Abstract
Immunology has now developed into an independent discipline in medicine which covers not only germ infection which is related to immunity solely but also covers a lot of non-infectious diseases such as autoimmune disease, allergies, and others. Therefore, “The Immune Mechanism: “A Double-Edged Sword” means that the immune mechanism (consisted of antibody mediated mechanism and T cell mediated mechanism), just like one edge playing the role of giving benefit (immunity) as it destroys the agent of infection, and another one can be detrimental as it will cause tissue/cell damages and then give rise to immune diseases (immunopathology). Now, the prevalence of these immune diseases is on the rise and has become a new challenge to our country towards developed country in 2020. Therefore, we have to make ample preparation (laboratory facilities/services, main power, and research) from now on in order to face the problems and challenges.
Keywords: immune response, tuberculosis, vaccine, SLE
Introduction
We live in an environment with numerous substances or agents which may be detrimental towards our body such as bacteria, viruses, and other pathogens. For example, the air that we breathe contains germs which may cause diseases such as tuberculosis, H1N1, and others. Likewise, the water which we drink and the food which we take may also contain germs which may cause diseases such as typhoid, cholera and others. However, our bodies have been equipped with a defence mechanism which can prevent infection. At the same time our body’s defence mechanism also functions to control the development of cancerous cells.
There are two levels in the body’s defence system which are the innate immunity and the adaptive immunity (1–3). The innate immunity is also known as the first defence barrier exists in order to prevent infection. For example, our skin is the anatomy blockade which needs to be penetrated by infectious germs before entering into the body. Germs may infect through bruises or fire burns. In addition, acid in the stomach helps inhibit growth or kill bacteria contaminated in food or drinks. Tears also contain enzymes which can prevent infection. However, there are infectious germs that can overcome the first defence barrier and try attacking our bodies. As mentioned earlier, in the second level, it involves another unique body defence system which is the adaptive immunity (2,4). The maturation process of lymphocyte takes place in the thymus and the bone marrow, while the activation of lymphocyte is in spleen and lymph nodes. The germs that enter our bodies will stimulate the lymphocytes in the spleen and lymph nodes. This is an immune reaction which produces immunity with the production of antibodies and cytotoxic T cell. During the immune response, mediators such as cytokines are also produced. The adaptive immunity is divided into two types: antibody mediated immunity and cell immunity (mediated by cytotoxic T cells) (1–4). The immune mechanism produced may kill or destroy germs and thus, giving us protection/immunity.
Without an immune system which offers immunity, we are exposed to infections (as well as the development of cancer cells). Therefore, the immune system which gives immunity/the specific defence is beneficial for humans in fighting infections. Further, discussion on immune mechanism which destroys infectious agents, will be focused on tuberculosis in light of our research carried out so far.
What is Tuberculosis (TB)?
Tuberculosis (TB) is an infectious disease caused by bacterial infection known as Mycobacterium tuberculosis. This bacterium generally spreads through the breathing system and infects the lungs. The immunity developed may control the bacterial infection in the body without any clinical symptoms.
Only a little number of individuals are exposed to the TB bacteria develop pulmonary TB (active tuberculosis) which shows symptoms of acute primary TB such as prolonged coughing (5). Patients who show symptoms of acute primary TB and left untreated may enable the TB bacteria to spread to other organs such as bones, kidneys, the brain, and other vital organs. This phase is known as miliary or extra-pulmonary TB infection. Active TB patients will also be controlled by the formation of immunity. Although they are not showing the symptoms, the TB bacterium is still in the body and this is also referred to as latent TB infection. If their immunity level is weak, the latent TB infection may be active again and show symptoms of TB (5).
Immunity/Immune Mechanism towards TB
The TB bacteria enter the body through breathing and finally attack the lungs (6). There are immune cells such as lymphocytes and macrophages in the lungs which are stimulated by the TB infection.The immune response to TB infection include the production of antibodies, cytotoxic T cells activation, and macrophages (7–10). However, there are ample of research reports show, antibodies produced towards TB bacteria are unable to control infections, because the bacteria can live in cells undetected by the antibodies (5). Therefore, the TB infection control depends on the immunity cells (cytotoxic T cells and the most active macrophages) (7,10). This was proven as an active TB patient has high antibody level but has low T cell activity and macrophages. TB bacteria may live and multiply in normal macrophages, but as the macrophages are activated by the cytokines, it has the ability to kill the TB bacteria. Meanwhile, the active cytotoxic T cell can cause lysis to the cells infected by the TB bacteria and then causes the bacteria to be killed by the most active macrophages (7,10). However, if the immune system failed, an uncontrolled TB infection may take place.
What is the Importance of TB Research?
Although TB was once controlled with the existence of vaccines and medication, this disease is now becoming more serious epidemic worldwide. TB cases are reported to be higher and alarming. The World Health Organization Report (WHO) estimated that 1/3 of the world population has been infected with the TB bacteria and more than 20 million infected are cases of active TB (11,12). Apart from that, the TB bacteria are also the main cause of death among human immunodeficiency virus (HIV) patients (13).
Next, some of the world population has been infected with the TB strains which are resistant to various antibiotics (Multi-Drug Resistance-MDR) (14,15). These strains cannot be destroyed by typical treatment, but it needs the combination of suitable antibiotics. Therefore, treatment success rates using a combination of drugs for MDR TB infection strain is low or it is difficult to be cured, and thus, causing high mortality rates. Hence, prevention using vaccination method is one of the best ways to overcome this problem. The production of new vaccines which are more effective should be carried out promptly.
Vaccination Principle
Each time an infection takes place as mentioned above, our immune system will be stimulated to produce immunity. This means, because of the infection, the symptoms occur first while the immune system produces immunity, and later demolishes the agent of infection. This is subjected to the status and the ability of our immune system. Our immune system can also be stimulated in an artificial way or it can be created without any symptom of diseases. This method is known as the immunization or vaccination using the vaccine. Vaccines are made up of certain infectious germs which are intended to be controlled such as weakened germs (can no longer cause disease) or certain components from the germs which are safe for use (1,4). Unlike natural infection, vaccination can stimulate the immune system without any symptoms of disease but can still produce antibodies and cytotoxic T cells that destroy infection agents which have been discussed earlier. This means, with vaccination, our bodies are equipped with the immunity, and if the infection took place, the immune system will rapidly be stimulated to produce immunity which is stronger and faster in destroying the germ infection more effectively (1,4). Therefore, vaccination serves the purpose of the wise saying, ‘prevention is better than cure’.
The vaccination method has been used in order to prevent certain diseases such as measles, poliomilitis, hepatitits, TB and others. This approach has been a focal point for the research up till today in producing new vaccines which are more effective, and vaccines for diseases which are yet to be prevented. Our achievements in developing new forms of vaccines for TB will be discussed further based on the researches which have been carried for more than 15 years.
Research in Relations to Vaccine Candidates for TB
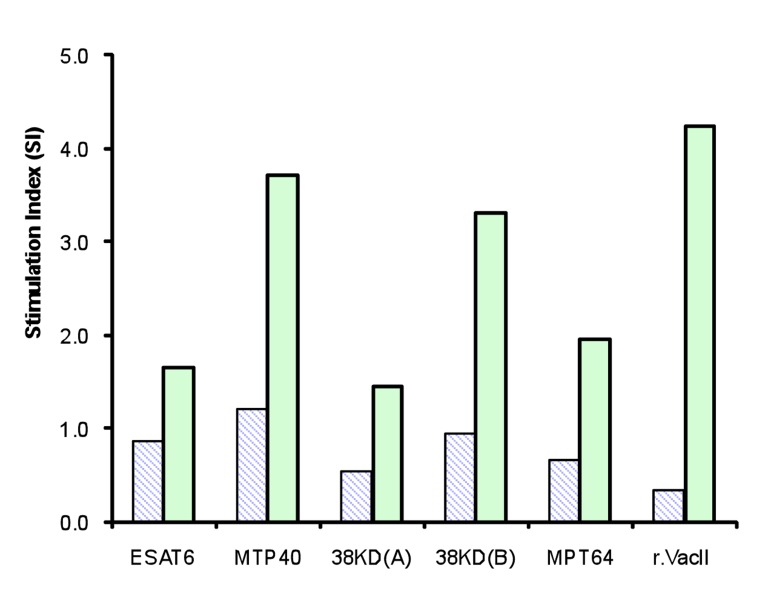
More than a decade ago, a new vaccine named Bacillus Calmette-Guerin (BCG) has been produced to prevent TB (16). This vaccine is still used to this day. The BCG vaccine is given to newborn babies to prevent TB infection. However, its effectiveness used in certain countries is questionable (17). This is based on the increment of TB cases and the problem in controlling the spread of the TB bacteria. Therefore, the production of a better or alternative TB vaccine candidates which are more effective is now being carried out extensively all over the world (18–20). Researchers use numerous methods of approach in developing TB vaccines based on deoxyribonucleic acid (DNA) technology (21). The technique used involves the development of synthetic genes of various epitopes and gene cloning (19). The epitopes TB bacteria have the potential to stimulate cellular immunity were identified and selected. Based on the epitope combination, the synthetic gene is generated by using the assembly PCR technique. Our studies have successfully produced new synthetic TB genes known as VacII and VacIII which has different combination of epitopes. Next, these synthetic genes are cloned into certain plasmid vectors to produce vaccine candidates known as DNA vaccine and surface display vaccine (22). In order to determine if the produced vaccine can stimulate lymphocyte or not, these vaccine were tested on mice model of vaccination. The lymphocyte responses and the production of cytokines from the group of mice that have been vaccinated and the control group (the blank vector) were measured and compared. For an example, our results show that lymphocyte stimulation index (SI) from the mice in DNA vaccination group was higher compared to the SI from the mice in the control group (Figure 1). A similar result were also obtained for surface display vaccination which shows SI from the vaccinated mice which was higher compared to the SI from the control mice (Figure 2).
Figure 1:
Lymphocyte Stimulation Index (SI) from mice vaccinated with DNA vaccine (the red bar) compared with control mice (the green bar) after stimulation with various epitopes of M. tuberculosis at 5 ug/mL and 10 ug/mL.
Figure 2:
The lymphocyte stimulation index from the mice with surface display vaccination (the green bar) compared with the control mice (the striped bar) after stimulation with various epitopes of M. tuberculosis and recombinant vacII proteins.
As a general conclusion, our research results show newly developed TB vaccine candidates are immunogenic which is able to stimulate the mice’s immune system. However, the initial finding needs further research to evaluate the effectiveness of the vaccines which were developed. A challenge or protection study needs to be carried out in order to determine the efficacy of the vaccine. Next the safety study needs also to be done as well before the extensive research which involves human or the clinical trial to be carried out.
The Contribution and the Implication of TB Candidate Vaccine Research and Development
The outcome of this research is the production of new vaccine candidates which are very much potential to be developed further as alternative vaccines which may prevent TB infection. At least the vaccines, can be utilized with the existing BCG vaccine in order to prevent TB disease more effectively. If this can be done, it can give an important impact because it will increase the health status of the world population and indirectly lessen the burden of the health service costs which are related to management and control of TB. Furthermore, this research has also developed DNA technology method in vaccine production and this makes Universiti Sains Malaysia (USM) as the research hub and training for the related field. In addition, TB research currently is one of the thrust areas especially in USM with its group of unique researchers.
Diseases Mediated by Immune Mechanism (Immunopathology)
Back to the topic of discussion which is the ‘Immune Mechanism: “A Double-Edged Sword”, it has been further elaborated that the immune mechanism (humoral immunity and cellular immunity) can benefit us as our defence towards the infection by destroying the infectious agents (the same mechanism involved in the controlling of the spread of cancer cells). The immune mechanism can be produced when the infectious agents attacks our body or going through vaccination. For example, vaccine for TB infection is being developed to boost the immune system in mice as an initial research towards the effort in preventing TB soon.
However, the same immune mechanism (antibodies and cytotoxic T cells) which were discussed earlier, in certain situations can cause the destruction to the cells or tissues in our body. In a normal condition, the immune response does not happen to the cells or tissues in our body but, if there is interference or disorders towards the immune system, and other environmental factors, the immune mechanism produced can destroy our own cells and tissues. In return, there will be a prevalent of other diseases such as immune diseases (diseases mediated by immune mechanism) such as autoimmune diseases, allergic diseases, and others. This field is known as immunopathology. It is the adverse effects from the immune mechanism compared to the beneficial immunity mentioned earlier.
Immune mediated tissue damages
The immune mechanism which causes the damage of cells or tissues is divided into four types known as the hypersensitivity reaction (1,2). Hypersensitivity reaction Type I include the production of antibodies (IgE) towards environmental substances such as pollens, home dust, food, and others which are known as allergens. The pathology effect which takes place is as a result of mast cell activities that secretes enzymes and therefore, causes muscle contraction, overproduction of mucus and finally causing clinical symptoms such as allergic diseases. An example of an allergic disease is asthma, allergic rhinitis (runny nose), and others.
Hypersensitivity reaction Type II involves antibodies (IgG & IgM) towards surface-bound proteins, or cell membranes, or our body tissue. The pathology effects which happen include lysis and cell destruction. Example diseases are such as autoimmune haemolytic anaemia (AIHA), myasthenia gravis (MG), autoimmune diabetes (Type 1) and others. In AIHA, red blood cells lysis due to autoantibodies against the red blood cells takes place causing anaemia. In MG, there are autoantibodies which destroys/blocks acetylcholine receptors and therefore causing muscle-nerve weakening. Meanwhile in autoimmune diabetes, there are autoantibodies that destroys insulin hormone production cells and therefore, causing symptoms of diabetes (1,2).
Hypersensitivity reaction Type III involves antibody production towards soluble protein in the body and thus, circulating immune complexes (CIC) circulate in our blood system. CIC may precipitate in certain organs such as kidney, joints, and others. At the base of this precipitation, a demolishing or tissue lysis may occur. For example, glomerulonephritis in the glomerulus of the kidney or arthritis of the joints. Lastly, hypersensitivity reaction Type IV does not involve antibody but on the contrary involves the activities of cytotoxic T cells and activated macrophages which destroy our own cell and body tissue. For example, in the dermato-myositis disease, lysis happens to the muscle by specific cytotoxic T cells towards muscle cells which weaken the function of the muscle. In one immune disease, more than one type of hypersensitivity reactions which has been mentioned earlier can be involved in tissue damage and this will cause various symptoms of the disease (2).
Next, the treatment for the immune disease depends on the immune mechanism involves in the tissue damage and symptoms inflicted with it. Generally, majority of the immune disease are autoimmune disease in which the production of autoantibody and autoreactive T cells damage patient’s cells or tissue. Among autoimmune disease in this country, Systemic Lupus Erythematosus (SLE) disease shows a high prevalence. Therefore, this disease is a research niche in the Immunology Department, School of Medical Science.
Eritematosus Lupus Systemic (SLE)
SLE is an autoimmune disease, with prolonged chronic inflammation which involves numerous organs. Among the main symptoms of SLE include rashes known as butterfly rashes in the face (rashes which resembles butterflies). Rashes may also present in body parts exposed to sunlight such as the neck and arms as patients develop sensitive skin towards sunlight (23). SLE’s main symptoms are serious with joint arthritis and renal disruption (glomerulonephritis) (24–26). Apart from that, it may also damage the brain, heart, lungs, and the blood circulatory system. The autoantibody profile which include anti-nuclear antibody (ANA), anti-ds DNA antibody have been shown to have an association with clinical manifestations in Malay SLE patients (27).
SLE is hard to detect in the initial prevalence because of its ambiguous symptoms. This is because the early lupus symptoms were not specific such as lethargy, fever, joint pain and hair loss (25). SLE’s aetiology is also not clear and understandable, but it was believed to involve a lot of factor such as descent, viral infection, sexual hormones, and environmental factor. The reported prevalence of SLE in Malaysia: 43 in 100 000 populations of the Chinese show the highest prevalence (28–30). Next, women are more inclined towards contracting it compared to men, and this may be related to hormonal factor (28,31). Age wise, SLE is reported to inflict as early as 10 to 50 years of age (32). SLE is incurable but it can be treated and controlled. Thus, SLE patients need longer treatment. Patients will also find themselves recuperating after treatment but it can also recur and it needs repeated treatment by specialists in order to make sure the target organs are not affected. A few research projects related to SLE have been carried out by lecturers in our Department of Immunology.
The Direction and Challenge of Immunology in the Future
Although infectious diseases such as TB, dengue, cholera, typhoid, and malaria is the main health issue in Malaysia, immune diseases still prevalent as faced by developed countries today. Therefore, we cannot underestimate immune disease problems as it needs thorough preparation to face it.
The number of clinical tests carried out samples from patients with immune disease in the Hospital USM is also increasing. Since the beginning, clinical test in the Department of Immunology, USM has focused on immune diseases such as tests for various autoantibodies, IgE measurement, immunophenotyping of various B & T cells sub-populations and the determination of related cell functions. Therefore, serological tests for infectious diseases have long been carried out by the Medical Microbiology Laboratory. In line with future aims, sufficient and compatible equipments should be provided in this focus field such as flow cytometry, nephelometer, chemiluminometer and fluorescent microscope. As it is, competent and trained medical laboratory technologists needs to be equipped sufficiently.
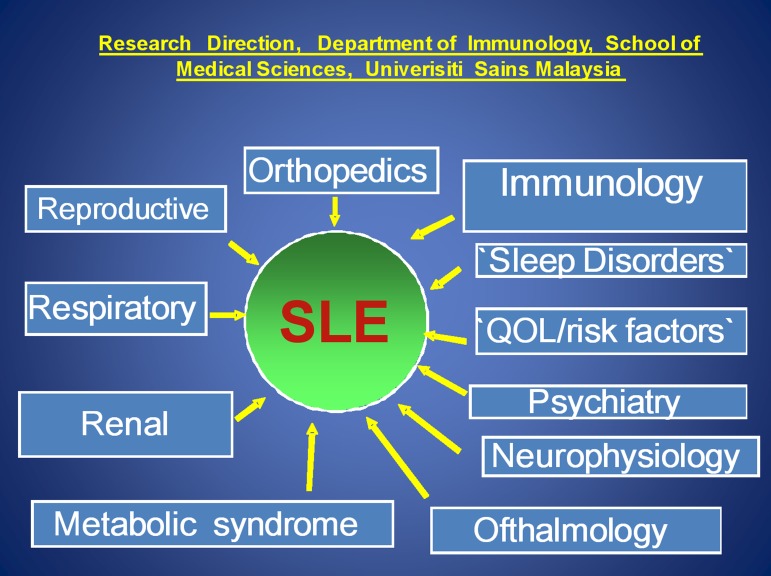
Immunology started with the medical microbiology discipline but now has expanded significantly into other fields or disciplines such as immunochemistry, immunohistochemistry, immunohaematology, immunopharmacology, reproductive immunology, immunoendocrinology, neuroimmunology and rheumatology. In conjuction with the development, there is a need for efficient and accurate treatment for immune diseases which also needs an addition of clinical immunology specialists. In order to encourage more specialists into this field, there is a need to create post for clinical immunologists for their career path. This niche of research in the Immunology Department, USM is also focusing on the same disease. Research for immune diseases such as SLE, allergies, and the likes of it must use cluster/multi-disciplinary. Suggested model for future direction of SLE research which include pathophysiology of the disease involving various disciplines and approaches is shown in Figure 3. The suggested model is based on the SLE disease attributes which cause damage to multiple organs or body systems such as renal system, respiratory system, psychiatry, orthopaedic, ophthalmology and others.
Figure 3:
Suggested model for future direction of SLE research which include pathophysiology of the disease involving various disciplines.
Acknowledgments
I thank Zainul F Zainuddin, Kwai-Lin Thong, Chee-Mun Fang and the staff of Department of Immunology, School of Medical Sciences, USM for the discussions and technical assistance afforded.
Footnotes
Conflict of interest
None.
Funds
The study described herein is partly funded by the Malaysian IRPA Grant (No. 36-02-03-6004).
References
- 1.Stites DP, Terr AI, Parslow TG. 8th ed. Los Altos (CA): A lange Medical Book; 1994. Basic & Clinical Immunology. [Google Scholar]
- 2.Male D, Brostoff J, Roth DB, Roitt IM. 7th ed. St Louis (MO): Mosby Elsevier; 2006. Immunology. [Google Scholar]
- 3.Klaus DE. 2nd ed. United States (US): Wiley & Son Publication; 2009. Immunology: understanding the immune system. [Google Scholar]
- 4.Janeway C, Paul T, Mark W, Mark S. 5th ed. New York (NY) and London (UK): Garlang Science; 2001. Immunobiology. [Google Scholar]
- 5.Flynn JL, Chan J. Tuberculosis: latency and reactivation. Infect Immun. 2001;69(7):4195–4201. doi: 10.1128/IAI.69.7.4195-4201.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bermudez LE, Goodman J. Mycobacterium tuberculosis invades and replicates within type II alveolar cells. Infect Immun. 1996;64(4):1400–1406. doi: 10.1128/iai.64.4.1400-1406.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaufmann SH. Immunity to intracellular microbial pathogens. Immunol Today. 1995;16(7):338–342. doi: 10.1016/0167-5699(95)80151-0. [DOI] [PubMed] [Google Scholar]
- 8.Andersen P. Host responses and antigens involved in protective immunity to Mycobacterium tuberculosis. Scand J Immunol. 1997;45(2):115–131. doi: 10.1046/j.1365-3083.1997.d01-380.x. [DOI] [PubMed] [Google Scholar]
- 9.Flynn JL. Immunology of tuberculosis and implications in vaccine development. Tuberculosis Edin. 2004;84(1–2):93–101. doi: 10.1016/j.tube.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Cho S, Mehra V, Thoma-Uszynski S, Stenger S, Serbina N, Mazzaccaro RJ, et al. Antimicrobial activity of MHC class I-restricted CD8+ T cells in human tuberculosis. Proc Natl Acad Sci USA. 2000;97(22):12210–12215. doi: 10.1073/pnas.210391497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reichman LB. Tuberculosis elimination - what’s to stop? Int J Tuberc Lung Dis. 1997;1(1):3–11. [PubMed] [Google Scholar]
- 12.Geneva (DE): World Health Organization; 2009. Global tuberculosis control surveillance, planning, financing. WHO report. Unpublished document WHO/TB/2002.287. [Google Scholar]
- 13.Frieden TR, Sterling TR, Munsiff SS, Watt CJ, Dye C. Tuberculosis. Lancet. 2003;362(9387):887–899. doi: 10.1016/S0140-6736(03)14333-4. [DOI] [PubMed] [Google Scholar]
- 14.Hemvani N, Chitnis DS, Bhatia GC, Sharma N. Drug resistance among tubercle bacilli from pulmonary tuberculosis cases in central India. Indian J Med Sci. 2002;55(7):382–392. [PubMed] [Google Scholar]
- 15.Campos PE, Suarez PG, Sanchez J, Zavala D, Arevalo J, Ticona E, et al. Multidrug-resistant Mycobacterium tuberculosis in HIV-infected persons, Peru. Emerg Infect Dis. 2003;9(12):1571–1578. doi: 10.3201/eid0912.020731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson P, Doherty TM. The success and failure of BCG – implications for a novel tuberculosis vaccine. Nat Rev Immunol. 2005;3:3656–3662. doi: 10.1038/nrmicro1211. [DOI] [PubMed] [Google Scholar]
- 17.Fine P. Variation in protection by BCG: implications of and for heterologous immunity. Lancet. 1995;346(8986):1339–1345. doi: 10.1016/s0140-6736(95)92348-9. [DOI] [PubMed] [Google Scholar]
- 18.Abou-Zeid C, Gares MP, Inwald J, Janssen R, Zhang Y, Young DB, et al. Induction of a type 1 immune response to a recombinant antigen from Mycobacterium tuberculosis expressed in Mycobacterium vaccae. Infect Immun. 1997;65(5):1856–1862. doi: 10.1128/iai.65.5.1856-1862.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agustine NF, Mustaffa M, Zainul FZ. Construction and immunogenicitystudy of a newly construct DNA vaccine candidate against Tuberculosis in mice. Aspac J Mol Biol Biotechnol. 2009;17(1):3–9. [Google Scholar]
- 20.Doherty TM. New vaccines against tuberculosis. Trop Med Int Health. 2004;9(7):818–826. doi: 10.1111/j.1365-3156.2004.01275.x. [DOI] [PubMed] [Google Scholar]
- 21.Britton WJ, Palendira U. Improving vaccines against tuberculosis. Immunol Cell Biol. 2003;81(1):34–45. doi: 10.1046/j.0818-9641.2002.01143.x. [DOI] [PubMed] [Google Scholar]
- 22.Fang CM. Development of muti-epitope vaccines for tuberculosis. School of Health Sciences (MY): USM; 2005. [PhD Thesis] [Google Scholar]
- 23.Millard TP, Hawk JL, McGregor JM. Photosensitivity in lupus. Lupus. 2000;9(1):3–10. doi: 10.1177/096120330000900103. [DOI] [PubMed] [Google Scholar]
- 24.Pisetsky DS. Systemic lupus erythematosus: Epidemiology, pathology, and pathogenesis. Primer on the rheumatic diseases. In: Klippel J, editor. 12th ed. Arthritis Foundation. Atlanta (GE). 2001. pp. 329–335. [Google Scholar]
- 25.Edworthy SM. Clinical manifestations of Systemic Lupus Erythematosus. Kelley’s Textbook of Rheumatology. In: Ruddy S, Harris ED, Sledge CB, editors. Philadelphis (US): Sunders; 2001. pp. 1105–1119. [Google Scholar]
- 26.Sharon GC. The pathogenesis of Systemic Lupus Erythematosus. Orthopaedic Nursing. 2006;25(2):140–145. doi: 10.1097/00006416-200603000-00013. [DOI] [PubMed] [Google Scholar]
- 27.CheMaraina CH, M.D. Kamaliah, M. Ishak. The autoantibody profile and its association with clinical manisfestations in Malay SLE patients. Asia Pac J of Allergy and Immunol. 2004;22(1):33–37. [PubMed] [Google Scholar]
- 28.Wang F, Wang CL, Tan CT, Manivasagar M. Systemic lupus erythematosus in Malaysia: a study of 539 patients and comparison of prevalence and disease expression in different racial and gender groups. Lupus. 1997;6(3):248–257. doi: 10.1177/096120339700600306. [DOI] [PubMed] [Google Scholar]
- 29.Frank AO. Ethnic distribution of patients with SLE seen in University Hospital, Kuala Lumpur 1967–1976. Med J Malaysia. 1980;34(3):230–237. [PubMed] [Google Scholar]
- 30.Osio-Salido E, Manapat-Reyes H. Lupus Epidemiology of systemic lupus erythematosus in Asia. Lupus. 2010;19(12):1365–1373. doi: 10.1177/0961203310374305. [DOI] [PubMed] [Google Scholar]
- 31.McCarty DJ, Manzi S, Medsger TA, Ramsey–Goldman R, LaPorte RE, Kwoh CK. Incidence of systemiclupus erythematosus: Race and gender differences. Arthritis and Rheumatism. 1995;38(9):1260–1270. doi: 10.1002/art.1780380914. [DOI] [PubMed] [Google Scholar]
- 32.Lahita RG. Gender and age in lupus. Systemic Lupus Erythematosus. In: Lahita RG, editor. 4th ed. New York (NY): Academic Press; 1999. pp. 203–221. [Google Scholar]