Abstract
The purpose of the present study was to evaluate the transport of ascorbic acid, a water soluble molecule, through a predominantly lipophilic cornea. Thus in-vitro permeation of ascorbic acid from aqueous drops through freshly excised mammalian cornea was studied. Aqueous isotonic ophthalmic solutions of ascorbic acid of different concentrations (0.125% w/v to 2% w/v) (pH 5.4) were made. Further 1.0% w/v or 0.5% w/v ascorbic acid solution containing NaCl or dextrose as tonicity modifiers or Na+K+-ATPase inhibitors were also made. Permeation characteristics of drug were evaluated by putting 1 ml formulation on freshly excised cornea fixed between donor and receptor compartments of an all-glass modified Franz diffusion cell and measuring the drug permeated in the receptor by spectrophotometry at 265 nm, after 120 min. Statistical analysis was done by one-way analysis of variance (ANOVA) followed by Dunnett’s test or paired t-test. Increase in drug concentration in the formulation resulted in an increase in the quantity permeated but after a certain level increase in permeation with increase in concentration was minimal. Aqueous drops made isotonic with dextrose showed decreased permeation through paired cornea compared with aqueous drops made isotonic with NaCl from 1% w/v ascorbic acid solution suggesting likely involvement of Na+ co-transporter but there was decreased permeation through 0.5% w/v ascorbic acid solution made isotonic with NaCl as compared to solution made isotonic with dextrose. Further aqueous drops containing Na+K+-ATPase inhibitor {MAG-Mono Ammonium Glycyrrhizinate (25 μmol)} showed decreased corneal permeation from 0.5% w/v ascorbic acid solution but there was not significant decrease from 1% ascorbic acid solution since MAG is a competitive inhibitor of ascorbic acid. Aqueous drops containing Na+K+-ATPase inhibitor {MAG (50 μmol) or Ouabain (1 mmol)} showed decreased corneal permeation of ascorbic acid compared with control from 1% ascorbic acid solution confirming the involvement of Na+ co-transporter.
Keywords: Cornea, Permeation, Na+K+-ATPase inhibitors, MAG, Ouabain
1. Introduction
Humans are unable to synthesize ascorbic acid, it is therefore actively absorbed from the diet by sodium dependent transport systems in the intestine (Liang et al., 2001). Ocular tissue accumulates higher concentration of ascorbic acid than other tissues, because ocular ascorbic acid being an antioxidant defends the cornea & lens, against photo oxidative damage (Maurice and Riley, 1970; Koskela et al., 1989; Bode et al., 1991; Davies and Truscott, 2001; Valero et al., 2002).
Topical delivery into the conjuctival cul-de sac is by far the most common route of ocular drug delivery. Absorption from this site may be corneal or non corneal. The corneal absorption represents the major mechanism of absorption for most therapeutic entities. The cornea is a trilaminate structure consisting of three major diffusional barriers, epithelium, stroma and endothelium (Prausnitz and Noonan, 1998; Mitra, 2003). There are two general processes of drug absorption across barrier membranes (Grass and Robinson, 1988; Grass et al., 2006). The first type is called “the transcellular transport process,” where drug molecules have to go through the barrier cells to reach the circulation. Transcellular transport is typically a two step process, starting with drug uptake into the cells, and ending with drug efflux out of the cells. The second type is called “the paracellular transport process,” where the drug molecules travel between the cells (or in the gaps) to reach the circulation (Prausnitz and Noonan, 1998). The mechanism of transcellular transport includes simple diffusion, facilitated diffusion, active transport, endocytosis and exocytosis.
Eyes are under continuous oxidative stress that can lead to cataract. In case of cataract there is deficiency of ascorbic acid in eye fluid that can improve by increasing oral intake of ascorbic acid which is 60% and gets accumulated into eyes to protect it from oxidative stress, but at the same time chronic intake of oral mega doses of ascorbic acid is known to cause kidney stones (Lamden and Chrystowski, 1954; Briggs et al., 1973; Hughes et al., 1981). To nullify this problem delivery of ascorbic acid to eyes through cornea appears to be promising as compared to taking it orally. Transport of ascorbic acid, a water soluble molecule, through a predominantly lipophilic cornea offers a lot of challenge to the formulation chemist (Mitra, 2003) and the same forms the basis of the study.
2. Materials and methods
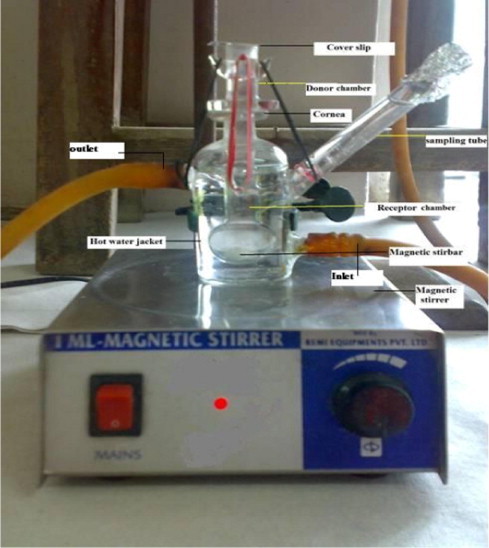
Ascorbic acid (99.97% pure) was obtained from Ranbaxy Laboratories (Gurgaon, India) as a gift sample. All other chemicals like Sodium Chloride (Qualigens), Sodium Hydroxide (Rankem), Hydrochloric acid (CDH Pharma) and Sodium bicarbonate (CDH Pharma) were also obtained. Mono Ammonium Glycyrrhizinate was obtained from Curewell Pharmaceutical (Faridabad) as gift sample & Ouabain Octahydrate (Sigma–Aldrich) obtained from National Institute of Immunology, New Delhi. Fresh eyeballs of goat, sheep, and buffalo were obtained from a local butcher shop (Ambedkar Nagar, New Delhi, India) within 1 h of the animal’s slaughtering. An all glass diffusion cell consisting of a receptor cell and donor cell was used for permeation studies. The apparatus was a modified version of the Franz diffusion cell as used by Malhotra and Majumdar. The receptor cell had an internal volume of 10 ml and side arm allowed sampling of receptor fluid. The donor cell was clamped onto the top of the receptor cell. Water at 37 °C was circulated through the water jacket surrounding the receptor cell and Teflon coated magnetic stir bar kept at the bottom of the receptor cell created a homogeneous receptor volume (Malhotra and Majumdar, 1997).
2.1. Method of permeation experiment
Freshly excised cornea was fixed between clamped donor and receptor compartments of an all-glass modified Franz diffusion cell in such a way that its epithelial surface faced the donor compartment. The receptor compartment contained 10 ml freshly prepared normal saline (pH 5.4), free from air bubbles. The corneal area available for diffusion was 0.45 cm2. An aliquot (1 ml) of aqueous drop formulation (freshly prepared ascorbic acid solution) was placed on the cornea and the opening of the donor cell was sealed with a glass cover slip; receptor fluid was kept at 37 °C with constant stirring using a Teflon coated magnetic stir bead. Permeation study was continued for 120 min, and samples were withdrawn from receptor and analyzed for ascorbic acid content by measuring absorbance at 265 nm in UV spectrophotometer (Shimadzu-1601, Kyoto, Japan). Results were expressed as amount permeated and percentage permeation or in vitro ocular availability. The permeation (%) or in vitro ocular availability was calculated as follows:
Permeation (%) = (amount of drug permeated in receptor/initial amount in donor) × 100
At the end of the experiment, each cornea (freed from adhering sclera) was weighed, soaked in 1 ml methanol, dried overnight at 90 °C, reweighed. From the difference in weights, corneal hydration was calculated. The permeation characteristics of ascorbic acid from control and various formulations were also evaluated through freshly excised paired goat, sheep, and buffalo corneas.
2.2. Preparation of test solutions
All solutions were made in distilled water and pH was adjusted to 5.4 with 1 N NaHCO3 and 0.01 N HCl solution using pH meter (Control Dynamics).
2.2.1. Ascorbic acid ophthalmic solutions of different concentration
The required amount of ascorbic acid was dissolved in a sufficient amount of distilled water, sodium chloride was added to make the final solution isotonic, the pH of the solution was adjusted to 5.4 using 1 N NaHCO3 and 0.1 N HCl, and distilled water was added as needed to bring the final volume up to 50 ml, creating solutions of 0.125%w/v (7.097 mmol), 0.25%w/v (mmol), 0.5%w/v (23.39 mmol), 75%w/v (42.58 mmol), 1%w/v (56.779 mmol), 1.25%w/v (70.974 mmol), 1.5%w/v (85.1692 mmol), and 2%w/v (113.56 mmol) concentration.
2.2.2. Ascorbic acid ophthalmic solutions (1% w/v or 0.5% w/v) containing different isotonicity modifiers
Ascorbic acid (1gm or 0.5 gm) was dissolved in sufficient amount of distilled water & made up the volume of final solution 50 ml with distilled water. One half of the solution was made isotonic with dextrose & other with NaCl, the pH of the solution was adjusted to 5.4 using 1 N NaHCO3 and 0.1 N HCl, and distilled water was added as needed to bring the final volume up to 50 ml, creating solutions having different tonicity modifiers.
2.2.3. Ascorbic acid ophthalmic solutions (1% w/v or 0.5% w/v) containing various Na+K+-ATPase inhibitors
Ascorbic acid was dissolved in sufficient amount of distilled water, sodium chloride was added to make the final solution isotonic & make up the volume of solution of 50 ml with distilled water. To one half of the solution Mono Ammonium Glycyrrhizinate (MAG) (Na+K+-ATPase inhibitor) (50 mmol or 50 mmol) or ouabain (1 mmol) was added, pH of the solution was adjusted to 5.4 and distilled water was added as needed to bring the final volume up to 50 ml, creating solutions containing various Na+K+-ATPase inhibitors.
2.2.4. Receptor media
For receptor media 0.9% NaCl solution having a pH of 5.4 was prepared. The adjustment of pH was done with 0.01 N HCl.
2.3. Statistical analysis
Statistical analyses were done by one-way ANOVA followed by Dunnett’s test. A paired t-test was used for studies with paired corneas. P value <0.05 was considered significant.
3. Results
Permeation results of ascorbic acid through freshly excised goat cornea from solutions of different concentration were shown in Table 1. In the concentration range of 0.125–0.75% w/v there was a linear increase in permeation through excised goat cornea. As the concentration was increased to 1%, there was a further increase in permeation. Further increase in concentration did not increase permeation significantly. Normal cornea has a hydration level of 75–80% (Maurice, 1971; Davies and Truscott, 2001). Corneal hydration observed in the present experiments was between 76 to 78%, indicating no damage to cornea.
Table 1.
Permeation of ascorbic acid through freshly excised goat cornea from solutions of different concentration. Values are mean ± SEM.
| Concentration (w/v) | Amount Permeated (mg) (120 min) | Permeation (%) (120 min) | Corneal Hydration (%) |
|---|---|---|---|
| 0.125% (7.097 mmol) | 0.014 ± 0.001 | 1.12 | 78.54 ± 0.65 |
| 0.25% (14.19 mmol) | 0.021 ± 0.001† | 0.83 | 78.55 ± 1.1 |
| 0.5% (23.39 mmol) | 0.03 ± 0.002† | 0.65 | 76.69 ± 0.83 |
| 0.75% (42.58 mmol) | 0.05 ± 0.003† | 0.62 | 78.53 ± 0.76 |
| 1.0% (56.78 mmol) | 0.089 ± 0.003† | 0.89 | 76.61 ± 0.76 |
| 1.25% (70.974 mmol) | 0.099 ± 0.01† | 0.79 | 77.2 ± 1.1 |
| 1.5% (85.17 mmol) | 0.104 ± 0.003† | 0.69 | 78.5 ± 0.70 |
| 2.0% (113.56 mmol) | 0.104 ± 0.001† | 0.52 | 77.79 ± 0.86 |
Statistically significant (P < 0.05) compared with solution of 0.125% concentration as determined by one-way ANOVA followed by Dunnett’s test.
To ascertain Na+ dependency of the transport of ascorbic acid 0.5% w/v (23.39 mmol) or 1% w/v (56.78 mmol) solution was made isotonic either with NaCl or dextrose. The pH was adjusted to 5.4 as before. The study was conducted with paired goat corneas i.e. one cornea of an animal received formulation made isotonic with sodium chloride while the contra lateral cornea received formulation made isotonic with dextrose. Permeation results (Table 2) showed increase in transport of ascorbic acid in presence of dextrose from 0.5% w/v (23.39 mmol) ascorbic acid solution indicating involvement of GLUT transporter. However with 1% w/v solution of ascorbic acid there was increase in permeation in the presence of NaCl. Corneal hydration remained in the normal range.
Table 2.
Permeation of ascorbic acid through freshly excised goat cornea (paired) from solutions made isotonic with NaCl or Dextrose. Values are mean ± SEM of 3 corneas in each group.
| Concentration (w/v) | Tonicity adjusting substances | Amount permeated (mg) (120 min) | Permeation (%) (120 min) | Corneal hydration (%) |
|---|---|---|---|---|
| 0.50% | NaCl∗ | 0.025 ± 0.004 | 0.5 | 75.04 ± 2.8 |
| Dextrose | 0.035 ± 0.01† | 0.98 | 77.22 ± 2.1 | |
| 1.0% | NaCl∗ | 0.075 ± 0.01 | 0.75 | 78.54 ± 0.621 |
| Dextrose | 0.048 ± 0.006† | 0.35 | 78.15 ± 0.31 |
Statistically significant (P < 0.05) compared with solution containing NaCl as determined by paired t-test.
To ascertain the role of Na+ co-transporters in the transport of ascorbic acid from 1% w/v solution, the experiment was repeated using paired corneas of sheep & buffalo. The results (Table 3) indicate marked reduction in permeation of ascorbic acid in the presence of dextrose in both the corneas similar to goat cornea. Corneal hydration remained in the normal range 76–78% indicating no damage to cornea.
Table 3.
Permeation of ascorbic acid through freshly excised goat, sheep and buffalo cornea (paired) from solutions made isotonic with NaCl or Dextrose. Values are mean ± SEM of 3 corneas in each group.
| Cornea | Tonicity adjusting substances | Amount permeated (mg) (120 min) | Permeation (%) (120 min) | Corneal hydration (%) |
|---|---|---|---|---|
| Goat | NaCl∗ | 0.075 ± 0.01 | 0.75 | 78.54 ± 0.621 |
| Dextrose | 0.048 ± 0.006† | 0.35 | 78.15 ± 0.31 | |
| Sheep | NaCl∗ | 0.059 ± 0.007 | 0.59 | 77.58 ± 0.37 |
| Dextrose | 0.043 ± 0.005† | 0.43 | 78.77 ± 0.42 | |
| Buffalo | NaCl∗ | 0.027 ± 0.0 | 0.27 | 75.44 ± 0.26 |
| Dextrose | 0.013 ± 0.0† | 0.13 | 76.32 ± 0.56 |
Statistically significant (P < 0.05) compared with solution containing NaCl as determined by paired t-test.
To confirm the involvement of Na+ in the transport of ascorbic acid, ascorbic acid 0.5% w/v (23.39 mmol) or 1% w/v (56.78 mmol) solution (pH 5.4, tonicity adjusted with sodium chloride) containing 25 μmol of MAG (competitive Na+–K+ ATPase inhibitor) was made, and permeation study was conducted with paired goat corneas i.e. one cornea of an animal received formulation containing MAG (25 μmol) while the contra lateral cornea received formulation without MAG (control). The results (Table 4) showed significant reduction in permeation of ascorbic acid from 0.5% w/v solution but there was no reduction in permeation from 1% w/v ascorbic acid solution. Further MAG concentration was increased from 25 to 50 μmol. Permeation studies with paired goat cornea (Table 5) showed that permeation of ascorbic acid was almost halved in the presence of MAG (50 μmol). When the experiment was repeated using Ouabain, a more specific Na+–K+ ATPase inhibitor, similar inhibition on permeation of ascorbic acid was observed.
Table 4.
Permeation of ascorbic acid through freshly excised goat cornea (paired) from the solution containing MAG (Na+–K+ ATPase inhibitor, 25 μmol). Values are mean ± SEM of 3 corneas in each group.
| Concentration (w/v) | Amount permeated (mg) (120 min) | Permeation (%) | Corneal hydration (%) | |
|---|---|---|---|---|
| 0.50% | Control | 0.06 ± 0.008 | 1.18 | 76.48 ± 0.48 |
| MAG | 0.04 ± 0.01† | 0.85 | 76.39 ± 1.33 | |
| 1.0% | Control | 0.09 ± 0.001 | 0.86 | 77.95 ± 1.66 |
| MAG | 0.08 ± 0.00† | 0.82 | 78.25 ± 1.62 |
Statistically significant (P < 0.05) compared with solution without MAG (control) as determined by paired t-test.
Table 5.
Permeation of ascorbic acid through freshly excised goat cornea (paired) from solution containing MAG (Na+–K+ ATPase inhibitor, 50 μmol) or Ouabain (Na+–K+ ATPase inhibitor, 1 mmol). Values are mean ± SEM of 3 corneas in each group.
| Concentration (w/v) | Amount permeated (mg) (120 min) | Permeation (%) (120 min) | Corneal hydration (%) | |
|---|---|---|---|---|
| 1.0% | Control | 0.087 ± 0.006 | 0.87 | 78.65 ± 1.46 |
| MAG∗ | 0.047 ± 0.003† | 0.47 | 77.15 ± 1.52 | |
| 1.0% | Control | 0.11 ± 0.017 | 1.1 | 79.64 ± 1.34 |
| Quabain | 0.066 ± 0.003† | 0.66 | 75.69 ± 1.67 |
Statistically significant (P < 0.05) compared with solution without MAG or without Ouabain (control) as determined by paired t-test.
4. Discussion
Rabbit corneal epithelium has been reported to contain Na+ transporters for ascorbic acid uptake (Bode et al., 1991; Talluri et al., 2006). The present study indicates, that from 1% w/v solution of ascorbic acid there was increase in permeation through goat cornea in presence of NaCl as compared to solution made isotonic with dextrose, suggesting likely the involvement of Na+ co-transporters. There was a marked reduction in permeation of ascorbic acid in presence of dextrose in both sheep and buffalo corneas similar to goat cornea suggesting contribution of Na+ co-transporters. Liang et al. (2001) studied that cellular uptake of ascorbic acid mediated by Na+ dependent ascorbic acid transporters (SVCT1 and SVCT2) that was further confirmed by Subramaniam et al. (2008). Since MAG is a competitive inhibitor, with increase in ascorbic acid concentration up to 1% w/v, the inhibitive effect on permeation could be decreased (Cooperstein, 1987; Song, 2002). The present study suggests, with increase in MAG concentration there was increased inhibitive effect on permeation of ascorbic acid from 1% solution through goat cornea and the same found with ouabain. Thus the study supports the involvement of Na+ transporters in ascorbic acid transport. Corneal hydration remained in the normal range which indicated no damage to cornea.
5. Conclusion
Talluri et al. (2006) showed the involvement of Na+ dependent transporter in the transport of ascorbic acid through rabbit cornea. Our finding suggests that the presence of Na+ dependent transporters in the cornea of goat, sheep and buffalo could be responsible for transport of ascorbic acid at low concentration. However further studies are needed to consolidate the fact.
Contributor Information
Shivali Singla, Email: singlashivali@gmail.com.
D.K. Majumdar, Email: dkmajumdaar@yahoo.com.
Sachin Goyal, Email: sachin_goyal14@yahoo.com.
Gurudas Khilnani, Email: drgurudas@gmail.com.
References
- Bode A.M., Vanderpool S.S., Carlson E.C., Meyer D.A., Rose R.C. Ascorbic acid uptake and metabolism by corneal endothelium. Invest. Opthalmol. Vis. Sci. 1991;32:2266–2271. [PubMed] [Google Scholar]
- Briggs M.H., Garcia-Webb P., Davies P. Urinary oxalate and vitamin-C Supplements. Lancet. 1973;2:201. doi: 10.1016/s0140-6736(73)93029-8. [DOI] [PubMed] [Google Scholar]
- Cooperstein P.F. Na+–K+ ATPase activity & transport process in toad corneal epithelium. Comp. Biochem. Phys. A. 1987;87:11119–11121. doi: 10.1016/0300-9629(87)90048-x. [DOI] [PubMed] [Google Scholar]
- Davies M.J., Truscott R.J.W. Photo-oxidation of proteins and its role in cataractogenesis. J. Photochem. Photobiol. B. 2001;63:114–125. doi: 10.1016/s1011-1344(01)00208-1. [DOI] [PubMed] [Google Scholar]
- Grass G.M., Robinson J.R. Mechanism of corneal drug penetration I: in vivo and in vitro kinetics. J. Pharm. Sci. 1988;77:3–14. doi: 10.1002/jps.2600770103. [DOI] [PubMed] [Google Scholar]
- Grass G.M., Cooper E.R., Robinson J.R. Mechanisms of corneal drug penetration III: modeling of molecular transport. J. Pharm. Sci. 2006;77:124–126. doi: 10.1002/jps.2600770105. [DOI] [PubMed] [Google Scholar]
- Hughes C., Dutton S., Truswell A.S. High intakes of ascorbic acid and urinary oxalate. J. Hum. Nutr. 1981;35:274–280. doi: 10.3109/09637488109143053. [DOI] [PubMed] [Google Scholar]
- Koskela T.K., Reiss G.R., Brubaker R.F., Ellefsonf R.D. Is the high concentration of ascorbic acid in the eye an adaptation to intense solar irradiation? Invest. Ophthalmol. Vis. Sci. 1989;30:2265–2267. [PubMed] [Google Scholar]
- Lamden M.P., Chrystowski G.A. Urinary oxalate excretion by man following ascorbic acid ingestion. Proc. Soc. Exp. Biol. Med. 1954;85:190–192. doi: 10.3181/00379727-85-20827. [DOI] [PubMed] [Google Scholar]
- Liang W.J., Johnson D., Jarvis S.M. Vitamin C transport systems of mammalian cells. Mol. Membr. Biol. 2001;18:87–95. doi: 10.1080/09687680110033774. [DOI] [PubMed] [Google Scholar]
- Malhotra M., Majumdar D.K. In vitro transcorneal permeation of ketorolac tromethamine from buffered and unbuffered aqueous ocular drops. Ind. J. Exp. Biol. 1997;35:941–947. [PubMed] [Google Scholar]
- Maurice D.M. Tonicity of eye drops and its dilution by tears. Exp. Eye. Res. 1971;11:30–33. doi: 10.1016/s0014-4835(71)80061-1. [DOI] [PubMed] [Google Scholar]
- Maurice D.M., Riley M.V. Ocular pharmacokinetics. In: Graymore C.N., editor. Biochemistry of the eye. Academic Press; London: 1970. pp. 6–16. [Google Scholar]
- Mitra A.K. second ed. Marcel Dekker Inc.; New York: 2003. Ophthalmic drug delivery systems. [Google Scholar]
- Prausnitz M.R., Noonan J.S. Permeability of cornea, sclera, and conjunctiva: a literature analysis for drug delivery to the eye. J. Pharm. Sci. 1998;87:1479–1488. doi: 10.1021/js9802594. [DOI] [PubMed] [Google Scholar]
- Song J. Flavonoid inhibition of sodium-dependent vitamin C transporter 1 (SVCT1) and glucose transporter isoform 2 (GLUT2), intestinal transporters for vitamin C and glucose. J. Biol. Chem. 2002;277:15252–15260. doi: 10.1074/jbc.M110496200. [DOI] [PubMed] [Google Scholar]
- Subramaniam V.S., Marchent J.S., Reidling J.C., Said H.M. N-Glycosylation is required for Na (+)-dependent vitamin C transporter functionality. Biochem. Biophys. Res. Commun. 2008;374:123–127. doi: 10.1016/j.bbrc.2008.06.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talluri R.S., Katragadda D., Mitra A.K. Mechanism of L-ascorbic acid epithelial cells: evidence for the involvement of sodium dependent vitamin C transporter. Curr. Eye Res. 2006;31:481–489. doi: 10.1080/02713680600693629. [DOI] [PubMed] [Google Scholar]
- Valero M.P., Fletcher A.F., Stavola B.L.D., Vioque J., Alepuz V.C. Vitamin C is associated with reduced risk of cataract in a mediterranean population. J. Nutr. 2002;132:1299–1306. doi: 10.1093/jn/132.6.1299. [DOI] [PubMed] [Google Scholar]


