ABSTRACT
BACKGROUND
Previous studies have reported that health literacy limitations are associated with poorer disease control for chronic conditions, but have not evaluated potential associations with medication adherence.
OBJECTIVE
To determine whether health literacy limitations are associated with poorer antidepressant medication adherence.
DESIGN
Observational new prescription cohort follow-up study.
PARTICIPANTS
Adults with type 2 diabetes who completed a survey in 2006 and received a new antidepressant prescription during 2006–2010 (N = 1,366) at Kaiser Permanente Northern California.
MAIN MEASURES
Validated three-item self-report scale measured health literacy. Discrete indices of adherence based on pharmacy dispensing data according to validated methods: primary non-adherence (medication never dispensed); early non-persistence (dispensed once, never refilled); non-persistence at 180 and 365 days; and new prescription medication gap (NPMG; proportion of time that the person is without medication during 12 months after the prescription date).
KEY RESULTS
Seventy-two percent of patients were classified as having health literacy limitations. After adjusting for sociodemographic and clinical covariates, patients with health literacy limitations had significantly poorer adherence compared to patients with no limitations, whether measured as early non-persistence (46 % versus 38 %, p < 0.05), non-persistence at 180 days (55 % versus 46 %, p < 0.05), or NPMG (41 % versus 36%, p < 0.01). There were no significant associations with primary adherence or non-persistence at 365 days.
CONCLUSIONS
Poorer antidepressant adherence among adults with diabetes and health literacy limitations may jeopardize the continuation and maintenance phases of depression pharmacotherapy. Findings underscore the importance of national efforts to address health literacy, simplify health communications regarding treatment options, improve public understanding of depression treatment, and monitor antidepressant adherence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-013-2402-8) contains supplementary material, which is available to authorized users.
KEY WORDS: health literacy, medication adherence, antidepressive agents, diabetes mellitus, healthcare disparities
INTRODUCTION
Individuals with sufficient health literacy are better equipped at managing chronic conditions effectively than those with inadequate health literacy. Health literacy has been defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions”.1 Because nearly 90 % of Americans have some difficulty using routine health information,2 the US Surgeon General has identified the improvement of health literacy as a national priority.3 Emerging data indicates that people with health literacy limitations have poorer disease control for chronic medical conditions such as diabetes, congestive heart failure4 and HIV, and that health literacy may partially mediate racial/ethnic differences in medication adherence for some conditions.5,6
Depression is a significant comorbidity for patients with chronic medical conditions, and occurs twice as frequently among adults with diabetes compared to adults without diabetes.7 Among adults with diabetes, depression is associated with impaired self-care and increased risk of microvascular and macrovascular complications, dementia, and mortality.8–12 Therefore, effective treatment for depression is particularly important for people with diabetes. However, little is known about factors that influence adherence to antidepressant medications, the most common treatment for depression, in this population.13 Some data suggests that patients with limited health literacy are more likely to have depression.14 Health literacy limitations may pose even greater barriers to care for depression than for other chronic diseases, due to misinformation about depression, stigma, and the adverse effects of depression on motivation, self-efficacy, and executive function. However, we are not aware of studies that have examined the association between health literacy and depression treatment among patients with diabetes.
Race/ethnicity is associated with the presence of both health literacy limitations and diabetes.2,15,16 Nationally, African American, Hispanic, American Indian/Alaska Native, and multiracial individuals, as well as people who did not speak English before entering school, have worse health literacy than white Americans and those who spoke only English prior to school.2 Similarly, across the United States, African American, Hispanic, American Indian/Alaska Native, and Asian Americans have a higher prevalence of diabetes and its complications than white Americans, with disparities in diabetes prevalence growing over time.15,16 Several studies have also reported that both Hispanic and African American patients prefer counseling over antidepressant medication when treating affective illness, which could influence adherence to these medications. Furthermore, diabetes control is more closely linked with depression and missing medication doses among African American relative to white patients.17 Findings such as these underscore the relevance of depression and self-management to health outcomes among African American patients, and may also be important for other racial/ethnic minority patients.
In this study, we examined whether diabetic adults who have health literacy limitations have poorer adherence to prescribed antidepressant medication than counterparts without health literacy limitations. Because health literacy is potentially modifiable, understanding its association with antidepressant medication adherence, a critical component of depression management, may guide the development of interventions to address disparities in depression care and improve depression outcomes among adults with diabetes. We examined non-adherence during a period of 12 months from the initial prescription date, which encompasses the acute, continuation, and maintenance phases of depression treatment.18
METHODS
Setting
Kaiser Permanente Northern California (KPNC) is a large, integrated healthcare delivery system that serves 30 % of the region’s population. The KPNC patients are a well-characterized multi-ethnic population similar to the population of Northern California, except for the extreme tails of the income distribution.19 Kaiser Permanente’s Institutional Review Board approved this study.
Study Population
The Diabetes Study of Northern California (DISTANCE) survey was conducted from 2005 to 2006 among an ethnically-stratified random sample of 40,735 adults with diabetes aged 30 to 75 years that oversampled racial/ethnic minorities. The final sample consisted of 20,188 participants, for a 62 % overall response rate (algorithm from the Council on American Survey Research Organizations that adjusts for eligibility). Participants completed the survey as a written (33.1 %) or web-based survey (15.2 %) in English, or as computer-assisted telephone interview (51.7 %) in English, Spanish, Cantonese, Mandarin, or Tagalog. Details of the design and methods have been previously reported.20
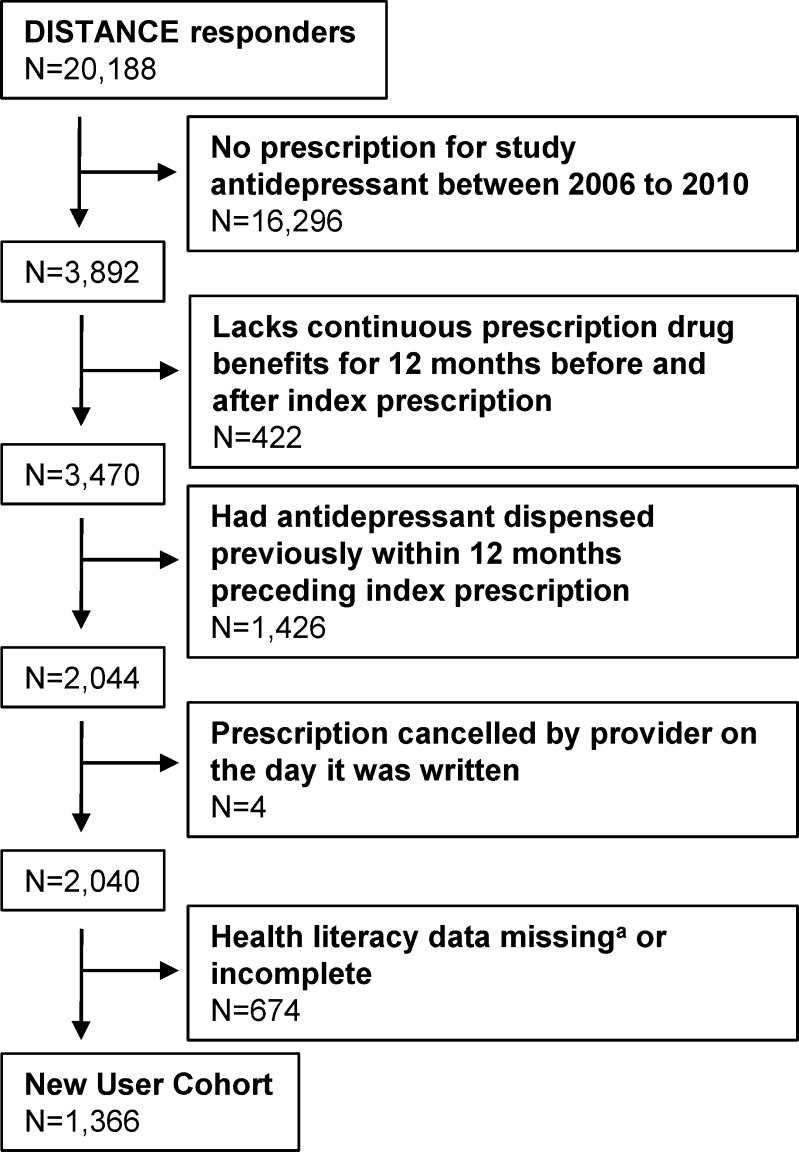
Eligibility for the current study was limited to 1,366 survey respondents who 1) were newly prescribed a serotonin reuptake inhibitor (SSRI), a serotonin-norepinephrine reuptake inhibitor (SNRI), bupropion or mirtazapine during 2006–2010 (index prescription); 2) were not dispensed antidepressants in the 12 months preceding the index prescription; 3) had continuous pharmacy benefits for at least 12 months after the index prescription date; and 4) provided complete responses to three survey items assessing health literacy (Fig. 1).
Figure 1.
Flowchart of new antidepressant user cohort. aHealth literacy items were not included on a short form of the survey (n = 216).
Exposure
Health literacy was based on a self-report scale that has been validated against direct measures of health literacy in a variety of settings, and among patients with diabetes.21–23 Participants responded on a 5-point scale to three items: (a) “How often do you have problems learning about your medical condition because of difficulty understanding written information (not including problems due to poor vision)?”; (b) “How confident are you filling out medical forms by yourself?”; (c) “How often do you have someone like a family member, friend, hospital or clinic worker or caregiver, help you read Kaiser health plan materials (such as written information about your health or care you are offered)?”. As in prior research, the sum of the item scores were coded dichotomously as having any health literacy limitations (scores 0–14), versus no evidence of health literacy limitations (score = 15).24
Outcomes
Indicators of adherence were based on pharmacy utilization according to validated methods.25 Because it is common for individuals to switch antidepressants early in the course of treatment, we considered patients to be adherent if pharmacy data indicated a switch from the index prescription to any other antidepressant medication under study. Primary non-adherence was defined as no dispensing of the index prescription within 60 days of the index prescription date. Early non-persistence was defined as the dispensing of the index prescription once, but no additional dispensing of that antidepressant within the period defined by the number of days supply of medication dispensed plus a grace period equal to 100 % of prior days supply. New prescription medication gap (NPMG) was calculated as the proportion of the time that the person was without the index prescription during 12 months after the initial prescription order, based on the daily dosage of medication prescribed, number of pills prescribed and refill dates.25 To evaluate antidepressant use during continuation and maintenance phases of therapy, we determined the proportion of patients who were non-persistent at 180 days and 365 days, based on days supply dispensed before the cutoff (for a terminal fill), or based on a gap equal to the prior days supply plus a grace period equal to 100 % of prior days supply.
Covariates
Participants reported demographic information including age, gender, race/ethnicity (white, African-American, Latino, Asian American, Filipino, or other/multiracial/unknown), English proficiency (coded as limited or good, based on difficulty understanding or speaking English), education (less than high school graduate, high school graduate or greater), and family income as a proportion of federal poverty level (FPL) adjusted for family size (dichotomized as < 300 %, ≥ 300 %), and whether they reported they were previously diagnosed with or received treatment for depression. Medical status was assessed with a dichotomous indicator for the history of any of the following self-reported diabetes complications: myocardial infarction, cerebrovascular accident, coronary artery disease (as indicated by coronary artery bypass surgery or angioplasty), lower extremity amputation, or renal failure requiring dialysis or transplantation.
Data Analysis
Bivariate associations between health literacy and categorical and continuous measures of antidepressant adherence were examined using Chi-square analysis and t-tests, respectively. After adjusting for age, gender, race/ethnicity, income, depression history, and diabetes complications, modified Poisson regression models were specified to estimate the relative risk of antidepressant non-adherence for those with health literacy limitations versus those without.26 The mean absolute prevalence (predicted probabilities) of non-adherence was generated for each health literacy group using modified least squares regression.27 A generalized linear regression model was specified with the same covariates to evaluate the relationship between health literacy and continuous NPMG outcome. All multivariate models were expansion weighted for the race-stratified sampling design (non-proportional sampling fractions) and weighted for survey nonresponse using the Horvitz–Thompson approach.28 Multiple imputation was used for missing covariates in multivariate models, and an alpha level of 0.05 was set as the threshold for statistical significance.
Three sets of sensitivity analyses were conducted. First, multivariate models were repeated on cases with complete data. Second, models were repeated after adjustment for English proficiency and for education, which has significant overlap with health literacy. Third, because bupropion and duloxetine are FDA-approved for nonpsychiatric indications (smoking cessation and diabetic peripheral neuropathy, respectively), the multivariate analyses were repeated after excluding patients prescribed either of these antidepressants who lacked a chart diagnosis of a depressive or anxiety disorder within 1 year preceding or after the index prescription.
RESULTS
Among 2,040 patients who were newly prescribed an antidepressant, complete data on health literacy was available for 1,366 (67 %), of whom the majority (72 %; n = 984) reported some health literacy limitations. Health literacy limitations were significantly associated with older age, racial/ethnic minority status, limited English proficiency, lower education and income (Table 1). We examined baseline differences between those with complete versus incomplete or missing health literacy data. Having incomplete or missing data was not associated with age (t = 0.95, 2,038 df, p = 0.34), but was slightly more common among men than women (44 % versus 39 %, χ2 = 3.47, 2 df, p = 0.06) and was associated with racial/ethnic minority status (χ2 = 102.13, 6 df, p < 0.0001), and less than high school education (χ2 = 30.27, 2 df, p < 0.0001).
Table 1.
Demographic and Clinical Characteristics by Health Literacy Group
| Any health literacy limitation N = 984 (72 %) N (%) or mean (SD) | No health literacy limitation N = 382 (28 %) N (%) or mean (SD) | Test statistic (df)* | p | |
|---|---|---|---|---|
| Age | 58.7 (10.5) | 55.0 (10.4) | t(703) = −5.84 | < 0.001 |
| Gender | ||||
| Male | 404 (41.1) | 135 (35.3) | χ2(1) = 3.76 | 0.05 |
| Female | 580 (59.9) | 247 (64.7) | ||
| Race/ethnicity | ||||
| African American | 177 (18.0) | 77 (20.2) | χ2(6) = 27.71 | < 0.001 |
| Asian American | 69 (7.0) | 19 (5.0) | ||
| Caucasian | 264 (26.8) | 146 (38.2) | ||
| Filipino | 72 (7.3) | 17 (4.5) | ||
| Latino | 250 (25.4) | 65 (16.8) | ||
| Multiracial | 113 (11.5) | 40 (10.5) | ||
| Other/unknown | 39 (4.0) | 19 (5.0) | ||
| Income (N = 1,232) | ||||
| Less than 300 % FPL | 446 (50.7) | 97 (27.6) | χ2(1) = 54.55 | < 0.001 |
| 300 % FPL or greater | 434 (49.3) | 255 (72.4) | ||
| Education (N = 1,345) | ||||
| Less than high school | 205 (21.2) | 26 (6.9) | χ2(1) = 39.47 | < 0.001 |
| High school graduate or greater | 761 (78.8) | 353 (93.1) | ||
| English proficiency (N = 1,353) | ||||
| Good | 890 (91.2) | 374 (99.2) | χ2(1) = 28.43 | < 0.001 |
| Limited | 86 (8.8) | 3 (0.8) | ||
| Prior depression diagnosis or treatment (N = 1,314) | 392 (41.4) | 146 (39.7) | χ2(1) = 0.34 | 0.56 |
| Any diabetes complication (N = 1,310) | 256 (27.1) | 61 (16.7) | χ2(1) = 15.71 | < 0.001 |
*t-tests use the Satterthwaite method, which does not assume equal variances
FPL federal poverty level
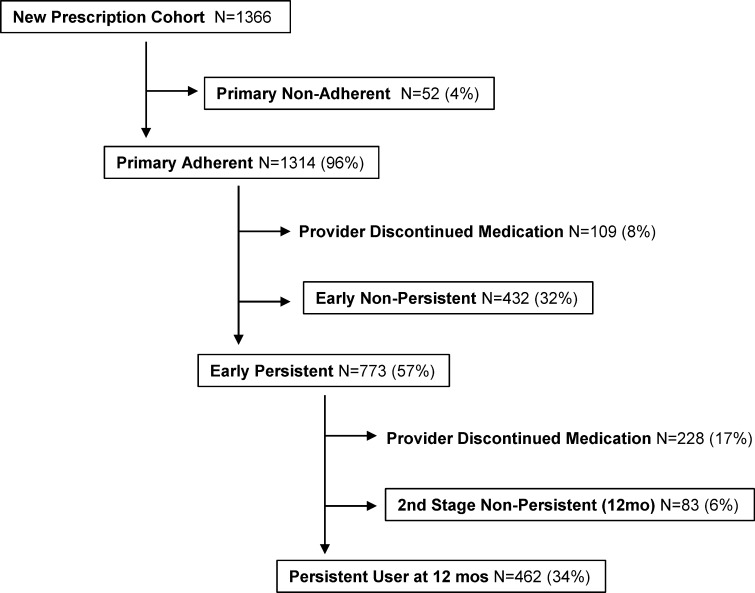
Among this sample, depression was frequently recurrent or chronic, with over 40 % reporting at least one prior depressive episode, and 30 % reporting three or more prior lifetime episodes (data not shown in table). Although primary non-adherence was uncommon in this sample (4 %), 43 % prescribed an initial antidepressant prescription never received a refill and nearly two-thirds of the new users had discontinued the antidepressant by the end of the 12-month period (Fig. 2).
Figure 2.
Antidepressant utilization among adults with diabetes.
Bivariate Associations
Primary non-adherence did not differ by health literacy status [χ2(1) = 0.0, NS]. Patients with any health literacy limitation, however, were significantly more likely than those with none to have early non-persistence [46 % versus 38 %, χ2(1) = 6.4, p = 0.01], to be non-persistent at 180 days [54 % versus 45 %, χ2(1) = 8.7, p < 0.01] and 365 days [68 % versus 62 %, χ2(1) = 4.1, p < 0.05], and had poorer overall adherence based on NPMG, with a higher mean percentage of days without antidepressant available [41 % versus 35 %, t(1,364) = −2.45, p < 0.05] during the year following index prescription date.
Multivariate Associations
After adjusting for age, gender, race/ethnicity, income, depression history, and diabetes complications, patients with any health literacy limitation were significantly more likely than those with none to discontinue before the first refill (i.e., early non-persistent: 46 % versus 38 %, RR = 1.28, p < 0.05) and to be non-persistent at 180 days (55 % versus 46 %, RR = 1.26, p < 0.05) (Table 2). Compared to patients with no health literacy limitation, after multivariate adjustment, those with limitations were not significantly more likely to be non-persistent at 365 days (70 % versus 62 %, RR = 1.12, p = 0.11), but did have significantly more days without antidepressant medications available over the entire year, as indicated by NPMG (41 % versus 36 %, β = 0.06, p < 0.01). This translates into approximately 21 additional days without antidepressant medications over the year.
Table 2.
Adjusted Associations Between Health Literacy Limitations and Antidepressant Medication Adherence (n = 1,366)
| Early non-persistent | Non-persistent at 180 days | Non-persistent at 365 days | NPMG | |||||
|---|---|---|---|---|---|---|---|---|
| RR (95 % CI) | p | RR 95 % CI | p | RR 95 % CI | p | β* 95 % CI | p | |
| Any health literacy limitation (reference = none) | 1.28 (1.03, 1.61) | 0.03 | 1.26 (1.04, 1.54) | 0.02 | 1.12 (0.97, 1.30) | 0.11 | 0.06 (0.01, 0.10) | 0.008 |
| Race/ethnicity (reference = white) | ||||||||
| African American | 1.48 (1.17, 1.87) | 0.001 | 1.42 (1.16, 1.74) | 0.001 | 1.33 (1.16, 1.52) | < 0.001 | 0.13 (0.07, 0.19) | < 0.001 |
| Asian | 1.37 (1.00, 1.88) | 0.05 | 1.49 (1.16, 1.92) | 0.002 | 1.36 (1.15, 1.60) | < 0.001 | 0.15 (0.03, 0.27) | 0.01 |
| Filipino | 1.56 (1.18, 2.06) | 0.002 | 1.49 (1.17, 1.91) | 0.001 | 1.19 (0.98, 1.44) | 0.07 | 0.12 (0.01, 0.24) | 0.04 |
| Latino | 1.73 (1.40, 2.14) | < 0.001 | 1.63 (1.36, 1.95) | < 0.001 | 1.30 (1.14, 1.48) | < 0.001 | 0.13 (0.08, 0.19) | < 0.001 |
| Multiracial | 1.51 (1.12, 2.02) | 0.007 | 1.52 (1.20, 1.93) | 0.001 | 1.20 (1.00, 1.45) | 0.05 | 0.11 (0.05, 0.18) | 0.001 |
| Other/unknown | 1.66 (1.14, 2.43) | 0.009 | 1.77 (1.37, 2.29) | < 0.001 | 1.28 (1.03, 1.59) | 0.03 | 0.16 (0.05, 0.27) | 0.004 |
| Low income (reference = higher income) | 1.07 (0.88, 1.30) | 0.49 | 1.08 (0.92, 1.28) | 0.33 | 1.13 (1.00, 1.27) | 0.05 | 0.05 (0.00, 0.09) | 0.04 |
Models adjusted for age, gender, diabetes complications, and prior depression diagnosis / treatment
*The β coefficient reported represents the absolute difference in NPMG (rounded to two decimal places) for each variable relative to the reference group. For example, the NPMG for individuals with any health literacy limitation is 0.414 versus 0.357 for individuals with no limitation, and thus the difference is 0.057, or 0.06 as indicated by the β coefficient reported in the Table. The interpretation of this number is that relative to those without health literacy limitations, individuals with limitations had 6 % more days over the course of the year without antidepressant medications available
The multivariate models also demonstrated noteworthy differences by sociodemographic and socioeconomic indicators. Being a non-white minority was strongly and significantly associated with the measures of antidepressant non-adherence for almost every index. Low income was significantly associated with non-persistence at 365 days and NPMG.
All three sensitivity analyses (complete data only, adjusting for English proficiency and education, and excluding bupropion or duloxetine for patients without a chart diagnosis of a depressive or anxiety disorder within 1 year of the index prescription date) yielded similar patterns and similar parameter estimates, although in a few instances, the statistical significance was reduced (i.e., some p values exceeded 0.05) in complete case analyses and models excluding patients on bupropion or duloxetine without chart diagnoses (Appendix Table, available online).
DISCUSSION
Among a large sample of ethnically-diverse adults with diabetes prescribed antidepressant medications, having any health literacy limitation was common and was associated with modestly increased likelihood of antidepressant discontinuation, particularly early in the course of treatment. The association between health literacy and antidepressant adherence was not accounted for by other indicators of social disadvantage, such as income or education, nor was it attributable to racial/ethnic differences or English proficiency. In addition, we did observe a strong association between racial/ethnic minority status and lower antidepressant adherence in multivariate models, suggesting that health literacy and race/ethnicity have independent effects on antidepressant adherence. The high rate of antidepressant non-adherence among racial/ethnic minority groups is consistent with prior research,29,30 yet noteworthy nevertheless, because all patients in this study were insured and received care in the same integrated healthcare system.
Depression in adults with diabetes is frequently chronic and recurrent, suggesting the need for long-term antidepressant therapy. Several prior studies have shown that approximately 70 % of patients with comorbid depression and diabetes reported that they have been depressed for more than 2 years.31,32 Nearly one-third of our sample reported three or more prior depressive episodes. The high rates of early discontinuation that were observed among adults with diabetes who had any health literacy limitation suggests that few of these individuals received continuation and maintenance phase antidepressant therapy, which are critical in preventing relapse and recurrence. Physicians should be aware of the increased risk for antidepressant discontinuation among patients with any health literacy limitation and among patients from racial/ethnic minority groups. For antidepressant treatment to succeed, these patients may require more intensive counseling about use of antidepressant medications and closer follow-up. Our findings underscore the need for physicians to improve health communication with their patients regarding depression management.33,34 Team-based approaches, such as collaborative depression care that provides educational materials regarding depression diagnosis, treatment, psychoeducation, and support by care managers, have been shown to significantly increase antidepressant adherence in patients with comorbid depression and diabetes, and improve disease control for both conditions.32,35 Such interventions may succeed in part by empowering patients to become more engaged in their depression management and communicate more effectively with their providers when they are experiencing medication side effects.35
Some study limitations should be noted. The health literacy questions we employed measure general health literacy for written materials. Future research should explore disease-specific health literacy for depression, which may encompass understanding and beliefs regarding depression and the options for depression treatment that are known to vary according to race/ethnicity.36,37 We note that in addition to health literacy, race/ethnicity was strongly related to antidepressant adherence; race/ethnicity may be serving as a proxy for cultural beliefs and attitudes (including stigma) about antidepressant use that could contribute to depression-specific health literacy, but were not measured in our study. Data on health literacy was missing or incomplete for one-third of patients newly prescribed an antidepressant. We examined patterns of missing data, and found that the response rate for the health literacy items was similar to the response rates for adjacent items in the survey, which suggests that participants were not selectively skipping these items. However, because individuals with incomplete or missing health literacy data were more likely to be non-white and had lower educational attainment, characteristics which were associated with medication non-adherence, this may have influenced our findings by excluding a group of people with higher rates of non-adherence. Similarly, antidepressant use was based on pharmacy utilization data according to methods that have been previously validated,25 and reasons for discontinuation were not known. Medication adherence can be estimated more directly from methods such as medication blood levels. However, these more costly and intensive methods are not practical for large-scale health services research. We note that dispensing records likely overestimate adherence, as it cannot be confirmed that the medication was actually used and it is unknown whether such overestimation is consistent across diverse patient groups. However, that misclassification is likely non-differential across levels of literacy, and thus our findings can be assumed to be conservative. Although this is a large, ethnically diverse sample, all participants were insured via KPNC, and therefore results may not generalize to settings serving more disadvantaged and uninsured populations. However, these findings do reflect what may be expected in settings where access to and quality of care, including mental health care, do not differ across social groups.
In summary, our findings suggest that clinicians treating patients with diabetes and depression should be alerted to the high rate of antidepressant discontinuation, and its association with health literacy limitations and with minority race/ethnicity. Our results add to emerging evidence about the importance of health literacy in adherence to prescribed medications for chronic conditions such as HIV and diabetes.5,6 Moreover, these findings underscore the importance of national efforts to address health literacy and simplify health communications regarding pharmacotherapy, improve public understanding of depression treatment, monitor antidepressant adherence, and provide additional service to support continuation and maintenance therapy.
Electronic supplementary material
Sensitivity analyses demonstrating the associations between health literacy limitations, race/ethnicity, and antidepressant medication adherence (DOCX 31 kb)
Acknowledgements
This research was supported by funding from the National Institutes of Health (R01-DK080726, R01-DK081796, P30-DK092924, and NCATS Grant KL2 TR000421). This research reported in this manuscript was presented at the annual meeting of the Academy of Psychosomatic Medicine in Atlanta GA, November 2012.
Conflict of Interest
Dr. Katon has received honoraria for CME lectures from Pfizer, Forest, and Eli Lilly and is on the advisory board for Eli Lilly. The authors report no other potential conflicts of interest.
REFERENCES
- 1.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Washington: National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: U.S. Department of Education. National Center for Education Statistics; 2006.
- 3.Benjamin R. Health literacy improvement as a national priority. J Health Commun. 2010;15(Suppl 2):1–3. doi: 10.1080/10810730.2010.499992. [DOI] [PubMed] [Google Scholar]
- 4.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26(9):979–86. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33(5):374–8. doi: 10.1016/j.amepre.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Osborn CY, Cavanaugh K, Wallston KA, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(Suppl 3):268–78. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 8.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 10.Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 11.Katon W, Lyles CR, Parker MM, Karter AJ, Huang ES, Whitmer RA. Association of depression with increased risk of dementia in patients with type 2 diabetes: the diabetes and aging study. Arch Gen Psychiatry. 2012;69(4):410–7. doi: 10.1001/archgenpsychiatry.2011.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan MD, O’Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL substudy. Diabetes Care. 2012;35(8):1708–15. [DOI] [PMC free article] [PubMed]
- 13.Katon WJ, Simon G, Russo J, et al. Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care. 2004;42(12):1222–9. doi: 10.1097/00005650-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 15.Carter JS, Pugh JA, Monterrosa A. Non-insulin-dependent diabetes mellitus in minorities in the United States. Ann Intern Med. 1996;125(3):221–32. doi: 10.7326/0003-4819-125-3-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Q, Wang Y, Huang ES. Changes in racial/ethnic disparities in the prevalence of type 2 diabetes by obesity level among US adults. Ethn Health. 2009;14(5):439–57. doi: 10.1080/13557850802699155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duru OK, Gerzoff RB, Selby JV, et al. Identifying risk factors for racial disparities in diabetes outcomes: the translating research into action for diabetes study. Med Care. 2009;47(6):700–6. doi: 10.1097/MLR.0b013e318192609d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3. Washington: American Psychiatric Association; 2010. [PubMed] [Google Scholar]
- 19.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287(19):2519–27. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 20.Moffet HH, Adler N, Schillinger D, et al. Cohort profile: The Diabetes Study of Northern California (DISTANCE)—objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol. 2009;38(1):38–47. doi: 10.1093/ije/dyn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94. [PubMed] [Google Scholar]
- 22.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26(3):265–71. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from the diabetes study of northern California (DISTANCE) J Health Commun. 2010;15(Suppl 2):183–96. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5 Pt 1):1640–61. doi: 10.1111/j.1475-6773.2009.00989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zou GY. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 27.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. Am J Epidemiol. 2007;166(11):1337–44. doi: 10.1093/aje/kwm223. [DOI] [PubMed] [Google Scholar]
- 28.Horvitz DG, Thompson DJ. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc. 1952;47(260):663–85. doi: 10.1080/01621459.1952.10483446. [DOI] [Google Scholar]
- 29.Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163(1):101–8. doi: 10.1176/appi.ajp.163.1.101. [DOI] [PubMed] [Google Scholar]
- 30.Wu CH, Erickson SR, Piette JD, Balkrishnan R. The association of race, comorbid anxiety, and antidepressant adherence among Medicaid enrollees with major depressive disorder. Res Soc Adm Pharm. 2012;8(3):193–205. doi: 10.1016/j.sapharm.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Katon WJ, Von Korff M, Lin EHB, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61(10):1042–9. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 32.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient Educ Couns. 2004;52(3):315–23. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 34.Swenson SL, Rose M, Vittinghoff E, Stewart A, Schillinger D. The influence of depressive symptoms on clinician–patient communication among patients with type 2 diabetes. Med Care. 2008;46(3):257–65. doi: 10.1097/MLR.0b013e31816080e9. [DOI] [PubMed] [Google Scholar]
- 35.Lin EH, Von Korff M, Ciechanowski P, et al. Treatment adjustment and medication adherence for complex patients with diabetes, heart disease, and depression: a randomized controlled trial. Ann Fam Med. 2012;10(1):6–14. doi: 10.1370/afm.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 37.Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. Gen Hosp Psychiatry. 2007;29(3):182–91. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sensitivity analyses demonstrating the associations between health literacy limitations, race/ethnicity, and antidepressant medication adherence (DOCX 31 kb)