Abstract
Background
There are large disparities in access to health-care professionals (HCP) in low-income African countries, leading to imbalanced and suboptimal health delivery. Part of the difficulty is recruiting and retaining care professionals to work in isolated settings.
Aim
To evaluate the impact of distance continuing education as a way to build capacity, increase satisfaction and enhance the performance of care professionals in these isolated health-care facilities.
Setting
Care professionals using RAFT (Telemedicine Network in French-speaking Africa) in isolated care facilities.
Program Description
Within RAFT, an organizational framework and computer-based tools have been developed and evolved to provide useful, qualitative, applicable training material.
Program Evaluation
The activity, satisfaction, perceptions and impact of RAFT on remote health-care workers are being monitored. RAFT’s potential to improve the recruitment, satisfaction and retention of care professionals in remote settings is widely recognized; however, the actual impact on the performance and quality of care remains to be demonstrated.
KEY WORDS: telemedicine, distance education, capacity building, low-resource, impact
Sub-Saharan Africa has a disproportionate burden of disease and an extreme shortage of health workers.1 “The exodus of skilled professionals in the midst of so much unmet health need places Africa at the epicenter of the global health workforce crisis.”2 Continuing education of health-care professionals (HCPs) and access to specialized advice are keys to improving the quality, efficiency and accessibility of health systems. In developing countries, these activities are usually limited to capitals, and this constitutes an obstacle for HCPs to practice in remote areas, where they are desperately needed. The recognition of the need was well articulated during a preparatory meeting of the World Summit on the Information Society3 in 2000; graduating medical students from the Bamako University Medical School asked, “How will we keep learning once we start practicing medicine and leave the capital?”4 Several recent studies highlight the potential of information and communication technology (ICT) to address this challenge, particularly in rural areas and isolated settings.5–7 Recognizing this potential, the Geneva University Hospitals developed the telemedicine network RAFT: Réseau en Afrique Francophone pour la Télémédecine (RAFT).
This article describes our experiences in developing, deploying and evolving a distance continuing education and telemedical network for care professionals in French-speaking Africa, and discusses preliminary results of a study that investigates the impact of eHealth tools on the recruitment and retention of HCP in remote places.
SETTING AND PARTICIPANTS
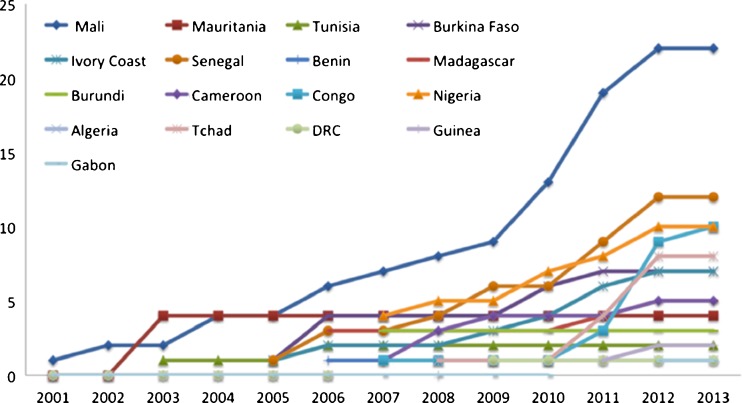
In 2001, RAFT was initiated as a pilot project in Mali and continuously expanded to other African countries. Currently, RAFT is active in 17 African countries with more than 100 connected sites (Fig. 1).
Figure 1.
Number of sites (vertical axis) connected to RAFT by year.
RAFT has a decentralized organizational structure with a central coordinating team in Switzerland and national coordination teams in each participating country.4 The national team consists of at least three collaborators: (1) a national RAFT focal point, an individual with recognized medical authority and good contacts in the government, who is in charge of overseeing the operations at the national level and ensuring that they are well integrated with any existing national e-health strategies; (2) a medical coordinator, a junior physician who is in charge of training, supporting and serving as the liaison for local health care providers to assess local educational needs and opportunities; (3) a technical coordinator, in charge of the technical aspects of the deployment and daily operations of the telemedicine tools.
Coordination meetings are organized once a year in Africa to strengthen personal links, evaluate the network development and decide about future activities. Key partners include the Université Numérique Francophone Mondiale (UNFM) and the World Health Organization (WHO). RAFT is recognized as an official WHO collaborating center for eHealth and telemedicine.
The following three case studies describe RAFT’s activities, with a greater focus provided on the third case study.
Case 1: Remote Access to Virtual Communities of Medical Experts
Health care is best delivered using collaborative approaches,8,9 rarely possible in remote locations. RAFT provides collaboration by connecting isolated providers to a virtual community via iPath,10 a secure Internet-based tele-consultation environment that enables remote consultation. This virtual collaboration helps with solving patient-specific problems, diagnosing disease and providing second opinions as well as with determining the need for and coordinating medical evacuations. Access is limited to users whose training level and expertise has been verified. iPath is currently gradually being replaced by the Bogou platform, which allows offline use with resynchronization, management of documents for long-term follow-up of patients and specialized Digital Imaging and Communications in Medicine (DICOM) interfaces for connecting imaging devices for tele-radiology and, in particular, tele-ultrasonography.
Case 2: Ultrasonography in Small Hospitals with Distant Expert Supervision
Bogou enables remote assistance with ultrasound and radiological images. Deployed in remote hospitals, these diagnostic tools, designed to sustain real-time operation under low network conditions, can significantly improve the decision-making capabilities of physicians and help them decide if a patient presenting with various medical problems, including acute abdominal pain or obstetrical problems, can be taken care of locally or needs to be evacuated.11 Such decisions are often crucial, as the risk and cost of evacuation to a regional or national hospital is high.
PROGRAM DESCRIPTION
Case 3: Distance Continuing Education of HCP
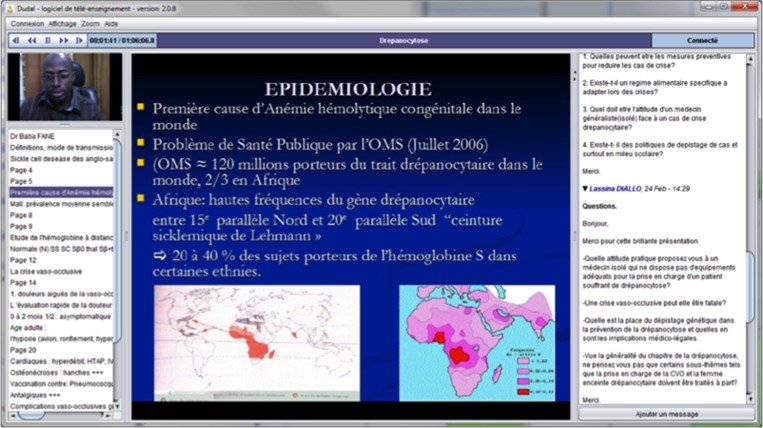
RAFT’s core activity is the weekly webcasting of interactive courses that are broadcasted via Dudal (Fig. 2), a distance education environment developed for RAFT, specifically designed to function over low-bandwidth connections (25 kilobits/s). Freely available to anyone, 80 % of the courses are produced in Africa and are regularly viewed by hundreds of care professionals. Webcast courses are generally followed by 30 min of discussion involving all participants. Once webcasted, these courses are immediately available for playback from RAFT’s website. These courses form a collection of training resources that can be organized in various ways (thematic, geographic) and even distributed offline, for example, on CD-ROMs. There is also opportunity for some participants to receive credit. For example, the African and Malagasy Council recognizes Dudal’s teaching activities for higher education (CAMES) and the Pan-African training program for specialists (Jinou). Senghor University plans to award certificates of advanced studies.
Figure 2.
A screenshot of the interactive webcasting software, Dudal.
An Educational Program Committee, consisting of six RAFT local leaders, coordinates the educational program. Each semester, the committee identifies up to five priority domains, issues a call for contributions and subsequently reviews and ranks the contributions.
PROGRAM EVALUATION
Network activity is continuously monitored for the number of educational sessions and their origin (Northern or Southern Hemisphere source), number of sites following live sessions, number of questions during sessions and number of downloads. To better understand target group needs as well as technical and organizational issues, surveys of providers from the six countries involved in RAFT at the time were conducted in 2006.12 These surveys documented high user satisfaction and good usability of the interface. The findings of this survey showed that for 92 % of the participants, the network was rated as having a great and positive impact on the African health-care system by creating access to a continuous medical training and virtually networking to HCPs that are otherwise geographically isolated.
Sixty-four percent of the users thought that the network could help solve the inequity of expertise between the countries of the North and South. Finally, this study concluded that success factors of a network such as RAFT are more organizational than technical.
Concerning the usability of the interface overall, the evaluation of “Dudal” was positive. More than half of the participants were using it without problems, one third thought that there were no significant problems with the interface, and less than one quarter were less than enthusiastic.
Impact on Human Resources
In 2010, the Equi-ResHuS action research project was established13 to document the impact of the distance education and tele-expertise support tools used in RAFT on the satisfaction and behavior of care professionals working in isolated settings and to document whether such improvements would lead to a more equitable geographic distribution of HCP in Mali. This evaluation initiative was unique because the impetus came from the Mali team rather than from the central coordinating office in Switzerland. The study is currently ongoing in four Malian district hospitals to measure the actual impact on human resource indicators such as, for example, employee retention and provider satisfaction. We report the preliminary data here.
Primary data were collected through a questionnaire, adapted from a prior study.14 The questionnaire consisted of 62 Likert-scaled (1–5) questions designed to probe 11 domains: information communication technology (ICT) access, ICT information, ICT training, ICT use (last month, last year), ICT use by colleagues, ICT advantages, impact on recruitment/retention and obstacles for recruitment/retention. Questionnaires were distributed to 45 health-care providers in four Equi-ResHuS project centers, including some not participating in RAFT activities. Descriptive statistics and regression analyses were performed to explore eHealth’s perceived advantages, disadvantages and their role in recruitment and retention of HCPs in remote regions. Survey consistency was assessed using Cronbach’s alpha with an alpha greater than 0.7 considered evidence of good consistency.15 Data were analyzed with SPSS (version 20.0).
Results
Thirty nine providers (87 %) completed surveys; participants were predominantly male (84.6 %), with an average age of 33.8 years (range 25–58 years). A third were general practitioners, 28 % nurses, 13 % medical assistants, 8 % midwives and 18 % other professionals.
The survey questionnaire was internally consistent (Table 1), with Cronbach’s alphas ranging from 0.71 to 0.97. Participants reported that they spent, on average, 6.3 % of their monthly work time using eHealth, while 12.4 % was spent on the Internet for clinical use and 13.2 % on online-education. All participants indicated that they had extended their professional network by using ICT and e-health. The highest rated advantage of RAFT was its provision of continuous medical education, followed by an ability to share field experiences with others and accessibility to training centers (Table 2). Respondents also felt that RAFT was beneficial for both recruitment and retention in remote areas, feeling that most providers were particularly concerned about accessibility of continuing education. The biggest perceived disadvantage was the fear that eHealth could replace external training. There was little concern that eHealth would replace on-site doctors or that it was perceived by patients as a lack of onsite staff.
Table 1.
Construct Validity Measures
| Questionnaire construct | Number of items | Cronbach’s alpha | Mean (standard deviation) |
|---|---|---|---|
| Access to ICT | 3 | 0.73 | 1.97 (1.07) |
| Information on ICT | 6 | 0.89 | 1.45 (0.76) |
| ICT training | 6 | 0.89 | 1.92 (0.99) |
| Last year ICT use | 4 | 0.85 | 1.75 (0.99) |
| Last month ICT use | 3 | 0.83 | 1.70 (1.02) |
| Use of ICT by colleagues | 3 | 0.87 | 2.69 (1.32) |
| Perceived advantages of ICT | 5 | 0.76 | 4.52 (0.72) |
| Perceived impact on the recruitment | 12 | 0.97 | 4.16 (0.98) |
| Perceived impact on the retention | 12 | 0.95 | 4.26 (0.74) |
| Obstacle for recruitment | 4 | 0.71 | 2.84 (1.03) |
| Obstacle for retention | 4 | 0.79 | 2.76 (1.24) |
Table 2.
Ratings of eHealth Effects by Users on a Likert Scale (1–5)
| Perceived advantage rating items | Impact on recruitment(mean) | Impact on retention(mean) |
| Availability of continuous medical education | 4.41 | 4.44 |
| Ability to share field experiences with others | 4.39 | 4.15 |
| Accessibility to training multi-centers | 4.25 | 4.26 |
| Possibility of promoting the health center | 4.24 | 4.32 |
| Possibility to participate in team meetings remotely | 4.22 | 4.17 |
| Improving the quality of practice | 4.18 | 4.32 |
| Rapid access specialized to resources | 4.16 | 4.25 |
| Possibility of a bi-directional distance learning program | 4.16 | 4.11 |
| Direct access to specialized resources | 4.08 | 4.27 |
| Continuity of service | 3.97 | 4.14 |
| Possibility to ask for a second opinion | 3.76 | 3.91 |
| Best impression of patients | 3.75 | 4.06 |
| Perceived disadvantage rating items | Impact on recruitment | Impact on retention |
| eHealth replaces the majority of external training | 3.28 | 3.18 |
| eHealth enters into competition with the allocation of resources to purchase other materials | 3.17 | 2.73 |
| eHealth replaces a doctor on site | 2.62 | 2.79 |
| eHealth stands for a lack of staff | 2.09 | 2.06 |
Our regression analysis suggested that four variables (attitude, perceived benefit, training and information) explained over half (52 %) of the variance in the impact of RAFT eHalth tools on recruitment in remote areas, suggesting a potentially large impact. For retention, eHealth had a perceived benefit, explaining 34 % of the variance in factors influencing retention.
Discussion
Our data indicate that providers generally have a positive perception of eHealth and that its availability could explain over half the factors that go into recruitment decisions for remote practice by providers. The impact on retention seems to be less important than on recruitment, although our data suggest that it could be influential, explaining over a third of decisions about staying in isolated areas. Access to training and the possibility to interact with other HCPs were highlighted as particularly important. These data suggest that eHealth tools have real potential to de-isolate health-care providers, ease recruitment and retention, and support networking and decision-making.
Our finding of differences in attitudes between users and nonusers of eHealth tools is consistent with the assumption of Rogers’ diffusion of innovations model,16 which states that the adoption of an innovation is particularly influenced by the perception of its advantages, the provability of its results and the opportunity to test it.
Access to continuing medical education is consistently considered the most important request by care professionals in isolated settings, with a preference for live, interactive online courses. There are a number of ongoing changes to help address various challenges. First, care professionals are increasingly requesting formal recognition of continuing medical education. There are multiple challenges for providing credit, including converting credentialing “voluntary lecture” types of activities as well as the reliable identification, tracking and evaluation of students, and integration into an institutional learning management system. To help translate acquired knowledge into operational knowledge, cases are being developed for VIPS,10 a Virtual Internet Patient Simulator that reproduces the diagnostic and therapeutic infrastructure of an isolated hospital and also provides challenging cases that focus on problem resolution issues and on the operational decision-making process. In addition, intermittent connectivity and mobility are important key drivers for accessing information. The system has been upgraded to allow courses to be downloaded when the user has connectivity and played on mobile devices later.
Conclusion
These preliminary results suggest that the availability of eHealth, especially access to continuous education, improves retention and facilitates the recruitment of young HCPs to remote locations. The results are sufficiently encouraging to merit investigating the actual impact of eHealth on isolated health-care provider practice in greater detail.
Acknowledgments
The work is being carried out thanks to the support from the Geneva International Solidarity Fund, a grant provided by the Research Centre for the International Development of Canada, and financial assistance from the Canadian government through the Canadian International Development Agency.
Conflict of Interest
The authors have no conflict of interest or commercial interest related to the work presented in the article.
REFERENCES
- 1.Mars M. Building the capacity to build capacity in e-health in sub-Saharan Africa: the KwaZulu-Natal experience. Telemed J E Health. 2012;18(1):32–7. doi: 10.1089/tmj.2011.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Organization WH. Working together for health: the World Health Report 2006. Geneva: World Health Organization; 2006. pp. 3–15. [Google Scholar]
- 3.ITU World Summit on the Information Society. Available at: http://www.itu.int/wsis. Accessed May 14, 2013.
- 4.Geissbuhler A, Bagayoko CO, Ly O. The RAFT network: 5 years of distance continuing medical education and tele-consultations over the Internet in French-speaking Africa. Int J Med Inform. 2007;76(5–6):351–6. doi: 10.1016/j.ijmedinf.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Curran VR, Fleet L, Kirby F. Factors influencing rural health care professionals’ access to continuing professional education. Aust J Rural Health. 2006;14(2):51–5. doi: 10.1111/j.1440-1584.2006.00763.x. [DOI] [PubMed] [Google Scholar]
- 6.Childs S, et al. Effective e-learning for health professionals and students—barriers and their solutions. A systematic review of the literature—findings from the HeXL project. Health Info Libr J. 2005;22(Suppl 2):20–32. doi: 10.1111/j.1470-3327.2005.00614.x. [DOI] [PubMed] [Google Scholar]
- 7.Clarke A, et al. A strategic approach to developing e-learning capability for healthcare. Health Info Libr J. 2005;22(Suppl 2):33–41. doi: 10.1111/j.1470-3327.2005.00611.x. [DOI] [PubMed] [Google Scholar]
- 8.McPherson K, Headrick L, Moss F. Working and learning together: good quality care depends on it, but how can we achieve it? Qual Health Care. 2001;10(Suppl 2):ii46–53. doi: 10.1136/qhc.0100046... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel VL, et al. The collaborative health care team: the role of individual and group expertise. Teach Learn Med. 2000;12(3):117–32. doi: 10.1207/S15328015TLM1203_2. [DOI] [PubMed] [Google Scholar]
- 10.Brauchli K, et al. iPath—a telemedicine platform to support health providers in low resource settings. Stud Health Technol Inform. 2005;114:11–7. [PubMed] [Google Scholar]
- 11.Bagayoko CO, et al. Deploying portable ultrasonography with remote assistance for isolated physicians in Africa: lessons from a pilot study in Mali. Stud Health Technol Inform. 2010;160(Pt 1):554–8. [PubMed] [Google Scholar]
- 12.Co B. Réseau de Télé-enseignement Médical, Identification des Barrières Technologiques, Organisationnelles et Humaines. Master Thesis. Paris 6 University, 2006.
- 13.Bagayoko CO, et al. Can ICTs contribute to the efficiency and provide equitable access to the health care system in Sub-Saharan Africa? The Mali experience. Yearb Med Inform. 2011;6(1):33–8. [PubMed] [Google Scholar]
- 14.Fortin J-P, et al. La télésanté: une stratégie pour soutenir la pratique des médecins en régions éloignées 2006: Canadian Health Services Research Foundation.
- 15.Nunnally JC. Psychometric theory. New York: McGraw-Hill Education; 2010. pp. 233–6. [Google Scholar]
- 16.Rogers EM. Diffusion of innovations. New York: Free Press; 2010. [Google Scholar]