfall on malaria transmission is expected to be lagged in time. Previous empirical studies suggested that the effect of rainfall on malaria transmission is lagged by approximately 8 weeks [45]–[47]. For each observation, we therefore calculated total weekly precipitation (cm) and lagged this estimate by 8 weeks.
Statistical analyses
The main outcome for this study is malaria infection status (a binary variable – Table 1) as determined by the Giemsa-stained thick smear. Malaria transmission is most directly related to the density of sporozoites-infected adult anophelines, which are not targeted by the larviciding activities. Therefore, a decline in the prevalence of malaria infection is not expected to be observed until the existing pool of infected mosquitoes dies off, and the overall density of mosquitoes is reduced. Based on observations of entomological indices and malaria incidence, it has been estimated that peaks in vector density are followed by peaks in malaria incidence after approximately 1–2 months [48]. Also, the implementation of larviciding activities requires fine-tuning before CORPs became fully familiar with the routine procedures, which could further lag any potential impacts. Based on programmatic and biological considerations, a lag of five weeks was deemed most appropriate and is consistent with results from a previous larviciding study in urban Cameroon [49].
The effects of the microbial larviciding activities on malaria occurrence were first examined using univariate statistics. Malaria prevalence was calculated for each survey round, stratifying by larviciding intervention status, if applicable. Confidence intervals for malaria prevalence were constructed using 9,999 bootstrapped replicates. Clustering of standard errors was taken into account by defining the sampling unit as the TCU [50].
Bayesian random effects logistic models where used to take into account clustering of observations at the household and TCU levels in multivariable analyses. We assumed that our binary outcome followed a Bernoulli distribution, Yi ∼ Bernoulli(pi), where pi is the probability of an individual harboring malaria parasites, which is itself a function of covariates modeled with a logit link. Our model has the following form:
where pitjk is the probability of individual i at time t living in TCU j and household k to be infected with malaria; β is the coefficient of the larviciding intervention; δ is a vector of coefficients for control variables in vector X (age, sex, sleeping outside of ward in previous weeks, taking antimalarial drug in previous two weeks, individuals treated for malaria in a previous survey round, sleeping under an ITN the night before, living in a house with a complete ceiling, and living in a house with window screens) – in the case of longitudinal observations, many of these variables are time variant; μj is a TCU-level random effect; υk is an household random effect; and εitjk are the residuals. Rainfall was modeled using a smooth function where the spline penalty follows a second-order random walk process (where second-order increments are assumed to be independent with mean of zero and variance σt2). This is appropriate when one wants to model smooth curves with small curvatures [51], [52], which is likely to be the case for the relationship between malaria and rainfall. Finally, the time trend was accounted for with f(.) and modeled as a first order autoregressive process [53]. It was chosen over other type of process based on the Deviance Information Criterion (DIC) [54], which provides information on the model’s fit while penalizing for model complexity.
Potential effect modification of the intervention by other determinants of malaria infection was also investigated for a number of covariates (e.g., age, use of ITN, house proofing, etc.). Variable selection for the final multivariable models was achieved through the consideration of a number of issues: (i) subject-matter knowledge about confounders, (ii) variable exhibiting sufficient variation, and (iii) extent of potential measurement errors.
In order to investigate the robustness of our results to modeling assumptions, we used three additional model specifications by including: (i) individual random effects, (ii) ward fixed effects, and (iii) spatially-structured random effects. We also performed a number of sensitivity analyses. Specifically, we tested for potential spillover effects of the intervention, used different lags for the larviciding intervention and for the rainfall estimates, further covariate adjustments (socio-economic status, educational level, and occupation), and varied the choice of penalty for the semi-parametric time trend (first and second-order random walk). Technical details and results are presented in the Supplemental online material (Text S1).
Models were fitted using Integrated Nested Laplace Approximations (INLA) [55]. A major advantage of INLA is that it calculates posterior marginal distributions in very short computational time as compared to more traditional Markov Chain Monte Carlo (MCMC) approaches. Further, INLA has been shown to yield very high accuracy that is comparable to MCMC [55], [56]. Non-informative priors for the regression parameters and hyperparameters were used (see Text S1 for details). All analyses were performed using the R statistical software [57] and estimation of the marginal posterior distribution of the parameters of interest was performed using the INLA library [58]. Observations with missing data for age (n = 44), place slept in previous two weeks (n = 52), occupation of the household head (n = 134), and education level of the household head (n = 136) were retained in the analysis using the missing indicator method [59].
Ethical considerations
Ethics approval was obtained from the Medical Research Coordination Committee of the National Institute for Medical Research, Ministry of Tanzania (Reference number NIMR/HQ/R.8a/Vol. IX/279 &234). Approval from Harvard School of Public Health Institutional Review Board was also obtained (Protocol # 20323-101). Written informed consent was obtained from all study participants after being provided with information regarding the goal, objectives, risk and benefits of the study. Parents or designated guardians provided signed informed consent on behalf of children under 18 years of age. These procedures were approved by the ethics committees.
Results
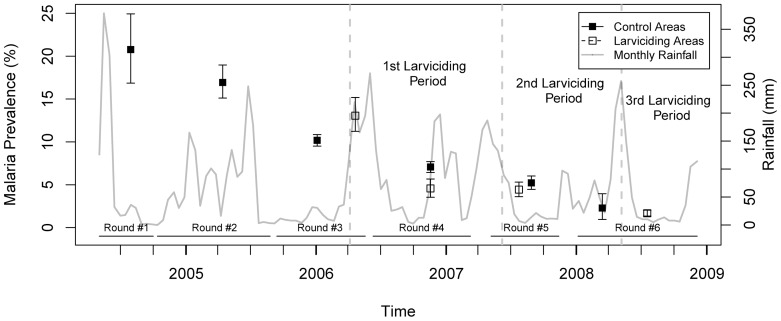
Throughout the study period, malaria prevalence exhibited a considerable decline. Malaria prevalence was highest during the first round of data collection in 2004, with 20.8% prevalence (95% CI: 16.8–24.9%). It decreased to 16.9% (95% CI: 15.1–18.8%) in the second survey round, 10.4% (95% CI: 9.7–11.0%) in the third, 6.6% (95% CI: 6.0–7.1%) in the fourth, 4.8% (95% CI: 4.3–5.4%) in the fifth, and 1.7% (95% CI: 1.4–2.1%) in the last survey round. Stratifying malaria prevalence by survey round and larviciding intervention status, we observed that prevalence was slightly lower in the intervention wards as compared to the control ones, with the notable exception of the third survey round (Figure 4). Note that the start of the larviciding phases did not precisely coincide with the beginning of the survey rounds due to operational issues (as shown in Figure 3, phase 1 of larviciding was launched in March 2006, while the fourth survey round started in June 2006; phase 2 in May 2007; and phase 3 in April 2008). Hence, median dates of interviews in larviciding and control areas do not necessarily coincide, and seasonality in malaria transmission could confound the observed differences in prevalence shown in Figure 4.
Figure 4. Crude prevalence of malaria infection stratified by survey round and larviciding status.
Confidence intervals are based on 9,999 bootstrap replicates and account for clustering at the ten-cell unit level. Monthly rainfall variation is also shown.
For each survey round, the socio-demographic characteristics of study participants and households, stratified by larviciding intervention status, are presented in Table 1. Use of bednet was highly variable through time and seems to be correlated with rainfall and, probably, abundance of nuisance insects. The proportion of interviews performed during the wet seasons also differs between larviciding and control groups. Interestingly, the proportion of individuals reporting having taken anti-malarial drug in the previous two weeks remained relatively constant through time despite the overall decline in malaria prevalence. Finally, we note that socio-economic status seems to be increasing with time, as exhibited by the rising proportion of individuals in the upper quintiles. Overall, individuals in control and larviciding areas do not seem to differ dramatically in their socio-demographic characteristics. Most differences are observed in either the third or sixth survey rounds where the sample sizes in the larviciding and control groups, respectively, are notably smaller.
Taking into account the previously stated limitations of our univariate analysis, we present in Table 2 the results from the random effects logistic regression models that account for clustering of observations within household and TCU. These analyses suggest a significant protective effect of larviciding, with a point estimate for the odds ratio of 0.79 (95% Credible Intervals (CrI): 0.66–0.93) in both univariate and multivariable analyses. When considering potential effect modification of the larviciding intervention by season, we see that larviciding activities achieved maximum programmatic impact during the dry season (Table 3) with an odds ratio of 0.60 (95% CrI: 0.47–0.75). The dry season is defined as the months of January, February, and June through September. The effect of the larviciding intervention also had synergistic effects with other malaria protective measures such as houses with window screens (OR = 0.68; 95% CrI: 0.54–0.85), houses with complete ceiling (OR = 0.66; 95% CrI: 0.53–0.83), and using an ITN the night before (OR = 0.63; 95% CrI: 0.48–0.82). Finally, the effect of the intervention was also heterogeneous among age groups with the larviciding intervention exhibiting a greater protective effect for children under five (OR = 0.61; 95% CrI: 0.46–0.80).
Table 2. Univariate and multivariable effect size estimates of the larviciding intervention on malaria prevalence in Dar es Salaam, 2004–2008 (N = 64,537).
| Univariate | Multivariable | |||
| OR* | 95% CrI† | OR* | 95% CrI† | |
| Larviciding intervention | 0.79 | 0.66–0.93 | 0.79 | 0.66–0.93 |
| Age | ||||
| Under five years of age | - | - | 1.00 | - |
| ≥5 and <15 years of age | - | - | 0.82 | (0.76–0.90) |
| ≥15 and <30 years of age | - | - | 0.67 | (0.61–0.73) |
| ≥30 and <45 years of age | - | - | 0.60 | (0.54–0.66) |
| ≥45 and <60 years of age | - | - | 0.55 | (0.48–0.63) |
| ≥60 years of age | - | - | 0.47 | (0.40–0.56) |
| Male sex | - | - | 1.08 | (1.01–1.15) |
| Slept outside ward (previous 2 weeks) | - | - | 0.90 | (0.77–1.04) |
| Treated for malaria (previous round) | - | - | 0.65 | (0.56–0.75) |
| Took malaria drug (previous 2 weeks) | - | - | 1.02 | (0.90–1.16) |
| ITN used the night before | - | - | 0.93 | (0.86–0.99) |
| House has closed ceiling | - | - | 0.93 | (0.85–1.01) |
| House has window screens | - | - | 0.90 | (0.83–0.98) |
| Trend for time (AR1 § ) | Yes | Yes | ||
| Semi-parametric smooth for rainfall | Yes | Yes | ||
| Random effects (TCU & Household) | Yes | Yes | ||
Statistically significant results are bolded.
OR = Odds Ratio.
CrI = Credible Intervals.
AR1 = First Order Autoregressive Process.
Table 3. Effect modification of the larviciding intervention by selected determinants of malaria prevalence in Dar es Salaam, 2004–2008 (N = 64,537).
| Effect modification of the larviciding intervention by selected determinants of malaria infection (Odds Ratio and 95% Credible Intervals)* | |||
| Control | Larviciding | Effect of Larviciding Within Strata | |
| Wet Season | 1.00 | 1.06 (0.84–1.33) | 1.06 (0.84–1.33) |
| Dry Season § | 0.97 (0.69–1.10) | 0.57 (0.41–0.77) | 0.60 (0.47–0.75) |
| Control | Larviciding | Effect of Larviciding Within Strata | |
| No Screen | 1.00 | 0.84 (0.70–1.02) | 0.84 (0.70–1.02) |
| Window Screens | 0.93 (0.85–1.02) | 0.80 (0.65–0.99) | 0.68 (0.54–0.85) |
| Control | Larviciding | Effect of Larviciding Within Strata | |
| Open Ceiling | 1.00 | 0.84 (0.70–1.01) | 0.84 (0.70–1.01) |
| Complete Ceiling | 0.97 (0.88–1.06) | 0.78 (0.63–0.97) | 0.66 (0.53–0.83) |
| Control | Larviciding | Effect of Larviciding Within Strata | |
| No ITN | 1.00 | 0.83 (0.69–0.99) | 0.83 (0.69–0.99) |
| ITN used | 0.96 (0.88–1.04) | 0.77 (0.61–0.96) | 0.63 (0.48–0.82) |
| Control | Larviciding | Effect of Larviciding Within Strata | |
| Aged ≥5 years | 1.00 | 0.83 (0.69–0.99) | 0.83 (0.69–0.99) |
| <5 years of age | 1.35 (1.23–1.47) | 0.73 (0.56–0.94) | 0.61 (0.46–0.80) |
Statistically significant results are bolded.
All models are adjusted for age, sex, sleeping outside of the ward (previous 2 weeks), being treated for malaria in a previous round, use of malaria drugs (previous 2 weeks), use of ITN, complete ceiling, window screen, precipitation, time trend. Random effects at household and TCU levels are also included.
Dry season is defined as the months of January, February, and June through September.
Model specifications seem to have little bearing on the estimates of the posterior marginal for the larviciding intervention (see Tables S1 and S2 in Text S1). Importantly, including fixed effects at the ward level, which would control for any time-invariant measured or unmeasured confounders of the larviciding-malaria relationship, had little impact on the point estimate of the larviciding intervention (adjusted OR = 0.80; 95% CrI:0.66–0.97).
Finally, our sensitivity analyses (see Table S3 and S4 in Text S1) demonstrated that spillover effects were not biasing our effect size estimate towards the null. As expected, effect size estimates were somewhat sensitive to variation in the assumed lag length between initiation of larviciding activities and malaria transmission but the effect remained statistically significant over lag lengths varying between 28 and 60 days. Results were also robust to changes in other model parameters.
Discussion
This study has shown that a community-based larviciding program, centrally managed by the UMCP, provided significant protection to individuals living in areas covered by the larviciding operations. The strength of association was robust to model specifications and consistently approximated a 21% reduction in the odds of malaria infection. Further, the larviciding intervention achieved maximum effectiveness during the dry season and had synergistic effects with other protective measures such as use of ITN, houses with windows screens, and houses with complete ceilings. In addition, we found no evidence of spillover effects between intervention and control areas.
Our estimated effect size for the larviciding intervention is much lower, but not statistically different, than the one previously reported for the first larviciding period of the UMCP, where the odds ratio of living in areas treated with larvicides and being infected with malaria was estimated to be 0.28 (95% CI: 0.10–0.80) as compared to individuals living in control areas [21]. This can be explained in part by the fact that our study considered all age ranges, while Geissbühler et al [21] restricted their analysis to children under five years of age. While there is no reason to believe that larviciding should be more protective for children than for adults, since the intervention acts at the population level by reducing vector density, children might be more likely to spend evenings and nights at or close to their home, a period of the day when most of malaria transmission occurs. There is thus less potential misclassification of exposure for this age group as compared to adults, who might visit friends or spend time during evenings near high exposure areas not covered by larviciding activities. Indeed, we found that the product term between the larviciding intervention and age was statistically significant. The estimated odds ratio for the larviciding intervention was of 0.61 (95% CrI: 0.46–0.80) for children under five years of age which is closer to the one reported by Geissbühler et al [21] but insufficient to explain this differential. Another reason which could explain this difference in impact is that our analysis covered all three phases of the intervention with a total of 33 months of larviciding activities, while Geissbühler et al [21] analyzed only the first phase, when the intervention was operational in only three wards for 12 months. Analyses over a longer period may be impacted by programmatic fatigue, coupled with the potential impact that other unmeasured and/or unknown interventions could have on the prevalence of malaria infection and overall transmission dynamics (e.g., artemisin-based combination therapy – ACT started to be the first line of treatment in 2007).
Larviciding during the dry season was shown to be more effective at lowering the prevalence of malaria infection than during the rainy season (when the stratified effect was not significant). This result is especially interesting since 49% of malaria cases were sampled during the dry season. Since larval habitats are less numerous and easier to access when rainfall is low, larviciding activities could have been more effective at suppressing larval production due to operational issues. This highlights one of the key aspects of successful larviciding programs: the ability to locate and access all potential breeding habitats in the targeted area. Also, larviciding should not be deployed alone, but in conjunction with other appropriate vector control activities [60]. The fact that we have estimated larviciding to be more effective than ITNs in Dar es Salaam should not be taken at face value, since the effect size estimate for ITNs does not take into account potential community effects that extend to non-users [61], [62], and that the use of ITNs and other protective measures is likely a function of perceived risk by household members. The combination of different vector control strategies is also supported by our findings of significant synergistic effects between larviciding and use of ITNs, window screens, and houses with a complete ceiling.
With renewed impetus for the long-term goal of malaria eradication [63], the need for tailored programs is imperative, including vector control [30]. Vector control programs should not be established as stand-alone entities. Rather, intersectoral collaboration, health system strengthening, and community mobilization are instrumental to vector control program success. Integrated Vector Management (IVM), as endorsed by WHO [31], [64], emphasizes rational decision making processes to efficiently use resources and attain health-based targets [65]. IVM specifically acknowledges that a ‘one size fits all’ strategy for malaria control will be ineffective. Larviciding should be considered as part of an IVM approach in other urban areas of sub-Saharan Africa, if the local malaria ecology warrants its use. Our study provides a number of important lessons regarding the implementation of larval control: (i) breeding habitats can, and should, be mapped at high resolution using low-cost technology [36], (ii) locally relevant entomological information should be collected to inform operational activities, (iii) monitoring and evaluation systems should be implemented to ensure effective and appropriate delivery and fine-tuning of interventions, and (iv) community involvement and sensitization can be beneficial to programmatic activities. Other strategies included in an IVM approach could facilitate the use of larviciding. For example, in Dar es Salaam 33% of Anopheles breeding habitats are found in clogged drains [66]. In this context, the use of environmental management to restore the functionality of drains would result in fewer breeding habitats [43], and therefore reduce the area to be covered with larviciding.
Strengths of this study include its large sample size, longitudinal design, large temporal and spatial extent of larviciding activities that limited potential spillover effects, and availability of reliable baseline information. This study also has some limitations. First, the wards targeted by the UMCP were not randomly allocated to the larviciding intervention. This entails that our effect size estimates for the larviciding intervention could be biased by residual confounding. This is unlikely to be the case as including fixed effects at the ward level, which would control for such time-invariant non-measured confounders, did not impact our results. Second, ACTs were effectively introduced in Dar es Salaam in January 2007. With its gametocidal proprieties, this drug, if used on a large scale, has the potential to significantly reduce the reservoir of malaria in the general population. Although attempts were made at collecting information on ACT use from health facility data, we were not able to assemble reliable temporal information for the targeted 15 wards. Thus, some of the secular decline in the prevalence of malaria infection observed in control areas before the introduction of larviciding may be a result of ACT use (and possibly of other unobserved activities that could potentially impact the risk of malaria transmission).
Our results have important implications for malaria control in sub-Saharan Africa. Specifically, we have provided evidence that a community-based application of microbial larvicides was effective in reducing malaria transmission in urban Dar es Salaam. Microbial larvicides have been shown to be environmentally safe, specific in their action, and highly effective in killing Anopheles larvae under field conditions [67]–[69]. With important projected increases in urban population in sub-Saharan Africa, mosquitoes’ behavioral adaptation to current control strategies, and the already recorded emergence of resistance to pyrethroid insecticides, larval source management, and larviciding in particular, should be given careful consideration by managers of malaria control programs.
Supporting Information
Supplemental online information. Description of results from additional model specifications (Tables S1 and S2), potential spillover effects (Table S3), sensitivity analyses performed (Table S4), and detailed information on the prior distributions used.
(DOC)
Acknowledgments
We acknowledge the team work involved in activities of the UMCP during 2004–2008. Particularly, we thank Gerry F. Killeen, Ulrike Fillinger, Burton Singer, Marcel Tanner, Steve Lindsay, Michael Kiama (in memoriam), and Deo Mtasiwa. We recognize the financial support for the UMCP provided by the Swiss Tropical Institute, the Bill & Melinda Gates Foundation, Valent Biosciences Corporation, USAID (Environmental Health Program, Dar es Salaam Mission and the President’s Malaria Initiative, all administered through Research Triangle International), and the Wellcome Trust. We are deeply thankful to all community members involved during different phases of the UMCP; to municipal, city, and ward officers; to local leaders and to community-owned resource persons; and to all interviewers, nurses, laboratory technicians, and data entry personnel who supported the assembly of the UMCP database. We are particularly thankful to Khadija Kannady, Abdullah Hemed, James Msami, and George Makanyadigo. We thank Francesca Dominici for valuable comments on an earlier version of this paper.
Funding Statement
This research was supported by Award Number R03AI094401-01 (PI MCC) from the National Institute of Allergy and Infectious Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health. MMG was supported by an International Fulbright Science & Technology Award sponsored by the Bureau of Educational and Cultural Affairs of the U.S. Department of State, and a Doctoral Foreign Study Award from the Canadian Institutes of Health Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Keiser J, Singer BH, Utzinger J (2005) Reducing the burden of malaria in different eco-epidemiological settings with environmental management: a systematic review. Lancet Infect Dis 5: 695–708. [DOI] [PubMed] [Google Scholar]
- 2. Shousha AT (1948) Species-eradication: The Eradication of Anopheles gambiae from Upper Egypt, 1942-1945. Bull World Health Organ 1: 309–352. [PMC free article] [PubMed] [Google Scholar]
- 3.Soper F, Wilson D (1943) Anopheles gambiae in Brazil, 1930 to 1940. New York, NY: Rockefeller Foundation. 262 p.
- 4.Watson M (1953) African Highway: The Battle for Health in Central Africa. London, UK: John Murray. 294 p.
- 5. Ross R (1907) An address on the prevention of malaria in British possessions, Egypt, and parts of America. Lancet 2: 879–887. [Google Scholar]
- 6. Derryberry O, Gartrell F (1952) Trends in malaria control program of the Tennessee Valley Authority. American Journal of Tropical Medicine and Hygiene 1: 500–507. [DOI] [PubMed] [Google Scholar]
- 7. Nájera JA, González-Silva M, Alonso PL (2011) Some lessons for the future from the Global Malaria Eradication Programme (1955–1969). PLoS Med 8: e1000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baer F, McGahey C, Wijeyaratne P (1999) Summary of EHP Activities in Kitwe, Zambia, 1997–1999. Kitwe Urban Health Programs. Washington, DC: U.S. Agency for International Development. 48 p.
- 9.Lindsay S, Egwang T, Kabuye F, Mutambo T, Matwale G (2004) Community-Based Environmental Management Program for Malaria Control in Kampala and Jinga, Uganda. Washington, DC: U.S. Agency for International Development. 62 p.
- 10. Castro M, Yamagata Y, Mtasiwa D, Tanner M, Utzinger J, et al. (2004) Integrated urban malaria control: a case study in dar es salaam, Tanzania. Am J Trop Med Hyg 71: 103–117. [PubMed] [Google Scholar]
- 11. Chaki P, Dongus S, Fillinger U, Kelly A, Killeen G (2011) Community-owned resource persons for malaria vector control: enabling factors and challenges in an operational programme in Dar es Salaam, United Republic of Tanzania. Human Resources For Health 9: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chaki P, Govella N, Shoo B, Hemed A, Tanner M, et al. (2009) Achieving high coverage of larval-stage mosquito surveillance: challenges for a community-based mosquito control programme in urban Dar es Salaam, Tanzania. Malaria Journal 8: 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gu W, Utzinger J, Novak RJ (2008) Habitat-based larval interventions: a new perspective for malaria control. Am J Trop Med Hyg 78: 2–6. [PubMed] [Google Scholar]
- 14. Fillinger U, Lindsay SW (2011) Larval source management for malaria control in Africa: myths and reality. Malar J 10: 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Killeen GF, Fillinger U, Kiche I, Gouagna LC, Knols BG (2002) Eradication of Anopheles gambiae from Brazil: lessons for malaria control in Africa? Lancet Infect Dis 2: 618–627. [DOI] [PubMed] [Google Scholar]
- 16. Worrall E, Fillinger U (2011) Large-scale use of mosquito larval source management for malaria control in Africa: a cost analysis. Malar J 10: 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imbahale SS, Mweresa CK, Takken W, Mukabana WR (2011) Development of environmental tools for anopheline larval control. Parasit Vectors 4: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Walker K, Lynch M (2007) Contributions of Anopheles larval control to malaria suppression in tropical Africa: review of achievements and potential. Med Vet Entomol 21: 2–21. [DOI] [PubMed] [Google Scholar]
- 19.WHO (2012) Interim Position Statement - The role of larviciding for malaria control in sub-Saharan Africa. Geneva, Switzerland: World Health Organization - Global Malaria Programme. 21 p.
- 20. Fillinger U, Ndenga B, Githeko A, Lindsay S (2009) Integrated malaria vector control with microbial larvicides and insecticide-treated nets in western Kenya: a controlled trial. Bulletin of the World Health Organization 87: 655–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Geissbuhler Y, Kannady K, Chaki PP, Emidi B, Govella NJ, et al. (2009) Microbial larvicide application by a large-scale, community-based program reduces malaria infection prevalence in urban Dar es Salaam, Tanzania. PLoS One 4: e5107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Majambere S, Pinder M, Fillinger U, Ameh D, Conway D, et al. (2010) Is mosquito larval source management appropriate for reducing malaria in areas of extensive flooding in The Gambia? A cross-over Intervention Trial. American Journal of Tropical Medicine and Hygiene 82: 176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Geissbuhler Y, Chaki P, Emidi B, Govella NJ, Shirima R, et al. (2007) Interdependence of domestic malaria prevention measures and mosquito-human interactions in urban Dar es Salaam, Tanzania. Malar J 6: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Griffin JT, Hollingsworth TD, Okell LC, Churcher TS, White M, et al. (2010) Reducing Plasmodium falciparum malaria transmission in Africa: a model-based evaluation of intervention strategies. PLoS Med 7: e1000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ranson H, N'guessan R, Lines J, Moiroux N, Nkuni Z, et al. (2011) Pyrethroid resistance in African anopheline mosquitoes: what are the implications for malaria control? Trends Parasitol 27: 91–98. [DOI] [PubMed] [Google Scholar]
- 26. Cuamba N, Morgan JC, Irving H, Steven A, Wondji CS (2010) High level of pyrethroid resistance in an Anopheles funestus population of the Chokwe District in Mozambique. PLoS One 5: e11010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morgan JC, Irving H, Okedi LM, Steven A, Wondji CS (2010) Pyrethroid resistance in an Anopheles funestus population from Uganda. PLoS One 5: e11872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Munhenga G, Masendu HT, Brooke BD, Hunt RH, Koekemoer LK (2008) Pyrethroid resistance in the major malaria vector Anopheles arabiensis from Gwave, a malaria-endemic area in Zimbabwe. Malar J 7: 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ferguson HM, Dornhaus A, Beeche A, Borgemeister C, Gottlieb M, et al. (2010) Ecology: a prerequisite for malaria elimination and eradication. PLoS Med 7: e1000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. malERA Consultative Group on Vector Control (2011) A research agenda for malaria eradication: vector control. PLoS Med 8: e1000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO (2004) Global Strategic Framework for Integrated Vector Management. Geneva, Switzerland: World Health Organization. 15 p.
- 32.WHO (2012) Handbook for integrated vector management. Geneva, Switzerland: World Health Organization. 67 p.
- 33.UN-HABITAT (2010) The State of African Cities 2010 - Governance, Inequality and Urban Land Markets. United Nations Settlements Programme. 276 p.
- 34. Keiser J, Utzinger J, Castro CM, Smith TA, Tanner M, et al. (2004) Urbanization in sub-saharan Africa and implication for malaria control. Am J Trop Med Hyg 71: 118–127. [PubMed] [Google Scholar]
- 35. Robert V, Macintyre K, Keating J, Trape JF, Duchemin JB, et al. (2003) Malaria transmission in urban sub-Saharan Africa. Am J Trop Med Hyg 68: 169–176. [PubMed] [Google Scholar]
- 36. Fillinger U, Kannady K, William G, Vanek MJ, Dongus S, et al. (2008) A tool box for operational mosquito larval control: preliminary results and early lessons from the Urban Malaria Control Programme in Dar es Salaam, Tanzania. Malar J 7: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.UN (2007) World Population Prospects: The 2006 Revision and World Urbanization Prospects: The 2007 Revision. Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat.
- 38. Yhdego M, Paul M (1988) Malaria Control in Tanzania. Environment International 14: 479–483. [Google Scholar]
- 39. Dongus S, Nyika D, Kannady K, Mtasiwa D, Mshinda H, et al. (2007) Participatory mapping of target areas to enable operational larval source management to suppress malaria vector mosquitoes in Dar es Salaam, Tanzania. International Journal of Health Geographics 6: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dongus S, Mwakalinga V, Kannady K, Tanner M, Killeen G (2011) Participatory Mapping as a Component of Operational Malaria Vector Control in Tanzania Geospatial Analysis of Environmental Health. In: Maantay JA, McLafferty S, Jensen RR, editors: Springer Netherlands. pp. 321–336.
- 41.Vanek M, Shoo B, Mtasiwa D, Kiama M, Lindsay S, et al. (2006) Community-based surveillance of malaria vector larval habitats: a baseline study in urban Dar es Salaam, Tanzania. Bmc Public Health 6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Filmer D, Pritchett LH (2001) Estimating wealth effects without expenditure data - or tears: an application to educational enrollments in states of India. Demography 38: 115–132. [DOI] [PubMed] [Google Scholar]
- 43. Castro M, Tsuruta A, Kanamori S, Kannady K, Mkude S (2009) Community-based environmental management for malaria control: evidence from a small-scale intervention in Dar es Salaam, Tanzania. Malar J 8: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Xie P, Arkin P (1996) Analyses of global monthly precipitation using gauge observations, satellite estimates, and numerical model predictions. Journal of Climate 9: 840–858. [Google Scholar]
- 45. Krefis AC, Schwarz NG, Krüger A, Fobil J, Nkrumah B, et al. (2011) Modeling the relationship between precipitation and malaria incidence in children from a holoendemic area in Ghana. Am J Trop Med Hyg 84: 285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhou G, Minakawa N, Githeko AK, Yan G (2004) Association between climate variability and malaria epidemics in the East African highlands. Proc Natl Acad Sci U S A 101: 2375–2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Loevinsohn ME (1994) Climatic warming and increased malaria incidence in Rwanda. Lancet 343: 714–718. [DOI] [PubMed] [Google Scholar]
- 48. Kristan M, Abeku TA, Beard J, Okia M, Rapuoda B, et al. (2008) Variations in entomological indices in relation to weather patterns and malaria incidence in East African highlands: implications for epidemic prevention and control. Malar J 7: 231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Barbazan P, Baldet T, Darriet F, Escaffre H, Djoda DH, et al. (1998) Impact of treatments with Bacillus sphaericus on Anopheles populations and the transmission of malaria in Maroua, a large city in a savannah region of Cameroon. J Am Mosq Control Assoc 14: 33–39. [PubMed] [Google Scholar]
- 50. Cameron A, Gelbach J, Miller D (2008) Bootstrap-based improvements for inference with clustered errors. Review of Economics and Statistics 90: 414–427. [Google Scholar]
- 51. Schrodle B, Held L (2011) A primer on disease mapping and ecological regression using INLA. Computational Statistics 26: 241–258. [Google Scholar]
- 52. Natario I, Knorr-Held L (2003) Non-parametric ecological regression and spatial variation. Biometrical Journal 45: 670–688. [Google Scholar]
- 53.Congdon P (2006) Bayesian statistical modelling. Chichester, England ; Hoboken, NJ: John Wiley & Sons. xi, 573 p. p.
- 54. Spiegelhalter DJ, Best NG, Carlin BP, Linde Avd (2002) Bayesian measures of model complexity and fit. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 64: 583. [Google Scholar]
- 55. Rue H, Martino S, Chopin N (2009) Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. Journal of the Royal Statistical Society Series B-Statistical Methodology 71: 319–392. [Google Scholar]
- 56. Beguin J, Martino S, Rue H, Cumming SG (2012) Hierarchical analysis of spatially autocorrelated ecological data using integrated nested Laplace approximation. Methods in Ecology and Evolution 3: 921–929. [Google Scholar]
- 57.R Development Core Team (2012) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing.
- 58.Rue H, Martino S, Lindgren F (2009) INLA: Functions which allow to perform a full Bayesian analysis of structured (geo-)additive models using Integrated Nested Laplace Approximaxion. R Package version 0.0 ed.
- 59.Miettinen OS (1985) Theoretical epidemiology : principles of occurrence research in medicine. New York: Wiley. xxii, 359 p. p.
- 60.WHO (2004) Global Strategic Framework for Integrated Vector Management. Geneva, Switzerland: World Health Organization. 12 p.
- 61. Howard SC, Omumbo J, Nevill C, Some ES, Donnelly CA, et al. (2000) Evidence for a mass community effect of insecticide-treated bednets on the incidence of malaria on the Kenyan coast. Trans R Soc Trop Med Hyg 94: 357–360. [DOI] [PubMed] [Google Scholar]
- 62. Hawley WA, Phillips-Howard PA, ter Kuile FO, Terlouw DJ, Vulule JM, et al. (2003) Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western Kenya. Am J Trop Med Hyg 68: 121–127. [PubMed] [Google Scholar]
- 63. Alonso PL, Brown G, Arevalo-Herrera M, Binka F, Chitnis C, et al. (2011) A research agenda to underpin malaria eradication. PLoS Med 8: e1000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.WHO (2004) Global Strategic Framework for Integrated Vector Management. Geneva, Switzerland: World Health Organization. 14 p.
- 65.WHO (2008) WHO position statement on integrated vector management. Geneva, Switzerland: World Health Organization. 4 p.
- 66. Castro M, Kanamori S, Kannady K, Mkude S, Killeen G, et al. (2010) The importance of drains for the larval development of lymphatic filariasis and malaria vectors in Dar es Salaam, United Republic of Tanzania. PLoS Negl Trop Dis 4: e693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Shililu JI, Tewolde GM, Brantly E, Githure JI, Mbogo CM, et al. (2003) Efficacy of Bacillus thuringiensis israelensis, Bacillus sphaericus and temephos for managing Anopheles larvae in Eritrea. J Am Mosq Control Assoc 19: 251–258. [PubMed] [Google Scholar]
- 68. Majambere S, Lindsay SW, Green C, Kandeh B, Fillinger U (2007) Microbial larvicides for malaria control in The Gambia. Malar J 6: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Fillinger U, Knols BG, Becker N (2003) Efficacy and efficiency of new Bacillus thuringiensis var israelensis and Bacillus sphaericus formulations against Afrotropical anophelines in Western Kenya. Trop Med Int Health 8: 37–47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental online information. Description of results from additional model specifications (Tables S1 and S2), potential spillover effects (Table S3), sensitivity analyses performed (Table S4), and detailed information on the prior distributions used.
(DOC)