Abstract
Combination treatment of antiplatelet drugs containing aspirin and clopidogrel reduces systemic ischemic events after percutaneous coronary intervention (PCI) in high risk patients. However, this combination treatment of antiplatelet drugs is associated with increased risk of nonfatal and fatal bleeding. Diffuse alveolar hemorrhage after PCI is a rare complication that has been mostly reported in association with glycoprotein IIb/IIIa inhibitors. We report the case of a 62-year-old man who presented with ST elevation myocardial infarction and suffered a diffuse alveolar hemorrhage after clopidogrel use following primary PCI.
Keywords: Hemoptysis, Antiplatelet drugs, Myocardial infarction
Introduction
The treatment combination of clopidogrel and aspirin reduces systemic ischemic events after percutaneous coronary intervention (PCI) in high risk patients.1-3) However, the combination treatment of these antiplatelet drugs is associated with an increased tendency towards bleeding. Except for gastrointestinal bleeding, the occurrence of a major bleeding is rare.4-6) Herein, we report a rare case of serious alveolar hemorrhage induced by clopidogrel use following primary PCI for ST elevation myocardial infarction.
Case
A 62-year-old man was transferred to our hospital because of chest pain. The patient had a medical history of hypertension and had been a heavy smoker for 40 pack-years. On arrival, his blood pressure was 114/70 mm Hg, heart rate was 75 bpm, respiratory rate was 16/minute, and body temperature was 36.5℃. White blood cell count was 13930/mm3, hemoglobin was 14.2 g/dL, and platelets were 294000/mm3. Aspartate aminotransferase was 79 U/L and alanine aminotransferase was 104 U/L. Blood urea nitrogen, creatinine, and electrolytes were all within normal limits. Electrocardiogram showed an ST elevation in the V 1 through V 6 leads, and ST depression in the II, III and aVF leads. The patient was diagnosed as having ST elevation myocardial infarction. After the patient had taken 300 mg aspirin and 600 mg clopidogrel, he underwent primary PCI. Coronary angiograms showed 99% stenosis of the mid-left anterior descending artery (Fig. 1). Therefore, a coronary stent (Endeavor®, Zotarolimus-Eluting Coronary Stent, 3.0×26 mm, Medtronic) was implanted (Fig. 1). The patient was admitted to the coronary care unit (CCU) and triple antiplatelet therapy was started.
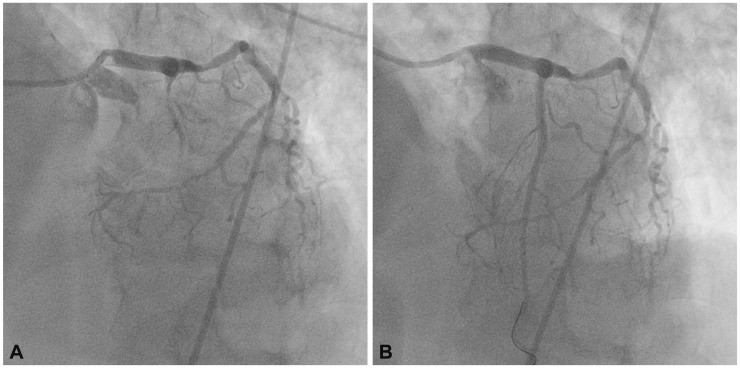
Fig. 1.
A: coronary angiograms show 99% stenosis of mid left anterior descending artery with large occlusive thrombus. B: coronary angiogram after stent implantation demonstrates adequate luminal diameter of mid left anterior descending artery.
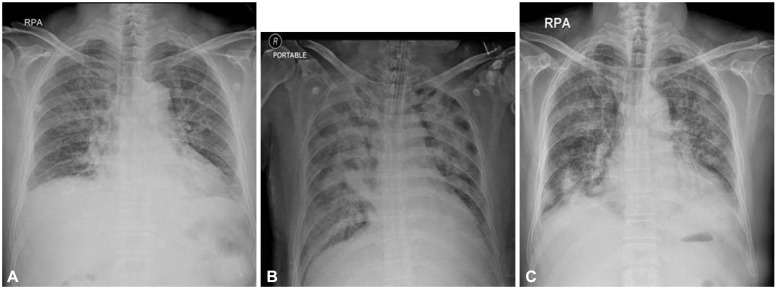
On the third day after admission, the patient coughed up bloody sputum and had a fever. The chest radiograph showed mild infiltration of both upper lung fields (Fig. 2A). We diagnosed pneumonia and administered piperacillin/tazobactam. The patient's vital signs, symptoms, and cardiac markers improved; then the patient was transferred to the general ward.
Fig. 2.
Chest radiographs on the third day after admission (A), after acute respiratory distress thereby showing diffuse alveolar hemorrhage on both lung field (B) and showing decreased infiltration on both lung field on the seventeenth day (C).
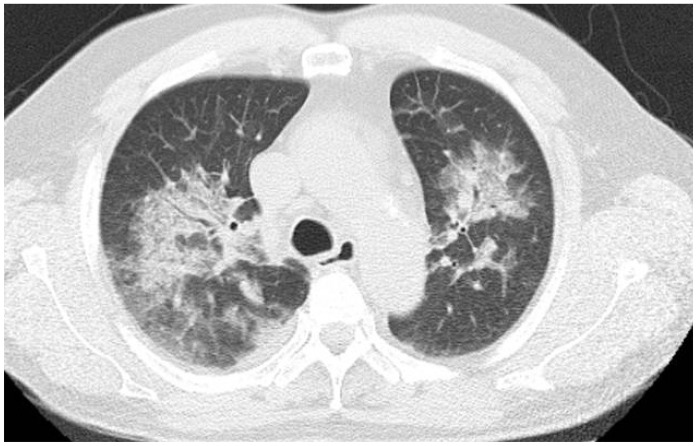
On the sixth day after admission, the patient complained of dyspnea and continuous bloody sputum. Chest computed tomography with enhancement showed patchy areas of ground-glass opacity in a central distribution in both upper lobes (Fig. 3). The findings were consistent with diffuse alveolar hemorrhage. We considered triple antiplatelet therapy as the most likely cause. We discontinued cilostazol and carried out a study to discriminate between alveolar hemorrhage caused by antiplatelet therapy and alveolar hemorrhage due to a different disease. Anti-phospholipid antibody, anti-cardiolipin antibody, P-antinuclear and antineutrophil cytoplasmic autoantibodies (ANCA), C-ANCA, ANA, complement 3, complement 4, anti-ds deoxyribonucleic acid antibody, anti-Leptospira antibody were all negative. The patient's platelet count was 257000/mm3.
Fig. 3.
Chest computed tomography on the sixth day after admission shows diffuse alveolar hemorrhage on both lung fields.
On the eleventh day after admission, the patient suddenly fell into acute respiratory failure and was transferred to the CCU. We intubated the patient. The chest radiograph showed diffuse infiltration in both lung fields (Fig. 2B). Bronchoscopy revealed diffuse hemorrhage of the bronchial walls in the bilateral lung fields. We discontinued clopidogrel on the ninth day after admission.
On the seventeenth day after admission, his symptoms improved and we extubated the patient. The chest radiograph showed decreased infiltration of both the lung fields (Fig. 2C). The patient was transferred to the general ward. The patient wanted to be transferred to another hospital. On the third day after the transfer, the patient died of ventricular fibrillation at the hospital to which he had been transferred.
Discussion
Diffuse alveolar hemorrhage is a syndrome characterized by bleeding into the alveolar spaces. In general, the causes of pulmonary alveolar hemorrhage are Wegener's granulomatosis, microscopic polyangitis, Goodpasture's syndrome, antiphospholipid antibody syndrome, infection, toxin, pulmonary embolism, mitral stenosis, and malignancy. Diffuse alveolar hemorrhage associated with antiplatelet drugs is a very rare and serious complication.
In the present case, triple antiplatelet therapy with aspirin, clopidogrel, and cilostazol was started at first, but alveolar hemorrhage improved after the discontinuation of clopidogrel. Therefore, this patient's alveolar hemorrhage was likely associated with clopidogrel.
The combination of clopidogrel and aspirin decreases long-term cardiac events in patients with acute coronary syndrome undergoing PCI. The current treatment guidelines for ST elevation myocardial infarction recommend that clopidogrel should be given for at least 12 months.7) However, the use of multiple antithrombotic drugs increases the risk of major bleeding.8) Pulmonary alveolar hemorrhage is a very rare complication among the major bleeding events. It has been reported primarily in patients that receive glycoprotein IIb/IIIa inhibitors in combination with other antiplatelet agents.9) Thus far, there have only been limited reports of pulmonary alveolar hemorrhage caused solely by dual antiplatelet therapy without glycoprotein IIb/IIIa inhibitors. Kilaru et al.10) reported the first case of diffuse alveolar hemorrhage developing after clopidogrel therapy given for placement of a coronary stent. Recently, Ikeda et al.11) reported a case of diffuse pulmonary hemorrhage developing after combination therapy with aspirin and ticlopidine following coronary stent implantation for ST elevation myocardial infarction.
This case highlights that antiplatelet treatment including aspirin and clopidogrel may lead to rare, life-threatening alveolar hemorrhage. Therefore, physicians should carefully observe patients and discontinue antithrombotic agents if an alveolar hemorrhage is suspected.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003;108:1682–1687. doi: 10.1161/01.CIR.0000091201.39590.CB. [DOI] [PubMed] [Google Scholar]
- 2.Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010;376:1233–1243. doi: 10.1016/S0140-6736(10)61088-4. [DOI] [PubMed] [Google Scholar]
- 3.Chae SC. Antiplatelet agents in high-risk patients with coronary artery disease. Korean Circ J. 2004;34:23–27. [Google Scholar]
- 4.Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation. 2004;110:1202–1208. doi: 10.1161/01.CIR.0000140675.85342.1B. [DOI] [PubMed] [Google Scholar]
- 5.Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170:1433–1441. doi: 10.1001/archinternmed.2010.271. [DOI] [PubMed] [Google Scholar]
- 6.Payne DA, Hayes PD, Jones CI, Belham P, Naylor AR, Goodall AH. Combined therapy with clopidogrel and aspirin significantly increases the bleeding time through a synergistic antiplatelet action. J Vasc Surg. 2002;35:1204–1209. doi: 10.1067/mva.2002.122027. [DOI] [PubMed] [Google Scholar]
- 7.Kushner FG, Hand M, Smith SC, Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006;114:774–782. doi: 10.1161/CIRCULATIONAHA.106.612812. [DOI] [PubMed] [Google Scholar]
- 9.Ener RA, Bruno N, Dadourian D, et al. Alveolar hemorrhage associated with platelet glycoprotein IIb/IIIa receptor inhibitors. J Invasive Cardiol. 2006;18:254–261. [PubMed] [Google Scholar]
- 10.Kilaru PK, Schweiger MJ, Kozman HA, Weil TR. Diffuse alveolar hemorrhage after clopidogrel use. J Invasive Cardiol. 2001;13:535–537. [PubMed] [Google Scholar]
- 11.Ikeda M, Tanaka H, Sadamatsu K. Diffuse alveolar hemorrhage as a complication of dual antiplatelet therapy for acute coronary syndrome. Cardiovasc Revasc Med. 2011;12:407–411. doi: 10.1016/j.carrev.2011.03.003. [DOI] [PubMed] [Google Scholar]