Abstract
Objective
The objective is to evaluate whether physician body mass index (BMI) impacts their patients’ trust or perceptions of weight-related stigma.
Methods
We used a national cross-sectional survey of 600 non-pregnant overweight and obese patients conducted between April 5 and April 13, 2012. The outcome variables were patient trust (overall and by type of advice) and patient perceptions of weight-related stigma. The independent variable of interest was primary care physician (PCP) BMI. We conducted multivariate regression analyses to determine whether trust or perceived stigma differed by physician BMI, adjusting for covariates.
Results
Patients reported high levels of trust in their PCPs, regardless of the PCPs body weight (normal BMI = 8.6; overweight = 8.3; obese = 8.2; where 10 is the highest). Trust in diet advice was significantly higher among patients seeing overweight PCPs as compared to normal BMI PCPs (87% vs. 77%, p = 0.04). Reports of feeling judged by their PCP were significantly higher among patients seeing obese PCPs (32%; 95% confidence interval (CI): 23–41) as compared to patients seeing normal BMI PCPs (14%; 95% CI: 7–20).
Conclusion
Overweight and obese patients generally trust their PCP, but they more strongly trust diet advice from overweight PCPs as compared to normal BMI PCPs.
Keywords: Physician BMI, Patient trust, Weight stigma, Weight-related advice
Introduction
Recent changes to obesity coverage among the publically insured population make an understanding of primary care physician (PCP) barriers in providing effective obesity care critical. In November 2011, the Centers for Medicare and Medicaid announced that Medicare will begin covering obesity screening and intensive behavioral therapy for beneficiaries with a body mass index (BMI) ≥30 kg/m2 in the primary care setting (Center for Medicaid and Medicare, 2011). This will be fully paid by Medicare with no copayment and more than 30% of the Medicare population is expected to qualify. In addition, the 2010 Affordable Care Act (ACA) incentivizes state Medicaid programs to cover the preventive services recommended by the U.S. Preventive Service Task Force (USPSTF) without patient cost sharing which were recently updated to recommend that clinicians screen patients for obesity and then offer or refer those patients who meet or exceed that level “intensive, multi-component behavioral interventions” to help them lose weight (Moyer, 2012). These benefit expansions have implications beyond the publically insured population as private insurers may follow suit.
PCPs face numerous challenges to providing optimal obesity care which include knowledge deficits (e.g., inadequate training) (Block et al., 2003), negative attitudes (Foster et al., 2003), and structural barriers (e.g., time) (Ruelaz et al., 2007). One factor that has recently been identified is PCP body weight. In a national survey of PCPs, normal weight physicians were more likely to discuss weight loss, report greater confidence in providing diet and exercise counseling, and perceive their weight loss advice as trustworthy compared to overweight/obese physicians (Bleich et al., 2012). Given that trust is the cornerstone of an effective doctor–patient relationship, these results raise the question of whether physicians’ weight impacts their patients’ trust. Patient trust in PCP’s advice may be especially important in the Medicare population, as PCPs will be counseling patients to modify lifelong obesity promoting behaviors to lose or control weight. The finding that PCP weight impacts obesity care also raises the question of whether the well documented weight bias among health professionals (Puhl and Brownell, 2001) differs by PCP weight. For example, physicians have been shown to view obese patients as noncompliant, lazy, lacking in self-control, weak-willed, dishonest, and unsuccessful (Campbell et al., 2000; Hebl and Xu, 2001; Kristeller and Hoerr, 1997).
Questions related to the impact of physician personal traits on patient trust are not new. Past research has shown that physician characteristics (e.g., gender), attributes (e.g., compassion) and appearance (e.g., white coat) each influence patient trust (Cooper et al., 2003; Pickett-Blakely et al., 2011; Spruill et al., 2007). However, the potential impact of physician body weight on patient trust has not been examined. Understanding the potential relationship between trust and physician body weight is an important area of inquiry given that trust is a critical precursor to behavior change and is linked to patient adherence to physician advice, patient satisfaction, and continuity of care (Thom et al., 2004).
Trust is one of the central features of patient–physician relationships. A trusting relationship between the patient and the provider can facilitate patient disclosure, potentially increase patient compliance with therapies and facilitate behavior change (Gilson, 2003; Gray, 1997). Patient trust is a complicated, multidimensional construct which has been described in many ways. For this paper, we are most interested in interpersonal trust which refers to the trust built through repeated interactions through which expectations about a person’s trustworthy behavior can be tested over time (Mechanic and Schlesinger, 1996) rather than social trust which is trust in collective institutions, influenced broadly by the media and by general social confidence in particular institutions.
Understanding whether physician weight-related stigma towards obese patients differs by PCP body weight, is also important as stigma has been shown to negatively impact physician and patient behavior. Compared to normal weight patients, obese patients receive inferior care; their doctors spend less time, give more assignment of negative symptoms and are reluctant to perform certain screenings (Bertakis and Azari, 2005; Campbell et al., 2000; Galuska et al., 1999; Hebl and Xu, 2001). Negative attitudes of health professionals towards obese patients have been shown to impact medical care. For example, one study found that obese women delayed seeking preventative care services due to perceived disrespect from providers, embarrassment of being weighed, and negative provider attitudes (Amy et al., 2006).
The extent to which patient trust or perceived weight-related stigma differs by PCP BMI is unknown. Our objective was to evaluate whether PCP BMI impacts their patients’ trust or perceptions of weight-related stigma among a sample of overweight and obese patients. We specifically examined patient trust overall, patient trust in weight loss advice and whether patients felt judged because of their weight. We hypothesized that higher physician BMI would be associated with higher patient trust and lower weight-related stigma given that the mechanism through which doctor–patient demographic concordance has been associated with positive patient–physician interaction is through perceptions of similarity (Bissell et al., 2004; Burgess et al., 2004; Street et al., 2008).
Methods
Study design
We used a national cross-sectional survey of non-pregnant overweight and obese adults (BMI ≥ 25 kg/m2) in the United States for our study design.
Survey development and implementation
We consulted SSRS/Social Science Research Solutions to design and implement the survey. The survey instrument was reviewed for content by experts in the field of obesity, and was then pretested for length and comprehensibility among individuals who met the inclusion criteria for the study (described below). The survey was revised on the basis of these pilot tests and the final version included thirty-three questions.
We surveyed 600 non-pregnant overweight or obese adults (BMI ≥ 25 kg/m2) between April 5 and April 13, 2012. The fieldwork for this survey was conducted via the Internet by Authentic Response (AR) web panel company, which consists of approximately 4,000,000 registered members. Although some research has suggested that web-based surveys may be biased with respect to measuring health outcomes (Rivara et al., 2011), other studies have suggested that web-based administration is comparable to other modes with respect to respondents’ demographics and reported health behavior risks (Fricker et al., 2005; McMorris et al., 2009). To improve data validity, AR includes panel members by invitation only and uses algorithms to identify and exclude professional survey-takers. The panel members were recruited to represent a general U.S. population sample, and data were weighted to address non-response bias and to match demographic patterns of the overweight adult population. Panel members were not eligible if they had not seen a primary care doctor (PCP) within the past year, their BMI was less than 25 kg/m2, or they were pregnant. The sample was intentionally restricted to the overweight/obese population who had a primary care visit in the past year as the survey was interested in perspectives on weight-related care.
Of the 1380 panel members who responded to the survey invitation, 335 were excluded since they had not seen a doctor in the past year, 396 did not have a qualifying BMI, 43 had incomplete survey responses, and 6 were pregnant. This resulted in a 93% completion rate, which is consistent with recently published Internet survey research (Puhl et al., 2012).
This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Measures
Outcome variables
We examined two trust variables in this analysis: overall trust and trust in weight-related advice. Trust overall was measured on a scale from 0 to 10 (10 was the highest). Overall trust was assessed by the survey question: “Using any number from 0 to 10, where 0 means that you do not trust this doctor at all and 10 means that you trust this doctor completely, what number would you use to rate how much you trust this doctor?” This question was obtained from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Cultural Competence Item Set—a survey which assesses the cultural competence of health care providers from the patient’s perspective (Agency for Healthcare Quality and Research, 2013). Trust in weight-related advice was assessed by the survey question: “How much do you trust the advice from this doctor about how to [control your weight/improve your diet/increase your physical activity]—a great deal, a good amount, only some, or very little?” For the questions about weight related advice, the response categories were dichotomized to ‘a great deal/a good amount’ vs. ‘only some/very little’. These questions were adapted from the Trust in Physician Scale, an 11-item, interviewer-administered measure that assesses patient trust in physician in the domains of dependability, confidence, and confidentiality of information (Anderson and Dedrick, 1990). Weight-related stigma was assessed by the survey question: “In the last 12 months, did you ever feel that this doctor judged you because of your weight?”—yes, often; yes, sometimes; no, never. The response categories were dichotomized to ‘yes, often or sometimes’ vs. ‘no, never’. All variables were dichotomized based on the cut-points in the data.
Independent variables
The primary independent variable of interest was PCP BMI, reported by their patient. To determine patient perceptions of their PCPs body weight, respondents selected one of the five different pictograms representing normal BMI to class III obese. We elected to use pictures rather than provide BMI categories in an effort to not bias patient responses and because we expected patients would be less likely to know their physicians BMI. We are unaware of previous studies which have validated these pictures against observed BMI. Additional patient-level covariates of interest included body weight (overweight or obese), gender, race/ethnicity, age, education, region of the country, length of time since last visit with PCP (less than 3 months vs. at least 3 months to less than 1 year), and length of relationship with PCP (less than 3 years vs. 3 years or more). PCP-level covariates included gender, race/ethnicity and age, all reported by the patient.
Statistical analyses
We performed descriptive analyses for all variables. We conducted multivariate regression analyses (linear and logistic) adjusting for patient-level (body weight, gender, race/ethnicity, age, education, region of the country, length of time since last visit with PCP, and length of relationship with PCP and PCP-level covariates (gender, race/ethnicity and age)). Because odds ratios can be difficult to interpret in terms of policy relevance when the outcomes under study are common (Altman et al., 1998; Kleinman and Norton, 2009), we calculated the marginal effects of the independent variables and report predicted probabilities and their associated 95% confidence intervals from the regression models. We did not stratify the results by demographic characteristics (e.g. gender, race, age) as we were not sufficiently powered to do so.
To verify that the study sample was representative of the U.S. population, we compared our descriptive statistics to the 2010 Behavioral Risk Factor Surveillance System (BRFSS) subset to non-pregnant, overweight and obese individuals (BMI ≥ 25) who reported having a routine check-up in the past year, published elsewhere (Jarlenski et al., 2013). Characteristics of our sample are similar to the 2010 BRFSS subset. The BRFSS data were chosen for comparison because, as with the survey data reported in this paper, BMI is calculated based on self-reported height and weight.
We used weighting to address systematic under- or over-representation of the physician subpopulations in the panel, account for systematic non-response along known demographic characteristics of the physicians, and adjust for sampling biases due to differences in non-response rates (Keeter et al., 2000). All analyses used weights to account for differential sampling rates and were conducted using the “SVY” commands in Stata 11 (StataCorp LP, College Station, TX). The weighted margin of error for the survey was +/− 4.9%.
Results
Table 1 reports the characteristics of the study sample. Survey participants were 51% obese, 48% female, 65% White, 65% under age 55, and 67% had some college education or more. Most patients had seen their PCP in the past 3 months (60%) and 41% knew their PCP for 3 years or more. The majority of patients reported having an overweight (53%) or obese (30%) PCP. Survey participants categorized their PCPs as 64% male, 67% White and 67% aged 45 or older. As mentioned above, characteristics of our sample are similar to the 2010 BRFSS subset to non-pregnant, overweight and obese individuals (BMI ≥ 25) who reported having a routine check-up in the past year (Jarlenski et al., 2013).
Table 1.
Characteristics of the study sample (n = 600).
| n | % | |
|---|---|---|
| Patient characteristics | ||
| Body weight | ||
| Overweight | 294 | 49 |
| Obese | 306 | 51 |
| Gender | ||
| Female | 286 | 48 |
| Male | 314 | 52 |
| Race/ethnicity | ||
| White | 392 | 65 |
| Black | 77 | 13 |
| Hispanic | 89 | 15 |
| Other race | 40 | 7 |
| Age, year | ||
| Under 40 | 210 | 35 |
| Aged 40–64 | 288 | 49 |
| Aged 65 and older | 102 | 17 |
| Education | ||
| Less than high school | 53 | 9 |
| High school | 148 | 25 |
| Some college | 237 | 40 |
| College degree or more | 162 | 27 |
| Region | ||
| Northeast | 100 | 17 |
| Midwest | 115 | 19 |
| South | 208 | 35 |
| West | 128 | 21 |
| Length of time since last visit with PCP | ||
| Less than 3 months | 360 | 60 |
| At least 3 months to less than 1 year | 240 | 40 |
| Length of relationship with PCP | ||
| Less than 3 years | 236 | 39 |
| 3 years or more | 364 | 41 |
| PCP characteristics | ||
| Body weight | ||
| Normal weight | 103 | 17 |
| Overweight | 318 | 53 |
| Obese | 179 | 30 |
| Gender | ||
| Female | 217 | 36 |
| Male | 383 | 64 |
| Race | ||
| White | 404 | 67 |
| Other race | 196 | 33 |
| Age | ||
| Less than 45 years | 200 | 33 |
| 45 years or older | 400 | 67 |
Notes: Numbers may not add up to 100% because of rounding. Patient body weight is based on self-reported height and weight: overweight (BMI, 25.0 to 29.9 kg/m2), and obese (BMI, ≥30 kg/m2). PCP body weight is based on patient report. The survey displayed pictures of five different body sizes that ranged from normal BMI to class III obese, where image 1 represented normal BMI and image 5 represented class III obese, and respondents were asked to select the size which most closely corresponded to their PCP.
Table 2 shows predicted probabilities of patient trust in physicians by PCP BMI, adjusted for covariates. The full models are available upon request to the authors. Overall, patients reported high levels of trust in their PCPs, regardless of the PCPs BMI—normal BMI = 8.6 (95% CI: 8.3 to 8.9) overweight = 8.3 (95% CI: 8.0 to 8.6); obese = 8.2 (95% CI: 7.9 to 8.5); where 10 indicates the highest level of trust. We observed no significant differences in the predicted probabilities of overall levels of trust by physician BMI (p > 0.5). For the measure of trust in weight control advice, the predicted probability of reporting a great deal or a good amount of trust in their PCP increased with physician body weight, but not significantly—normal BMI PCP = 76% (95% CI: 68–85); overweight PCP = 85% (95% CI: 80–89); and obese PCP = 85% (95% CI: 80–91). For the measure of trust in diet advice, the predicted probability of reporting a great deal or a good amount of trust in their PCP also increased with physician body weight and was significantly higher for patients seeing overweight PCPs as compared to normal BMI PCPs—normal BMI = 77% (95% CI: 68–86); overweight PCP = 87% (95% CI: 83–91; p = 0.04); and obese PCP = 82% (95% CI: 76–89; p = 0.06). For the measure of trust in physical activity advice, the predicted probability of reporting a great deal or a good amount of trust in their PCP generally increased with physician body weight, but not significantly—normal BMI PCP = 79% (95% CI: 71–88); overweight PCP = 86% (95% CI: 82–91); and obese PCP = 80% (95% CI: 73–87; p = 0.001 for normal BMI vs. obese and p = 0.005 for overweight vs. obese).
Table 2.
Predicted probability of patient trust in physicians by PCP BMI.
| Normal (n = 118) | Overweight (n = 312) | Obese (n = 170) | |
|---|---|---|---|
| Overall trust (scale of 1 to 10) | 8.6 | 8.3 | 8.2 |
| Trust advice on weight control | |||
| A great deal/a good amount | 76% | 85% | 85% |
| Only some/very little | 24% | 15% | 15% |
| Trust advice on diet | |||
| A great deal/a good amount | 77% | 87%† | 82% |
| Only some/very little | 23% | 13% | 18% |
| Trust advice on physical activity | |||
| A great deal/a good amount | 79% | 86% | 80% |
| Only some/very little | 21% | 14% | 20% |
Note: Weighted to be representative of the national population. Models adjust for patient-level (body weight, gender, race/ethnicity, age, education, region of the country, length of time since last visit with PCP, and length of relationship with PCP and PCP-level covariates (gender, race/ethnicity and age)).
p < 0.05, reference category is normal BMI.
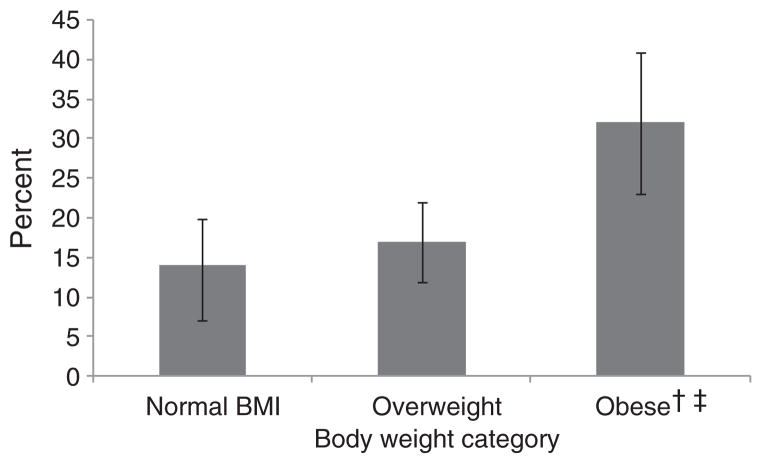
Fig. 1 shows predicted probabilities of patient perceptions of being judged by their physician because of their weight by PCP BMI, adjusted for covariates. Overall, 21% (95% CI: 17–25) of the sample reports being judged by their physician because of their body weight. The predicted probability of reporting feeling judged by their PCP was significantly higher among patients seeing obese PCPs as compared to patients seeing overweight and normal BMI PCPs—normal BMI = 14% (95% CI: 7–20); overweight PCP = 17% (95% CI: 12–23; p = 0.04); and obese PCP = 32% (95% CI: 23–41).
Fig. 1.
Patients perceptions of being judged by their physician because of their weight, by PCP BMI. Note: Weighted to be representative of the national population. Models adjust for patient-level (body weight, gender, race/ethnicity, age, education, region of the country, length of time since last visit with PCP, and length of relationship with PCP and PCP-level covariates (gender, race/ethnicity and age)). † p < 0.05, reference category is normal BMI. ‡ p < 0.05, reference category is overweight.
Discussion
This paper is the first to examine the associations between physician BMI and patient trust as well as physician BMI and weight-related stigma. With respect to overall trust, our results suggest that overweight and obese patients trust their PCPs, regardless of their body weight. With respect to trust in weight-related advice, we found that patients more strongly trusted diet advice from overweight PCPs as compared to normal BMI PCPs which is consistent with our hypotheses. Inconsistent with our study hypotheses was the finding that patient perceptions of weight-related stigma increased with physician BMI. Patients seeing obese PCPs, as compared to normal BMI physicians, were significantly more likely to report feeling judged because of their weight. In our sample of overweight and obese patients, a fifth of all respondents reported feeling judged by their physician because of their weight.
These results suggest that physician BMI impacts patient trust in their PCP. Interestingly, these results are contrary to our early study looking at the impact of physician BMI and obesity care. In that study we found that normal weight doctors are more likely to provide recommended obesity care and feel comfortable doing so as compared to overweight and obese physicians (Bleich et al., 2012). High levels of trust in weight-related advice from PCPs, particularly heavier PCPs, could be due to the fact that concordance between patient and PCP body weight improves the relationship from the patient perspective. In particular, the shared weight identity between an overweight/obese patient and an overweight/obese PCP may improve their interaction and communication about weight-related behaviors (Bissell et al., 2004; Burgess et al., 2004; Street et al., 2008). However, patients’ high levels of trust in weight-related advice may be inappropriate as prior studies of PCPs show lack of knowledge and low self-efficacy regarding obesity care (Block et al., 2003; Eriksen and Ujam, 1992; Forman-Hoffman et al., 2006; Jay et al., 2008; Vetter et al., 2008).
While weight-related stigma has been documented among health professionals for decades (Puhl and Heuer, 2009) as well as lowers physician respect towards patients with a higher BMI (Huizinga et al., 2009), our finding that weight-related stigma increases with physician BMI is puzzling. One potential reason could be that physicians with a higher BMI have been stigmatized themselves and internalization of these negative attitudes could, in turn, lead to perpetration of the same behavior among patients (García et al., 2004). Recent research among adolescents suggests that obese teens are more likely to be recipients and perpetrators of weight-related teasing (Kukaswadia et al., 2012). Another explanation could be that heavier physicians simply do not perceive themselves as overweight or obese. The misclassification of weight status has increased among heavier individuals with overweight and obese individuals becoming increasingly less likely to self-identify as overweight (Johnson et al., 2008). Therefore, our finding of high rates of weight-related stigma may be a reflection of general physician stigma towards obesity (Kristeller and Hoerr, 1997).
Improving rates of weight related counseling in primary care settings is an important strategy to promote behavior change in obese patients, particularly due to the recent expansions of Medicare and Medicaid coverage for obesity care. There is a growing body of evidence suggesting that patients who are told by their physician that they are overweight are more likely to lose weight relative to those who are not told (Kant and Miner, 2007; Levy and Williamson, 1988), that patients who are counseled about their weight or weight-related behaviors are more likely to report working on those areas (Calfas et al., 1997; Galuska et al., 1999; Loureiro and Nayga, 2006; Sciamanna et al., 2000), and that patients who are advised by their physician to modify their behavior are generally more confident and motivated to engage in lifestyle modifications (e.g., dietary changes, increased physical activity) (Galuska et al., 1999; Huang et al., 2004; Kreuter et al., 2000).
However, effective screening and counseling from PCPs is necessary but not sufficient to solve the problem of obesity. The relative success of these new public insurance obesity benefits may largely hinge on whether knowledge, self-efficacy, and stigma-related barriers faced by PCPs can be addressed. It is reassuring to know that overweight and obese patients generally trust their PCPs. This may help enhance the impact of intensive behavioral counseling even if patient-, physician- and health-system barriers to obesity care persist.
Future research should further examine the impact of physician BMI on obesity care. In particular, why patient perceived physician stigma is higher among heavier PCPS and why the patterns we observed between physician BMI and trust in weight-related counseling differ by the type of counseling. More research is also needed to understand the mechanisms driving higher trust among heavier PCPs as well as whether particular physician practices related to obesity care engender higher levels of trust in patients. It will also be interesting to examine why patient trust in diet advice was significantly higher among overweight (but not obese) PCPs as compared to normal BMI PCPs. Finally, it is puzzling that we observed relationships between patient trust in diet advice and physician BMI but not between patient trust in weight control/physical activity advice and physician BMI. Going forward, it will be important to better understand these relationships.
There are several limitations to this analysis. First, it is cross-sectional which only allows us to address associations rather than causal inferences. Second, we relied on respondents’ self-reported height and weight which typically underestimate BMI (Ezzati et al., 2006). Third, unmeasured patient or physician factors may have affected our findings. Examples include patient familiarity with their physician and patient and physician attitudes towards obesity and preferred communication styles. Fourth, even though the survey was reviewed by experts in the fields of obesity and primary care as well as pilot tested for comprehensibility, it is possible that respondents differentially interpreted some of the questions. Fifth, the study population is restricted to those individuals who reported having a primary care visit in the past year, so findings are not generalizable to those individuals who lack this level of access to health care. Sixth, trust may mean different things for survey respondents (e.g., technical competency, interpersonal competency etc.) which could lead the survey question to capture different components of the trust concept. Seventh, the pictures of body images have not been have previously validated against observed BMI. Therefore, it is unknowable whether patients are more likely to misclassify the body weight of their physicians in some categories but not others. Patient reports of physician weight need to be validated against actual physician weight to fully understand the validity of the pictogram and whether misclassification – if any – exists. Eighth, it is possible that patient trust influenced their memory of PCP weight since PCP visits occurred prior to data collection. To address this potential recall bias, we did adjust for the length of time since the patients’ last visit with their PCP. Ninth, given that the use of web-based surveys is relatively new, potential sources of biases are not entirely understood. Finally, all PCP characteristics are reported by patients, which could misrepresent some of the physicians in the sample.
Conclusion
In conclusion, this study suggests that overweight and obese patients generally trust their PCP, but that they more strongly trust diet advice from overweight PCPs as compared to normal BMI PCPs. We also observed higher patient-perceived weight-related stigma among obese physicians. Going forward, it will be important to improve training for students, residents and practicing providers about weight-related counseling so they are prepared to provide these newly covered Medicare and Medicaid services.
Acknowledgments
Funding
This work was supported by two grants from the National Heart, Lung, and Blood Institute (1K01HL096409, K24HL083113, P50 HL0105187) and one grant from the Health Resources and Services Administration (T32HP10025-17-00).
Footnotes
Contributors
SNB, LAC, KAG, and WLB conceived the study and developed the hypotheses. SNB analyzed the data. All authors contributed to the interpretation of study findings. SNB drafted the manuscript and all authors contributed to the final draft. SNB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
None.
References
- Agency for Healthcare Quality and Research. About the CAHPS® Cultural Competence Item Set. CAHPS® Clinician & Group Surveys and Instructions; Washington DC: 2013. [Google Scholar]
- Altman DG, Deeks JJ, Sackett DL. Odds ratios should be avoided when events are common. BMJ. 1998;317 (7168):1318. doi: 10.1136/bmj.317.7168.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes (Lond) 2006;30 (1):147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- Anderson LA, Dedrick RF. Development of the Trust in Physician Scale: a measure to assess interpersonal trust in patient–physician relationships. Psychol Rep. 1990;67(3 Pt 2):1091–1100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13(9):1615–1623. doi: 10.1038/oby.2005.198. [DOI] [PubMed] [Google Scholar]
- Bissell P, May CR, Noyce PR. From compliance to concordance: barriers to accomplishing a re-framed model of health care interactions. Soc Sci Med. 2004;58(4):851–862. doi: 10.1016/s0277-9536(03)00259-4. [DOI] [PubMed] [Google Scholar]
- Bleich SN, Bennett WL, Gudzune KA, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring) 2012;20 (5):999–1005. doi: 10.1038/oby.2011.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36(6):669–675. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- Burgess DJ, Fu SS, van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004;19(11):1154–1159. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calfas KJ, Sallis JF, Oldenburg B, Ffrench M. Mediators of change in physical activity following an intervention in primary care: PACE. Prev Med. 1997;26(3):297–304. doi: 10.1006/pmed.1997.0141. [DOI] [PubMed] [Google Scholar]
- Campbell K, Engel H, Timperio A, Cooper C, Crawford D. Obesity management: Australian general practitioners’ attitudes and practices. Obes Res. 2000;8(6):459–466. doi: 10.1038/oby.2000.57. [DOI] [PubMed] [Google Scholar]
- Center for Medicaid and Medicare. Decision Memo for Intensive Behavioral Therapy for Obesity (CAG-00423 N) 2011 [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Martin H, Skjold S, Hoorn SV, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99:250–257. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. doi: 10.1186/1471-2296-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–1177. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- Fricker S, Galesic M, Tourangeau R, Yan T. An experimental comparison of Web and telephone surveys. Public Opin Q. 2005;69(3):370–392. [Google Scholar]
- Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? J Am Med Assoc. 1999;282(16):1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- García Coll CT, Bearer EL, RML . Nature and Nurture: The Complex Interplay of Genetic and Environmental Influences on Human Behavior and Development. Lawrence Erlbaum; Mahwah: 2004. [Google Scholar]
- Gilson L. Trust and the development of health care as a social institution. Soc Sci Med. 2003;56:1453–1468. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- Gray B. Trust and trustworthy care in the managed care era. Health Aff. 1997;16:34–49. doi: 10.1377/hlthaff.16.1.34. [DOI] [PubMed] [Google Scholar]
- Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156–161. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24(11):1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarlenski MP, Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Insurance coverage for weight loss: overweight adults’ views. Am J Prev Med. 2013;44 (5):453–458. doi: 10.1016/j.amepre.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay M, Gillespie C, Ark T, et al. Do internists, pediatricians, and psychiatrists feel competent in obesity care?: using a needs assessment to drive curriculum design. J Gen Intern Med. 2008;23(7):1066–1070. doi: 10.1007/s11606-008-0519-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson F, Cooke L, Croker H, Wardle J. Changing perception of weight in the UK: comparison of two population surveys. BMJ. 2008;337:a494. doi: 10.1136/bmj.a494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant AK, Miner P. Physician advice about being overweight: association with self-reported weight loss, dietary, and physical activity behaviors of US adolescents in the National Health and Nutrition Examination Survey, 1999–2002. Pediatrics. 2007;119 (1):e142–e147. doi: 10.1542/peds.2006-1116. [DOI] [PubMed] [Google Scholar]
- Keeter S, Miller C, Kohut A, Groves RM, Presser S. Consequences of reducing non-response in a national telephone survey. Public Opin Q. 2000;64:125–148. doi: 10.1086/317759. [DOI] [PubMed] [Google Scholar]
- Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44(1):288–302. doi: 10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–433. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- Kristeller JL, Hoerr RA. Physician attitudes toward managing obesity: differences among six specialty groups. Prev Med. 1997;26(4):542–549. doi: 10.1006/pmed.1997.0171. [DOI] [PubMed] [Google Scholar]
- Kukaswadia A, Craig W, Janssena I, Picketta W. Obesity as a determinant of two forms of bullying in Ontario youth: a short report. Obesity facts Eur J Obes. 2012;4:469–472. doi: 10.1159/000335215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy BT, Williamson PS. Patient perceptions and weight loss of obese adults. J Fam Pract. 1988;27(3):285–290. [PubMed] [Google Scholar]
- Loureiro ML, Nayga RM., Jr Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62(10):2458–2468. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- McMorris BJ, Petrie RS, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Use of Web and in-person survey modes to gather data from young adults on sex and drug use: an evaluation of cost, time, and survey error based on a randomized mixed-mode design. Eval Res. 2009;33(2):138–158. doi: 10.1177/0193841X08326463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA. 1996;275 (21):1693–1697. [PubMed] [Google Scholar]
- Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(5):373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Pickett-Blakely O, Bleich SN, Cooper LA. Patient-physician gender concordance and weight-related counseling of obese patients. Am J Prev Med. 2011;40(6):616–619. doi: 10.1016/j.amepre.2011.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17 (5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Puhl R, Peterson JL, Luedicke J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int J Obes Lond. 2012;(4):162–169. doi: 10.1038/ijo.2012.110. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Koepsell TD, Wang J, et al. Comparison of telephone with World Wide Web-based responses by parents and teens to a follow-up survey after injury. Health Serv Res. 2011;46(3):964–981. doi: 10.1111/j.1475-6773.2010.01236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruelaz AR, Diefenbach P, Simon B, Lanto A, Arterburn D, Shekelle PG. Perceived barriers to weight management in primary care—perspectives of patients and providers. J Gen Intern Med. 2007;22(4):518–522. doi: 10.1007/s11606-007-0125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160(15):2334–2339. doi: 10.1001/archinte.160.15.2334. [DOI] [PubMed] [Google Scholar]
- Spruill TM, Pickering TG, Schwartz JE, et al. The impact of perceived hypertension status on anxiety and the white coat effect. Ann Behav Med. 2007;34(1):1–9. doi: 10.1007/BF02879915. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient–physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom DH, Hall MA, Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care. Health Aff (Millwood) 2004;23 (4):124–132. doi: 10.1377/hlthaff.23.4.124. [DOI] [PubMed] [Google Scholar]
- Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr. 2008;27(2):287–298. doi: 10.1080/07315724.2008.10719702. [DOI] [PMC free article] [PubMed] [Google Scholar]