Abstract
Objective
Inaccurate medication history at admission to hospitals leads to preventable adverse drug events, which in turn increase mortality, morbidity, and health care costs. The objective of this study was to investigate the role of pharmacists in identifying discrepancies in medication histories at admission to a tertiary referral hospital in Saudi Arabia.
Methods
We performed a prospective observational study in a 1200 bed tertiary hospital in Riyadh, Saudi Arabia. Patients were included if they were aged 16 years or older, were taking 5 or more medications, and were able to communicate or were accompanied by a caregiver who could communicate. Over 2 months in 2009, a pharmacist interviewed patients to ascertain all medications used prior to hospitalization, then all discrepancies were discussed with the admitting physician and unintended discrepancies were reported as errors.
Results
A pharmacist interviewed 60 patients who were taking 564 medications total. Of these patients, 65% were male, and their mean age was 62. Patients were taking an average of 9.4 medications. Twenty-two (37%) patients had at least one discrepancy, with the most common being omissions of medications (35%) and dosage errors (35%). The mean age for patients with discrepancies was 64.6 years, and without discrepancies, 60.8 years (P = 0.37).
Conclusion
Inaccurate medication history at admission to a hospital was common in Saudi Arabia. This has the potential to cause harm to patients if it remains undetected. Pharmacists could potentially play a major role in obtaining this medication history at the time of hospital admission.
Keywords: Medication errors, Transitions, Discrepancies
1. Introduction
Medication errors harm at least 1.5 million patients in the US every year, leading to 3.5 billion dollars in extra health care expenses to treat error-related injuries (Aspden et al., 2006). Studies have shown that 6.5% of hospitalized patients have adverse drug events (ADEs), and 28% of these events are preventable (Bates et al., 1995).
Medication errors can occur during hospitalization or at the time of a patient’s admission, transfer, or discharge from a hospital; transitions appear especially risky. Incomplete medication history at the time of hospital admission is responsible for up to 27% of all hospital prescribing errors (Tam et al., 2005). Therefore, accurate medication history was one of the patient safety solutions disseminated in 2007 by the World Health Organization (2007).
Studies have been conducted in North America, Europe, and Australia to describe the frequency and characteristics of medication history errors at admission to hospitals (Tam et al., 2005; Crook et al., 2007; Lubowski et al., 2007; Mersfelder and Bickel, 2008; Carter et al., 2006; Lau et al., 2000; Cornish et al., 2005; Vira et al., 2006). Errors in medication histories occurred in 10–61% of patients admitted to hospitals (Tam et al., 2005; Crook et al., 2007; Lubowski et al., 2007; Mersfelder and Bickel, 2008; Carter et al., 2006; Lau et al., 2000; Cornish et al., 2005; Vira et al., 2006). However, data are lacking regarding the magnitude of this patient safety issue in most developing countries.
Therefore, we performed a prospective study to investigate the role of pharmacists in identifying discrepancies in medication history at admission to hospitals in one developing country, Saudi Arabia. In Saudi Arabia, the same patient may be prescribed medications from physicians working in different hospitals, and routine communication between physicians or hospitals is lacking.
2. Methods
2.1. Setting and Participants
This prospective observational study was conducted at a tertiary, governmental 1200 bed hospital in the city of Riyadh, Saudi Arabia. Patients who are eligible for treatment in this hospital will not pay for all their inpatient and outpatient treatments, including prescribed medications. The hospital has both primary and specialized outpatient clinics. Prescribed medication histories for patients visiting these clinics can be accessed from the hospital health information system.
Most patients were recruited to the study while they were in the emergency department. The study was conducted over 2 months in 2009. Pharmacist who is working three days a week in the hospital recruited patients who were recently admitted to the hospital (<24 h) and met the inclusion criteria. We elected to include patients as soon as they were admitted to prevent potential harm from inaccurate medication histories. Patients were included in the study if they were aged 16 years or older, were taking 5 or more medications, and were able to communicate or were accompanied by a caregiver who could communicate. Patients receiving medications from other hospitals or clinics were excluded because of the difficulties in communicating with these hospitals and clinics to ascertain complete medication histories. The study was approved by the appropriate research and ethics committees and confidentiality was maintained throughout the study through the assignment of a code number for each patient.
2.2. Assessment of medication history
For eligible patients, a pharmacist screened the patient’s chart and reviewed recent lab results, discharge summaries, and all medications the patient was taking prior to hospitalization. Pharmacists interviewed patients to acquire a comprehensive medication history. At the beginning of each interview, the pharmacist introduced himself to the patient, explained the objectives of the study, and asked for the patient’s consent to be included in the study. Patients were asked to list all prescribed and over the counter medications they were using prior to hospitalization, including doses and frequency. The use of herbal and other supplements were also ascertained. At the end of the interview, the pharmacist answered the patient’s questions about the appropriate use of medications. All information obtained from patients was compared with medications recorded by the physician upon the patients’ admissions to the hospital.
2.3. Analyses
An inaccurate medication history was considered present if there was a discrepancy between the medication history obtained from the patient by the pharmacist and what was reported in the patient’s chart. Some discrepancies represent intentional adjustments of patient regimens by admitting physician. In this study, only unintentional discrepancies were considered as errors and included in the analysis. Since physicians may not document the reasons for changing a medication regimen on a patient’s chart, the pharmacist contacted the admitting physician and nurse to verify if a discrepancy was intentional or unintentional. Discrepancies were classified as omissions (not ordering a medication used by a patient prior to admission); commission (adding a medication not used prior to admission); or wrong dose, frequency, or route of administration.
Descriptive statistics were performed for demographic variables. The ch-i square test and t-test were used to compare categorical and continuous variables, respectively. The statistical package for social science (SPSS) software, version 17, was used for the analysis.
3. Results
Pharmacists interviewed 60 patients who were taking a total of 564 medications. Sixty-five percent were male, and the mean age was 62 years (standard deviation, 15.2; range, 16–86) (Table 1). Patients enrolled in the study were admitted under eleven various physician specialties (Table 2). The majority of patients (23%) were admitted to the medicine ward, followed by the emergency (21%) and cardiology (21%) wards. The mean number of medications was 9.4 (standard deviation, 5.7; range, 5–17), and the average time spent interviewing each patient and reviewing his or her medications was 20 min.
Table 1.
Characteristics of patients (n = 60).
| Variable | Value % (n) |
|---|---|
| Age (years) ⁎ | 62.2 (15.2) |
| Gender | |
| Male | 65 (39) |
| Female | 35 (21) |
| Education level | |
| Less than high school | 38 (23) |
| High school education | 22 (13) |
| College graduate | 40 (24) |
| Average number of medications⁎ | 9.4 (5.7) |
Mean (±SD).
Table 2.
Physician specialties under which patients was admitted to the hospital.
| Physician specialties | Percentage of patients (n = 60) |
|---|---|
| Medicine | 23 |
| Cardiology | 21 |
| Emergency | 21 |
| Nephrology | 7 |
| Surgery | 5 |
| Gastroenterology | 5 |
| Ophthalmology | 5 |
| Gynecology | 3 |
| Neurology | 3 |
| Oncology | 3 |
| Endocrinology | 2 |
| ENT | 2 |
Twenty-two (37%) patients had at least one discrepancy, and the most common discrepancies observed were omissions of medications (n = 15, 35%) and dosage errors (n = 15, 35%) (Fig. 1). Table 3 describes examples of medication discrepancies found after interviewing patients. These discrepancies have the potential of causing harm to patients if they remain undetected. The mean age for patients with a discrepancy was 64.6 years, and without a discrepancy, 60.8 years (P = 0.37). Thirty-nine percent of patients without a college degree had a discrepancy, while only 33.3% of patients with a college had a discrepancy (P = 0.67).
Figure 1.
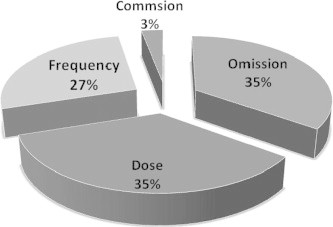
Incidence of discrepancies (Total number of discrepancies 43).
Table 3.
Examples of discrepancies in medication history.
| Discrepancy Type | Description |
|---|---|
| Omission | An essential eye drop medication to treat glaucoma (Latanoprost) was not ordered for the patient because the admitting physician was not ophthalmologist, the second day the patient had significant increase in the intraocular pressure |
| Omission | A patient with benign prostatic hyperplasia who was on Tamsulocin 0.4 mg once daily at home. On admission the Tamsulocin therapy was not ordered for the patient |
| Omission | Patient was on Amlodipine 5 mg once daily at home and was not ordered upon admission |
| Omission | Patient was on Bisoprolol 5 mg once daily at home and was not ordered upon admission |
| Dose | A diabetic patient on Metformin 500 mg three times daily at home but when admitted was prescribed instead Metformin 1 g three times daily |
| Dose | A patient at home was taking half tablet of digoxin 125 μg (62.5 μg) and half tablet of Bisoprolol 5 mg (2.5 mg), when admitted was prescribed digoxin 125 μg and Bisoprolol 5 mg. The reason for this error was misreading the symbols in the pharmacy computerized system by prescriber |
| Dose | Patient was on thyroxin 50 μg tablet at home, but the patient was prescribed thyroxin 100 μg in the hospital |
| Dose | A patient was on three tablet of thyroxin 25 μg (75 μg once daily) at home but the patient was prescribed thyroxin 25 μg once daily |
| Dose | A Patient admitted for cataract surgery was on Atorvastatin 20 mg daily at home and was started on 40 mg in the hospital |
| Dose | Phenytoin 300 mg three times daily was written by mistake to a patient who was on 300 mg once daily at home maintenance dose for epilepsy |
| Frequency | Warfarin 1 mg tablet twice daily was written by mistake to a patient who was on warfarin 4 mg once daily |
| Frequency | Erythropoietin 6000 units three times daily was written to a patient while the correct frequency was three times weekly |
4. Discussion
We evaluated the accuracy and completeness of medication histories acquired by healthcare providers upon hospital admission and found that 37% of patients admitted to a tertiary hospital had errors in their medication histories. The majority of these discrepancies consisted of omission or dosing errors. The reasons for these discrepancies included incorrect abstracts of patients’ medication lists from the health information system, not asking patients about their medications, and a lack of knowledge about the correct doses for prescribed medications. We assumed what patient reported as the current medication list. This study is the first such study from Saudi Arabia and one of few studies from a developing country.
A number of studies were carried out to describe the magnitude of inaccurate medication histories at the time of hospital admission (Crook et al., 2007; Lubowski et al., 2007; Mersfelder and Bickel, 2008; Carter et al., 2006; Lau et al., 2000; Cornish et al., 2005; Vira et al., 2006), and the frequency of discrepancies we found was lower than in some other studies. For example, a study conducted in Australia over a six-week period included 100 patients who were taking 1152 total medications. Discrepancies occurred in 84% of prescription medications (Crook et al., 2007), most of which were omitted medications (58%) and omitted doses and frequencies (32%). The mean number of discrepancies per patient was 9.7 (Crook et al., 2007). Another study conducted in The Netherlands in 1993 included 304 patients; approximately 67% of general medicine inpatients in this study experienced medication discrepancies on admission to a hospital (Lau et al., 2000). In Canada, over a three-month period in 2003, incomplete or inaccurate medication histories at admission occurred in about 54% of patients (Cornish et al., 2005). In our study, included patients only received medications from the same hospital. This made the process of ascertaining medication history by health care providers more accurate and complete, which is probably the reason that we found fewer discrepancies in this study compared to previous studies.
One important limitation of this study was that we were unable to assess the clinical outcomes of identified discrepancies since patients were interviewed within 24 h of admission. However, one study found that 59% of discrepancies in medication histories had the potential of causing bad clinical outcomes (Gleason et al., 2004).
Similar to our findings, previous studies have reported that medication omission is the most common type of medication error at the time of hospital admission. The rate of medication omission in our study (35%) was comparable to what was reported in the literature by Carter et al. (2006) (25%), Cornish et al. (2005) (46.4%), and Crook et al. (2007) (58.3%).
Pharmacists could potentially play a major role in ascertaining accurate and complete medication histories. Compared with other health care professionals, pharmacists are more familiar with drug names, therapeutic effects, available dosage forms and strengths, and routes of administration. When a pharmacist is involved in medication history-taking, hospital costs can be reduced and patients’ clinical outcomes improved (Vira et al., 2006; Gleason et al., 2004; Cavin and Sen, 2005; Nester and Hale, 2002; Bond et al., 1999, 2000, 2002; McFadzean et al., 2003). Studies showed that pharmacy students generally obtain accurate and complete medication histories (Lubowski et al., 2007; Mersfelder and Bickel, 2008). A prospective multi-centre study reported the value of involving Doctor of Pharmacy students in taking medication histories; these students identified 922 discrepancies in 330 patients, and 64% of discrepancies involved prescription medications (Lubowski et al., 2007).
This study has both clinical and research implications. Most hospitals in Saudi Arabia assign the task of medication history-taking to physicians or medical interns. Involving pharmacists in ascertaining medication histories has the potential to improve the completeness and accuracy of medication lists. Relying on hospitals’ health information systems will lead to inaccurate medication histories; therefore, it is important to link patients’ health information, including prescribed medications, from various health care systems. In the meantime, interviewing patients at the time of hospital admission is essential to obtain accurate medication histories. Further studies are needed to justify the cost of involving pharmacists in ascertaining medication histories in hospitals. Studies should examine the clinical outcomes associated with inaccurate medication histories, and these outcomes should be compared between pharmacist and control groups. Pharmacy students in Saudi Arabia start to learn and practice the skills of obtaining medication history while they are in college. This will empower them to start obtaining medication histories when they become pharmacists. It is therefore worth exploring the feasibility of pharmacy students’ obtaining medication histories during their internship.
In addition to the limitation noted earlier, this study has other limitations. Specifically, the study was conducted in only one large teaching hospital, so that the results might be different in other hospitals, especially if they are of different types. Furthermore, the results might be substantially different in other developing countries, especially as many have less resources than Saudi Arabia.
In conclusion, the current study shows that inaccurate medication histories at the time of hospital admission are common in Saudi Arabia. Pharmacists could play a major role in obtaining medication histories at the time of hospital admission, possibly preventing some of these inaccuracies. Further studies are needed to explore the clinical outcomes and cost savings of involving pharmacists in ascertaining medication histories.
Competing interest
None declared.
References
- Bates D.W., Cullen D.J., Laird N. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE prevention study group. JAMA. 1995;274(1):29–34. [PubMed] [Google Scholar]
- Bond C.A., Raehl C.L., Franke T. Clinical pharmacy services and hospital mortality rates. Pharmacotherapy. 1999;19(5):556–564. doi: 10.1592/phco.19.8.556.31531. [DOI] [PubMed] [Google Scholar]
- Bond C.A., Raehl C.L., Franke T. Clinical pharmacy services, pharmacy staffing, and the total cost of care in United States hospitals. Pharmacotherapy. 2000;20(6):609–621. doi: 10.1592/phco.20.7.609.35169. [DOI] [PubMed] [Google Scholar]
- Bond C.A., Raehl C.L., Franke T. Clinical pharmacy services, hospital pharmacy staffing, and medication errors in United States hospitals. Pharmacotherapy. 2002;22(2):134–147. doi: 10.1592/phco.22.3.134.33551. [DOI] [PubMed] [Google Scholar]
- Carter M.K., Allin D.M., Scott L.A. Pharmacist-acquired medication histories in a university hospital emergency department. Am. J. Health Syst. Pharm. 2006;63:2500–2503. doi: 10.2146/ajhp060028. [DOI] [PubMed] [Google Scholar]
- Cavin A., Sen B. Improving medication history recording and the identification of drug related problems in an A&E department. Hosp. Pharm. 2005;12:109–112. [Google Scholar]
- Philip Aspden, Julie Wolcott, J. Lyle Bootman, Linda R. Cronenwett, (Eds.), Committee on Identifying and Preventing Medication Errors, Preventing Medication Errors. Institute of Medicine National Academy Press, Washington, DC, 2006.
- Cornish P.L., Knowles S.R., Marchesano R. Unintended medication discrepancies at the time of hospital admission. Arch. Intern. Med. 2005;165(4):424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- Crook M., Ajdukovic M., Angley C. Eliciting comprehensive medication histories in the emergency department: the role of the pharmacist. Pharm. Prac. 2007;5(2):78–84. doi: 10.4321/s1886-36552007000200005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason K.M., Groszek J.M., Sullivan C. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am. J. Health Syst. Pharm. 2004;61(16):1689–1695. doi: 10.1093/ajhp/61.16.1689. [DOI] [PubMed] [Google Scholar]
- Lau H.S., Florax C., Porsius A.J. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine. Br. J. Clin. Pharmacol. 2000;49:597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubowski T.J., Cronin L.M., Pavelka R.W. Effectiveness of a medication reconciliation project conducted by PharmD students. Am. J. Pharm. Educ. 2007;71(5):94. doi: 10.5688/aj710594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadzean E., Isles C., Moffat J. Is there a role for a prescribing pharmacist in preventing prescribing errors in a medical asmission unit? Pharmaceut. J. 2003;270:896–899. [Google Scholar]
- Mersfelder T.L., Bickel R.J. Inpatient medication history verification by pharmacy students. Am. J. Health Syst. Pharm. 2008;65:2273–2275. doi: 10.2146/ajhp080013. [DOI] [PubMed] [Google Scholar]
- Nester T.M., Hale L.S. Effectiveness of a pharmacist acquired medication history in promoting patient safety. Am. J. Health Syst. Pharm. 2002;59:2221–2222. doi: 10.1093/ajhp/59.22.2221. [DOI] [PubMed] [Google Scholar]
- Tam C.V., Knowles S.R., Cornish P.L. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173(5):510–515. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vira T., Colquhoun M., Etchells E. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual. Saf. Health Care. 2006;15(2):122–126. doi: 10.1136/qshc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Patient Safety Solutions. 2007. Available from: <http://www.who.int/patientsafety/events/07/02_05_2007/en/index.html> (Accessed September 2010).


