Abstract
Hydrodynamically balanced systems (HBSs) of ofloxacin were prepared using lactose, HPMC K4M, PVP K 30, and liquid paraffin, which may increase the mean residence time in the gastrointestinal tract, and may be able to provide maximum drug at the site of absorption to improve oral bioavailability. All these formulated HBS capsules were floated well over 6 h with no floating lag time. They also showed sustained drug release over 6 h. Time for 50% release of ofloxacin was within the range, 2.47 ± 0.02 to 3.07 ± 0.08 h. The in vitro drug release from these HBS capsules was dependent on HPMC K4M, PVP K 30, and liquid paraffin content. The drug release pattern of these HBS capsules containing ofloxacin followed the Higuchi model with the anomalous transport mechanism.
Keywords: Hydrodynamically balanced system, Gastroretention, Drug release, HPMC K4M, Ofloxacin, Capsules
1. Introduction
Oral controlled-release drug delivery technology represents one of the frontier areas of science, involving multidisciplinary scientific approaches that all contribute to human healthcare. The challenge in the development of oral controlled-release drug delivery systems is not just to sustain the drug release, but also to prolong the gastric residence of dosage forms until all the drug is completely released at the desired period (Tadros, 2010). Prolonged gastric residence increases duration of drug release, and reduces drug waste with improved bioavailability (Garg and Gupta, 2008; Nayak et al., 2010b; Nayak et al., 2010c). Apart from these advantages, gastric residence of dosage forms offer various pharmacokinetic advantages like maintenance of constant therapeutic levels over a prolonged period, and thus, reduction in fluctuation in therapeutic levels minimizing the risk of resistance especially in the case of antibiotics. Over the past few decades, several gastroretentive drug delivery approaches are being designed and developed, including floatation (Sing and Kim, 2000; Arrora et al. 2005), mucoadhesion (Chowdary and Rao, 2004; Nayak et al., 2010a), sedimentation (Rouge et al. 1998), unfoldable, expandable, or swellable systems (Klausner et al., 2003), superporous hydrogel systems (Chen et al., 2000), magnetic systems (Fujimori et al., 1994) etc. Among them, floating drug delivery presents a number of applications for drugs having poor bioavailability because of the narrow absorption window in the upper part of gastrointestinal tract. It retains the dosage form at the site of absorption and thus enhances the bioavailability (Ali et al., 2007).
Ofloxacin (9-fluoro-2, 3-dihydro-3-methyl-10 (4-methyl-1-piperazinyl)-7-oxo-7H pyrido [1,2,3-de]-1,4-benzoxazine-6-carboxylic acid) is a synthetic fluroquinolone derivative, which acts by inhibiting the topoisomerase enzyme which is essential in the reproduction of the bacterial DNA (Tripathy, 2003). Ofloxacin is highly sensitive to both Gram-positive and Gram-negative bacteria. It is also active against mycoplasma, chlamydia and legionella. While widely used to treat infections, such as those affecting the gastrointestinal and respiratory tracts, it is also used to treat urinary tract infections (Zivanovic et al., 2006; Cui et al., 2008). It is highly soluble in acidic media and precipitates in alkaline media thereby losing its solubility. Hence, gastroretentive floating systems of ofloaxcin should enhance the bioavailability by retaining it in the acidic environment of the stomach. Few investigations have also been carried out to develop and evaluate gastroretentive floating systems of ofloaxcin (Janardhan et al., 2009; Semalty et al., 2010).
Among various gastroretentive floating systems, hydrodynamically balanced systems (HBSs) are able to improve absorption of drugs especially those that are absorbed from stomach and small intestine (Seth and Tossounian, 1984; Sahni et al., 2006). HBSs contain drug with gel-forming hydrocolloids meant to remain buoyant in the stomach content. They are mainly single-unit dosage forms, and are usually composed of one or more gel-forming hydrophilic polymeric substances and an active pharmaceutical ingredient (Dorozynski et al., 2007). Various gastroretentive HBSs for some drug candidates have already been investigated (Sahni et al., 2006; Ali et al. 2007; Dorozynski et al., 2007; Salunke et al., 2009; Wason and Nanda, 2009; Wamorkar et al., 2010). Ali et al. have investigated ofloxacin HBS capsules for gastroretentive delivery using HPMC and polyethylene oxide (Ali et al., 2006). In the present investigation, we have planned to develop HBS capsules of ofloxacin using lactose, hydroxypropyl methylcellulose (HPMC K4M), polyvinyl pyrrolidone (PVP K 30), and liquid paraffin for better delivery of ofloxacin. These HBS capsules of ofloxacin would remain buoyant on the gastric fluid for a prolonged period and the drug would be available in the dissolved form at the main site of its absorption, which leads to improved bioavailability of the drug.
2. Materials and methods
2.1. Materials
Ofloxacin (Klar Sehen Pvt. Ltd., India), hydroxypropyl methylcellulose K4M (Central Drug House, India), liquid paraffin (light, 25–80 mPa viscosity at 20 °C) (Nice Chemicals Pvt. Ltd., India), polyvinyl pyrrolidone K 30 and lactose (Lobochemie, India) were used. All other chemicals and reagents used were of analytical grade.
2.2. Preparation of ofloxacin HBS capsules
Ofloxacin HBS capsules were prepared by simple blending of 100 mg of ofloxacin, with lactose and different polymers like HPMC K4M, PVP K 30, and liquid paraffin. Magnesium stearate as lubricating agent was added to the blend and mixed for additional 3 min. Solid filling was done to fill the final blend above components into empty hard gelatin capsules (size 0) manually. Care was taken to fill the contents completely to maintain the uniformity of contents and weight. The composition of ofloxacin HBS capsules is given in Table 1.
Table 1.
Composition of various HBS ofloxacin capsules.a
| Formulation codes | Components (mg) |
|||||
|---|---|---|---|---|---|---|
| Ofloxacin | Lactose | HPMC K4MK4M | PVP K 30 | Liquid paraffin | Magnesium stearate | |
| F 1 | 100 | 45 | 100 | – | – | 5 |
| F 2 | 100 | 45 | 80 | 20 | – | 5 |
| F 3 | 100 | 45 | 80 | – | 20 | 5 |
| F 4 | 100 | 45 | 80 | 10 | 10 | 5 |
Solid filling was done for filling above components in capsules.
2.3. Evaluation of in vitro floating properties
The HBS capsules were immersed in 900 ml of 0.1 N HCl, pH 1.2 in USP type II apparatus at 50 rpm maintained at 37 ± 5 °C for 6 h. The time for which the capsules constantly remain afloat on the surface of the medium (buoyant) was observed visually and was taken as the floating time.
2.4. In vitro drug release studies
In vitro drug release studies were carried in USP type II apparatus at 50 rpm maintained at 37 ± 5 °C. A single HBS capsule was transferred into the dissolution medium of 900 ml of 0.1 N HCl, pH 1.2. Then 5 ml of aliquots was withdrawn from the dissolution vessel at specific time intervals and replaced with equivalent volume of fresh medium. Collected dissolution samples were filtered using Whatmann filter (Grade I) paper and then, used for determination of released ofloxacin concentrations by using a UV–vis spectrophotometer (U.V. 2440 Double beam spectrophotometer, SHIMADZU Corporation, Japan) against a blank. Maximum wavelength (λmax) was obtained by scanning all samples from 200 to 400 nm and this was 291 nm. Three repetitions were done for each formulation.
2.5. Drug release kinetics
The in vitro drug release data from various HBS capsules were evaluated kinetically in various mathematical models like zero order, first order, Higuchi, and Korsmeyer–Peppas models (Higuchi, 1961; Korsmeyer et al., 1983; Mulye and Turco, 1996; Varelas et al., 1995).
Zero-order Model: F = K0 t, where F represents the fraction of drug released in time t, and KO is the apparent release rate constant or zero-order release constant.
First-order Model: ln (1−F) = −K1st t, where F represents the fraction of drug released in time t, and K1 is the first-order release constant.
Higuchi Model: F = KH t½, where F represents the fraction of drug released in time t, and KH is the Higuchi dissolution constant.
Korsmeyer–Peppas Model: F = KP tn, where F represents the fraction of drug released in time t, KP is the rate constant and n is the diffusional exponent, this indicates the drug release mechanism.
2.6. Statistical analysis
The time for 50% release of ofloxacin from HBS capsules was analyzed for significant differences by one-way analysis of variance (ANOVA) using a Student-Newman-Keuls test for all pair wise comparisons in this study. The statistical analysis was conducted using MedCalc software version 9.6.4.0.
3. Results and discussion
All these HBS capsules containing ofloxacin were floated well with no floating lag time. The floating time of these ofloxacin HBS capsules was more than 6 h (Fig. 1). This may be accounted to increased gel strength of the polymeric combination matrices with drug in the form of HBS capsules. The mechanism involved in buoyancy of these HBS capsules, could be rapid hydration and swelling of the polymeric matrices producing a floating mass in the gastric pH (1.2). The matrix integrity of these HBS capsules was satisfactory.
Figure 1.
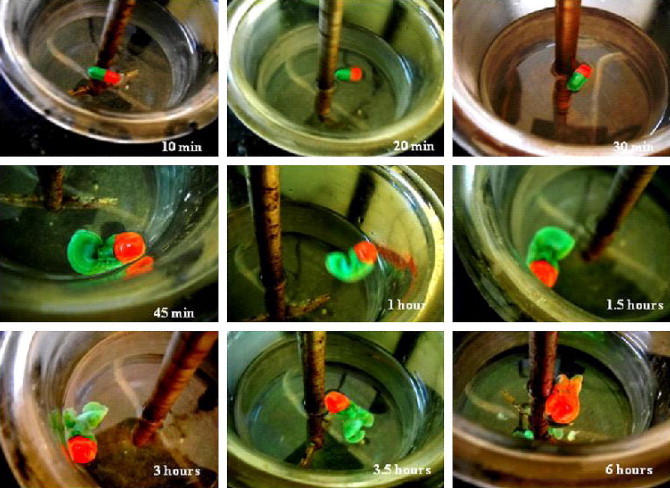
Floating behavior of HBS ofloxacin capsules (F 4) in 0.1 N HCl, pH 1.2.
In vitro drug release studies were carried out in 0.1 N HCl, pH 1.2, as dissolution medium. All these HBS ofloxacin capsules showed sustained drug release over 6 h (Fig. 2). Time for 50% release of ofloxacin from HBS capsules was calculated from the plot of percentage drug release vs. time and presented in Table 2. Time for 50% release of ofloxacin was higher (3.27 ± 0.04 h) in the case of HBS capsules of formulation F 3, whereas this was lower (2.47 ± 0.02 h) in the case of HBS capsules of formulation F 2. There were significant differences (p < 0.05) in the time for 50% release of ofloxacin from HBS capsules. As HPMC K4M content in HBS capsules was increased, the drug release rate from HBS capsules was sustained and vice-versa. The higher viscosity due to higher content of HPMC K4M may promote the formation of highly viscous gels upon contact with aqueous fluids. This would retard the drug release rate from these HBS ofloxacin capsules containing higher HPMC K4M content. In a parallel line, Siepmann and Peppas (Siepmann and Peppas, 2001) suggested that the drug release from HPMC matrices is sequentially governed as follows: (i) At the beginning, steep water concentration gradients are formed at the polymer/water interface resulting in water imbibition into the matrix; (ii) Due to the imbibition of water, HPMC swells resulting in dramatic changes of polymer, drug concentrations and increasing dimensions of the system; (iii) Upon contact with water, the drug dissolves and diffuses out of the device due to concentration gradient; and (iv) With increasing water content, the diffusion coefficient of the drug increases substantially. Ofloxacin capsules containing PVP K 30 showed higher drug release rates than other formulations; whereas, liquid paraffin containing capsules gave a more sustained drug release rate than other formulations. As liquid paraffin content in HBS capsules was increased, the drug release rate from these HBS capsules was decreased more. Thus, liquid paraffin was the best release modifier amongst those excipients evaluated.
Figure 2.
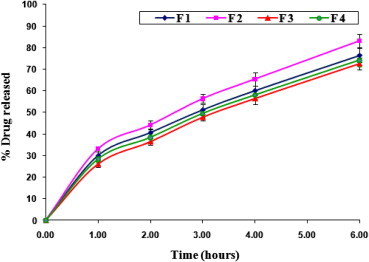
In vitro ofloxacin release from various HBS capsules in 0.1 N HCl, pH 1.2 (Mean ± SD).
Table 2.
Times for 50% release of ofloxacin from HBS capsules in 0.1 N HCl (pH 1.2), calculated from the plot of percentage drug release vs. time.
| Formulation codes | Times for 50% release of ofloxacin from HBS capsules (h) a,b |
|---|---|
| F 1 | 2.89 ± 0.02 |
| F 2 | 2.47 ± 0.02 |
| F 3 | 3.27 ± 0.04 |
| F 4 | 3.07 ± 0.08 |
Mean ± SD.
Values were significantly different from each other. Statistically significance (p < 0.05) compared with all formulations was determined by one-way ANOVA followed by using Student-Newman-Keuls test for all pair wise comparisons.
To analyze the mechanism of drug release from these HBS capsules, the in vitro dissolution data were fitted to various mathematical models like zero order, first order, Higuchi, and Korsmeyer–Peppas models. The results of the curve fitting into these above-mentioned mathematical models are given in Table 3. The drug release pattern of these HBS capsules followed Higuchi model (R2 = 0.9942–0.9962), and this was observed to be closest to Korsmeyer–Peppas model (R2 = 0.9916–0.9955). Again, the Korsmeyer–Peppas model has been employed in the in vitro drug release behavior analysis of various pharmaceutical formulations to distinguish between various competing release mechanisms: Fickian release (diffusion-controlled release), non-Fickian release (anomalous transport), and case-II transport (swelling-controlled release). When n takes the value 0.5 it indicates diffusion-controlled drug release and for the value 1.0 indicates swelling-controlled drug release. Values of n between 0.5 and 1.0 can be regarded as an indicator for both the phenomena (anomalous transport). These extreme values for the exponent n, 0.5 and 1.0, are only valid for slab geometry and for spheres and cylinders different values have been derived (Blagoeva and Nedev, 2006). For a capsule, a cylindrical geometry is considered for the determination of values of n for all these HBS ofloxacin capsules. The values of n were within the range of 0.5148–0.5816 indicating anomalous transport. This could be attributed to the high water uptake by these capsule matrixes leading to higher swelling of these capsules that supported the anomalous release mechanism of ofloxacin (Chavanpatil et al., 2006).
Table 3.
Results of curve fitting of the in vitro ofloxacin release data in 0.1 N HCl (pH 1.2) from different HBS capsules.
| Formulation codes | Correlation coefficient (R2) values |
|||
|---|---|---|---|---|
| F 1 | F 2 | F 3 | F 4 | |
| Zero order Model | 0.9848 | 0.9854 | 0.9920 | 0.9849 |
| First order Model | 0.9871 | 0.9791 | 0.9746 | 0.9818 |
| Higuchi Model | 0.9962 | 0.9942 | 0.9951 | 0.9949 |
| Korsmeyer-Peppas Model | 0.9955 | 0.9916 | 0.9921 | 0.9933 |
| Diffusion exponent (n) | 0.5159 | 0.5148 | 0.5816 | 0.5415 |
4. Conclusion
Gastroretentive HBS capsules of ofloxacin were prepared using lactose, HPMC K4M and liquid paraffin. All these formulated HBS capsules were floated well over 6 h with no floating lag time. They also showed sustained drug release in 0.1 N HCl, pH 1.2 over 6 h. Time for 50% release of ofloxacin was within the range, 2.47 ± 0.02 to 3.27 ± 0.04 h. In addition, there were significant differences (p < 0.05) in the times for 50% release of ofloxacin from all these HBS capsules. The in vitro drug release from these HBS capsules was dependent on HPMC K4M, PVP K 30, and liquid paraffin content. The drug release pattern of these HBS capsules containing ofloxacin followed Higuchi model with the anomalous transport mechanism.
Footnotes
Peer review under responsibility of King Saud University.
References
- Ali J., Arora S., Ahuja A., Babbar A.K., Sharma R.K., Khar R.K., Baboota S. Formulation and development of hydrodynamically balanced system for metformin: In vitro and in vivo evaluation. Eur. J. Pharm. Biopharm. 2007;67:196–201. doi: 10.1016/j.ejpb.2006.12.015. [DOI] [PubMed] [Google Scholar]
- Ali J., Hasan S., Ali M. Formulation and development of gastroretentive drug delivery system for ofloxacin. Methods Find. Exp. Clin. Pharmacol. 2006;28:1–7. doi: 10.1358/mf.2006.28.7.1003574. [DOI] [PubMed] [Google Scholar]
- Arrora S., Ali J., Khar R.K., Baboota S. Floating drug delivery systems: A review. AAPS PharmSciTech. 2005;6(3):372–390. doi: 10.1208/pt060347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blagoeva R., Nedev A. Monolithic controlled delivery systems: Part II. Basic mathematical models. Bioautomation. 2006;5:106–117. [Google Scholar]
- Chavanpatil M.D., Jain P., Chaudhari S., Shear R., Vavia P.R. Novel sustained release, swellable and bioadhesive gastroretentive drug delivery system for ofloxacin. Int. J. Pharm. 2006;316:86–92. doi: 10.1016/j.ijpharm.2006.02.038. [DOI] [PubMed] [Google Scholar]
- Chen J., Blevins W.E., Park H., Park K. Gastric retention properties of superporous hydrogel composites. J. Control. Release. 2000;65:73–82. doi: 10.1016/s0168-3659(99)00139-x. [DOI] [PubMed] [Google Scholar]
- Chowdary K.P.R., Rao Y.S. Mucoadhesive microspheres for oral controlled drug delivery. Biol. Pharm. Bull. 2004;27:717–1724. doi: 10.1248/bpb.27.1717. [DOI] [PubMed] [Google Scholar]
- Cui Y., Zhang Y., Tang X. In vitro and in vivo evaluation of ofloxacin sustained release pellets. Int. J. Pharm. 2008;360:47–52. doi: 10.1016/j.ijpharm.2008.04.014. [DOI] [PubMed] [Google Scholar]
- Dorozynski, P., Kulinowski, P., Jachowicz, R. and Jasinski, A. (2007). Development of a simultaneous studies and magnetic resonance imaging of water transport in hydrodynamically balanced systems: A technical note. AAPS PharmSciTech. 8(1): Article 15. [DOI] [PubMed]
- Fujimori J., Machida Y., Nagai T. Preparation of a magnetically-responsive tablet and configuration of its gastric residence in beagle dogs. STP Pharma. Sci. 1994;4:425–430. [Google Scholar]
- Garg R., Gupta G.D. Progress in controlled gastroretentive delivery systems. Trop. J. Pharm. Res. 2008;7(3):1055–1066. [Google Scholar]
- Higuchi T. Rate of release of medicaments from ointment bases containing drugs in suspension. J. Pharm. Sci. 1961;50:874–875. doi: 10.1002/jps.2600501018. [DOI] [PubMed] [Google Scholar]
- Janardhan D., Sreekanth J., Bharat V., Subramaniyan P.R. Formulation and evaluation of gastro retentive drug delivery system for ofloxacin. Int. J. Pharm. Sci. Nanotechnol. 2009;2(1):428–434. [Google Scholar]
- Klausner E.A., Lavy E., Friedman M., Hoffman A. Expandable gastroretentive dosage forms. J. Control. Release. 2003;90:143–162. doi: 10.1016/s0168-3659(03)00203-7. [DOI] [PubMed] [Google Scholar]
- Korsmeyer R.W., Deolkar G.E.P., Peppas N.A. Mechanisms of potassium chloride from compressed, hydrophilic, polymeric matrices: effect of entrapped air. J. Pharm. Sci. 1983;72:1189–1191. doi: 10.1002/jps.2600721021. [DOI] [PubMed] [Google Scholar]
- Mulye N.V., Turco S.T. An examination of assumptions underlying the first-order kinetic model for release of water soluble drugs from dicalcium phosphate dehydrate matrices. Drug Dev. Ind. Pharm. 1996;22(7):673–679. [Google Scholar]
- Nayak A.K., Hasnain M.S., Beg S., Alam M.I. Mucoadhesive beads of gliclazide: Design, development, and evaluation. Sci. Asia. 2010;36:319–325. [Google Scholar]
- Nayak A.K., Maji R., Das B. Gastroretentive drug delivery systems: a review. Asian J. Pharm. Clin. Res. 2010;3(1):2–10. [Google Scholar]
- Nayak A.K., Malakar J., Sen K.K. Gastroretentive drug delivery technologies: Current approaches and future potential. J. Pharm. Educ. Res. 2010;1(2):1–12. [Google Scholar]
- Rouge N., Allemann E., Gex-Fabry M., Balant L., Cole E.T., Buri P., Doelker E. Comparative pharmacokinetic study of a floating multiple-unit capsule, a high density multiple-unit capsule and an immediate-release tablet containing 25 mg atenolol. Pharm. Acta Helbetiae. 1998;73:81–87. doi: 10.1016/s0031-6865(97)00050-2. [DOI] [PubMed] [Google Scholar]
- Sahni J.K., Ahmad F.J., Ahuja A., Khar R.K. Formulation and evaluation of a hydrodynamically balanced system of paracetamol. The Indian Pharmacist. 2006;(46):64–66. [Google Scholar]
- Salunke, R.J., Shahi, S.R. and Atram, S.C. (2009). Formulation and evaluation of hydrodynamically balanced system of ciprofloxacin HCl. Int. J. Pharm. Res. Dev. 7: Article 001.
- Semalty M., Yadav S., Semalty A. Preparation and characterization of gastroretentive floating microspheres of ofloxacin hydrochloride. Int. J. Pharm. Sci. Nanotechnol. 2010;3(1):819–823. [Google Scholar]
- Seth P.R., Tossounian J. The hydrodynamically balanced system, a novel drug delivery system for oral use. Drug Dev. Ind. Pharm. 1984;10:313–339. [Google Scholar]
- Siepmann J., Peppas N.A. Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC) Adv. Drug Del. Rev. 2001;48:139–157. doi: 10.1016/s0169-409x(01)00112-0. [DOI] [PubMed] [Google Scholar]
- Sing B.N., Kim K.H. Floating drug delivery systems: an approach to oral controlled drug delivery via gastric retention. J. Control. Release. 2000;63:235–259. doi: 10.1016/s0168-3659(99)00204-7. [DOI] [PubMed] [Google Scholar]
- Tadros M.I. Controlled-release effervescent floating matrix tablets of ciprofloxacin hydrochloride: Development, optimization and in vitro–in vivo evaluation in healthy human volunteers. Eur. J. Pharm. Biopharm. 2010;74:332–339. doi: 10.1016/j.ejpb.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Tripathy, K.D. (2003). Sulfonamides, cotrimoxazole and qunolones. In: Essentials of Medical Pharmacology. 5th edition, section 12, chapter 48, Jaypee Brothers Medical Publishers (P) Ltd. New Delhi, India, pp. 646-652.
- Varelas C.G., Dixon D.G., Steiner C. Zero-order release from biphasic polymer hydrogels. J. Control. Release. 1995;34:185–192. doi: 10.1016/s0168-3659(97)00182-x. [DOI] [PubMed] [Google Scholar]
- Wamorkar V.V., Varmal M.M., Vijay Kumar B., Reddy V.M. Effect of hydrophilic and hydrophobic polymers and in vitro evaluation of hydrodynamically balanced system of metoclopramide hydrochloride. Int. J. Pharm. Sci. Nanotechnol. 2010;3(3):1129–1135. [Google Scholar]
- Wason R., Nanda A. Development and optimization of a gastroretentive FDDS using ciprofloxacin hydrochloride. The Indian Pharmacist. Dec: 2009:81–89. [Google Scholar]
- Zivanovic L., Zigic G., Zecevic M. Investigation of chromatographic conditions for the separation of ofloxacin and its degradation products. J. Chromatogr. A. 2006;1119:224–230. doi: 10.1016/j.chroma.2006.02.029. [DOI] [PubMed] [Google Scholar]



