Abstract
Context
Early identification of Bipolar Disorder (BD) remains poor despite the high levels of disability associated with the disorder.
Objective
We developed and evaluated a new DSM orientated scale for the identification of young people at risk for BD based on the Child Behavior Checklist (CBCL) and compared its performance against the CBCL-Pediatric Bipolar Disorder (CBCL-PBD) and the CBCL-Externalizing Scale, the two most widely used scales.
Methods
The new scale, CBCL-Mania Scale (CBCL-MS), comprises 19 CBCL items that directly correspond to operational criteria for mania. We tested the reliability, longitudinal stability and diagnostic accuracy of the CBCL-MS on data from the TRacking Adolescents' Individual Lives Survey (TRAILS), a prospective epidemiological cohort study of 2230 Dutch youths assessed with the CBCL at ages 11, 13 and 16. At age 19 lifetime psychiatric diagnoses were ascertained with the Composite International Diagnostic Interview. We compared the predictive ability of the CBCL-MS against the CBCL-Externalising Scale and the CBCL-PBD in the TRAILS sample.
Results
The CBCL-MS had high internal consistency and satisfactory accuracy (area under the curve = 0.64) in this general population sample. Principal Component Analyses, followed by parallel analyses and confirmatory factor analyses, identified four factors corresponding to distractibility/disinhibition, psychosis, increased libido and disrupted sleep. This factor structure remained stable across all assessment ages. Logistic regression analyses showed that the CBCL-MS had significantly higher predictive ability than both the other scales.
Conclusions
Our data demonstrate that the CBCL-MS is a promising screening instrument for BD. The factor structure of the CBCL-MS showed remarkable temporal stability between late childhood and early adulthood suggesting that it maps on to meaningful developmental dimensions of liability to BD.
Introduction
Bipolar Disorder (BD) is a complex mental disorder affecting between 0.1% and 4.4% of the general population [1]. BD is the sixth leading cause of disability worldwide particularly amongst adolescents and young adults [2]. This is partly due to the typically early onset of BD with the majority of patients presenting between 19–25 years of age [1], [3]. More important however is the failure in recognizing and treating BD particularly in the early stages of the disorder. The typical delay between onset and diagnosis is 5–10 years [4]–[6] and is associated with greater clinical severity, increased psychosocial morbidity and higher treatment costs [7]–9. Although mania is the diagnostic hallmark of BD [10], [11] the differential diagnosis from Major Depressive Disorder (MDD) is often difficult as BD is commonly dominated by depressive symptoms [12], [13]. Furthermore, BD is also associated with high rates (between 60–80%) of psychotic symptoms during mood episodes [14], [15]. High rates of psychotic symptoms have also been reported in young patients and confirm their role as a key symptom dimension of BD in adolescence [16], [17]. Additional diagnostic challenges arise from the symptomatic overlap between BD and Attention Deficit Hyperactivity Disorder (ADHD), which also presents with poor attentional and emotional regulation [18].
In response to the need for the early identification of individuals at high risk for BD there have been several attempts to develop and validate screening instruments. In adults, one of the most widely studied screening instruments is the Mood Disorder Questionnaire (MDQ) [19], a self-report questionnaire based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for mania. A positive MDQ screen is based on participants endorsing 7 or more lifetime manic symptoms, several co-occurring, resulting to moderate or serious functional impairment. In outpatient psychiatric settings the MDQ was reported to achieve sensitivity and specificity rates of 67%–83% and 86%, respectively [5]. Although specificity and sensitivity are theoretically independent of prevalence, in practice they are influenced by the clinical composition of the sample (e.g. proportion of severe to mild cases) and interviewers' assumptions about the frequency of a disorder [20]. Typically, in general population samples sensitivity is lower and specificity is higher than that reported in clinical populations. For example, the sensitivity and specificity of the MDQ in the general population are respectively 23–25% and 97–99% [21], [22]. Additionally, many individuals with MDD, anxiety disorders or ADHD screen positive on the MDQ [22], [23].
A significant number of screening instruments for juvenile BD have been developed and have been used mostly in clinical populations. These include the Parent version of the Young Mania Rating Scale (P-YMRS) [24], the Parent General Behavior Inventory (P-GBI) [25], the Adolescent General Behavior Inventory (A-GBI) [26], the Youth Self Report (YSR) [27], the Teacher Report Form (TRF) [28], the Child Mania Rating Scale (CMRS) [29], the Child Behaviour Checklist (CBCL) [30], and the Mood Disorder Questionnaire Adolescent Version (MDQ-A) [31]. The CBCL [30] is the instrument most commonly used to generate profiles relevant to BD in youth. The CBCL is a parent report checklist of 118 items mapping onto multiple aspects of psychopathology over a 6-month period [30], [32]. The CBCL items are grouped in eight behavioural domains: aggressive behaviour, anxiety/depression, attention problems, rule-breaking behavior, withdrawal/depression, somatic complaints, social problems and thought problems [30]. Different scales have been generated based on varied combinations of these behavioural domains. Of relevance to BD, are the Externalizing Scale (comprising item scores from the rule-breaking and aggressive behavior domains) and the CBCL-Pediatric Bipolar Disorder scale (CBCL-PBD) (comprising item scores from the aggressive behavior, anxiety/depression and attention problems domains) [33]. The CBCL-PBD is also referred to as the Dysregulation Profile as it has been associated with disorder involving extensive behavioural and emotional dysregulation [34] including BD [35]. However all available instruments have limited specificity for BD as they have been associated with MDD, ADHD and anxiety disorders [36]–[40].
Therefore there is still a need for screening instruments for BD particularly for use in non-clinical populations of young individuals. In an attempt to address this need we developed and evaluated a new screening scale for BD in children and adolescents based on the CBCL 6–18 [30]. Despite the limited success of previous CBCL-based screening instruments for juvenile BD we decided to use it as the base of the new scale because of its cross-cultural generalizability [41]. However, instead of using summary scores of the existing behavioural domains we constructed this new scale following the methodology defined for DSM-oriented subscale development by Achenbach et al. (2003) [42]. Content validity of the new scale was evaluated by an expert panel of child and adolescent psychiatrists who selected 19 CBCL items that relate directly to the diagnostic criteria for mania as currently operationalized in the DSM5 (details in File S1). The new scale called CBCL-Mania Scale (CBCL-MS) was tested for its psychometric properties, sensitivity and specificity on data from the TRacking Adolescents' Individual Lives Survey (TRAILS) [http://www.trails.nl/en/] [43]. TRAILS is a prospective study of an epidemiologically representative cohort of 2230 Dutch adolescents who were assessed with the full CBCL at age 11,13 and 16. Clinical outcomes were evaluated at age 19 using the Composite International Diagnostic Interview (CIDI) [44]. We also compared the performance of the CBCL-MS against the CBCL-Externalising Scale and the CBCL-PBD to test whether it presents an improvement in terms of accuracy and predictive ability.
Methods
Participants
The sample consisted of participants of 2230 Dutch youth participating in the TRacking Adolescents' Individual Lives Survey (TRAILS). The sampling procedure and cohort details for TRAILS have been previously described in detail [43] and can be found at the study website [http://www.trails.nl/en/]. Briefly, the cohort includes children born between 1 October 1989 and 30 September 1991 in a well-defined geographic area in the north Netherlands (information about the representativeness of the sample in S2). Permission to use anonymised data from the TRAILS was granted by the study management committee and ethical approval was granted by the Dutch Central Committee on Research Involving Human Subjects (CCMO). All data were anonymised by a research company TNS NIPO [http://www.tns-nipo.com/].
Assessments
When TRAILS cohort members were 11, 13 and 16 years old, their parents or parent surrogates completed the CBCL 6–18. Each CBCL item was scored on a three point scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true) on the basis of the preceding 6 months. At age 19 years the diagnostic status of the TRAILS participants was ascertained using the Computer Assisted Personal Interview version 20 (CAPI) of the CIDI [http://www.hcp.med.harvard.edu/wmhcidi/]. The CIDI is a comprehensive, structured interview which was used by trained lay interviewers to assess mental disorders according to current diagnostic systems. It has high test-retest reliability for the diagnosis of BD type I (BD-I) [45] as well as excellent concordance rates with the Structured Clinical Interview for DSM-IV (SCID) for lifetime bipolar spectrum disorders [46]. Diagnostic assessments were conducted blind to participants' CBCL scores.
Child Behavior Check List - Mania Scale (CBCL-MS)
An expert panel of child and adult psychiatrists, based at the Institute of Psychiatry and the South London and Maudsley NHS Foundation Trust, independently screened all CBCL items to select those that correspond to the DSM operational criteria for mania. As the diagnostic criteria for mania in DSM5 and ICD-10 are identical [www.who.int/classificatios/icd/en/GRNBOOK.pdf] this selection is applicable to both diagnostic systems. In addition, the panel considered CBCL items relating to psychotic-like experiences as childhood and adolescent psychosis and high CBCL total scores are frequently associated with later development of mania [37]–[40]. Following consensus meetings, 19 items were selected for inclusion in the new CBCL- Mania Scale (CBCL-MS) (Table 1). Detailed information on the item selection procedure is included in File S1. The scoring of the CBCL-MS at each assessment age was based on summing the scores of each of the 19 individual items. Scores were then standardized (T scores) following the scoring procedure recommended by Achenbach and Rescorla (2001) [32] using the TRAILS data as the standardization sample. Standardization of the CBCL scores for the CBCL-MS, as well as for other CBCL-based syndrome scales, was performed separately at each assessment age. The CBCL-MS and its scoring are available in File S5.
Table 1. Child Behavior Checklist-Mania Scale items and corresponding core and extended DSM-IV criteria for Mania.
| CBCL Items | DSM-IV criteria for Mania |
| Core Symptoms | |
| 37. Gets in many fights | A distinct period of abnormally and persistently elevated, expansive or irritable mood |
| 87. Sudden changes in mood or feelings | |
| 96. Thinks about sex too much | |
| 74. Showing off or clowning | Inflated self-esteem or grandiosity |
| 94. Teases a lot | |
| 76. Sleeps less than most kids | Decreased need for sleep (e.g., feels rested after only 3 hours of sleep) |
| 100. Trouble sleeping | |
| 93. Talks too much | More talkative than usual or pressure to keep talking |
| 104. Unusually loud | Flight of ideas or subjective experience that thoughts are racing |
| 78. Inattentive or easily distracted | Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli) |
| 10. Can't sit still, restless or hyperactive | Increase in goal-directed activity (at work, at school, or sexually) or psychomotor agitation |
| 60. Plays with own sex parts too much | |
| 41. Impulsive or acts without thinking | Excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments) |
| 59. Plays with own sex parts in public | |
| Extended Symptoms | |
| 34. Feels others are out to get him/her | Delusions |
| 85. Strange ideas | |
| 89.Suspicious | |
| 40. Hears sound or voices that aren't there | Hallucinations |
| 70. Sees things that aren't there | |
Statistical Analysis
Analyses were performed using IBM SPSS Statistics, Version 19 (www.spss.com) and MPlus 6.0 (www.statmodel.com).
Reliability and validity of the CBCL-MS
As the CBCL-MS is a new scale the consistency of its items at each assessment wave was evaluated using Cronbach's alpha. In order to determine the number of factors that best describe the latent factor structure of the CBCL-MS at ages 11, 13 and 16 the following criteria were considered: the shape of the scree plot, parallel analysis using a permutated data approach (number of data sets: 5000; confidence interval 95%) [47], [48], the Kaiser criterion as an upper bound for the number of factors to be retained, and the interpretability of the obtained factor structure. In order to conduct the parallel analysis, principal components analysis (PCA) was performed first, with oblique or varimax rotation (as appropriate). For each assessment age, the model fit of the final solutions was established using Confirmatory Factor Analysis (CFA) and assessed using two fit indices, the Root Mean Square Error of Approximation (RMSEA) (cut-off values less than 0.06 indicate good fit and values as high as 0.08 represent reasonable errors of approximation in the population) and the Confirmatory Fit index (CFI) (values above 0.90–0.95 indicate good fit) [49].
Sensitivity and Specificity of the CBCL-MS
Omnibus tests using the standardized T scores of the CBCL-MS, the CBCL-Externalizing Scale and the CBCL-PBD were performed to compare the scores of participants with CIDI diagnoses of BD type I (BD-I) to those of healthy participants and participants with other CIDI diagnoses that are considered relevant to BD as they involve mood abnormalities (anxiety or depression) or inattention and behavioral disruption. We present data on Major Depressive Disorder (MDD), General Anxiety Disorder (GAD), and ADHD as the most pertinent exemplars. Finally, Receiver Operating Characteristics (ROC) curves [50] were used to calculate the diagnostic efficiency of the CBCL-MS, CBCL-PBD and CBCL-Externalizing Scale. A ROC curve illustrates the sensitivity (true positive rate) of different cut-offs on the y axis and the 1-specificity (false positive rate) of the corresponding cut-offs on the x axis. In the ROC analysis, the area under the curve (AUC) statistic provides a summary of test performance. AUC values range from 0 to 1 with higher values denoting greater discriminative power and diagnostic efficiency. The focus of the analysis was on BD-I as the usefulness of a test with poor discriminative ability for core syndromal BD would be questionable. However, we also performed ROC analysis using a more expanded definition of caseness that also included BD type II (BD-II) and hypomania with no major depressive episode.
Results
TRAILS participants with BD
At age 19, 56 of the TRAILS participants were diagnosed with BD-I. Thirty-four cases had attracted other psychiatric diagnoses prior to being diagnosed with BD; seventeen had a single previous diagnosis either for Oppositional Defiant Disorder (ODD) (n = 5) or Conduct Disorder (CD) (n = 5) or ADHD (n = 4) or GAD (n = 3). Of the remaining seventeen BD cases, eleven had two prior diagnoses (ADHD/ODD = 2, ADHD/CD = 1, ADHD/GAD = 1, ADHD/MDD = 1, ODD/CD = 3, ODD/GAD = 2, ODD/MDD = 1), five had three prior diagnoses (ODD/CD/GAD = 3, ODD/CD/ADHD = 2) and one had four (ODD/CD/ADHD/GAD).
Internal consistency and factor structure of the CBCL-MS
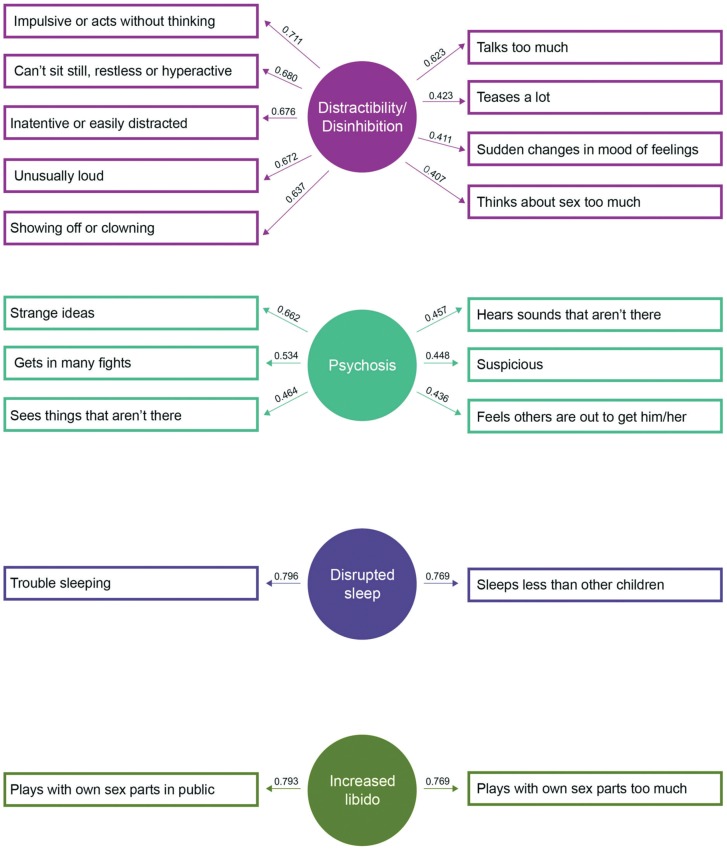
Reliability analysis demonstrated high internal consistency for the 19 items of the CBCL-MS at all assessment ages (Cronbach's alpha≥80; total item correlation >0.37). A PCA of the CBCL-MS data assessed at age 16 extracted four factors corresponding to: (1) distractibility/disinhibition (2) psychotic symptoms (3) increased libido (4) disrupted sleep (Figure 1). These factors were plausible and interpretable as items' loading segregated among the four factors as shown in File S3 and Table S2. The factor structure represents the orthogonal solution of the PCA, as the factors extracted using oblique rotation were only weakly correlated (r<0.3). Both the Parallel Analysis and Kaiser's criterion supported the retention of four factors. The scree plot of the extracted eigenvalues from the parallel analysis is given in Figure S1, available on line. Analyses of the CBCL-MS data at ages 11 and 13 years resulted in an almost identical factor structure indicating longitudinal stability of this solution (File S3 and Tables S2, S3 and S4). Confirmatory factor analyses further supported the goodness of fit of 4-factor structure (RMSEA≤0.05 and CFI≥0.92).
Figure 1. Factors and Factor Loadings of the Child Behavior Checklist-Mania Scale.
Discriminative ability and performance of the CBCL-MS
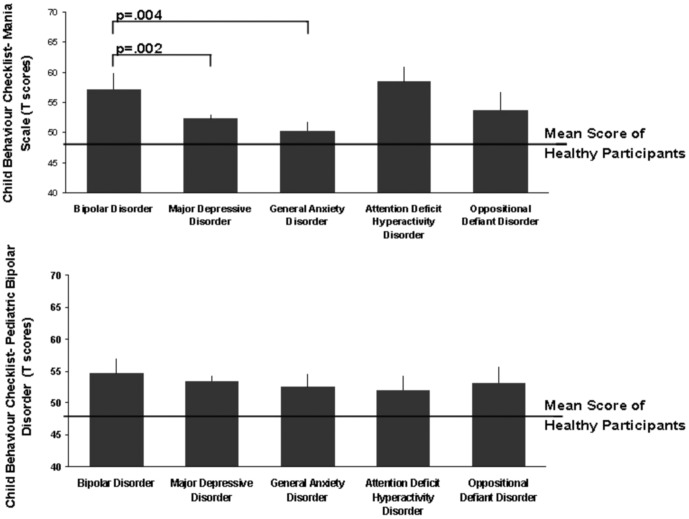
Table 2 presents the mean total and CBCL-MS factor scores for TRAILS participants who were diagnosed with BD-I and for those who did not have any lifetime psychiatric diagnosis. Participants with BD had significantly higher mean total CBCL-MS scores compared with participants with MDD (n = 178; p = 0.002) and GAD (N = 20; p = 0.004) but not ADHD (N = 26; p>0.05) (Figure 2).
Table 2. Child Behavior Checklist-Mania Scale total and Factor Scores in TRAILS participants with Bipolar Disorder (BD) and healthy participants.
| BD participants (N = 56) | Healthy Participants (N = 1201) | ||
| Mean Score (Standard Deviation) | p | ||
| Total CBCL-MS | 57.28 (16.08) | 49.33 (8.95) | <0.001 |
| Distractibility/Disinhibition | 56.01 (14.71) | 49.18 (8.98) | <0.001 |
| Psychotic Symptoms | 56.19 (20.20) | 49.44 (8.84) | <0.001 |
| Increased Libido | 51.99 (12.28) | 49.48 (8.88) | 0.088 |
| Disrupted Sleep | 54.42 (12.28) | 49.63 (9.33) | 0.002 |
Figure 2. Child Behavior Checklist-Mania Scale Scores in TRAILS Participants.
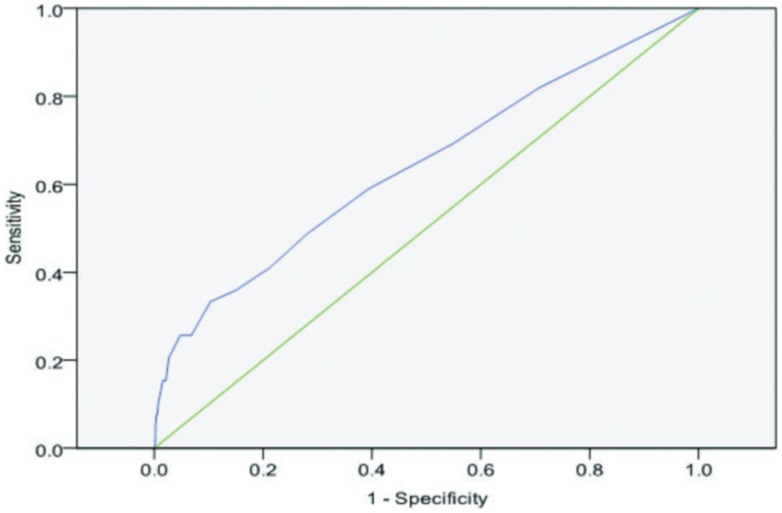
The ROC curve analysis on the CBCL-MS data at age 16 is illustrated in Figure 3. The AUC was 0.64 (p<0.01) which represents a satisfactory performance for a general population sample with low prior probability of true positives. The AUC remained unchanged when caseness was expanded to include BD-II and hypomania without major depressive episode. Moreover, the total CBCL-MS score performed better than the scores of each individual factors used independently or sequentially (details in supporting information S4 and Tables S5 and S6).
Figure 3. Receiver Operating Characteristics curve of the Child Behavior Checklist-Mania Scale for Bipolar Disorder vs. healthy TRAILS participants.
Comparison to CBCL-PBD: TRAILS participants with BD-I had significantly higher CBCL-PBD mean scores (56.51, SD = 15.91) in comparison to healthy participants (49.79, SD = 9.69) but not compared to participants with MDD (p = 0.54), GAD (p = 0.51) or ADHD (p = 0.37). ROC curve analysis showed a moderate ability of the CBCL-PBD in distinguishing BD-I cases from healthy TRAILS participants (AUC = 61%, p = 0.002).
Comparison to the Externalizing scale of the CBCL: Externalizing scale mean scores were significantly higher for TRAILS participants with BD-I (58.49, SD = 18.27) in comparison to healthy participants (48.44, SD = 8.25) and participants with MDD (52.00, SD = 9.80) or GAD (50.52, SD = 7.80), but not compared to participants with ADHD (p = 0.23). ROC analysis showed that the Externalizing scale had AUC = 63%, p = 0.003 when discriminating between TRAILS cases with BD-I and healthy participants.
A forward stepwise logistic regression model showed that the CBCL-MS had significantly increased ability to predict BD-I compared to the CBCL-PBD (Wald χ2 = 12.69, p<0.001) and the CBCL-Externalizing Scale (Wald χ2 = 3.47, p = 0.05).
Discussion
We present data on the psychometric properties and discriminative ability of the CBCL-MS, a new DSM based screening scale for BD-I based on the CBCL. We demonstrate that the new scale has excellent psychometric properties; its discriminative ability and accuracy in a general population sample of young people represent an improvement over other commonly used scales particularly CBCL-PBD and the CBCL-Externalizing Scale.
Prevalence and Characteristics of TRAILS participants with BD
The lifetime prevalence of BD-I in the TRAILS sample was 2.5% which is identical to that reported in a recent epidemiological study of US adolescents [51]. Also consistent with previous literature, nearly 61% of BD-I cases in the TRAILS sample had prior diagnoses associated with disruptive behaviour most commonly ADHD and ODD [18], [50]–[54].
Factor Structure of the CBCL-MS reveals developmentally meaningful dimensions of liability to BD
The structural model of the CBCL-MS consisted of four factors. These factors correspond to dimensions of distractibility/disinhibition, psychosis, increased libido and disrupted sleep. The factor structure of the CBCL-MS showed remarkable temporal stability between the ages of 11 to 16 which strongly supports the notion that it defines developmentally meaningful dimensions of liability to BD. This report is the first to describe developmental dimensions of liability to BD. All other studies have focused on symptom dimensions during acute manic episodes in patients with established BD [54]–[58]. Nevertheless, there are significant similarities. Cassidy and colleagues identified 5 factors in acute mania of which the “psychomotor pressure”, “psychosis” and “increased hedonic” factors correspond to the distractibility/disinhibition, psychosis and increased libido factors in this study [55]. Picardi et al [56] defined a four factor structure of acute mania based on the Brief Psychiatric Rating Scale. The factors they named “mania” and “disorganisation” include items similar to the distractibility/disinhibition factor identified here. In addition their “positive symptoms” factor overlaps with the psychosis factor in this study. Cassano et al [57] identified 5 factors in acute mania of which “psychomotor agitation” and “psychoticism” correspond to the factors of distractibility/disinhibition and psychosis in the TRAILS cohort. All three studies also defined factors relating to dysphoric/euphoric mood and aggression that seem to be present only during acute mania and may not represent an independent dimension of developmental liability to BD.
Discriminative ability of the CBCL-MS
The overall accuracy was 0.64 for the CBCL-MS and CBCL-Externalising Scale and 0.61 for the CBCL-PBD. The results of the logistic regression comparing the three scales showed that the CBCL-MS was statistically better in predicting BD outcome.
As seen by the ROC, different cut-off scores will influence the sensitivity and specificity of the CBCL-MS. In general population screening the emphasis is usually on specificity thus selecting individuals at highest risk for detailed follow-up assessments. To illustrate this point, in a hypothetical community sample of 10000 youth with a 2.5% prevalence of BD we would expect 250 individuals to have BD (true positives). A CBCL-MS score of 70 or above will correctly identify 8,775 individuals (90% of this sample) as not having BD (true negatives). At the same threshold, 1,050 individuals will be classified as possible cases. This sample will include 75 true cases of BD (true positives) and 975 individuals without BD (false positives). At first glance, one might be concerned about the number of false positive cases. However, those scoring above 70 in the CBCL-MS were at a six-fold increased risk for BD (Positive Predictive Value: 16.57%; Negative Predictive Value: 98.01%) compared to the rest of the sample and therefore they represent a high risk group. The field of early intervention in BD is currently in its infancy [59] but as effective therapies become available [60] scales such as the CBCL-MS may contribute to the identification of those at high risk.
None of the scales differentiated participants with BD from those with ADHD in terms of mean scores. The relationship between these two disorders is complex. Available evidence suggests at least partially overlapping aetiology and pathophysiology for BD and ADHD because of familial co-segregation of the two disorders [61], [62], commonalities in their neurobiological correlates [18], [63], [64], and frequent comorbidity [18]. Additionally, there is significant overlap in the symptoms of the two disorders particularly with regards to increased activity, talkativeness and mood dysregulation [10], [11]. Two main features distinguishing BD from ADHD have been proposed. Geller and colleagues emphasized the importance of either elevated mood or grandiosity for a diagnosis of mania [65]. However, in our study these symptoms clustered with others in one factor and did not differ across the two diagnostic categories. Others have suggested that episodicity is more indicative of BD than ADHD [66] but this distinction seems less clear in children and adolescents [51]. It is therefore possible that scales based on observed behaviour lack assay sensitivity in distinguishing between BD and ADHD.
Methodological Issues and Future Directions
The present study has a number of strengths and limitations. The TRAILS sample is representative of the population of young people in the Netherlands (Table S6). The prevalence of BD in the TRAILS is nearly identical to that of general population samples elsewhere [1], [51] which supports the generalizability of findings. Case ascertainment in the TRAILS does not depend on help-seeking behaviour or concern about impairment or severity and thus the sample is free from referral bias present in clinical populations. However, the CIDI although widely used is designed for lay interviewers who rely on its structured format and may not probe or interpret participant responses further. Case ascertainment was conducted at age 19. Since participants have not yet passed the entire period of risk for BD it is possible that further cases of BD may present in the future.
The CBCL-MS performed well within the context of a general population sample, it represents an improvement on available scales and could contribute to future public health initiatives for the identification of youth at high risk for BD. Its accuracy is moderate and in the same broad range of the other CBCL-based screening instruments. Although it could be argued that this is reflects limitations in the CBCL we would suggest that behavioural ratings alone are unlikely to provide us with high levels of accuracy in case identification for BD or any mental disorder. However a great strength of this study was the availability of CBCL assessments at multiple time points from late childhood to early adulthood. This allowed us to test the temporal stability of the CBCL-MS factors which supports the validity of these dimensions as developmentally meaningful premorbid indicators of BD.
Supporting Information
Scree Plot.
(TIF)
Selection of Items for the CBCL-MS.
(DOC)
Representativeness of the TRAILS sample.
(DOC)
Psychometric properties of the CBCL-MS across ages.
(DOC)
Discriminative ability of the CBCL-MS.
(DOC)
Appendix: CBCL-MS (scale and scoring sheet).
(PDF)
Acknowledgments
Participating centers of TRAILS in the Netherlands, including the University Medical Center and University of Groningen, the Erasmus University Medical Center Rotterdam, the University of Utrecht, the Radboud Medical Center Nijmegen, and the Parnassia Bavo group.
Funding Statement
TRAILS has been supported by grants from the Netherlands Organization for Scientific Research NWO (Medical Research Council program grant GB-MW 940-38-011; ZonMW Brainpower grant 100-001-004; ZonMw Risk Behavior and Dependence grants 60-60600-97-118; ZonMw Culture and Health grant 261-98-710; Social Sciences Council medium-sized investment grants GB-MaGW 480-01-006 and GB-MaGW 480-07-001; Social Sciences Council project grants GB-MaGW 452-04-314 and GB-MaGW 452-06-004; NWO large-sized investment grant 175.010.2003.005; NWO Longitudinal Survey and Panel Funding 481-08-013), the Dutch Ministry of Justice (WODC), the European Science Foundation (EuroSTRESS project FP-006), Biobanking and Biomolecular Resources Research Infrastructure BBMRI-NL (CP 32), and the participating universities. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Merikangas KR, Jin R, He JP, Kessler RC, Lee S, et al. (2011) Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry 68: 241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Murray CJ, Lopez AD, Jamison DT (1994) The global burden of disease in 1990: summary results, sensitivity analysis and future directions. Bull World Health Organ 72: 495–509. [PMC free article] [PubMed] [Google Scholar]
- 3. Perlis RH, Miyahara S, Marangell LB, Wisniwski SR, Ostacher M (2004) Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry 55: 875–881. [DOI] [PubMed] [Google Scholar]
- 4. Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM (1994) The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 31: 281–294. [DOI] [PubMed] [Google Scholar]
- 5. Hirschfeld RM, Lewis L, Vornik LA (2003) Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry 64: 161–174. [PubMed] [Google Scholar]
- 6. Berk M, Dodd S, Callaly P, Berk L, Fitzgerald P, et al. (2007) History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J Affect Disord 103: 181–186. [DOI] [PubMed] [Google Scholar]
- 7. Keck PE Jr, Kessler RC, Ross R (2008) Clinical and economic effects of unrecognized or inadequately treated bipolar disorder. J Psychiatr Pract 14 Suppl 2: 31–38. [DOI] [PubMed] [Google Scholar]
- 8. Post RM, Leverich GS, Kupka RW, Keck PE Jr, McElroy SL, et al. (2010) Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry 71: 864–872. [DOI] [PubMed] [Google Scholar]
- 9. Ketter TA (2011) Strategies for the early recognition of bipolar disorder. J Clin Psychiatry 72: e22. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association (2013) Diagnostic and Statistical Manual for Mental Disorders, 5th Edition (DSM5). Washington, D.C.: American Psychiatric Association.
- 11.World Health Organisation (1992) ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organisation.
- 12. Perugi G, Micheli C, Akiskal HS, Madaro D, Socci C, et al. (2000) Polarity of the first episode, clinical characteristics, and course of manic depressive illness: a systematic retrospective investigation of 320 bipolar I patients. Compr Psychiatry 41: 13–18. [DOI] [PubMed] [Google Scholar]
- 13. Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, et al. (2002) The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 59: 530–537. [DOI] [PubMed] [Google Scholar]
- 14. Keck PE Jr, McElroy SL, Havens JR, Altshuler LL, Nolen WA (2003) Psychosis in bipolar disorder: Phenomenology and impact on morbidity and course of illness. Compr Psychiatry 44: 263–269. [DOI] [PubMed] [Google Scholar]
- 15. Coryell W, Leon AC, Turvey C, Akiskal HS, Mueller T, et al. (2001) The significance of psychotic features in manic episodes: A report from the NIMH collaborative study. J Affect Disord 67: 79–88. [DOI] [PubMed] [Google Scholar]
- 16. Johns LC, Nazroo JY, Bebbington P, Kuipers E (2002) Occurrence of hallucinatory experiences in a community sample and ethnic variations. Br J Psychiatry 180: 174–178. [DOI] [PubMed] [Google Scholar]
- 17. Topor DR, Swenson L, Hunt JI, Birmaher B, Strober M, et al. (2013) Manic symptoms in youth with bipolar disorder: Factor analysis by age of symptom onset and current age. J Affect Disord 145: 409–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Skirrow C, Hosang GM, Farmer AE, Asherson P (2012) An update on the debated association between ADHD and bipolar disorder across the lifespan. J Affect Disord 141: 143–159. [DOI] [PubMed] [Google Scholar]
- 19. Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L (2000) Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry 157: 1873–1875. [DOI] [PubMed] [Google Scholar]
- 20. Robins LN (1985) Epidemiology: reflections on testing the validity of psychiatric interviews. Arch Gen Psychiatry 42: 918–924. [DOI] [PubMed] [Google Scholar]
- 21. Hirschfeld RM, Holzer C, Calabrese JR, Weissman M, Reed M (2003) Validity of the mood disorder questionnaire. Am J Psychiatry 160: 178–180. [DOI] [PubMed] [Google Scholar]
- 22. Dodd S, Williams LJ, Jacka FN, Pasco JA, Bjerkeset O, et al. (2009) Reliability of the Mood Disorder Questionnaire: comparison with the Structured Clinical Interview for the DSM-IV-TR in a population sample. Aust N Z J Psychiatry 43: 526–530. [DOI] [PubMed] [Google Scholar]
- 23. Zimmerman M, Galione JN, Ruggero CJ, Chelminski I, Dalrymple K, et al. (2011) Are screening scales for bipolar disorder good enough to be used in clinical practice? Compr Psychiatry 52: 600–606. [DOI] [PubMed] [Google Scholar]
- 24. Gracious BL, Youngstrom EA, Findling RL, Calabrese JR (2002) Discriminative validity of a parent version of the Young Mania Rating Scale. J Am Acad Child Adolesc Psychiatry 41: 1350–1359. [DOI] [PubMed] [Google Scholar]
- 25. Youngstrom EA, Findling RL, Danielson CK, Calabrese JR (2001) Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychol Assess 13: 267–276. [PubMed] [Google Scholar]
- 26. Danielson CK, Youngstrom EA, Findling RL, Calabrese JR (2003) Discriminative validity of the general behavior inventory using youth report. J Abnorm Child Psychol 31: 29–39. [DOI] [PubMed] [Google Scholar]
- 27.Achenbach TM (1991) Integrative guide for the 1991 CBCL/4-18, YSR and TRF profiles. Deaprtment of Psychiatry, Burlington, VT: University of Vermont
- 28.Achenbach TM (1991) Manual for the Teacher Report Form and 1991 profile. Deaprtment of Psychiatry, Burlington, VT: University of Vermont.
- 29. Pavuluri MN, Henry DB, Devineni B, Carbray JA, Birmaher B (2006) Child mania rating scale: development, reliability, and validity. J Am Acad Child Adolesc Psychiatry 45: 550–560. [DOI] [PubMed] [Google Scholar]
- 30.Achenbach TM (1991) Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Department of Psychiatry. Burlington, VT: University of Vermont.
- 31. Wagner KD, Hirschfeld RM, Emslie GJ, Findling RL, Gracious BL, et al. (2006) Validation of the Mood Disorder Questionnaire for bipolar disorders in adolescents. J Clin Psychiatry 67: 827–830. [DOI] [PubMed] [Google Scholar]
- 32.Achenbach TM, Rescorla LA (2001) Manual for the ASEBA School-Age Forms & Profiles. Research Center for Children, Youth and Families. Burlington, VT: University of Vermont.
- 33. Biederman J, Wozniak J, Kiely K, Ablon S, Faraone S, et al. (1995) CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry 34: 464–471. [PubMed] [Google Scholar]
- 34. Kim J, Carlson GA, Meyer SE, Bufferd SJ, Dougherty LR, et al. (2012) Correlates of the CBCL-dysregulation profile in preschool-aged children. J Child Psychol Psychiatry 53: 918–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Faraone SV, Althoff RR, Hudziak JJ, Monuteaux M, Biederman J (2005) The CBCL predicts DSM bipolar disorder in children: a receiver operating characteristic curve analysis. Bipolar Disord 7: 518–524. [DOI] [PubMed] [Google Scholar]
- 36. Mick E, Biederman J, Pandina G, Faraone SV (2003) A preliminary meta-analysis of the child behavior checklist in pediatric bipolar disorder. Biol Psychiatry 53: 1021–1027. [DOI] [PubMed] [Google Scholar]
- 37. Youngstrom EA, Findling RL, Calabrese JR, Gracious BL, Demeter C, et al. (2004) Comparing the diagnostic accuracy of six potential screening instruments for bipolar disorder in youths aged 5 to 17 years. J Am Acad Child Adolesc Psychiatry 43: 847–858. [DOI] [PubMed] [Google Scholar]
- 38. Volk HE, Todd RD (2007) Does the Child Behavior Checklist Juvenile Bipolar Disorder Phenotype Identify Bipolar Disorder? Biol Psychiatry 62: 115–120. [DOI] [PubMed] [Google Scholar]
- 39. Diler RS, Birmaher B, Axelson D, Goldstein B, Gill M, et al. (2009) The Child Behavior Checklist (CBCL) and the CBCL-bipolar phenotype are not useful in diagnosing pediatric bipolar disorder. J Child Adolesc Psychopharmacol 19: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J (2010) Adult outcomes of childhood dysregulation: a 14-year follow-up study. J Am Acad Child Adolesc Psychiatry 49: 1105–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ivanova MY, Dobrean A, Dopfner M, Erol N, Fombonne E, et al. (2007) Testing the 8-syndrome structure of the child behavior checklist in 30 societies. Holland to Australia. J Clin Child Adolesc Psychol 36: 405–417. [DOI] [PubMed] [Google Scholar]
- 42. Achenbach TM, Dumenci L, Rescorla LA (2003) DSM-oriented and empirically based approaches to constructing scales from the same item pools. J Clin Child Adolesc Psychol 32: 328–340. [DOI] [PubMed] [Google Scholar]
- 43. Huisman M, Oldehinkel AJ, de Winter A, Minderaa RB, de Bildt A, et al. (2008) Cohort Profile: The Dutch ‘TRacking Adolescents’ Individual Lives ‘Survey’; TRAILS. Int J Epidemiol 37: 1227–1235. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organisation (1990) Composite International Diagnostic Interview (CIDI). Geneva:World Health Organisation.
- 45. Wittchen HU (1994) Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 28: 57–84. [DOI] [PubMed] [Google Scholar]
- 46. Kessler RC, Akiskal HS, Angst J, Guyer M, Hirschfeld RM, et al. (2006) Validity of the assessment of bipolar spectrum disorders in the WHO CIDI 3.0. J Affect Disord 96: 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Horn JL (1965) A rationale and test for the number of factors in factor analysis. Psychometrika 30: 179–185. [DOI] [PubMed] [Google Scholar]
- 48. Zwick WR, Velicer WF (1986) Comparison of Five Rules for Determining the Number of Components to Retain. Psychol Bull 99: 432–442. [DOI] [PubMed] [Google Scholar]
- 49. Hu Lt, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling 6: 1–55. [Google Scholar]
- 50. Grzybowski M, Younger JG (1997) Statistical methodology: III. Receiver operating characteristic (ROC) curves. Acad Emerg Med 4: 818–826. [DOI] [PubMed] [Google Scholar]
- 51. Merikangas KR, Cui L, Kattan G, Carlson GA, Youngstrom EA, et al. (2012) Mania with and without depression in a community sample of US adolescents. Arch Gen Psychiatry 69: 943–951. [DOI] [PubMed] [Google Scholar]
- 52. Biederman J, Faraone SV, Wozniak J, Mick E, Kwon A, et al. (2004) Further evidence of unique developmental phenotypic correlates of pediatric bipolar disorder: findings from a large sample of clinically referred preadolescent children assessed over the last 7 years. J Affect Disord 82 Suppl 1: S45–58. [DOI] [PubMed] [Google Scholar]
- 53. Duffy A, Alda M, Crawford L, Milin R, Grof P (2007) The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disord 9: 828–838. [DOI] [PubMed] [Google Scholar]
- 54. Biederman J, Petty CR, Monuteaux MC, Mick E, Parcell T, et al. (2008) The longitudinal course of comorbid oppositional defiant disorder in girls with attention-deficit/hyperactivity disorder: findings from a controlled 5-year prospective longitudinal follow-up study. J Dev Behav Pediatr 29: 501–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cassidy F, Forest K, Murry E, Carroll BJ (1998) A Factor analysis of the signs and symptoms of mania. Arch Gen Psychiatry 55: 27–32. [DOI] [PubMed] [Google Scholar]
- 56. Picardi A, Battisti F, de Girolamo G, Morosini P, Norcio B, et al. (2008) Symptom structure of acute mania: a factor study of the 24-item Brief Psychiatric Rating Scale in a national sample of patients hospitalized for a manic episode. J Affect Disord 108: 183–189. [DOI] [PubMed] [Google Scholar]
- 57. Cassano GB, Mula M, Rucci P, Miniati M, Frank E, et al. (2009) The structure of lifetime manic-hypomanic spectrum. J Affect Disord 112: 59–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Agrawal A, Nurnberger JI Jr, Lynskey MT (2010) Item response modeling of DSM-IV mania symptoms in two representative US epidemiological samples. Psychol Med 40: 1549–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Berk M, Hallam K, Malhi GS, Henry L, Hasty M, et al. (2010) Evidence and implications for early intervention in bipolar disorder. J Ment Health 19: 113–126. [DOI] [PubMed] [Google Scholar]
- 60. Miklowitz DJ, Schneck CD, Singh MK, Taylor DO, George EL, et al. (2013) Early intervention for symptomatic youth at risk for bipolar disorder: a randomized trial of family-focused therapy. J Am Acad Child Adolesc Psychiatry 52: 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Neslihan Inal-Eiroglu F, Ozerdem A, Miklowitz D, Baykara A, Akay A (2008) Mood and disruptive behavior disorders and symptoms in the offspring of patients with bipolar I disorder. World Psychiatry 7: 110–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Faraone SV, Biederman J, Mennin D, Wozniak J, Spencer T (1997) Attention-deficit hyperactivity disorder with bipolar disorder: a familial subtype? J Am Acad Child Adolesc Psychiatry 36: 1378–1387. [DOI] [PubMed] [Google Scholar]
- 63. Passarotti AM, Sweeney JA, Pavuluri MN (2010) Neural correlates of response inhibition in pediatric bipolar disorder and attention deficit hyperactivity disorder. Psychiatry Res 181: 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Passarotti AM, Sweeney JA, Pavuluri MN (2010) Emotion processing influences working memory circuits in pediatric bipolar disorder and attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49: 1064–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Geller B, Williams M, Zimerman B, Frazier J, Beringer L, et al. (1998) Prepubertal and and early adolescent bipolarity differentiate from ADHD by manic symptoms, grandiose delusions, ultra-rapid or ultradian cycling. J Affect Disord 51: 81–91. [DOI] [PubMed] [Google Scholar]
- 66. Leibenluft E, Rich BA (2008) Pediatric bipolar disorder. Annu Rev Clin Psychol 4: 163–187. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Scree Plot.
(TIF)
Selection of Items for the CBCL-MS.
(DOC)
Representativeness of the TRAILS sample.
(DOC)
Psychometric properties of the CBCL-MS across ages.
(DOC)
Discriminative ability of the CBCL-MS.
(DOC)
Appendix: CBCL-MS (scale and scoring sheet).
(PDF)