Abstract
The authors provide an overview of nasal soft tissue reconstruction and of the senior author's practice. Nasal soft tissue reconstruction is a challenging endeavor as the nose is one of the most prominent and complex facial features. A multitude of surgical repair options exist, which can make the decision-making process unnecessarily complicated. It is advisable that the reconstructive surgeon become facile with a handful of surgical techniques versus trying to master many techniques.
Keywords: nasal reconstruction, Mohs surgery, forehead flap, nasolabial flap, dorsonasal flap, secondary intention, full-thickness skin graft
The nose is one of the most prominent and distinctive features of the face. Its contours are complex, with intersecting concavities and convexities. In addition, the overlying skin of the nose varies in thickness and composition from one area to another. These characteristics impart significant complexity to the nasal soft tissues and make nasal soft tissue reconstruction a formidable, yet enjoyable challenge.
The overwhelming majority of nasal soft tissue defects are secondary to skin cancer excision. Highly susceptible to sun exposure and ultraviolet damage, the nose is the most common site of skin cancer in the head and neck.1,2,3 In the United States, an estimated 225,000 new cases of nasal nonmelanoma skin cancers are diagnosed every year.4 Modern treatment of these cancers involves Mohs histographic tumor excision with subsequent reconstruction by a plastic surgeon. This technique has revolutionized the treatment of skin cancer, resulting in increased cure rates and minimizing the amount of soft tissue excised.5 Despite this more fastidious approach, the resultant soft tissue defect continues to be a significant challenge for the reconstructive surgeon.
Nasal soft tissue reconstruction after Mohs surgery is a challenging endeavor for which a multitude of surgical options exist. In this article, we give a brief overview of 7 years of nasal soft tissue reconstruction performed by the lead author at a single institution and the techniques used for nasal soft tissue reconstruction.
Overview of Senior Author's Practice
The senior author (JFT) has performed over 791 nasal soft tissue reconstructions from 2004 through the first half of 2010 (Table 1 and Fig. 1). Well over 98% of the patients were status post-Mohs resection. The average patient age was 63.5 years. Nasolabial flaps (29%), full-thickness skin grafts (26%), and forehead flaps (20%) made up the vast majority of repair techniques. It should be noted that initially a wide variety of repair options was utilized in the senior author's practice. The number of different reconstruction options per patient has been reduced, reflecting the development of and reliance on “tried and true” techniques. The emphasis on utilizing tried and true techniques may be the greatest value of this presentation. A young surgeon should focus on only a handful of reconstructive techniques and become competent with them. Proficiency with a few techniques is superior to having a superficial understanding of many techniques.
Table 1. Summary of procedures for nasal soft tissue reconstruction from 2004-2010.
| Closure | Bilobed | Dorsal nasal flap | Full-thickness skin graft | Linear closure | Median forehead flap | Nasolabial flap | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 56) | (N = 72) | (N = 204) | (N = 72) | (N = 158) | (N = 229) | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| Year of operation | |||||||||||||
| 2004 | 2 | 3.6 | 8 | 11.1 | 18 | 8.8 | 6 | 8.3 | 16 | 10.2 | 6 | 2.6 | |
| 2005 | 1 | 1.8 | 4 | 5.6 | 15 | 7.4 | 2 | 2.8 | 7 | 4.4 | 20 | 8.7 | |
| 2006 | 1 | 1.8 | 19 | 26.4 | 51 | 25.0 | 5 | 6.9 | 21 | 13.3 | 38 | 16.6 | |
| 2007 | 3 | 5.4 | 11 | 15.3 | 17 | 8.3 | 10 | 13.9 | 25 | 15.8 | 27 | 11.8 | |
| 2008 | 19 | 33.9 | 15 | 20.8 | 43 | 21.1 | 29 | 40.3 | 44 | 27.8 | 69 | 30.1 | |
| 2009 | 19 | 33.9 | 9 | 12.5 | 32 | 15.7 | 12 | 16.7 | 34 | 21.5 | 44 | 19.2 | |
| 2010 | 11 | 19.6 | 6 | 8.3 | 28 | 13.7 | 8 | 11.1 | 11 | 7.0 | 25 | 10.9 | |
| Age (mean) | 60.1 | 65.8 | 60.9 | 59.8 | 67.3 | 67.2 | |||||||
| Sex | Male | 32 | 57.1 | 42 | 58.3 | 82 | 40.2 | 24 | 33.3 | 84 | 53.2 | 103 | 45.0 |
| Female | 24 | 42.9 | 30 | 41.7 | 122 | 59.8 | 48 | 66.7 | 74 | 46.8 | 126 | 55.0 | |
| Location of defect | |||||||||||||
| Ala | 16 | 28.6 | 0 | 0.0 | 52 | 25.5 | 5 | 6.9 | 22 | 13.9 | 102 | 44.7 | |
| Sidewall | 14 | 25.0 | 2 | 2.8 | 37 | 18.1 | 18 | 25.0 | 0 | 0.0 | 10 | 4.4 | |
| Tip | 6 | 10.7 | 10 | 13.9 | 21 | 10.3 | 11 | 15.3 | 18 | 11.4 | 30 | 13.2 | |
| Dorsum | 5 | 8.9 | 35 | 48.6 | 35 | 17.2 | 19 | 26.4 | 5 | 3.2 | 0 | 0.0 | |
| Columella | 0 | 0.0 | 0 | 0.0 | 2 | 1.0 | 1 | 1.4 | 0 | 0.0 | 0 | 0.0 | |
| Soft Triangle | 0 | 0.0 | 0 | 0.0 | 3 | 1.5 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | |
| Heminasal | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 31 | 19.6 | 0 | 0.0 | |
| Combined | S & A | 7 | 12.5 | 0 | 0.0 | 11 | 5.4 | 0 | 0.0 | 9 | 5.7 | 16 | 7.0 |
| T & A | 4 | 7.1 | 0 | 0.0 | 11 | 5.4 | 1 | 1.4 | 18 | 11.4 | 32 | 14.0 | |
| T & S | 2 | 3.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 0.9 | |
| D & S | 1 | 1.8 | 8 | 11.1 | 14 | 6.9 | 9 | 12.5 | 8 | 5.1 | 2 | 0.9 | |
| D & T | 0 | 0.0 | 14 | 19.4 | 4 | 2.0 | 3 | 4.2 | 14 | 8.9 | 8 | 3.5 | |
| C & S | 0 | 0.0 | 0 | 0.0 | 5 | 2.4 | 1 | 1.4 | 4 | 2.5 | 0 | 0.0 | |
| A & D | 0 | 0.0 | 0 | 0.0 | 2 | 1.0 | 0 | 0.0 | 3 | 1.9 | 0 | 0.0 | |
| St & C | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | |
| St & A | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | |
| H & C | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 1.3 | 0 | 0.0 | |
| T & C | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.4 | 2 | 1.3 | 1 | 0.4 | |
| A & C | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.4 | 7 | 4.4 | 9 | 3.9 | |
| T & St | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 2 | 0.9 | |
| A & S & C | 0 | 0.0 | 1 | 1.4 | 0 | 0.0 | 0 | 0.0 | 3 | 1.9 | 0 | 0.0 | |
| A & T & S | 1 | 1.8 | 0 | 0.0 | 1 | 0.5 | 0 | 0.0 | 2 | 1.3 | 6 | 2.6 | |
| D & T & A | 0 | 0.0 | 2 | 2.8 | 1 | 0.5 | 1 | 1.4 | 1 | 0.6 | 1 | 0.4 | |
| T & D & S | 0 | 0.0 | 0 | 0.0 | 4 | 2.0 | 1 | 1.4 | 5 | 3.2 | 3 | 1.3 | |
| D & S & A | 0 | 0.0 | 0 | 0.0 | 1 | 0.5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |
| S & C & T | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | |
| C & T & A | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | |
| T & A & St | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | |
| C & St & A | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | |
| A & T & St & C | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | |
Abbreviations: S, sidewall; A, ala; T, tip; St, soft triangle; D, dorsum, C, columella; H, heminasal.
Fig. 1.
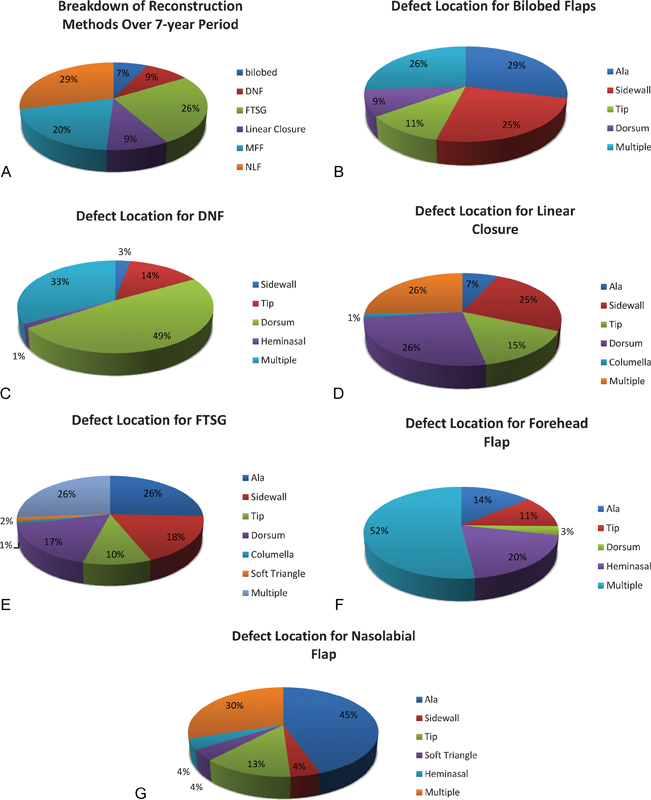
Reconstruction types broken down by defect location. (A) Overview of reconstruction techniques utilized by senior author. (B) Bilobed flap. (C) Dorsal nasal flap (DNF). (D) Linear closure. (E) Full-thickness skin graft (FTSG). (F) Forehead flap. (G) Nasolabial flap.
Currently, the senior author's practice is essentially all at outpatient facilities. Mohs patients are seen the same or next day. The great majority of these patients' procedures are done under propofol intravenous (IV) sedation and local infiltration, with the exception of forehead flaps, which require general anesthesia for the initial flap. The patients are sent home that day.
To optimize treatment for Mohs surgical resection patients, it is important to understand that these patients are different than most plastic surgery patients because they are not seen by the surgeon beforehand. They are seen for the first time by the plastic surgeon after they have already had their resection. As such, it is imperative that the surgeon be able to rapidly assess both their current medical condition and expectations to formulate an operative plan that is suitable for that patient's health, expectations, and lifestyle. Obviously, a multistage procedure, despite it potentially offering superior aesthetic results, may not be the most appropriate reconstructive option for some patients. For example, if a patient is an elderly smoker with care issues, a complex multistage procedure may not be suitable. A single stage procedure, such as linear closure or skin graft, may be the best option in this case. It is important to individualize the reconstruction for each patient and involve the patient in the decision-making process.
During the preoperative discussion, liberal use of photographs and rapid assessment of the patient's expectations are used. An accessible collection of before and after photographs, including images prior to division and inset for multistage reconstructions, is an excellent way to give the patient a realistic idea of the reconstructive process. Attentive postoperative care with frequent clinic visits is needed and will help maintain a low level of complication rates from surgery.
For nasal reconstruction after Mohs surgery, it is important that the anesthesiologist realizes that these patients are undergoing a minimal procedure from a tissue transfer and fluid shift perspective. Local anesthesia and mild sedation provide more than adequate comfort for the patient during the procedure. There is little need for any undue preoperative testing or preparation, and patients tolerate the procedure well.
To fully understand the preoperative assessment, it is important to mention anticoagulation. The majority of nasal reconstruction patients are elderly, and in following commonly accepted practices in dermatology surgery, no effort is made to change their anticoagulation status prior to surgery.6,7 It is our experience that nasal reconstruction can be done safely in patients fully anticoagulated. The one exception to this is a patient that is on clopidogrel. We will no longer undertake forehead flaps on patients currently taking clopidogrel as the bleeding is significant; in our experience, this precludes a safe procedure.
Nasal Reconstruction
As nasal reconstruction is sometimes considered the “flagship” procedure in facial reconstruction, numerous textbooks and articles have been written regarding surgical techniques. To a starting reconstructive surgeon, this can be confusing both in procedure selection and execution. It is important to realize that there are really only four general categories of techniques for nasal reconstruction and deciding upon the appropriate reconstruction starts with these very basic principles.
The four techniques are
Allowing the defect to heal by secondary intention or with assisted wound healing
Skin grafting
Nasal skin rearrangement
Nasolabial and forehead flaps
Seemingly narrow, the above four categories are not an oversimplification. They contain within them all the principles a practicing surgeon would need to reconstruct the full spectrum of nasal defects. The pluses and minuses of the individual techniques and their indications will be discussed throughout this issue.
It is important to comment on the subunit principle versus the defect-only principle of nasal reconstruction and these principles' application in guiding nasal reconstruction. The subunit principle, popularized by Burget and Menick in 1985, divides the nose into eight subunits: the ala, sidewalls, soft triangles, tip, and dorsum. The underlying idea was that scars are well hidden at the borders of the subunits given the interplay of light and shadows at the junctions of these subunits. As a result, Burget and Menick advocated excising the remaining nasal subunit if the defect involved greater than 50% of a subunit.8 They argued that this technique helped prevent a patchwork appearance and conspicuous skin bulging as a result of the replaced soft tissue. However, defect-only reconstruction has been shown to be effective for nasal reconstruction in many cases, in particular for lower third defects.9,10 As in many things in plastic surgery, the practicing surgeon need not be dogmatic about defect-only or subunit reconstruction, but rather should be facile with both. Both techniques have their utility; it is up to the surgeon to decide their best application.
Secondary Intention
Secondary intention or assisted wound healing should be the starting point for decision making during Mohs nasal reconstruction. Concave surfaces and small defects are better suited for healing by secondary intention.11,12 In our experience, allowing wounds to heal secondarily yields a satisfactory result in only a very small subset of patients. These wounds heal by contraction of the wound edges and scar deposition over the remaining defect, often resulting in a flat, shiny, depressed area (Fig. 2). Although wound closure is achieved, the risk of retraction, irreversible alar notching, and facial asymmetry typically makes this option unpredictable and unacceptable. Although in its infancy, the senior author strongly believes that healing by secondary intention assisted by acellular dermal matrices (ADM) will bear a very significant role in the next generation of plastic surgeons' practices. Our own experience with ADM and secondary intention is limited, but with careful patient selection, the proper implementation of these products has yielded very satisfactory results. As this technique evolves and the products improve, it will play a larger role in wound healing, in particular in a patient population that is elderly and intolerant of surgical procedures.
Fig. 2.

A nasal tip defect allowed to heal by secondary intention at 6 months, demonstrating a depressed scar.
Skin Grafting
Skin grafting, long a mainstay of dermatologists, is sometimes considered a secondary or inferior technique by plastic surgeons. However, it has a very strong role in safe aesthetic nasal reconstruction. In many ways, skin grafting on the upper two-thirds of the nose is a preferred technique. A flat featureless nasal sidewall and nasal dorsum are well suited for color-matched full-thickness skin grafts, and is really the reconstruction method of choice for defects less than 2 cm. The ease of design, harvest, and inset make full-thickness skin grafts an approachable option, even for the young surgeon. The preauricular and forehead donor sites allow for simple closure and color matching (Fig. 3). Avoidance of hair-bearing regions is paramount. Even though little has been written about using full-thickness skin grafts in lower third reconstruction in the plastic surgery literature, it is widely accepted in the dermatologic literature and is well practiced. In carefully selected patients, full-thickness skin grafting of the upper two-thirds, or the lower third with appropriate selection of patient and donor site, can provide a superior result and needs to be in the plastic surgeon's armamentarium.
Fig. 3.

(A) Pre-auricular donor site. (B) Forehead donor site.
Nasal Skin Rearrangement
This technique includes local nasal flaps, such as the bilobed, dorsal nasal, note, V-Y advancement, and banner flaps to name a few. These have a very wide role in nasal reconstruction. Numerous articles have been written on the various local flaps and familiarity with these is a must for all plastic surgeons. With appropriate patient selection, local skin rearrangement can be the ideal reconstruction technique. However, these flaps, when used inappropriately, have the tendency to distort the nose and lead to contour irregularities, necessitating revision. Despite the literally hundreds of descriptions of local flaps, the practicing plastic surgeon actively involved in nasal reconstruction only needs to master fewer than a half dozen local flaps for exceptional aesthetic results. Ultimately, local flaps have a limited role in nasal reconstruction.
Nasolabial and Forehead Flaps
Tissue transfer or interpolated flaps truly are the gold standard in nasal reconstruction. The reconstructive surgeon should become adept at performing a forehead flap. This repair technique is safe, reliable, and repeatable with predictable donor site morbidity. Similar skin characteristics and quantity of soft tissue provided make the forehead flap a robust reconstructive option. The nasolabial flap is an excellent repair technique for the lower third of the nose, with qualities specifically suited for reconstruction of the ala. Use of this technique has been expanded to include reconstruction of the nasal tip, dorsum, soft triangle, and partial alar defects. Although these flaps require multiple stages and can appear objectionable to the patient after the primary procedure, they often result in superior aesthetic results (Figs. 4 and 5). It is prudent that the surgeon become proficient at performing these two flaps. It cannot be emphasized enough, but reliance on a few tried and true techniques will improve the surgeon's overall results as his familiarity with the technique and its execution improves with practice.
Fig. 4.

Forehead flap. (A) Preoperative defect. (B) 3-weeks postoperative. (C) 12-months postoperative.
Fig. 5.

Nasolabial flap. (A) Preoperative defect. (B) 4-months status post division and inset.
Postoperative Care
It must be noted that postoperative care for patients undergoing nasal reconstruction is extremely important. Dermabrasion down to punctuate bleeding is recommended for all scars, donor sites, and defects, at 6 weeks postoperatively to smooth the skin contour, improve pigmentation, and blend the scar into the surrounding tissues. Ample sunscreen should be applied to all scars for 12 months. Any reddening of the scar as a result of sun exposure can ruin a perfectly good nasal reconstruction. Silicon sheeting is used at our institution in all nasal soft tissue reconstruction to improve scar appearance. Finally, it is very important that the operating surgeon interested in nasal reconstruction maintain an accurate photographic database and as his technique is refined, frequently refer back to gauge his evolution in surgical maturity.
Conclusion
Nasal soft tissue reconstruction can be both a challenging and gratifying procedure for the plastic surgeon. Numerous techniques exist for reconstruction, which may confuse the surgeon whose practice is not solely focused on nasal reconstruction. By focusing on a few tried and true techniques and mastering these, a surgeon will rapidly improve his results. Additionally, as more cases have been accumulated by the senior author, the techniques have evolved often to less intervention with equally superior results. It is imperative to note that attentive postoperative care is necessary to ensure high-quality results.
References
- 1.Evans G R, Williams J Z, Ainslie N B. Cutaneous nasal malignancies: is primary reconstruction safe? Head Neck. 1997;19(3):182–187. doi: 10.1002/(sici)1097-0347(199705)19:3<182::aid-hed3>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 2.Preston D S, Stern R S. Nonmelanoma cancers of the skin. N Engl J Med. 1992;327(23):1649–1662. doi: 10.1056/NEJM199212033272307. [DOI] [PubMed] [Google Scholar]
- 3.Diepgen T L, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002;146 61:1–6. doi: 10.1046/j.1365-2133.146.s61.2.x. [DOI] [PubMed] [Google Scholar]
- 4.Moolenburgh S E, McLennan L, Levendag P C. et al. Nasal reconstruction after malignant tumor resection: an algorithm for treatment. Plast Reconstr Surg. 2010;126(1):97–105. doi: 10.1097/PRS.0b013e3181da872e. [DOI] [PubMed] [Google Scholar]
- 5.Mohs F E. Chemosurgery for the microscopically controlled excision of skin cancer. J Surg Oncol. 1971;3(3):257–267. doi: 10.1002/jso.2930030307. [DOI] [PubMed] [Google Scholar]
- 6.Kirkorian A Y, Moore B L, Siskind J, Marmur E S. Perioperative management of anticoagulant therapy during cutaneous surgery: 2005 survey of Mohs surgeons. Dermatol Surg. 2007;33(10):1189–1197. doi: 10.1111/j.1524-4725.2007.33253.x. [DOI] [PubMed] [Google Scholar]
- 7.Khalifeh M R, Redett R J. The management of patients on anticoagulants prior to cutaneous surgery: case report of a thromboembolic complication, review of the literature, and evidence-based recommendations. Plast Reconstr Surg. 2006;118(5):110e–117e. doi: 10.1097/01.prs.0000221114.01290.85. [DOI] [PubMed] [Google Scholar]
- 8.Burget G C, Menick F J. The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76(2):239–247. doi: 10.1097/00006534-198508000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Rohrich R J Griffin J R Ansari M Beran S J Potter J K Nasal reconstruction—beyond aesthetic subunits: a 15-year review of 1334 cases Plast Reconstr Surg 200411461405–1416., discussion 1417-1419 [DOI] [PubMed] [Google Scholar]
- 10.McCluskey P D, Constantine F C, Thornton J F. Lower third nasal reconstruction: when is skin grafting an appropriate option? Plast Reconstr Surg. 2009;124(3):826–835. doi: 10.1097/PRS.0b013e3181b03749. [DOI] [PubMed] [Google Scholar]
- 11.Zitelli J A. Secondary intention healing: an alternative to surgical repair. Clin Dermatol. 1984;2(3):92–106. doi: 10.1016/0738-081x(84)90031-2. [DOI] [PubMed] [Google Scholar]
- 12.van der Eerden P A, Lohuis P JFM, Hart A AM, Mulder W C, Vuyk H. Secondary intention healing after excision of nonmelanoma skin cancer of the head and neck: statistical evaluation of prognostic values of wound characteristics and final cosmetic results. Plast Reconstr Surg. 2008;122(6):1747–1755. doi: 10.1097/PRS.0b013e31818a9aaa. [DOI] [PubMed] [Google Scholar]


