Abstract
Background
Health inequities in developing countries are difficult to eradicate because of limited resources. The neglect of adult mortality in Sub-Saharan Africa (SSA) is a particular concern. Advances in data availability, software and analytic methods have created opportunities to address this challenge and tailor interventions to small areas. This study demonstrates how a generic framework can be applied to guide policy interventions to reduce adult mortality in high risk areas. The framework, therefore, incorporates the spatial clustering of adult mortality, estimates the impact of a range of determinants and quantifies the impact of their removal to ensure optimal returns on scarce resources.
Methods
Data from a national cross-sectional survey in 2007 were used to illustrate the use of the generic framework for SSA and elsewhere. Adult mortality proportions were analyzed at four administrative levels and spatial analyses were used to identify areas with significant excess mortality. An ecological approach was then used to assess the relationship between mortality “hotspots” and various determinants. Population attributable fractions were calculated to quantify the reduction in mortality as a result of targeted removal of high-impact determinants.
Results
Overall adult mortality rate was 145 per 10,000. Spatial disaggregation identified a highly non-random pattern and 67 significant high risk local municipalities were identified. The most prominent determinants of adult mortality included HIV antenatal sero-prevalence, low SES and lack of formal marital union status. The removal of the most attributable factors, based on local area prevalence, suggest that overall adult mortality could be potentially reduced by ∼90 deaths per 10,000.
Conclusions
The innovative use of secondary data and advanced epidemiological techniques can be combined in a generic framework to identify and map mortality to the lowest administration level. The identification of high risk mortality determinants allows health authorities to tailor interventions at local level. This approach can be replicated elsewhere.
Introduction
The achievement of the Millenium Development Goals (MDG) in many developing countries has been compromised because of the persistent nature of many health problems combined with limited resources [1]–[2]. Excess adult mortality in Sub Saharan Africa (SSA) has been neglected due to a focus on improving infant and child survival [3]–[4], as well as a lack of data and a failure to exploit available databases for monitoring and evaluating purposes [5]–[7]. Estimates of adult mortality in the region vary depending on which data source was used, the assumptions made and the methodology employed. However, it is evident that adult mortality in some countries of the region are still the highest in the world [8]–[9]. SSA, moreover, is the epicentre of the HIV/AIDS pandemic [10]–[11], maternal mortality remains a problem [12] and the impact of non-communicable disease is expected to increase [11], [13]–[14]. The high level of adult mortality and morbidity in SSA has also impacted negatively on the economy and healthcare resources of the region. In particular, HIV/AIDS has reduced the availability and productivity of working aged adults [14]–[18]. Given the disturbing adult mortality data in the region, as well as its impact on the economies of its countries, the lack of adult mortality research and policy development is surprising.
A standard framework for the identification and analysis of geographical areas of high risk mortality and population attributability of prominent determinants, is an important policy issue [19]. This importance is underlined by the limited healthcare resources of developing countries which often precludes the implementation of population-wide intervention programs in favour of targeted high risk areas or “hotspots” (local areal units with significantly higher than expected mortality) at a regional or local level [20]. Recent advances in data availability, software and analytic methods, have created new opportunities to address this challenge. These advances, moreover, have improved the identification, analysis and mapping of health inequality from national to local level [21]–[24].
This paper develops a generic framework for SSA to identify and assess adult mortality and its associated determinants. Using South African national survey data as an example, the generic framework first identifies the spatial risk of high adult mortality clusters at four levels. The framework then quantifies the relationship between adult mortality and a range of high impact determinants before developing a mortality reduction index to show the effect of the removal of the most attributable factors. This is especially important given the limited resources for healthcare interventions in the region [25]. Finally, the discussion supports the wider application of the proposed generic framework in SSA rather than expanding on the social determinants of adult mortality.
Materials and Methods
Study Area
South Africa is administratively divided into nine secondary regions (provinces) responsible for health service delivery (Figure 1) that are further sub-divided into 52 tertiary regions. At the time of the study these consisted of 46 district municipalities and 6 metropolitan districts (currently South Africa’s provinces are sub-divided into 44 district municipalities and 8 metropolitan districts). These districts are then further disaggregated into 248 quaternary areas (local municipalities which are the lowest administrative unit).
Figure 1. Map of South Africa, with provinces and neighbouring countries.
Data Sources
The data were drawn from the random cross sectional national survey run by Statistics South Africa in 2007. These data included information regarding demographic indicators (such as mortality) and socio-economic data including education, employment, household assets, as well as access to facilities and services [26]. The survey sample covered 274 348 dwelling units across all the provinces and attained a response rate of 93.9% [27]. The South African Statistics Council [28] also found the reported demographic data to be plausible when compared to other censuses.
This secondary data analysis focused on adults aged 15 to 59 years. Mortality was based on interviewee reported mortality of household members in the preceding 12 months. Individual level mortality data were not provided due to confidentiality reasons. Thus, aggregated adult mortality at the smallest available aggregation (quaternary level) was used. Demographic (age, gender and population group), social (marital status, disability, education, household goods) economic activity (employment, income, occupation) and household service (water, sanitation, refuse removal, settlement type) data were extracted. Household level demographic indicators were calculated based on individual characteristics. Additional data, regarding district level antenatal HIV sero-prevalence in 2007, were extracted from the District Health Barometer for 2007/2008 [29]. Mortality data from the vital registration system (available at the provincial level) were also used for validation purposes and cause-of-death fractions.
Statistical Analyses
Identification of significant spatial ‘hotspots’ using difference and equivalence testing
Adult mortality proportions were calculated for each district and local municipality (sub-district) by dividing the observed number of deaths by the total population in a given areal unit. To identify areas in which the mortality proportion was significantly above average, we first constructed the exact 95% confidence intervals (CI) for each proportion using the binomial distribution of the observed number of deaths [30]. Areal unit mortality was considered significantly above average if the lower 95% CI limit (α = 0.025) of the mortality proportion for that district or local municipality was above the overall national average [31]. Standardised mortality ratios (SMRs) were also estimated by dividing observed deaths by the expected number of deaths if the national average mortality incidence applied to that areal unit’s total adult population.
Potential determinants of identified spatial hotspots
This component of the analysis compared significantly high risk local municipalities (unit of analysis) with the remaining local municipalities with regards to significant differences in the breakdown of various individual, household and community or local municipality level determinants. Given the aggregated nature of the mortality data, an ecological modelling approach was employed.
Various multilevel determinants assessed included: age, gender, education, population group, marital status, employment status and income, household services, and antenatal HIV sero-prevalence. The outcome was defined at the individual level and whether they resided in one of the identified local municipality mortality hotspots. The ecological relationship between adult mortality hotspots (dichotomous) and various determinants was assessed using preliminary bivariate associations, clustering on the unit of analysis (quaternary level) to correctly adjust the standard errors and not overestimate significance. Covariates significant at the 10% level were then incorporated into a multivariable model. The multivariable model is formulated as follows with Yij being a dichotomous outcome classification (1 = local municipality hotspot, 0 = non-hotspot) for individual i in local municipality j:
where x 1ij,…,xkij represents the various covariates, α 1 is the constant (or intercept) and βk are the regression coefficients. We employed a Poisson modelling approach (with log link) for binary (dichotomous) outcome data [32] to estimate risk ratios (RR) directly as odds ratios (OR) could overestimate coefficient “risk” given a prevalent outcome. Use of ordinary Poisson regression with binary data may however result in standard errors that are too conservative (i.e. overestimate significance) due to under-dispersion from fitting a Poisson regression model to binomial data [32]–[33]. However, one can use a Poisson approach with robust standard errors to give correct standard errors (deals with variance overestimation) [34]. We therefore also used robust error variance in our model and again clustered on the unit of analysis (quaternary level) to correctly adjust the standard errors and not overestimate significance.
Population Attributable Fractions (PAF)
We also assessed the degree to which small area unit exposure (prevalence) to a particular variable (e.g. access to water and sanitation) impacted on mortality. This could provide an indication for policy makers about what intervention(s) to prioritise and the potential impact of removing such an exposure. We linked determinant coefficient estimates with the actual prevalence of exposure to those determinants within the lowest level areal units. The following standard formula for calculating an attributable fraction for each determinant was based on its prevalence of exposure (pe) in a given areal unit, as well as the exponentiated model coefficient (risk ratio[RR]) for that determinant:
Software
Analysis was carried out in STATA 12.0 SE and WinBUGS. Maps were constructed in MapInfo Professional.
Results
Primary Level (National)
The study sample comprised 640 761 adults aged 15–59 with a mean age of 32.6 years (std.dev. 12.4). The overall adult mortality proportion was approximately 145.2 deaths per 10 000 population (95% CI: 142.3, 148.2), with males having a significantly (p-value<0.001) higher mortality proportion of 155.1 (95% CI: 150.8, 159.6) compared to females at 135.9 (95% CI: 132.0, 140.0) per 10 000 population respectively.
Secondary Level (Province)
Secondary level adult mortality differs significantly across South Africa’s nine provinces (Figure 2a). Two neighbouring provinces, namely, Kwazulu-Natal and the Eastern Cape have significantly higher adult mortality compared to the national average. Conversely, the Western Cape and Gauteng displayed much lower levels. The top five broad causes of deaths among adults aged 15to59 years (based on vital registration estimates available at provincial or national level only) by province are presented in Table 1. The leading cause of death among adults in all provinces was attributed to infectious causes (largely HIV/TB). The remaining four of the top five cause of death by province were generally (with minor variations in ranking) attributed to external, diseases of the respiratory system, unknown (R00-R99) and diseases of the circulatory system. Deaths attributed due to infectious causes strongly and significantly correlate (Pearson correlation coefficient [ρ] = 0.841, p-value<0.01) with provincial level estimates of all-cause adult mortality based on survey estimates (Figure 2a,b). Western Cape was the only province where neoplasm (cancer) related mortality appeared in the top five ranking (∼12% of adult deaths and ranked 3rd).
Figure 2. a) Descending all-cause adult mortality proportions (survey) and b) cause-specific fractions attributed to infectious causes (vital registration) at the secondary level (province), South Africa, 2007.
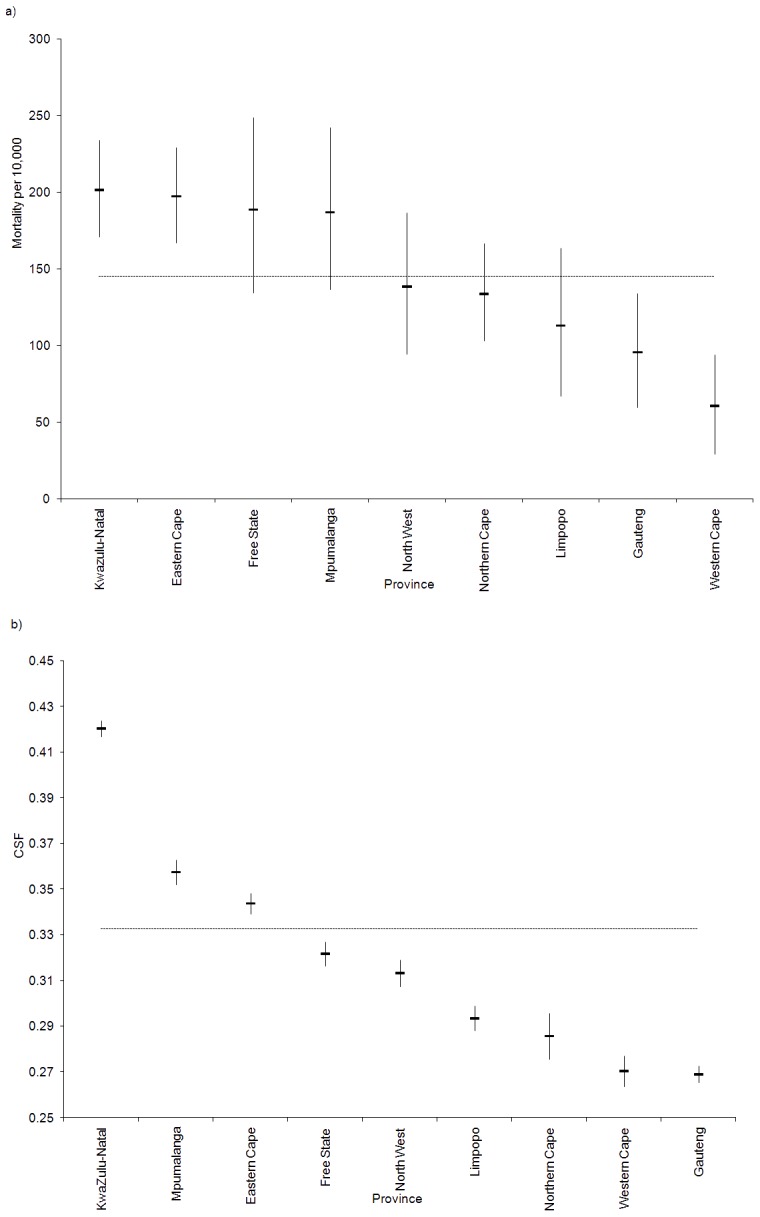
[CSF = cause specific fraction].
Table 1. Top five broad causes of death by province, South Africa, 2007.
| Province | Cause | Cause specificdeath count | Totaldeaths | CSF |
| Eastern Cape | Certain infectious and parasitic diseases (A00–B99) | 14505 | 42190 | 34.38% |
| External (V01–Y98) | 5536 | 42190 | 13.12% | |
| Diseases of the respiratory system (J00–J99) | 5060 | 42190 | 11.99% | |
| Ill defined (R00–R99) | 4995 | 42190 | 11.84% | |
| Diseases of the circulatory system (I00–I99) | 3257 | 42190 | 7.72% | |
| Free State | Certain infectious and parasitic diseases (A00–B99) | 9982 | 31031 | 32.17% |
| Diseases of the respiratory system (J00–J99) | 6001 | 31031 | 19.34% | |
| Ill defined (R00–R99) | 3307 | 31031 | 10.66% | |
| External (V01–Y98) | 2538 | 31031 | 8.18% | |
| Diseases of the circulatory system (I00–I99) | 2511 | 31031 | 8.09% | |
| Gauteng | Certain infectious and parasitic diseases (A00–B99) | 15149 | 56330 | 26.89% |
| External (V01–Y98) | 8852 | 56330 | 15.71% | |
| Diseases of the respiratory system (J00–J99) | 7722 | 56330 | 13.71% | |
| Ill defined (R00–R99) | 7569 | 56330 | 13.44% | |
| Diseases of the circulatory system (I00–I99) | 5112 | 56330 | 9.08% | |
| KwaZulu-Natal | Certain infectious and parasitic diseases (A00–B99) | 32921 | 78323 | 42.03% |
| Ill defined (R00–R99) | 8709 | 78323 | 11.12% | |
| External (V01–Y98) | 8697 | 78323 | 11.10% | |
| Diseases of the respiratory system (J00–J99) | 8625 | 78323 | 11.01% | |
| Diseases of the circulatory system (I00–I99) | 5519 | 78323 | 7.05% | |
| Limpopo | Certain infectious and parasitic diseases (A00–B99) | 7910 | 26947 | 29.35% |
| Diseases of the respiratory system (J00–J99) | 4542 | 26947 | 16.86% | |
| Ill defined (R00–R99) | 4151 | 26947 | 15.40% | |
| External causes of morbidity and mortality (V01–Y98) | 2613 | 26947 | 9.70% | |
| Diseases of the circulatory system (I00–I99) | 1980 | 26947 | 7.35% | |
| Mpumalanga | Certain infectious and parasitic diseases (A00–B99) | 10695 | 29918 | 35.75% |
| Diseases of the respiratory system (J00–J99) | 5198 | 29918 | 17.37% | |
| External causes of morbidity and mortality (V01–Y98) | 2877 | 29918 | 9.62% | |
| Diseases of the circulatory system (I00–I99) | 2332 | 29918 | 7.79% | |
| Diseases of the blood and immunity disorders (D50–D89) | 2103 | 29918 | 7.03% | |
| North West | Certain infectious and parasitic diseases (A00–B99) | 7835 | 25009 | 31.33% |
| Diseases of the respiratory system (J00–J99) | 4257 | 25009 | 17.02% | |
| Ill defined (R00–R99) | 2873 | 25009 | 11.49% | |
| External causes of morbidity and mortality (V01–Y98) | 2741 | 25009 | 10.96% | |
| Diseases of the circulatory system (I00–I99) | 2540 | 25009 | 10.16% | |
| Northern Cape | Certain infectious and parasitic diseases (A00–B99) | 2217 | 7760 | 28.57% |
| Diseases of the respiratory system (J00–J99) | 1126 | 7760 | 14.51% | |
| External causes of morbidity and mortality (V01–Y98) | 994 | 7760 | 12.81% | |
| Ill defined (R00–R99) | 980 | 7760 | 12.63% | |
| Diseases of the circulatory system (I00–I99) | 683 | 7760 | 8.80% | |
| Western Cape | Certain infectious and parasitic diseases (A00–B99) | 4722 | 17466 | 27.04% |
| External causes of morbidity and mortality (V01–Y98) | 4012 | 17466 | 22.97% | |
| Neoplasm’s (C00–D48) | 2128 | 17466 | 12.18% | |
| Diseases of the circulatorysystem (I00–I99) | 1977 | 17466 | 11.32% | |
| Diseases of the respiratorysystem (J00–J99) | 1190 | 17466 | 6.81% |
Tertiary Level (District)
Tertiary level adult mortality differs significantly different across South Africa’s 52 districts (Figure 3) in line with the levels reflected in the nine provinces. Particularly, 16 districts in Kwazulu-Natal and the Eastern Cape (mostly) show the highest levels while 12 districts in the Western Cape and Gauteng generally have the lowest levels.
Figure 3. Descending district level adult mortality proportions with 95% confidence intervals and highlighting significantly high or low tertiary (districts) areas, South Africa, 2007 (KZN Kwazulu-Natal: EC: Eastern Cape; MPU: Mpumalanga; FS: Free State; NW: North West; NC: Northern Cape; LP: Limpopo; G: Gauteng; WC: Western Cape).
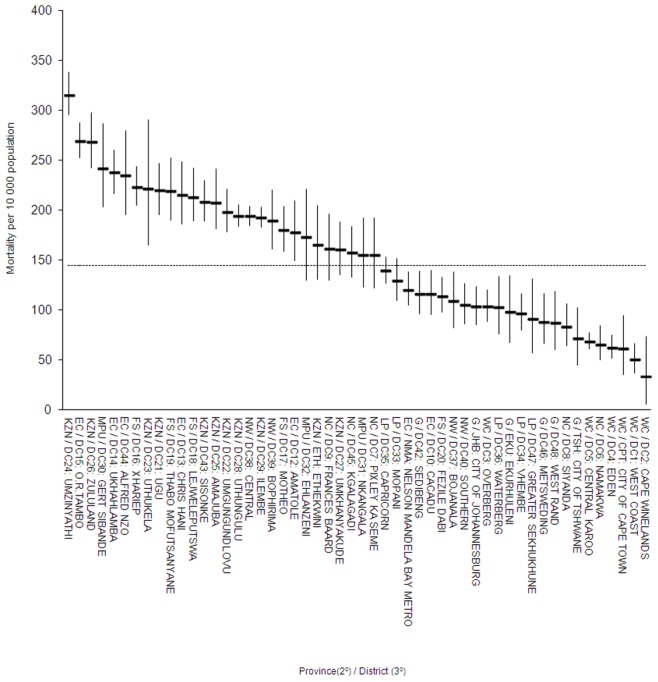
Dashed line represents the national average.
Quaternary Level (Local Municipality)
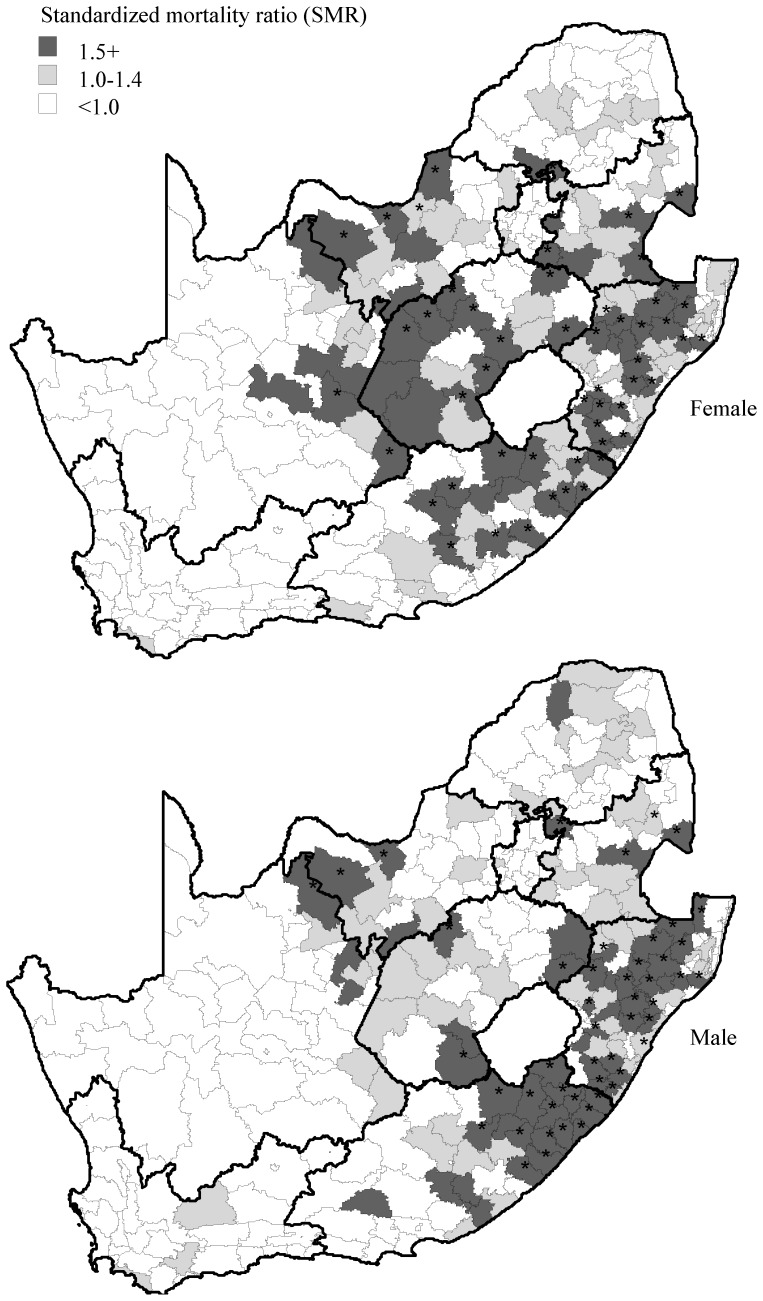
A total of 67 mortality “hotspots” were identified in South Africa’s 248 local municipalities. Further analysis by gender (Figure 4) shows the biggest clusters of adult mortality for both males and females in Kwazulu-Natal and the Eastern Cape. Conversely, the Western Cape and Gauteng recorded none. A highly significant (p-value<0.01) level of correlation (ρ = 0.65) was observed between female and male adult mortality. A strong cluster of female mortality was observed in seven local municipalities in the Free State that also displayed a significantly higher risk of pregnancy related mortality based on vital registration data (259 per 100,000) than all the other provinces except for the Eastern Cape.
Figure 4. Adult mortality risk by gender at the quaternary (local municipality) level, South Africa, 2007.
Districts with significant excess risk (p<0.05) are highlighted (*).
Common Determinants and their Impact on Mortality in Quaternary Level “Hotspots” based on an Ecological Approach
A comparison of the distribution of potential determinants, for high risk versus remaining local municipalities, indicated significant differences for a range of individual and household characteristics (Table 2). High risk local municipalities exhibited significant individual level differences including a lower age, a higher proportion of females and no income and less stable marital patterns. Differences in education were only marginally significant (p-value = 0.128). At household level, high risk local municipalities showed a higher proportion of households with no annual income, a higher mean number of household occupants, lower asset status, lower levels of formal housing and less access to basic household services. Death rates during pregnancy were also markedly elevated in the high risk local municipalities. As antenatal HIV sero-prevalence data were not available at local municipality level, data at tertiary level were used to show that a strong degree of correlation was displayed between adult mortality rates and antenatal HIV sero-prevalence (ρ = 0.48, p-value<0.01).
Table 2. Bivariate multilevel determinants for high risk adult mortality areas using an ecological framework, South Africa, 2007.
| High risk local municipalities | Remaining local municipalities | ||||
| Factors | N (168 774) | (95% CI) | N (471 983) | (95% CI) | P-value i |
| Individual characteristics | |||||
| Mean age | 168 774 | 26.80 (26.72,26.87) | 471 983 | 29.00 (28.95,29.04) | <0.001 |
| Percentage female | 168 774 | 53.14 (52.97,53.32) | 471 983 | 51.29 (51.17,51.40) | <0.001 |
| Percentage African | 168 774 | 89.60 (89.49,89.70) | 471 983 | 72.00 (71.90,72.10) | 0.010 |
| Education | 155 010 | 422 296 | 0.128 | ||
| Percentage with no education | 11.22 (11.09,11.35) | 9.20 (9.12,9.27) | |||
| Percentage with primary level | 40.57 (40.38,40.77) | 34.23 (34.11,34.35) | |||
| Percentage with secondary level | 46.69 (46.49,46.89) | 53.72 (53.60,53.85) | |||
| Percentage with tertiary level | 1.52 (1.47,1.57) | 2.85 (2.81,2.89) | |||
| Marital status | 155 010 | 422 296 | <0.001 | ||
| Percentage union (non-poly) | 22.15 (22.00,22.31) | 29.29 (29.18,29.40) | |||
| Percentage union (poly) | 0.055 (0.046,0.064) | 0.046 (0.041,0.051) | |||
| Percentage never married | 71.43 (71.26,71.60) | 64.73 (64.62,64.85) | |||
| Percentage widower/widow | 5.23(5.14,5.31) | 4.02 (3.98,4.07) | |||
| Percentage with serious disability | 155 010 | 2.97 (2.90,3.03) | 422 296 | 2.27 (2.24,2.31) | 0.006 |
| Percentage with no monthly income | 168 774 | 45.86 (45.68,46.03) | 471 983 | 41.23 (41.12,41.35) | <0.001 |
| Household characteristics | |||||
| Mean occupants | 168 774 | 3.50 (3.48,3.52) | 471 983 | 2.88 (2.87,2.89) | <0.001 |
| Percentage living in a modern dwelling | 168 774 | 41.47 (41.14,41.80) | 471 983 | 50.58 (50.39,50.77) | 0.002 |
| Mean absolute asset count | 153 722 | 2.94 (2.93,2.96) | 418 764 | 3.58 (3.57,3.59) | 0.017 |
| Services | 168 774 | 471 983 | |||
| Percentage with no water service provider | 25.59 (25.29,25.88) | 10.15 (10.03,10.26) | 0.002 | ||
| Percentage with no toilet facilities | 12.84 (12.61.13.06) | 5.23 (5.15,5.32) | 0.003 | ||
| Percentage with no refuse removal | 8.63 (8.45.8.84) | 4.69 (4.60,4.77) | 0.013 | ||
| Percentage with none of the above | 2.62 (2.5.2.73) | 0.66 (0.63,0.69) | 0.001 | ||
| Percentage with no annual income | 168 774 | 6.97 (6.80,7.15) | 471 983 | 5.45 (5.36,5.54) | 0.018 |
| Local municipality deaths in pregnancy per 100 000 live births | 168 774 | 240.54 (173.68,307.41) | 471 983 | 54.35 (35.52,73.19) | <0.001 |
| District antenatal HIV sero-prevalence (%) | 168 774 | 31.67 (30.10,33.24) | 471 983 | 24.46 (23.01,25.90) | <0.001 |
Robust logistic regression for categorical variables and linear regression for comparison of means were employed. Note these formulations were used in place of standard χ2 and t- tests respectively to allow for clustering on the unit of analysis (quaternary level) and thus correctly adjust the standard errors (robust) and not erroneously overestimate significance.
Further analysis illustrates the multivariable adjusted association of selected identified determinants (Table 3). Not being in a formal marital union, low socio-economic status (SES), lack of basic household services and high district antenatal HIV sero-prevalence (> = 30%) were significantly more frequent among individuals in the high risk areal units based on the bivariate analysis. Not being in a formal union, lack of basic household services and antenatal HIV sero-prevalence remained significant following multivariable adjustment. HIV was the most attributable factor followed by not being in a formal union and lastly low SES.
Table 3. Example of a targetable framework of modifiable determinants for high risk adult mortality areas using a multivariable Poisson ecological approach and including population attributable fractions, South Africa, 2007.
| Factors | Unadjusted RR(95% CI) | Adjusted RR(95% CI) | Prevalence ofexposure | PAFi(95% CI) |
| Individual: Male gender | 1.13 (1.07,1.19) | 1.13 (1.07,1.19) | 0.52 | 0.06 (0.04,0.09) |
| Individual: Not in a formal unionii | 1.28 (1.16,1.41) | 1.40 (1.26,1.56) | 0.62 | 0.20 (0.14,0.26) |
| Individual/Household: Low socio-economic statusiii | 1.43 (0.97,2.12) | 1.70 (1.15,2.51) | 0.39 | 0.21 (0.06,0.37) |
| Household: No basic household serviceiv | 2.05 (1.27,3.29) | 3.19 (1.59,6.39) | 0.01 | 0.03 (0.01,0.07) |
| Local municipality: metropolitan area | 0.56 (0.06,5.07) | – | – | – |
| District: Antenatal HIV sero-prevalence > = 30 percent | 2.63 (1.28,5.42) | 3.98 (1.38,11.45) | 0.42 | 0.56 (0.14,0.81) |
population attributable fraction.
never married, separated, divorced or widowed.
based on individual level education status, monthly income and household assets (e.g. fridge, radio etc).
no water service, sanitation and refuse disposal.
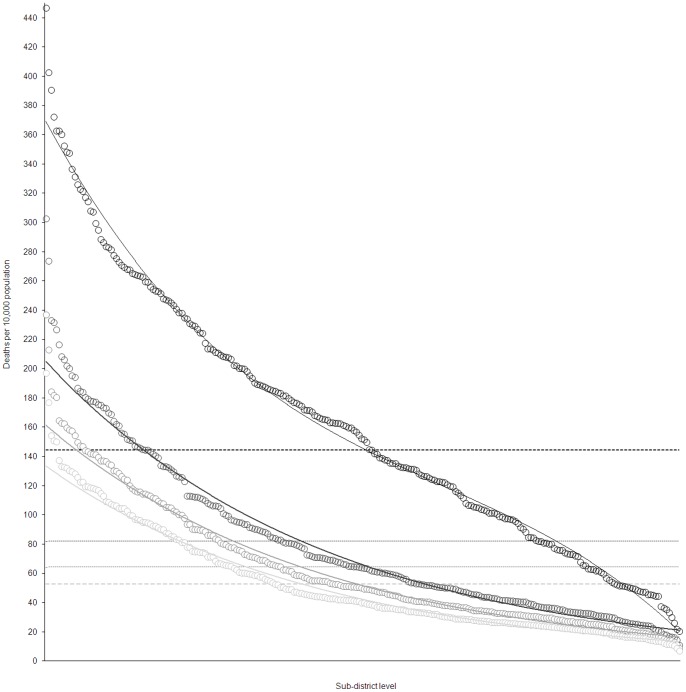
The Removal of Attributable Factors
Antenatal HIV sero-prevalence was the most attributable factor in the high risk quaternary (local municipality) areas with the highest PAF in 37 of the 67 (55%) high risk quaternary areas. For the remaining high risk areas, low SES appeared to be the other most attributable (28 local municipalities or 42%). Low SES ranked as the second most attributable factor in the high risk municipalities (34 local municipalities or 51%) followed by lack of formal union (30 municipalities or 45%). Lack of formal union status and male gender appeared to be the third most attributable ranked factors (34 and 25 local municipalities or 51 and 37% respectively). Results suggest that primary level attributable factors at local municipality level account for approximately 44% (95% CI: 42–48%) of adult deaths. Secondary attributable factors appeared to account for 21% (95% CI: 20–22%). The impact of removing these determinants, based on the prevalence of the primary and secondary most attributable factors in the individual quaternary units, is illustrated in Figure 5. If the most attributable in selected quaternary units are removed, a reduction in overall mortality from the observed 145 to 82 deaths per 10,000 is predicted. If we also remove the second and third most attributable risk factors, the overall mortality level potentially reduces to ∼53 deaths per 10,000 i.e. a projected net total reduction of ∼92 deaths per 10,000 population. Notably we observe a stabilisation of the lowest unit mortality disparity as high risk determinants are removed.
Figure 5. Mortality proportion by quaternary unit: observed and projections based on attributable factor removal based on quaternary unit level prevalence of exposure, South Africa, 2007.
Local municipalities are ordered from highest to lowest mortality: black curve represents the observed mortality; dark grey curve represents adjusted mortality following removal of the most attributable local municipality factors, grey curve following removal of the secondary most attributable factors, light grey line following removal of the tertiary most attributable factors. Overall average reductions are displayed using horizontal dash lines of the same colour.
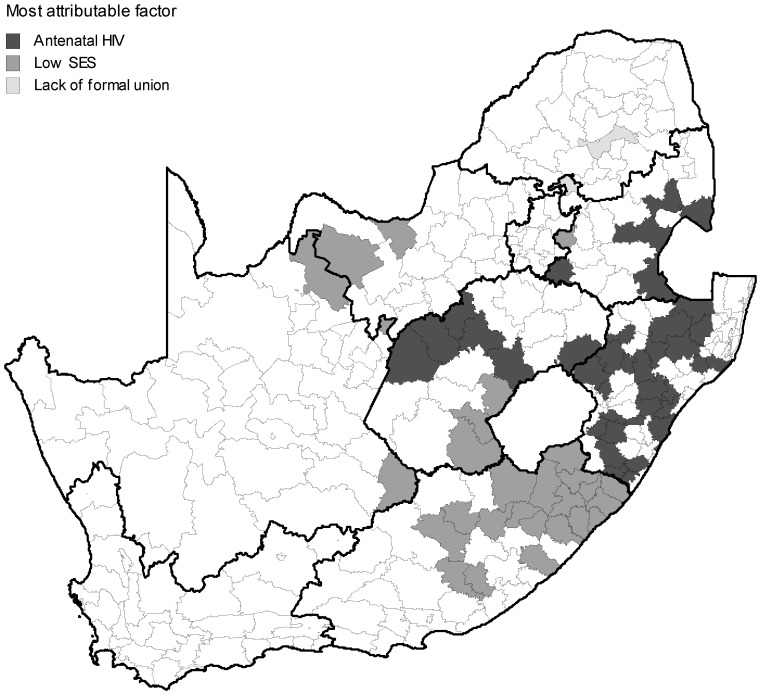
A “policy maker” map is developed showing the distribution of the most attributable risk factors in the high risk local municipalities (Figure 6). Findings suggest that HIV is the more prominent factor in Kwazulu-Natal and Free State while low SES appears to feature more strongly in the Eastern Cape. This could easily be extended to the secondary and tertiary most attributable factors.
Figure 6. Distribution of primary attributable factors in significant high risk adult mortality local municipalities, South Africa, 2007.
Provincial boundaries are shown in bold.
Discussion
Usefulness of the Proposed Framework and Applicability in Other Settings
The integration of spatial disparities of mortality, and the estimation of modifiable determinants using secondary data to most effectively guide resources at sub-national levels, has received little attention despite its prominence as a policy issue [19]. This framework extends the use of prediction models to estimate mortality at a sub-national level in a developing country context [35]. The proposed framework is also easily adaptable to other settings and could also be used for mortality in other age groups, especially for example children <5 years.
The primary purpose of the study was to present a reusable generic framework that could be used in the SSA setting. To illustrate the framework we employed common determinants only to illustrate the properties of the proposed framework rather than explore the detailed causal relationships between adult mortality and related determinants. This study, therefore, does not present a thorough conceptual framework to assess adult mortality nor does it attempt to discuss the identified adult mortality determinants and related policy implications.
Disaggregating Adult Mortality and Identification of Hotspots
The national (primary) adult mortality rate in South Africa is consistent with SSA, largely due to the general impact of the HIV/AIDS pandemic in the region [6] although South Africa has the highest HIV/AIDS infected population in the world with 5.5 million infected individuals [36]. The estimated adult mortality rate of 145 per 10,000, based on the survey, was slightly higher than those based on “comprehensive” vital registration estimates (120 per 10,000). The proportionally higher mortality rates of males is consistent within the SSA although the female mortality in the region appears to be increasing sharply [4]. This increasing level of maternal mortality is reflected in our data and has been associated with the HIV/AIDS pandemic, poverty, a lack of maternal education and poor health facilities in many rural areas [12]. A stronger concentration of significant higher risk local municipality areas for females, compared to males, is also illustrated in one province (Free State). National vital registration data also suggest that this province has the highest level of pregnancy related mortality.
The adult mortality results delivered by our generic framework are well supported by other studies in South Africa that show significant differences across its nine provinces [37]–[38]. Interestingly, a distribution of adult mortality at provincial level as a result of communicable disease only, shows an identical pattern of differences across the nine provinces illustrating the continuing influence of the HIV/AIDS pandemic on overall mortality levels. In particular, Kwazulu-Natal and the Eastern Cape, show markedly higher levels of adult mortality than the Western Cape and Gauteng [38].
Adult mortality in South Africa’s 52 districts (tertiary) shows a further level of disaggregation that is consistent with the distribution of adult mortality at regional (provincial level). Adult mortality in certain districts in Kwazulu-Natal and the Eastern Cape is in excess of 300 deaths per 10,000 whilst it is less than 50 in some districts of the Western Cape. Finally, we disaggregated adult mortality to the lowest administrative level (quaternary) mortality to identify 67 high risk local municipality (quaternary) areas. These results are consistent with other mortality studies that reflect high levels of adult mortality at local municipality level in Kwazulu-Natal, the Eastern Cape, the Free State and Mpumalanga [38].
Modifiable Determinants of Mortality and Impact of Removal
In order to demonstrate the use of the generic framework, we used a range of well discussed determinants to illustrate attributable factors influencing adult mortality in the region. Population attributable fractions (PAF) for specific predictors are useful to help guide policymakers in planning public health interventions [39]–[40]. Our model, therefore, combines a spatial analysis and high impact determinants to examine the association of individual, household and local municipality (“community”) characteristics on adult mortality hotspots by using an ecological type design. A recent study using demographic and health surveys (DHS) data from 20 countries in sub-Saharan Africa has shown that local context independently affects the mortality of residents, in addition to individual and household level determinants [41]. Our study confirms the enduring importance of contextual higher level factors (e.g. HIV, low SES) as important determinants of adult health and mortality in the region. The continuing impact of the HIV/AIDS epidemic on adult mortality has been documented elsewhere, for example [42]. In further support of the generic framework, other potentially high impact determinants can be evaluated for policy development purposes. A generic mortality framework for the SSA region appears feasible and can be readily adapted to other age-groups and related outcomes.
The Removal of Attributable Factors at a Population Level
The proposed framework demonstrates the impact of some common determinants of mortality in South Africa including a lack of basic services, low education, age, income, gender, marital status and HIV sero-prevalence [43]. The results, therefore, show that the proposed framework can effectively target “hotspots” at the lowest areal level, as well as identify possible association based on exposure prevalence within these units. A PAF estimates the proportion of a given outcome (in this case mortality) in a given population that would “theoretically” not have occurred if none of the individuals had been exposed to a given risk factor. The proposed intervention is thus not at the traditional individual (or “downstream”) level but rather at a societal or population level. Whether the full theoretical population level gain can be achieved in practice is difficult and would require large scale support and policy change at a governmental level to effect population level reductions [44]–[45]. Furthermore distal determinants of health (for example national, political, and socio-cultural factors) indirectly influence health by acting on the more proximal factors [46]. Certain factors used in this study could potentially be more distal in nature rather than directly modifiable proximal causal factors. Health policies aimed at preventable factors (i.e. modifiable by public health) should play a key role in the overall assessment of health systems [46]. Utilizing more directly “modifiable” proximal risk factors in the proposed framework would also be a suggested approach in future policy related applications. The possible impact of confounding on coefficient estimates and related overestimation of the associated PAF cannot also be discounted and is discussed further in the limitations section below. The acuteness of geographical location, as well as the range of mortality determinants, illustrate the need to integrate healthcare interventions with other programs like rural development and education [17]. By targeting the top two most attributable determinants in this empirical example (local HIV, low SES), the framework demonstrates the potential to “theoretically” reduce adult mortality levels from 145 to 53 deaths per 10,000 population which is more in line with levels in more developed settings [4]. This approach has a definite application in other settings and for other outcomes in SSA and can assist policy makers to more effectively guide resources at sub-national levels to reduce overall national mortality in line with MDGs. By selective targeting of the most attributable determinants in high risk areas (e.g. Figure 6), there is the potential to reduce overall national mortality levels to those in line with more developed settings.
Data Exploitation in SSA
The use of spatial mortality risk maps at a local level is especially important in SSA due to a limitation in national health care budgets, as well as donor funds [36]. The innovative use of databases in the region, like the DHS combined with national and survey data, offer much potential to improve our knowledge of adult mortality in the region [6]. The use of spatial analysis can also be used to map high risk mortality at local level in order to target interventions in a country with limited resources [47]. Death registration data, however, needs to be improved in the SSA to pinpoint differential interventions for cause-specific outcomes, as well as show changing trends of lifestyle and chronic disease types due to economic growth and population ageing in the region [48].
Certain limitations and potential systematic errors were identified by Statistics SA and the South African Statistical Council when reviewing the survey data [27]. This secondary data analysis is limited by the data that were included in the primary community survey. The consistency of our findings with other national estimates would suggest that our findings are fairly reliable and valid. Given the ecological (aggregated) nature of the data, caution should be taken with interpretation of the direct causal inferences found in our bivariate and multivariable analysis. The data were extracted down to the smallest administrative areal unit available (namely local municipality) which should reduce the ecological effect. For PAF estimation if one or more factors act as confounders between exposure and health outcome, this may lead to biased crude PAF estimates and there is a need for adjustment when estimating the PAF [49]. Multivariable models allow taking into account confounding factors [50] and the model needs to be as complete as possible. However, even when using adjusted relative risk estimates, PAF estimates can be biased if there are unaccounted confounding factors leadings to overestimation of PAF [51].
Funding Statement
The authors have no support or funding to report.
References
- 1. Feachem RG (2000) Poverty and inequity: a proper focus for the new century. Bull World Health Organ 78: 1–2. [PMC free article] [PubMed] [Google Scholar]
- 2. Gupta N, Zurn P, Diallo K, Dal Poz MR (2003) Uses of population census data for monitoring geographical imbalance in the health workforce: snapshots from three developing countries. Int J Equity Health 2: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murray CJL, Feachem RGA (1990) Adult mortality in developing countries. Transactions of the Royal Society of Tropical Medicine and Hygiene 84: 1–2. [DOI] [PubMed] [Google Scholar]
- 4. Rajaratnam JK, Marcus JR, Levin-Rector A, Chalupka AN, Wang H, et al. (2010) Worldwide mortality in men and women aged 15–59 years from 1970 to 2010: a systematic analysis. The Lancet 375: 1704–1720. [DOI] [PubMed] [Google Scholar]
- 5. Kaufman J, Asuzu M, Rotimi C, Johnson O, Owoaje E, et al. (1997) The absence of adult mortality data for sub-Saharan Africa: a practical solution. Bull World Health Organ 75: 389–395. [PMC free article] [PubMed] [Google Scholar]
- 6. Obermeyer Z, Rajaratnam JK, Park CH, Gakidou E, Hogan MC, et al. (2010) Measuring adult mortality using sibling survival: a new analytical method and new results for 44 countries, 1974–2006. PLoS medicine 7: e1000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Adjuik M, Smith T, Clark S, Todd J, Garrib A, et al. (2006) Cause-specific mortality rates in sub-Saharan Africa and Bangladesh. Bulletin of the World Health Organization 84: 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lopez AD, Ahmad OB, Guillot M, Ferguson BD, Salomon JA, et al.. (2002) World mortality in 2000: life tables for 191 countries: World Health Organization.
- 9.Bradshaw D, Timæus IM (2006) Chapter 4 Levels and trends of adult mortality in Disease and mortality in sub-Saharan Africa; Jamison DT, editor: World Bank, Washington (DC). [PubMed]
- 10. Murray CJL, Lopez AD (1997) Mortality by cause for eight regions of the world: Global Burden of Disease Study. The Lancet 349: 1269–1276. [DOI] [PubMed] [Google Scholar]
- 11. Murray CJLLAD (1997) Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Stu. Lancet 349: 1498. [DOI] [PubMed] [Google Scholar]
- 12. Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, et al. (2010) Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. The Lancet 375: 1609–1623. [DOI] [PubMed] [Google Scholar]
- 13. Preston S, Nelson V (1974) Structure and change in causes of death: an international summary. Population Studies 28: 19–51. [DOI] [PubMed] [Google Scholar]
- 14.WHO (2008) Indicator definitions and metadata. WHO Statistical Information - System - WHOSIS 2008; Geneva.
- 15.Feachem R, Philips M, Bulatao R (1992) Introducing adult health. In: The health of adults in the developing world. Feachem, R, Kjellstrom, T, Murray, C, Over, M, Phillips, M (eds). New York: Oxford University Press.
- 16. Schatz E, Ogenmefun C (2007) Caring and contributing: The role of older women in multi generational households in the HIV/Aids era. World Development 35: 1390–1403. [Google Scholar]
- 17.Sartorius K, Sartorius BK, Tollman S, Schatz EJ, Collinson MA, et al.. (2011) Rural poverty dynamics and refugee communities in South Africa: A spatial- temporal model,. Population, Space and Place. [DOI] [PMC free article] [PubMed]
- 18. Yamauchi F, Buthelezi T, Velia M (2008) Impacts of Prime-age Adult Mortality on Labour Supply: Evidence from Adolescents and Women in South Africa*. Oxford Bulletin of Economics and Statistics 70: 375–398. [Google Scholar]
- 19. Mathers CD, Boerma T, Fat DM (2009) Global and regional causes of death. British medical bulletin 92: 7–32. [DOI] [PubMed] [Google Scholar]
- 20. Benzler J, Sauerborn R (1998) Rapid risk household screening by neonatal arm circumference. Results from a cohort study in Burkina Faso. Trop Med Int Health 3: 62–74. [DOI] [PubMed] [Google Scholar]
- 21.Walter S (2000) Disease mapping: a historical perspective. Spatial Epidemiology - Methods and Applications; Elliott P WJ, Best N, Briggs DJ, editor. Oxford: Oxford University Press.
- 22. Best N, Richardson S, Thomson A (2005) A comparison of Bayesian spatial models for disease mapping. Statistical Methods in Medical Research 14: 35–39. [DOI] [PubMed] [Google Scholar]
- 23. Rezaeian M, Dunn G, St Leger S, Appleby L (2007) Geographical epidemiology, spatial analysis and geographical information systems: a multidisciplinary glossary. J Epidemiol Community Health 61: 98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Clements AC, Lwambo NJ, Blair L, Nyandindi U, Kaatano G, et al. (2006) Bayesian spatial analysis and disease mapping: tools to enhance planning and implementation of a schistosomiasis control programme in Tanzania. Trop Med Int Health 11: 490–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Laaksonen MA, Knekt P, Harkanen T, Virtala E, Oja H (2010) Estimation of the population attributable fraction for mortality in a cohort study using a piecewise constant hazards model. Am J Epidemiol 171: 837–847. [DOI] [PubMed] [Google Scholar]
- 26.Statistics South Africa (2007) Community Survey 2007: Methodology, Processes and Highlights of Key Results. Pretoria: Statistics South Africa.
- 27.Statistics South Africa (2008) Community Survey 2007: Statistical Release Basic Results Municipalities. Pretoria: Statistics South Africa.
- 28.South African Statistics Council (2007) Statement on the results of the Community Survey (CS).
- 29.Day C, Barron P, Monticelli F, Sello E, editors (2009) The District Health Barometer 2007/2008. Durban: Health Systems Trust.
- 30.Esteve J, Benhamou E, Raymond L (1994) Statistical methods in cancer research, Vol. IV, descriptive epidemiology. Lyon: International Agency for Research on Cancer (IARC). [PubMed]
- 31. Pickle L, Mason T, Howard N, Hoover R, Fraumeni J (1987) Atlas of US cancer mortality among whites. 1950–1980: 87–2900. [Google Scholar]
- 32. Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159: 702–706. [DOI] [PubMed] [Google Scholar]
- 33. Zocchetti C, Consonni D, Bertazzi PA (1995) Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol 24: 1064–1067. [DOI] [PubMed] [Google Scholar]
- 34.Royall RM (1986) Model robust confidence intervals using maximum likelihood estimators. International Statistical Review/Revue Internationale de Statistique: 221–226.
- 35. Ahmed S, Hill K (2011) Maternal mortality estimation at the subnational level: a model-based method with an application to Bangladesh. Bulletin of the World Health Organization 89: 12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Herbst AJ, Cooke GS, Bärnighausen T, KanyKany A, Tanser F, et al. (2009) Adult mortality and antiretroviral treatment roll-out in rural KwaZulu-Natal, South Africa. Bulletin of the World Health Organization 87: 754–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bradshaw D, Laubscher R, Dorrington R, Bourne DE, Timaeus IM (2008) Unabated rise in number of adult deaths in South Africa. South African Medical Journal 94: 278. [PubMed] [Google Scholar]
- 38.Bradshaw D, Nannan N, Laubscher R (2006) South African national burden of disease study 2000. Estimates of provincial mortality: summary report.. Parow, Western Cape: Medical Research Council.
- 39. Rowe AK, Powell KE, Flanders WD (2004) Why population attributable fractions can sum to more than one. American journal of preventive medicine 26: 243. [DOI] [PubMed] [Google Scholar]
- 40.Rothman KJ, Greenland S, Lash TL (2008) Modern epidemiology: Lippincott Williams & Wilkins.
- 41. Magadi M, Desta M (2011) A multilevel analysis of the determinants and cross-national variations of HIV seropositivity in sub-Saharan Africa: evidence from the DHS. Health Place 17: 1067–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shiffman J (2006) HIV/AIDS and the rest of the global health agenda. Bulletin of the World Health Organization 84: 923–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tollman S, Kahn K, Sartorius B, Collinson M, Clark S, et al.. (2008) Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet 372. [DOI] [PMC free article] [PubMed]
- 44.Rose G (1992) The strategy of preventive medicine. The strategy of preventive medicine.
- 45. McKinlay JB (1998) Paradigmatic obstacles to improving the health of populations: implications for health policy. salud pública de méxico 40: 369–379. [DOI] [PubMed] [Google Scholar]
- 46. Arah OA, Westert GP, Delnoij DM, Klazinga NS (2005) Health system outcomes and determinants amenable to public health in industrialized countries: a pooled, cross-sectional time series analysis. BMC Public Health 5: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sachs JD (2004) Health in the developing world: achieving the Millennium Development Goals. Bulletin of the World Health Organization 82: 947–949. [PMC free article] [PubMed] [Google Scholar]
- 48.Mathers C, Loncar D (2011) Updated projections of global mortality and burden of disease, 2002–2030: data sources, methods and results. Geneva, Switzerland: World Health Organization; 2005.
- 49. Rockhill B, Newman B, Weinberg C (1998) Use and misuse of population attributable fractions. American journal of public health 88: 15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Benichou J (2001) A review of adjusted estimators of attributable risk. Statistical Methods in Medical Research 10: 195–216. [DOI] [PubMed] [Google Scholar]
- 51. Rückinger S, von Kries R, Toschke AM (2009) An illustration of and programs estimating attributable fractions in large scale surveys considering multiple risk factors. BMC Medical Research Methodology 9: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]