Abstract
Factors associated with antibiotic use, resistance and safety have been well recognized worldwide in the literature. Nevertheless, only few studies have been conducted in Jordan in this area. The aim of this study was to assess knowledge, behavior and attitude toward antibiotics use among adult Jordanians. The study represents a cross sectional survey using an interviewer administered questionnaire. Data collected from a random sample of 1141 adult Jordanians, recruited at different settings, regarding their knowledge about the effectiveness of, resistance toward, and self medications with antibiotics against bacterial, viral and parasitic diseases. 67.1% believed that antibiotics treat common cold and cough. 28.1% misused antibiotics as analgesics. 11.9% of females showed inadequate knowledge about the safe use of antibiotics during pregnancy and nursing. 28.5% kept antibiotics at home for emergency use and 55.6% use them as prophylaxis against infections. 49.0% use left-over antibiotics without physicians’ consultation while 51.8% use antibiotics based on a relative advice. 22.9% of physicians prescribe antibiotics over the phone and >50.0% routinely prescribe antibiotics to treat common cold symptoms.
Our findings indicated that young adults showed unsatisfactory knowledge of proper antibiotic use. Therefore, there is an urge for educational programs using all media means.
Keywords: Antibiotics misuse, Self medication, Microbial resistance, Left-over antibiotics, Prophylaxis, Antibiotics’ indications
1. Introduction
Antibiotics are considered among the most commonly sold drug classes in the developing countries (Buke et al., 2003). The irrational and overuse of antibiotics result not only in the emergence of resistant bacterial strains but also in adverse reactions and economical burden on national health system (Gyssens, 2001). This irrational use arises from the economical factors, health policies concerning medical insurance, lack of physicians’ concerns about long term resistance and effect versus treating current symptoms, pharmaceutical marketing and the sale of antibiotics without prescription in some countries (Metlay et al., 1998; McManus et al., 1997).
In Jordan, patients visit a community pharmacy to purchase a pharmaceutical product much like they would at a supermarket. Also, like most other developing countries, having a valid prescription is not always enforced for receiving prescription-only drugs (POM). With the exception of narcotics and major tranquilizers, patients can buy any medication, including antibiotics, without a prescription (Shankar et al., 2002).
Previous researches in Jordan revealed different patterns of inappropriate antibiotics prescription and dispensing (Al-Bakri et al., 2005, Al-Azzam et al., 2007, Sawair et al., 2009a). Moreover, research has shown that the prevalence of self-medication with antibiotics in Jordan is alarmingly high (Al-Azzam et al., 2007; Sawair et al., 2009a). The prescribing practices of practitioners are not regulated (Al-Momany et al., 2009; Dar-Odeh et al., 2010) and regulatory laws that prevent unprescribed dispensing of antibiotics to the adult do exist but are not enforced in community pharmacies (Albsoul-Younes et al., 2010, Yousef et al., 2008). All of these factors highlight the need for exploring and tackling such health practices.
The aim of this study was to investigate the level of knowledge, behavior, and attitude of adults (over 18 years old) living in Jordan concerning the use, awareness about resistance toward and self-medication.
2. Materials and methods
This study was carried out using a cross-sectional design; a pretested, pre-validated structured and anonymous questionnaire was administered to a sample of 1500 Jordanian adults (anybody who appeared to be 18 years old or above) after obtaining verbal informed consent to participate in the study. In order to achieve generalizability of the sample, research assistants interviewed members of the general public at different study sites (e.g. shopping malls, supermarkets, The University of Jordan cafeteria, gyms, female beauty centers, etc.). The research assistants collected the questionnaire from respondents after completion on the spot. The questionnaire was developed by reviewing available questionnaires in the literature (Buke et al., 2005; Chen et al., 2005; You et al., 2008). Comparability with those surveys and the validity of the instrument were important factors in determining which questions to be included in this survey. Every effort was made during the literature review to ensure content validity. Moreover, various drafts of the questionnaire were evaluated individually by two clinical pharmacists, one statistician and one sociologist in order to ensure face validity and to be applicable to Jordan. To facilitate data collection, the questionnaire was translated from English into Arabic and back into English by two individuals who are fluent in both languages. The amended Arabic version questionnaire was then handled to the research assistants and then to the respondents. Additionally, a preliminary test was applied on representative sample (around 3% of the target sample) (n = 45) to address any ambiguity in the questions and to determine whether the data would provide reliable information. Data collected during this pilot part of the study were excluded from the final data analysis.
Consequently 33 revised questions were used in the questionnaire. Data were collected between February and June 2009. In this study, demographic data of the respondents such as sex, age, monthly household income, and education level were explored as shown in Table 1. Education was categorized as low (incomplete primary education, completed primary education and lower vocational or general education) or high (intermediate or higher vocational or general education, college or university). In addition, participant’s perception and behavior regarding antibiotics use were evaluated based on four areas
-
1.
Knowledge regarding the indications for antibiotic use: The purpose of using antibiotic (bacterial, viral or parasitic infection, common cold or nasal congestion, stomachache and combination of the above).
-
2.
Resistance due to misuse: Causes of antibiotic resistance (unnecessary use, not completing the course, no physician’s prescription (e.g. self-medication; over-the-counter OTC), using antibiotic with other drugs).
-
3.
Safety: Antibiotic side effects such as allergies and the potential harm to children’s teeth.
-
4.
Antibiotics’ prescription patterns: Obtaining antibiotic prescription (requesting prescription from one’s own physician or consulting other physician to obtain one, over the phone prescription and improper reasons of prescription).
Table 1.
Demographic characteristics of the 1141 respondents in Jordan.
| Gender (N = 1141) | Number | Percentage |
|---|---|---|
| Female | 809 | 70.9 |
| Male | 332 | 29.1 |
| Age (N = 1127)a | ||
| 18–25 | 612 | 54.3 |
| 26–35 | 274 | 24.3 |
| 36–45 | 101 | 9.0 |
| >45 | 140 | 12.4 |
| Marital status (N = 1141) | ||
| Single | 763 | 66.9 |
| Married | 350 | 30.7 |
| Divorced | 15 | 1.3 |
| Widowed | 13 | 1.1 |
| Education level (N = 1126)a | ||
| Low (bellow College) | 180 | 15.8 |
| High(College and above) | 943 | 82.9 |
| Income JDb(N = 1141) | ||
| <500 JD | 405 | 54.0 |
| >500 JD | 525 | 46.0 |
| Place of living (N = 1127)a | ||
| Capital (Amman) | 896 | 79.5 |
| All other cities | 231 | 20.5 |
Total number <1141 due to unanswered questions/missing data.
Jordanian Dinar (JD 0.71 = USD 1.0).
Responses were coded and entered into SPSS for Windows, version 16, for statistical analysis. Chi-square and Fisher exact tests were used to test for significant differences between groups (P < 0.05). Descriptive measures presented include percentages and corresponding 95% confidence intervals (CIs).
The knowledge concerning the aim of antibiotic use, resistance and safety between respondents was assessed by calculating the number of correct responses to nine statements with asterisks as shown in Table 2. Poor, adequate and good knowledge were defined as total knowledge scores of 1 (<50% correct response), 2 (50–70% correct response) and 3 (>70% correct response). Association of respondents’ knowledge score with sex, age, education level and income was analyzed using Chi-square test. 95% confidence intervals along with associated p-values were presented. P-values less than or equal 0.05 were considered significant.
Table 2.
The knowledge of respondent regarding antibiotic use.
| Statements evaluating indication and efficacy of antibiotics | Group Aa |
Group Bb |
Totalc |
P | |||
|---|---|---|---|---|---|---|---|
| Number/total | Percent agreeing | Number/total | Percent agreeing | Number/total | Percent agreeing | ||
| (A) The aim of antibiotic use for | |||||||
| - fever | 88/895 | 9.8 | 22/234 | 9.4 | 110/1129 | 9.7 | 0.08 |
| - viral infection | 69/895 | 7.7 | 9/234 | 3.8 | 78/1129 | 6.9 | 0.08 |
| - bacterial infection⁎ | 295/895 | 33.0 | 76/234 | 32.5 | 372/1129 | 32.9 | 0.08 |
| - parasitic infection | 9/895 | 1.0 | --------- | ------ | 9/1129 | 0.8 | 0.08 |
| - both viral and bacterial infections | 164/895 | 18.3 | 48/234 | 20.5 | 212/1129 | 18.8 | 0.08 |
| - bacterial, viral, parasitic and fever | 195/895 | 21.8 | 50/234 | 21.4 | 245/1129 | 21.7 | 0.08 |
| -Bacterial infection with fever | 25/895 | 2.8 | 4/234 | 1.7 | 29/1129 | 2.6 | 0.08 |
| -Viral infection with fever | 1/895 | 0.1 | 1/234 | 0.4 | 2/1129 | 0.2 | 0.08 |
| - common cold, cough and nasal congestion⁎ | 441/845 | 52.2 | 103/219 | 47.0 | 544/1064 | 51.1 | 0.44 |
| - Stomach ache⁎ | 253/895 | 28.3 | 65/232 | 28.0 | 318/1127 | 28.2 | 0.75 |
| - the treatment of sore throat | 306/851 | 36.0 | 12/161 | 7.5 | 318/937 | 33.9 | <0.01 |
| (B) An antibiotic will always be effective in the treatment of same infection in the future | 241/886 | 27.2 | 52/229 | 22.7 | 295/1116 | 26.4 | 0.27 |
| (C) Antibiotic resistance is due to: | |||||||
| - Using antibiotics when they are not necessary⁎ | 304/843 | 36.1 | 79/221 | 35.7 | 385/1068 | 36.0 | 0.26 |
| - Not completing the full course of antibiotic⁎ | 557/902 | 61.8 | 143/235 | 60.9 | 702/1141 | 61.5 | 0.75 |
| - Using antibiotic without physician prescription (Self medication)⁎ | 232/902 | 25.7 | 72/235 | 30.6 | 305/1141 | 26.7 | 0.37 |
| - Taking antibiotic before meal | 95/902 | 10.5 | 27/235 | 11.5 | 122/1141 | 10.7 | 0.82 |
| - Using antibiotic in febrile illness | 187/902 | 20.7 | 43/235 | 18.3 | 230/1141 | 20.2 | 0.72 |
| - Taking antibiotic with another drug (Drug-Drug interaction)⁎ | 101/902 | 11.2 | 22/235 | 9.4 | 124/1141 | 10.9 | 0.31 |
| - Using the same antibiotic with a different brand | 117/902 | 13.0 | 31/235 | 13.2 | 148/1141 | 13.0 | 0.95 |
| (D) Antibiotic safety | |||||||
| - Antibiotics could be harmful for children’s teeth⁎ | 595/896 | 66.4 | 116/233 | 49.8 | 762/1132 | 67.3 | 0.01 |
| - Antibiotic might develop allergy leading to death⁎ | 614/891 | 68.9 | 165/228 | 72.4 | 781/1122 | 69.6 | 0.01 |
Group A: respondents who reported receiving antibiotics during the last year.
Group B: respondents who reported not receiving antibiotic in the last year.
Total percentage denote those who answered the question and agreed with the statement.
Statement used in scoring respondents knowledge.
3. Results
A total of 1500 questionnaires were distributed, out of which 1141 were completed (response rate = 76.1%). The majority of respondents (70.9%) were female, out of which 612 (54.3%) were between 18 and 25 years old. Over half of the respondents (66.9%) were single. More than 3 out of 4 respondents (79.1%) were used antibiotic on an outpatient basis at least once during the past year (Group A). The demographic details of the sample are summarized in Table 1.
Almost one fifth (19.5%, CI 17.2–21.8)) of respondents used antibiotics more than three times in the past year. The frequency of antibiotic use by respondents in the past year is shown in Fig. 1a. Forty-one percent of respondents (40.9%, CI (38.1–43.8)) reported purchasing antibiotics from retail pharmacies using physician’s prescription, while almost one in every three respondents (30.0%, CI 27.3–32.6) reported obtaining antibiotics directly from pharmacies without a physician’s prescription (OTC) as shown in Fig. 1b which summarizes the sources of antibiotics obtained by respondents in the past year. Thirty-four percent (33.9%, CI 30.8–37.0 and 16.9% CI 14.4–19.3) of respondents in group A took antibiotics for sore throat and bronchitis, respectively, as shown in Fig. 1c.
Figure 1.
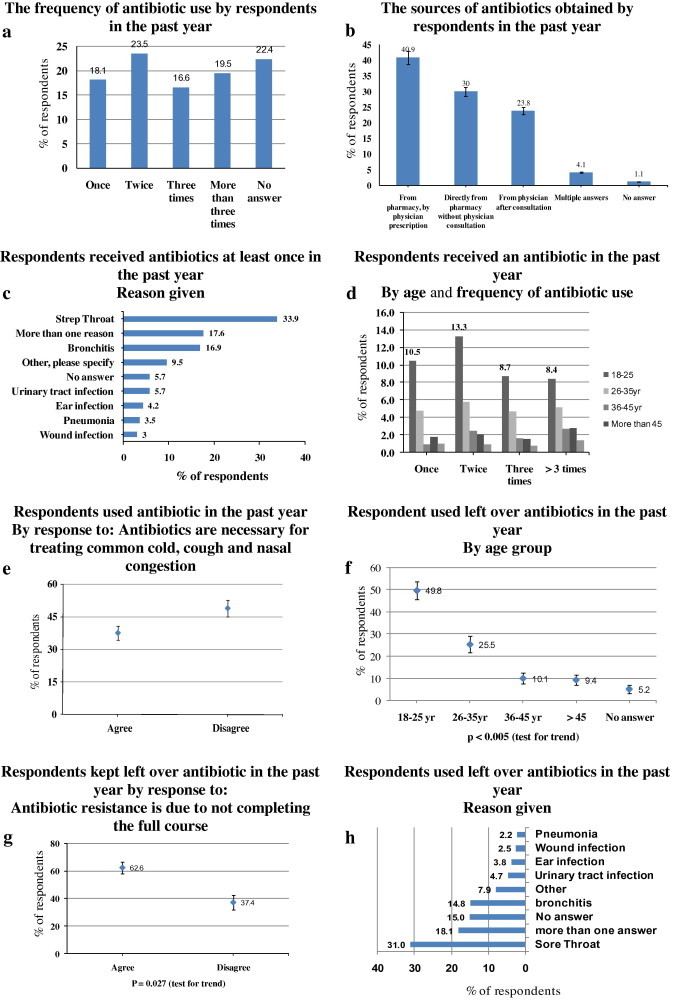
Antibiotic use and misuse.
The level of knowledge about the use, effectiveness, resistance and safety of antibiotics was evaluated using statements shown in Table 2. The numbers in Table 2 denote those who responded and agreed with the statements. Respondents were less knowledgeable about whether antibiotics were active against bacteria, viruses, and/or parasites. No significant difference in the level of knowledge about the effectiveness of antibiotics against common cold was noticed between respondents in Groups A and B. Of the total respondents, 32.9% agreed correctly that antibiotics are effective only against bacteria, whereas, 6.9% of respondents incorrectly agreed that antibiotics are effective against viruses. It is worth noting that 9.7% of the respondents believed that antibiotics were the same as antipyretic drugs used to decrease fever and 28.2% believed that they are similar to pain-killers used for stomachache. More than half of the respondents (51.1%, CI 48.1–54.1) agreed that antibiotics work on common cold, cough and nasal congestion.
In fact, one third of the respondents (38.5%, CI 35.7–41.4) agreed that antibiotics effectiveness would not be affected by antibiotic misuse (defined in this study as not completing the full course of antibiotic), and only 36.0% agreed that antibiotics would not be effective if they were overused (i.e. using antibiotics when they are not necessary).
Both the groups A and B awareness about antibiotics possible adverse effects was obviously very low, since one third of respondents (33.2%, P = 0.008) were unaware that certain antibiotics could be harmful for children’s teeth and 41.6% P = 0.013) disagreed with the statement ‘Antibiotics might develop allergy leading to patient death’.
Data on respondents’ behavior and attitude toward antibiotic use are shown in Table 3. Only 16.1% of respondents reported that they would take antibiotics before a meal and the majority (94.0%) reported taking antibiotic with water. Concerning storage, 48.3% did not store oral (Tablets or Capsule) antibiotics in a medicine cabinet.
Table 3.
Attitude and behavior towards antibiotic use among respondents.
| Statements evaluating attitude and behavior | Number | Percentage | 95% CI |
|---|---|---|---|
| When would you take antibiotics? | |||
| Before meal | 144/896 | 16.1 | 13.7–18.5 |
| With meal | 80/896 | 8.9 | 7.1–10.8 |
| After meal | 646/896 | 72.1 | 69.2–75.0 |
| Before or after (no preference) | 26/896 | 2.9 | 1.8–4.0 |
| How would you take antibiotics? | |||
| With water | 315/335 | 94.0 | 91.4–96.6 |
| With tea | 2/335 | 0.6 | −0.2–1.4 |
| With juice | 12/335 | 3.6 | 1.6–5.6 |
| Other methods | 6/335 | 1.8 | 0.–3.20 |
| In general, how do you store oral antibiotic/?tablets and capsules? | |||
| In a medicine cabinet | 577/1116 | 51.7 | 48.8–54.6 |
| On kitchen shelf | 131/1116 | 11.7 | 9.9–13.6 |
| In the refrigerator | 459/1116 | 41.1 | 38.2–44.0 |
| Females accepting to take antibiotics during pregnancy.84/708 | 11.9 | 9.5–14.2 | |
| Females accepting to take antibiotics during breastfeeding | 235/669 | 35.1 | 31.5–38.8 |
| Respondents asking their physicians for antibiotic allergy test | 258/1132 | 22.8 | 20.5–25.2 |
| Respondents keeping antibiotic at home for emergency for children | 320/1121 | 28.5 | 25.9–31.3 |
| Respondents using siblings (brothers and Sisters) antibiotics | 601/1125 | 53.4 | 50.5–56.3 |
| Respondents using antibiotics as a prophylaxis | A: 38/1125 | 55.6 | 52.7–58.5 |
| S: 462/1125 | |||
| N:625/1125 | |||
| Respondents using antibiotics on relative advice | A: 60/1064 | ||
| S: 454/1064 | |||
| N:551/1064 | 51.8 | 48.8–54.8 | |
| Respondents using left-over antibiotics without physician consultation | 554/1130 | 49.0 | 46.1–51.9 |
A/S/N: Always/Sometimes/Never.
Female attitude toward antibiotic use during pregnancy and lactation was also assessed. Twelve percent CI = (9.5, 14.2) of females agreed that antibiotics in general are safe to use during pregnancy and 35.1% agreed that antibiotics are safe to use during lactation. Only 22.8% of the respondents were aware of antibiotic allergy and requested an allergy test from their physicians.
Self-medication with antibiotics was one of the major issues to be evaluated in our study. Almost one third (28.5%, CI 25.9–31.3) of respondents kept antibiotics at home for emergency use for children younger than 12 years of age, and almost half (49.0%, CI 46.1–51.9) of respondents indicated that they did use left-over antibiotics (antibiotics remaining from uncompleted previously prescribed courses) without physician consultation. Fifty-two percent (CI 48.8–54.8) used antibiotics based on a relative advice and 55.6% reported that they do use antibiotics as prophylaxis against infection.
No statistical difference was seen in the total scores between males and females and in both genders; around 50% of the male and female participants had less than 50% of correct answers. Although participants who reported previous use of antibiotics during the past year had lower scores, 18% (18.4%, CI 15.9–20.9) had scores more than 70%. Non users percentage was slightly higher (23%, CI 17.6–28.4), however, this difference did not reach statistical significance. As for age, 22.4% (CI 19.1–25.7) of the younger participants of age 18–25 had scores above 70% which was statistically lower (p < 0.0001) than the other age groups with scores of 16% or below. Role of education was not significant (p = 0.871) as around 19% of both groups, below and above college level, had scores above 70%. There was significant (P < 0.0001) difference in the scores between the two income level groups. The percent of participants with scores more than 70% was 14% (CI 10.9–17.7) in the low income group compared to 24.8% (CI 21.1–28.5) in the higher income group as shown in Table 5.
Table 5.
The knowledge score of respondents.
| Score 1 | Score 2 | Score 3 | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| <50% | 50–70% | >70% | ||||||
| Total | Count (%) | 95% CI | Count (%) | 95% CI | Count (%) | 95% CI | ||
| Gender | ||||||||
| Female | 809 | 375(46.4) | (42.9–49.8) | 280(34.6) | (31.3–37.9) | 154(19.0) | (16.3–21.7) | >0.05 |
| Male | 332 | 165(49.7) | (44.3–55.1) | 101(30.4) | (25.5–35.4) | 66(19.9) | (15.6–24.2) | |
| Antibiotic Use | ||||||||
| No | 235 | 105(44.7) | (38.3–51.0) | 76(32.3) | (26.4–38.3) | 54(23.0) | (17.6–28.4) | >0.05 |
| Yes | 902 | 433(48.0) | (44.7–51.3) | 303(33.6) | (30.5–36.7) | 166(18.4) | ||
| No answer | 4 | 2(50.0) | (1.0, 99.0) | 2(50.0) | (1.0–99.0) | (15.9–20.9) | ||
| Age | ||||||||
| 18–25 yr | 612 | 241(39.4) | (35.5–43.3) | 234(38.2) | (34.4–42.1) | 137(22.4) | (19.1–25.7) | <0.05 |
| 26–35 yr | 274 | 163(59.5) | (53.7–65.3) | 66(24.1) | (19.0–29.2) | 45(16.4) | (12.0–20.8) | |
| 36–45 yr | 101 | 53(52.5) | (42.7–62.2) | 34(33.7) | (24.4–42.9) | 14(13.9) | (7.1–20.6) | |
| >45 | 140 | 74(52.9) | (44.6–61.1) | 44(31.4) | (23.7–39.1) | 22(15.7) | (9.7–21.7) | |
| No answer | 14 | 9(64.3) | (39.2–89.4) | 3(21.4) | (−0.1–42.9) | 2(14.3) | (−4.0–32.6) | |
| Education | ||||||||
| College and Above | 943 | 441(46.8) | (43.6–50.0) | 318(33.7) | (30.7–36.7) | 184(19.5) | (17.0–22.0) | >0.05 |
| No answer | 18 | 11(61.1) | (38.6–83.6) | 5(27.8) | (7.1–48.5) | 2(11.1) | (−3.4–25.6) | |
| Income | ||||||||
| 500 JD and less | 405 | 227(56.0) | (51.2–60.9) | 120(29.6) | (25.2–34.1) | 58(14.3) | (10.9–17.7) | <0.05 |
| >500 JD | 525 | 208(39.6) | (35.4–43.8) | 187(35.6) | (31.5–39.7) | 130(24.8) | (21.1–28.5) | |
| No answer | 211 | 105(49.8) | (43.0–56.5) | 74(35.1) | (28.6–41.5) | 32(15.2) | (10.3–20.0) | |
Physician’s prescribing patterns of antibiotics were evaluated by four questions presented in Table 4. Among the respondents, 3.5% and 29.3% had always and sometimes, respectively, requested antibiotic prescription from their physician. Fortunately, 67.1% of respondents awaited the outcome of the physician’s examination and decision making. Twenty-nine percent (29.1%, CI 26.3–31.8) of respondents had a clear expectation of receiving antibiotics and so consulted other physician to prescribe antibiotics when the first one did not. Almost one in every four respondents (22.9%, CI 20.4–25.3) had been prescribed antibiotics by their physician over the phone without being examined.
Table 4.
Patient–physician relationship.
| Parameter | Number/total | Percentage | 95% CI |
|---|---|---|---|
| Respondents requesting antibiotic prescriptions from their physicians | A: 37/1047 | 3.5 | 2.41–4.7 |
| S: 307/1047 | 29.3 | 26.6–32.1 | |
| N: 703/1047 | 67.1 | 64.3–70.0 | |
| Respondents consulting another physician to prescribe antibiotics if their physician disagreed to do so | A: 39/1060 | 3.7 | 2.6–4.8 |
| S: 269/1060 | 25.4 | 22.8–28.0 | |
| N: 752/1060 | 71.8 | 68.2–73.7 | |
| Physicians routinely prescribed antibiotics to treat common cold symptoms | 579/1131 | 51.2 | 48.3–54.1 |
| Physicians prescribing antibiotics over the phone without examining the patient | 258/1129 | 22.9 | 20.4–25.3 |
4. Discussion
Knowledge about antibiotics therapy among the residents of many countries including Jordan has only been studied to a limited extent (Al-Bakri et al., 2005; You et al., 2008; McNulty et al., 2007). Therefore, this study aimed to collect data reflecting the state of knowledge, attitude and use of antibiotics within the Jordanian community, the prevalence of unrestricted acquisition of antibiotics, the pattern of physicians’ prescriptions and the impact of these factors on antibiotics resistance.
The results of our study showed that the knowledge of when antibiotics should be used, the efficacy of antibiotics as well as the risk of antibiotic resistance is inadequate in Jordan since 47.3% of participants illustrated <50% correct response Table 5. Confusion among the adult regarding whether antibiotics are effective against bacteria and viruses was clear. Actually, it was argued that many people do not understand the differences between bacteria and viruses and believed that antibiotics work against both (McKee et al., 1999). The knowledge concerning these issues is striking. Significantly, respondents knowledge regarding antibiotic use was associated with age (P = 0.042). Younger respondents (18–25 years old) were more likely to utilize antibiotic(s) in the past year (P = 0.001) as shown in Fig. 1d. This excessive use of antibiotics must be deduced by giving priority to knowledge-based education programs for younger generation in the Jordanian community. However, it is not this simple. Respondent who disagreed with the statement that ‘Antibiotics are effective in the treatment of common cold, cough and nasal congestion’ were 44.8% and were as likely to be prescribed antibiotics in the past year with those who did agreed (Fig. 1e).
The confusion regarding antibiotics resistance is persisting. It is a well known fact that the uncontrolled use of antibiotics could lead to substantial and serious problems with the emergence and prevalence of resistant microbial strains, which is a worldwide problem (Hawkey, 1998) Resistance to antibiotics drugs has been linked to levels of consumption (Austin et al., 1999; Linares, 1998) with evidence of a cause–effect relationship (Steinke and Davey, 2001).
Notably, in this study, poor respondent knowledge about antibiotic resistance was obvious since 60.7% of participants illustrated <50% correct answer. Only one out of four (26.4%, CI 23.8–28.9) respondents believed that antibiotics are less likely to be effective in the future if taken too often and 36.0% did not agree that antibiotic resistance is due to unnecessary use. On the other hand, 20.2% of respondents were aware about the misuse of antibiotics in the treatment of every febrile disease. However, more than half of respondents acknowledge the importance of completing the full course of antibiotics for successful outcome.
Young single respondents (18–25 years) were more knowledgeable about antibiotic safety, since 75.8% (P = 0.002) were aware of the harmful effect of certain antibiotics on children’s teeth’ and 77.9% (P ⩽ 0.0005) were knowledgeable about possible death caused by antibiotics allergy despite of the good knowledge about antibiotics allergy, only 26.8% requested an allergy test from physician. Therefore, education campaign should target younger generation to reduce the risk associated with antibiotics.
Concerning antibiotics usage and storage, respondents need to be educated to take antibiotics as prescribed and to store antibiotics and all medications in a special medicine cabinet (unless otherwise specified).
Self-medication with antibiotics is defined as the acquisition of antibiotics and self-administering them with the aim of treating a preserved infection (Awad et al., 2005) This practice is worldwide, in both the developing (Awad et al., 2005; Vaandnen et al., 2006) and industrial countries (Awad et al., 2005). This study revealed that a high percentage of antibiotics being used without physician’s consultation either directly from pharmacies as OTC (35.0%), or self-medication using sibling antibiotics (53.4%) and left-over antibiotics (49.0%). In general, these percentages are comparable to those reported previously, 40.7% and 46.0% for a sample of Jordanians attending a department of dentistry and a sample of consecutive customers arriving at community pharmacy stores in Amman seeking antibiotics for treating systemic infections, respectively (Sawair et al., 2009b; Al-Bakri et al., 2005).
In this survey, significant association between self medication (using of left-over antibiotics), the level of education (P = 0.005), age (P ⩽ 0.001) and gender (P = 0.011) were revealed. The majority tends to be males with low level of education (65.6%) and about half respondents (49.8%, CI 45.7–54.0) tend to be younger (18–25 years old) as shown in Fig. 1f. Furthermore, crosstab analysis did not reveal significant relation between household monthly income (P = 0.137) and self-medication. Whereas, in previous studies in Jordan self medication prevails as income increases (Sawair et al., 2009a; Al-Azzam et al., 2007).
Almost one third (30.5%, CI 27.7–33.2) of respondents (Group A), with a high level of education have got the antibiotic directly from pharmacy without physician consultation. Of those who were prescribed an antibiotic in the past year and did agree with the statement ‘Antibiotic resistance is due to not completing the full course’, 53.1% reported using left-over antibiotic compared to 51.3% (P = 0.027) of the same group who did not agree with the above statement as shown in Fig. 1g. This result showed the contradicting knowledge and behavior among the respondents.
Thirty-one percent of respondents reported using left-over antibiotics for sore throat which in most cases is due to viral and not bacterial infection (Fig. 1h). This is in agreement with Sawair et al. (2009b) findings. However, the percentage reported by Al-Bakri et al. (2005) in Jordan was even higher (70.0%) (Al-Bakri et al., 2005). This big difference may be due to the fact that interviewing real cases of patients purchasing antibiotics (in the latter study) may have given a clearer picture of consumers’ real behavior regarding antibiotic use in Jordan.
Notably, in this study, being more educated and more knowledgeable about antibiotics was independently associated with taking antibiotics without physician’s consultation and keeping left-over antibiotics. Therefore, educational campaigns and ‘Do not recycle antibiotics’ message, should focus on young Jordanians who were more likely to store and take antibiotics without prescription. Additionally, physicians should shorten the course of antibiotics prescribed to 3 or 5 days. Successful implementation of International antibiotic regulations can be supported by urging pharmacists to dispense antibiotics according to the number of days stated by the physician and not in set pack sizes.
One of the important factors to have an impact on general adult use of antibiotics is physicians prescribing patterns. In this study, one third of respondents have reported requesting antibiotic prescription from physicians, more than half (51.2%, CI 48.3–54.1) had been prescribed antibiotics to treat common cold symptoms and one in every four (22.9%) had been prescribed an antibiotic over the phone without examination. This practice may deprive the physician of many diagnostic clues that may help to rule out viral from bacterial infections. In fact, several previous studies have reported that patient pressure was the most frequently cited reason for physicians’ discomfort with prescribing antibiotics (Britten, 1995; McManus et al., 1997). Despite the accumulating evidence from clinical trials that antibiotics might modify the course of common cold symptoms (if at all), almost all physicians acknowledged that antibiotics were prescribed too often in such cases (Little et al., 1997; Mainous et al., 1996; Stott, 1979; Whitfield and Hughes, 1981). This practice would misguide adult belief about antibiotic use and put them at unnecessary risk for contracting infections with resistant pathogens. Therefore, a major change in prescribing practice supported by a national adult information campaign is essential to reduce patient expectations from antibiotics and to raise awareness about antibiotic resistance.
In Jordan, inadequate enforcement of drug regulations raised inappropriate antibiotics consumption. As revealed in this study, one third of respondents bought antibiotics directly from pharmacy without prescriptions over the past year. To prevent this practice, health authorities have to implement their regulations to prohibit the selling of POM without prescription.
5. Limitations and future directions
This study has certain limitations that merit discussion. The surveyed group was found to be a real representative category for the evaluation of the knowledge, behavior and attitude of young educated females in particular toward antibiotic use and misuse. This was due to handling the questionnaire to respondents during day time in common places as malls, supermarkets and female beauty centers where female abundance is extremely higher at this time. However, these young females are the prospect mothers.
As for the arbitrary high percentage of education among the respondents was due to the fact that Jordanian population belongs to high education level category (According to Jordanian statistics department, 33% of Jordanian population belongs to high education level category, whereas, higher percentage (42%) in Amman, the Capital).
Therefore, a larger-scale study is needed where more heterogeneous population mix would define further the scope of antibiotic use and misuse among Jordanian adults.
The key results of this study would form the basis for future interventional directions to improve knowledge among Jordanian people. To achieve this, the authors suggest a number of fundamental keystones for controlling antibiotics misuse and subsequent antibiotic resistance. These include the followings: (1) establishing adult educational programs using all media means about the illnesses that require antibiotic therapy and emphasizing when antibiotics will not do any good, (2) controlling channels of obtaining antibiotics by implementing strict drug regulations, (3) direct patient compliance to the treatment as prescribed, (4) emphasizing pharmacists role and responsibility in stopping antibiotic sale without prescription and (5) consultation strategies and guidelines that make patient expectations explicit without damaging physician–patient relationship, all those points might reduce inappropriate antibiotics use.
Funding
The study was financially supported by The University of Jordan.
Disclosure statement
The authors report no conflict of interest to declare.
Acknowledgements
The authors would like to thank the questionnaire respondents who kindly devoted their time to the study. We also thank Miss Heba A.N. Al-Ejal research assistant at the faculty of pharmacy. Many thanks for the Deanship of the Scientific Research in The University of Jordan for the financial support.
References
- Al-Azzam S.I., Al-Husein B.A., Alzoubi F., Masadeh M.M., Al-Horani M.S. Self-medication with antibiotics in Jordanian population. Int. J. Occup. Med. Environ. Health. 2007;4:373–380. doi: 10.2478/v10001-007-0038-9. [DOI] [PubMed] [Google Scholar]
- Al-Bakri A.G., Bustanji Y., Yousef A.M. Community consumption of antibacterial drugs within the Jordanian population: sources, patterns and appropriateness. Int. J. Antimicrob. Agents. 2005;26:389–395. doi: 10.1016/j.ijantimicag.2005.07.014. [DOI] [PubMed] [Google Scholar]
- Albsoul-Younes A., Wazaify M.M., Yousef A.M., Tahaineh L. Abuse and misuse of prescription and nonprescription drugs sold in community pharmacies in Jordan. Med. Misuse. 2010;45:1319–1329. doi: 10.3109/10826080802490683. [DOI] [PubMed] [Google Scholar]
- Al-Momany N.H., Al-Bakri A.G., Makahleh Z.M., Wazaify M.M. Adherence to international antimicrobial prophylaxis guidelines in cardiac surgery: a Jordanian study demonstrates need for quality improvement. J. Manag. Care Pharm. 2009;15:262–271. doi: 10.18553/jmcp.2009.15.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin D.J., Kristinsson K.G., Anderson R.M. The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc. Natl. Acad. Sci. USA. 1999;96:1152–1156. doi: 10.1073/pnas.96.3.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awad A., Eltayeb I., Matowe L., Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J. Pharm. Pharm. Sci. 2005;8:326–331. [PubMed] [Google Scholar]
- Britten N. Patients demands for prescriptions in primary-care. Br. Med. J. 1995;310:1084–1085. doi: 10.1136/bmj.310.6987.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buke A.C., Ermertcan S., Hosgor-Limoncu M., Ciceklioglu M., Eren S. Rational antibiotic use and academic staff. Int. J. Antimicrob. Agents. 2003;21:63–66. doi: 10.1016/s0924-8579(02)00272-8. [DOI] [PubMed] [Google Scholar]
- Buke C., Hosgor-Limoncu M., Ermertcan S., Ciceklioglu M., Tuncel M., Köse T., Eren S. Irrational use of antibiotics among university students. J. Infect. 2005;51:135–139. doi: 10.1016/j.jinf.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Chen C., Chen Y.M., Hwang K.L., Lin S.J., Yang C.C., Tsay R.W., Liu C.E., Young T.G. Behavior, attitudes and knowledge about antibiotic usage among residents of Changhua. Taiwan J. Microbiol. Immunol. Infect. 2005;38:53–59. [PubMed] [Google Scholar]
- Dar-Odeh N.S., Abu-Hammad O.A., Al-Omiri M.K., Khraisat A.S., Shehabi A.A. Antibiotic prescribing practices by dentists: a review. Ther. Clin. Risk Manage. 2010;6:301–306. doi: 10.2147/tcrm.s9736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyssens I.C. Quality measures of antimicrobial drug use. Int. J. Antimicrob. Agents. 2001;17:9–19. doi: 10.1016/s0924-8579(00)00208-9. [DOI] [PubMed] [Google Scholar]
- Hawkey P.M. Action against antibiotic resistance: no time to lose. Lancet. 1998;351:1298–1299. doi: 10.1016/S0140-6736(98)22018-6. [DOI] [PubMed] [Google Scholar]
- Linares J. Community-acquired antimicrobial resistance: is it controllable? Int. J. Clin. Pract. 1998:23–26. [PubMed] [Google Scholar]
- Little P., Williamson I., Warner G., Gould C., Gantley M., Kinmonth A.L. Open randomised trial of prescribing strategies in managing sore throat. Brit. Med J. 1997;314:722–727. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mainous A.G., Hueston W.J., Clark J.R. Antibiotics and upper respiratory infection – do some folks think there is a cure for the common cold? J. Fam. Pract. 1996;42:357–361. [PubMed] [Google Scholar]
- McKee M.D., Mills L., Mainous A.G. Antibiotic use for the treatment of upper respiratory infections in a diverse community. J. Fam. Pract. 1999;48:993–996. [PubMed] [Google Scholar]
- McManus P., Hammond M.L., Whicker S.D., Primrose J.G., Mant A., Fairall S.R. Antibiotic use in the Australian community, 1990–1995. Med. J. Aust. 1997;167:124–127. doi: 10.5694/j.1326-5377.1997.tb138809.x. [DOI] [PubMed] [Google Scholar]
- McNulty C.A., Boyle P., Nichols T., Clappison P., Davey P. Don’t wear me out – the adult’s knowledge of and attitudes to antibiotic use. J. Antimicrob. Chemother. 2007;59:727–738. doi: 10.1093/jac/dkl558. [DOI] [PubMed] [Google Scholar]
- Metlay J.P., Stafford R.S., Singer D.E. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch. Intern. Med. 1998;158:1813–1818. doi: 10.1001/archinte.158.16.1813. [DOI] [PubMed] [Google Scholar]
- Sawair F.A., Baqain Z.H., Karaky A.A., Eid R.A. Assessment of self-medication of antibiotics in a Jordanian population. Med. Princ. Pract. 2009;18:21–25. doi: 10.1159/000163041. [DOI] [PubMed] [Google Scholar]
- Sawair F.A., Shayyab M.H., Al-Rabab’ah M.A., Saku T. Prevalence and clinical characteristics of tori and jaw exostoses in a teaching hospital in Jordan. Saudi Med. J. 2009;30:1557–1562. [PubMed] [Google Scholar]
- Shankar P.R., Partha P., Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam. Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinke D., Davey P. Association between antibiotic resistance and community prescribing: A critical review of bias and confounding in published studies. Clin. Infect. Dis. 2001;33:S193–S205. doi: 10.1086/321848. [DOI] [PubMed] [Google Scholar]
- Stott N.C.H. Management and outcome of winter upper respiratory-tract infections in children aged 0–9 years. Br. Med. J. 1979;1:29–31. doi: 10.1136/bmj.1.6155.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaandnen M.H., Pietila K., Airaksinen M. Self-medication with antibiotics – does it really happen in Europe? Health Policy. 2006;77:166–171. doi: 10.1016/j.healthpol.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Whitfield M.J., Hughes A.O. Penicillin in sore throat. Practitioner. 1981;225:234–239. [PubMed] [Google Scholar]
- You J.H., Yau B., Choi K.C., Chau C.T.S., Huang Q.R., Lee S.S. Adult knowledge, attitudes and behavior on antibiotic use: a telephone survey in Hong Kong. Infection. 2008;36:153–157. doi: 10.1007/s15010-007-7214-5. [DOI] [PubMed] [Google Scholar]
- Yousef A.M., Al-Bakri A.G., Bustanji Y., Wazaify M.M. Self-medication patterns in Amman, Jordan. Pharm. World. Sci. 2008;30:24–30. doi: 10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]


