Abstract
Objective:
To compare diagnostic performances of two reduced z-axis coverages to full coverage of the abdomen and pelvis for the diagnosis of acute appendicitis and alternative diseases at unenhanced CT.
Methods:
This study included 152 adults suspected of appendicitis who were enrolled in two ethical committee-approved previous prospective trials. Based on scans covering the entire abdomen and pelvis (set L), two additional sets of images were generated, each with reduced z-axis coverages: (1) from the top of the iliac crests to the pubis (set S) and (2) from the diaphragmatic crus to the pubis (set M). Two readers independently coded the visualisation of the appendix, measured its diameter and proposed a diagnosis (appendicitis or alternative). Final diagnosis was based on surgical findings or clinical follow-up. Fisher exact and McNemar tests and logistic regression were used.
Results:
46 patients had a definite diagnosis of appendicitis and 53 of alternative diseases. The frequency of appendix visualisation was lower for set S than set L for both readers (89% and 84% vs 95% and 91% by Readers A and B, respectively; p=0.021 and 0.022). The probability of giving a correct diagnosis was lower for set S (68%) than set L (78%; odds ratio, 0.611; p=0.008) for both readers, without significant difference between sets L and M (77%, p=0.771); z-axis coverage being reduced by 25% for set M.
Conclusion:
Coverage from diaphragmatic crus to pubis, but not focused on pelvis only, can be recommended in adults suspected of appendicitis.
Advances in knowledge:
In suspected appendicitis, CT-coverage can be reduced from diaphragmatic crus to pubis.
CT is a well-established diagnostic tool in patients suspected of acute appendicitis because of its availability, high reproducibility, excellent diagnosis performance and low discomfort [1,2]. Since the emergence of multidetector-row CT (MDCT), the ability to rapidly scan large ranges along the z-axis makes it tempting to scan the entire abdomen and pelvis in all patients suspected of any abdominal disorder in order to also detect any alternative and/or additional diseases [3–5]. As individuals suspected of acute appendicitis are generally young—with a mean age approximating 30 years [6]—radiation dose is of particular concern, and all effort should be made to restrict exposure to the absolute minimum required for sufficient diagnosis.
Limiting z-axis coverage is an easy way to reduce the radiation dose [7]. High diagnostic performance of pelvic- and appendiceal-focused CT has been reported for acute appendicitis [2,8–13], but only two studies have compared appendiceal-focused CT with scans on the entire abdomen and pelvis [2,13]. However, these studies used various administration protocols involving intravenous (IV) and enteric contrast material, preventing us generalising their results. A third study has reported that limiting CT acquisition to the pelvis could result in 7% of missed alternative diseases because of their location. In this study, the readers classified the anatomic location of CT abnormalities as abdominal (above the iliac crest) or pelvic (below the iliac crest) [8]. Finally, a very recent study by Pooler et al [14] assessed CT in the diagnosis of alternative diseases in 1571 patients suspected of acute appendicitis. The authors advocated that the appendix itself as well as alternative diseases may not be demonstrated by CT acquisition limited to the pelvis. Therefore, they suggested an investigation of the rates of alternative diagnosis detectable at focused pelvic CT.
We hypothesised that an optimal z-axis coverage ranging from the diaphragmatic crus (easily seen on the frontal scout view and at least 2 cm above the top of the kidney) to the upper aspect of the pubic symphysis would allow us to accurately diagnose acute appendicitis as well as alternative diseases with substantial dose reduction compared with scanning the entire abdomen and pelvis (i.e. from the top of the liver to the lowest part of the ischiopubic branches). This coverage will be referred to in this paper as “restricted abdominal coverage”. The purpose of this study, therefore, was to compare two types of reduced coverage (the restricted abdominal coverage as defined above and that focused on the pelvis only) to coverage that included the entire abdomen and pelvis and to evaluate the diagnostic performance of each for acute appendicitis and alternative diseases.
METHODS AND MATERIALS
Patients
This study includes patients who were enrolled in two previous ethical committee-approved clinical trials, which aimed to investigate the diagnostic performance of CT in patients suspected of acute appendicitis [15,16]. In these two prospective trials, consecutive adult patients seen in the emergency room (between March 2002 and December 2002 for the first trial and between May 2005 and November 2006 for the second trial) were asked to participate. Inclusion criterion was acute right lower quadrant abdominal pain for which CT examination was requested by the physician to evaluate for possible acute appendicitis. In order to consider patients who were examined with the same scan protocol in terms of contrast material administration in these two previous trials, only those who had unenhanced CT (without any enteric or IV contrast) were included in the present study sample (n=160). Among these 160 patients, 8 (3 with acute appendicitis, 1 with epiploic appendagitis and 4 with non-specific abdominal pain) were excluded because the CT scans were irretrievable from our hard disc. In the present study, 152 patients were thus included—86 (51 females, 35 males) from our first trial and 66 (37 females, 29 males) from our second trial [15,16]. The patients were aged from 16 to 82 years [mean age 36 ± 17 (standard deviation, SD) years]. The mean body mass index was 23.9 ± 4.2 kg m−2 (range 16.4–45.7). Study protocol was approved by the institutional ethic committee. Written informed consent had been previously obtained from all patients or, for those younger than 18 years, from their parents.
CT examinations
All patients were examined in the supine position using a commercially available scanner with four detector rows (Somatom® Plus Volume Zoom; Siemens Healthcare, Forchheim, Germany). A frontal 512 mm scout view was first obtained with 120 kVp and 50 mA. This was followed by an abdominal helical scan from the top of the liver to the lowest part of the ischiopubic branches with 4×2.5 mm collimation at 120 kVp and 100 effective milliampere second. The pitch was 1.5:1 resulting from a table feed of 15 mm per 0.5 s scanner rotation. Acquisitions were performed without automated exposure control (AEC) devices because these systems were not available on our scanners at the time of enrolment. We did not use weight-specific tube current products since the relationship between body size parameters for individual dose adaptation in body CT of adults had not been implemented in our clinical routine at that time [17]. None of the patients received oral, rectal or IV contrast material, such protocol yielding high diagnostic performance even for alternative diseases as compared with enhanced CT [16,18–20]. From the raw data of the acquisition, 3-mm-thick axial sections were reconstructed with a 1.5 mm increment.
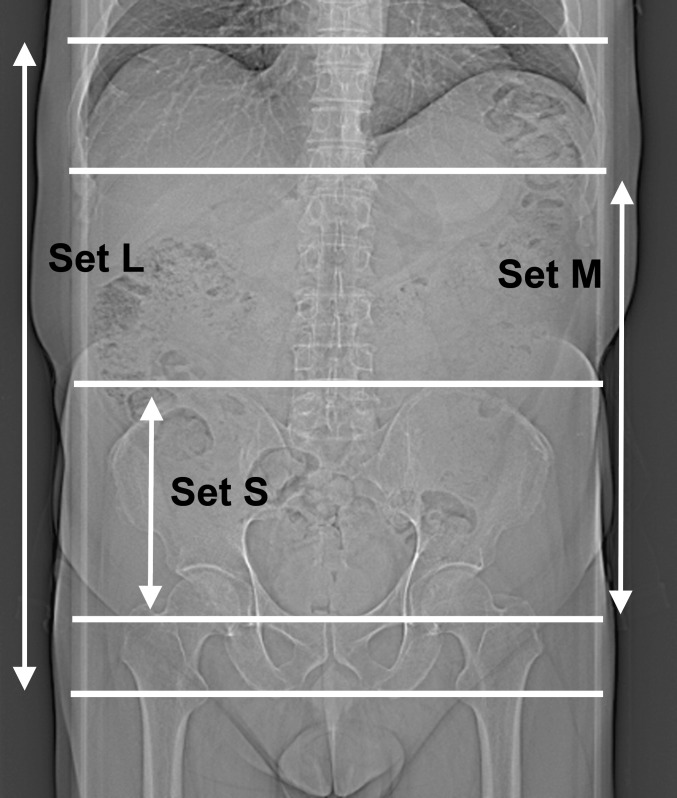
From the original set of axial images covering the entire abdomen and pelvis (long or set L; Figure 1), two additional sets were generated with two different reduced z-axis coverages. The smallest coverage (corresponding to the pelvic-focused coverage) was generated from the top of the iliac crests to the upper aspect of the pubis (small or set S; Figure 1). The intermediate coverage (corresponding to the restricted abdominal coverage) was generated from the diaphragmatic crus to the upper aspect of the pubis (medium or set M; Figure 1). Since the image sets were retrospectively generated and original frontal scout views were not available, we generated a coronal image simulating the frontal scout view for the purpose of this study. It was obtained on the three-dimensional functionality of the workstation (Syngo® Multimodality Workplace; Siemens Healthcare, Forchheim, Germany) by a 300-mm-thick coronal multiplanar reformated image based on the original set of axial images. The upper and lower limits of the restricted abdominal coverage (set M) were determined on this simulated frontal scout view as shown in Figure 2.
Figure 1.
Frontal scout view with upper and lower boundaries of each set.
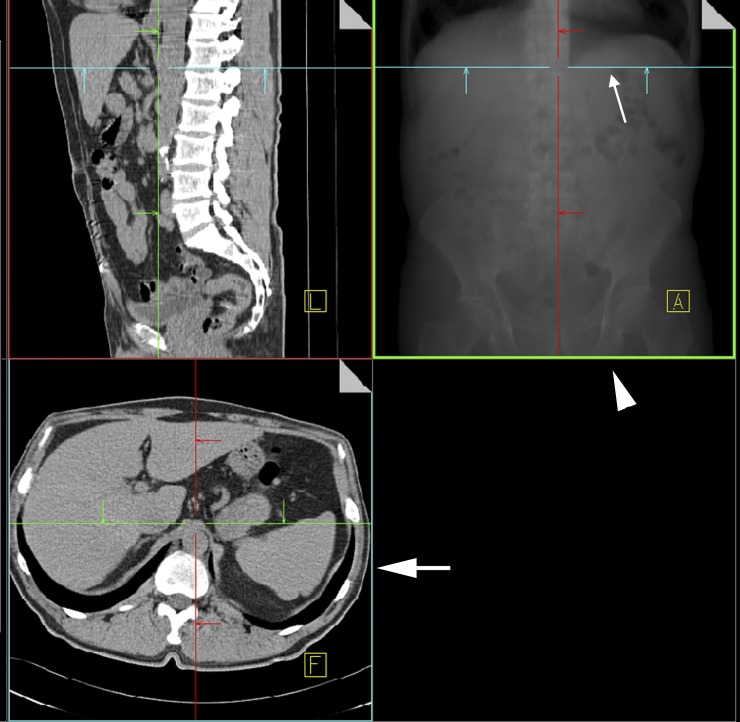
Figure 2.
Screen capture showing a 300-mm-thick coronal multiplanar reformated (MPR) image (thick arrowhead) obtained with three-dimensional functionality of the workstation (Syngo® Multimodality Workplace; Siemens Healthcare, Forchheim, Germany) and simulating a frontal scout view. The horizontal line (thin arrow) on the thick MPR image corresponds to the upper boundary of our restricted abdominal coverage and is at the level of the axial image seen in the left lower quadrant (thick arrow).
Image analysis
Patient information was erased from all images and the sets were loaded on a clinical workstation with interactive multiplanar reconstruction functionalities (3D, Syngo Multimodality Workplace) and interpreted independently by two board-certified radiologists (Readers A and B) with 13 and 9 years of experience, respectively, in reading abdominal CT in a clinical routine; neither of whom had been involved in the readings of either of our previous studies. Readers were aware that patients were clinically suspected of acute appendicitis, but they were blinded to CT reports, surgical and pathological findings and clinical follow-ups. Readers were free to interpret the scans in any plane with the multiplanar reconstruction display. Readings were performed in three separate and independent sessions (each session stretching over several days but not over one single day) with at least 2 weeks' interval. Images from set S were read in the first session, images from set M in the second session and images from set L in the third session. At each session, patients were presented in a random order determined by a free online random integer generator [21].
On each image set, readers first recorded independently whether the appendix was visible or not, measured its diameter (if visible) and proposed an overall diagnosis of acute appendicitis or alternative disease that could explain the abdominal pain. Incidental findings that could not explain this pain were not considered. Thereafter, readers reviewed in consensus the examinations with discrepancies in alternative disease between readers and/or between sets and determined whether these discrepancies could be explained by restricting z-axis coverage.
Final diagnosis
The final diagnosis was made during the two previous trials. It was based on the surgical findings or, for the patients who did not undergo surgery, on clinical follow-up and other diagnostic procedures (laboratory findings, colonoscopy with biopsy, barium enema study, vaginal smear and/or contrast material-enhanced MDCT). Information from the clinical follow-up was obtained by reviewing the medical charts and by telephone calls 1 month after the acute episode. These data were recorded by a radiologist that was not involved in the readings. In 62 patients of those included in the present study, the definite diagnosis was made on the basis of the surgical findings. In 90 patients, the definite diagnosis was made on the basis of other diagnostic procedures and clinical follow-up. No patient was lost to follow-up.
Radiation dose
The absorbed radiation dose per acquisition, expressed as the volume CT dose index (CTDIvol), was calculated using commercially available software (CT-Expo v. 2.0; G. Stamm, Medizinische Hochschule, Hanover, Germany) installed on a personal computer. With the CT parameters that we used, the calculated CTDIvol was 9 mGy. We multiplied the coverage length of each set by the CTDIvol to obtain the dose–length product (DLP) of each set, reflecting the effective dose, i.e. the tube output, for each set. The coverage length was calculated on the basis of z-axis table positions at the boundaries of each set.
Statistical analysis
Continuous quantitative variables are summarised by their mean and standard error of the mean. Proportions were compared using Fisher’s exact tests or McNemar tests when appropriate. Means of the continuous variables (appendiceal diameters) were compared using the analysis of variance (ANOVA) test. Binary logistic regressions (“Enter” procedure) were used to evaluate the possible influence of z-axis coverage and of readers on the probability of correct diagnosis (acute appendicitis and/or alternative disease). Corresponding odds ratios (ORs) were calculated with 95% confidence intervals. Statistical significance for all tests was set at p<0.05. Statistical software used included SPSS® for Windows (IBM SPSS Statistics v. 20, Somers, NY) and MedCalc (v. 12.2, Mariakerke, Belgium).
RESULTS
Final diagnosis
46 patients (30%) were classified as definitely having acute appendicitis confirmed by microscopic examination of the surgical specimen. 53 patients (35%) had alternative disease as listed in Table 1. One man had two simultaneous alternative diseases (cholecystitis and caecal volvulus). 53 patients (35%) were considered to have non-specific abdominal pain (NSAP) because their symptoms could not be elucidated by any diagnostic method and resolved spontaneously. There was no statistically significant difference in gender ratio according to the final diagnosis (p=0.226).
Table 1.
Alternative diseases
| Disease | Number of patients |
| Ileitis and/or colitis | 9 |
| Pyelonephritis | 9 |
| Pelvic inflammatory disease | 6 |
| Diverticulitis | 5 |
| Right ureteral stone | 5 |
| Mesenteric adenitis | 3 |
| Ovarian cyst | 3 |
| Lower right lobe pneumonia | 3 |
| Acute cholecystitis | 2 |
| Ileal occlusion | 2 |
| Perforated gastric ulcer | 2 |
| Epiploic appendagitis | 1 |
| Caecal neoplasia | 1 |
| Caecal volvulus and acute cholecystitis | 1 |
| Cystitis | 1 |
Visualisation and diameter of the appendix
The number of patients in whom the appendix was visible for each set and by each reader is listed in Table 2. Considering the entire study group, there was no statistically significant difference in the frequency of visualised appendix between readers for each set (p ranging from 0.109 to 0.180). This frequency was lower for set S than for set L by each reader (p=0.021 and 0.022). For Reader B, it was lower for set S than for set M (p=0.049) but not for Reader A (p=0.118). There was no statistically significant difference between set M and set L for each reader (p=0.687 and 1.000). In patients with a final diagnosis of acute appendicitis, the frequency of visualised appendix (which ranged from 96% for set S and 100% for L) did not significantly differ among sets for either reader (p=1.000). In set S, the appendix was not visualised in the same two patients with acute appendicitis by each reader, whereas in sets M and L, it was visualised by both readers. In contrast, the appendix was not visualised in two other patients in set M—in separate patients by each reader—but was visualised in set L and, more importantly, in set S by both readers. In set M, the 2% of non-visualised appendix could thus be considered as the consequence of reader variability and not as the result of difference in coverage. No case of acute appendicitis was thus not visible in set M. Examples of acute appendicitis with an appendix above the iliac crest (and thereby non-visible in set S) are shown in Figures 3 and 4.
Table 2.
Appendiceal diameter and frequency of visualisation of the appendix
| Set S | Set M | Set L | |||||
| Reader A | Reader B | Reader A | Reader B | Reader A | Reader B | ||
| Entire study group | Diametera | 8.4±0.3 | 8.3±0.3 | 8.2±0.4 | 8.2±0.3 | 8.4±0.3 | 8.3±0.3 |
| Visualised appendixb | 135/152 (89) | 128/152 (84) | 142/152 (93) | 137/152 (90) | 144/152 (95) | 138/152 (91) | |
| Patients with definite acute appendicitis | Diametera | 12.0±0.6 | 11.4±0.5 | 11.9±0.5 | 11.3±0.5 | 12.3±0.5 | 11.4±0.4 |
| Visualised appendixb | 44/46 (96) | 44/46 (96) | 45/46 (98) | 45/46 (98) | 46/46 (100) | 46/46 (100) | |
| Patients without definite acute appendicitis | Diametera | 6.5±0.3 | 6.7±0.2 | 6.3±0.2 | 6.6±0.2 | 6.3±0.2 | 6.4±0.2 |
| Visualised appendixb | 91/106 (86) | 84/106 (79) | 97/106 (92) | 92/106 (87) | 98/106 (93) | 92/106 (87) | |
Data are mean diameter in millimetres ± standard error of the mean.
Data in parentheses correspond to percentages.
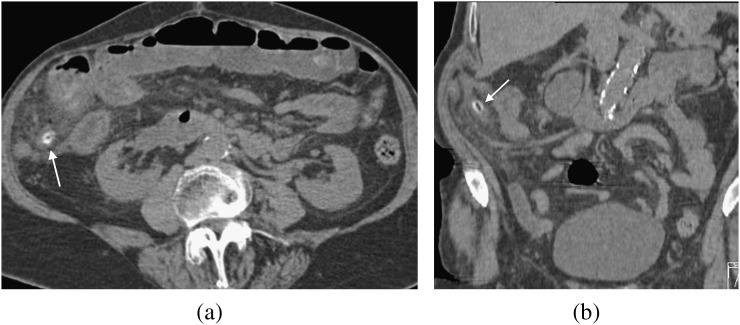
Figure 3.
Unenhanced CT images obtained in an 83-year-old female with definite diagnosis of acute appendicitis. Axial (a) and coronal (b) reformations of a restricted abdominal coverage show enlarged appendix (arrow) containing an appendicolith and periappendiceal fat stranding. The appendix is located above the iliac crest and was not visualised with pelvic focused coverage (set S) by both readers.
Figure 4.
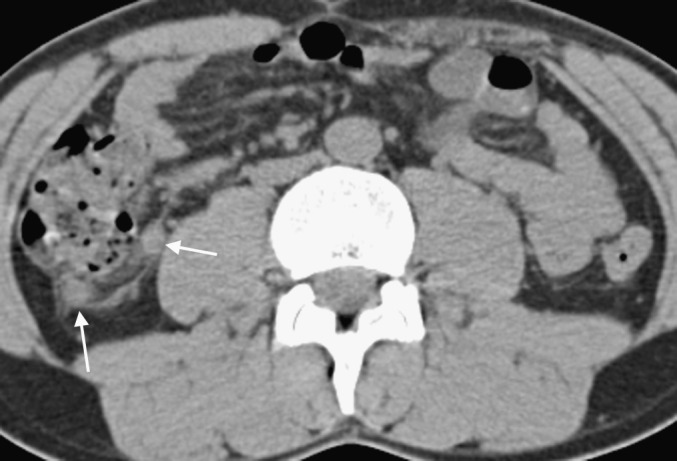
Unenhanced axial CT image obtained in a 30-year-old male with definite diagnosis of acute appendicitis showing an enlarged appendix (arrows) and periappendiceal fat stranding. The appendix is located above the iliac crest and was not visualised with pelvic focused coverage (set S) by both readers.
Mean diameters of the appendix as measured by each reader for each set are summarised in Table 2. The mean diameter of the appendix was significantly larger in patients with acute appendicitis than in those without appendicitis (p<0.001).
Misclassifications compared with definite diagnosis
In the patient with acute cholecystitis and caecal volvulus, each diagnosis was correctly made by both readers for sets M and L, but only caecal volvulus was diagnosed for set S. As only one correct diagnosis was not sufficient, we considered the findings by both readers as misclassified for set S. Of the 106 patients without acute appendicitis (53 with a definite alternative disease and 53 with NSAP), diagnosis was misclassified in 36 and 43 patients in set S, 24 and 32 patients in set M and 22 and 32 patients in set L by Readers A and B, respectively. Considering the entire study population, the logistic regression revealed that the probability of correct classification of the final diagnosis (acute appendicitis, alternative diseases or NSAP) was influenced by z-axis coverage—being significantly lower for set S than for set L (OR=0.611, p=0.008)—and not by the reader (p=0.056). Of the 46 patients with acute appendicitis, the logistic regression revealed that the probability of correct classification of the final diagnosis (acute appendicitis) was not influenced by the z-axis coverage or by the reader (p ranging from 0.126 to 0.808). Of the 106 patients without acute appendicitis, the logistic regression revealed that the probability of correct classification of the final diagnosis (alternative disease or NSAP) was influenced by the z-axis coverage—significantly lower for set S than for set L (OR=0.573, p=0.009)—as well as by the reader; the probability of correct classification being significantly higher for Reader A than for Reader B (OR=1.467, p=0.029). Logistic regressions are summarised in Table 3.
Table 3.
Influence of z-axis coverage and reader on the probability of correct final diagnosis
| Parameters | Odds ratio | p-value | |
| Entire study group (n=152)a | Set S vs set L | 0.61 (0.42, 0.88) | 0.008 |
| Set M vs set L | 0.94 (0.65, 1.38) | 0.771 | |
| Reader A vs Reader B | 1.34 (0.99, 1.81) | 0.057 | |
| Patients with acute appendicitis (n=46) | Set S vs set L | 0.80 (0.31, 2.03) | 0.635 |
| Set M vs set L | 0.89 (0.34, 2.31) | 0.808 | |
| Reader A vs Reader B | 0.54 (0.25, 1.19) | 0.126 | |
| Patients without acute appendicitis (n=106)b | Set S vs set L | 0.57 (0.34, 0.87) | 0.009 |
| Set M vs set L | 0.95 (0.62, 1.47) | 0.824 | |
| Reader A vs Reader B | 1.47 (1.04, 2.07) | 0.029 |
Appendicitis, alternative disease and non-specific abdominal pain (NSAP).
Alternative disease and NSAP. Data in parentheses are 95% confidence intervals.
Alternative diseases that readers considered by consensus as missed for set S owing to the z-axis coverage restriction are summarised in Table 4. Readers agreed that no alternative disease was missed owing to coverage restriction for set M. An example of pyelonephritis visible in set M and not visible in set S is illustrated in Figure 5.
Table 4.
Alternative diseases missed in set S because of reduced z-axis coverage
| Disease | Number |
| Pyelonephritis | 4 |
| Right lower lobe pneumonia | 3 |
| Mesenteric adenitis | 2 |
| Acute cholecystitis | 1 |
| Perforated gastric ulcer | 1 |
| Ileitis and/or colitis | 1 |
| Right ureteral stone | 1 |
| Caecal volvulus and acute cholecystitis | 1 |
| Total | 14 |
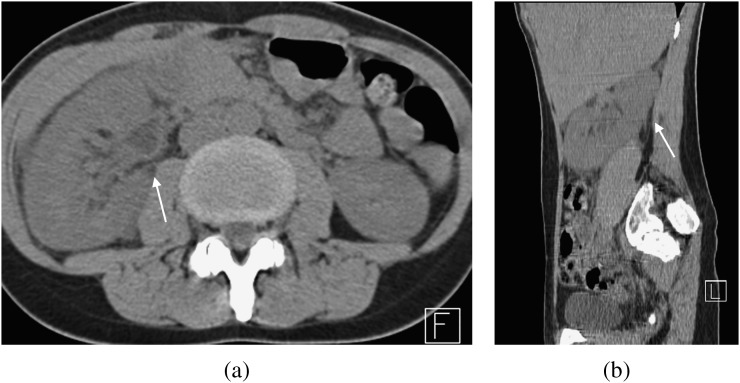
Figure 5.
Unenhanced CT images obtained in a 34-year-old female with definite diagnosis of acute pyelonephritis. Axial (a) and sagittal (b) reformations of a restricted abdominal coverage show an enlarged right kidney (arrow), perinephric fat stranding and minimal dilation of the urinary tract consistent with pyelonephritis. Diagnosis was missed with pelvic focused coverage (set S) by both readers.
Radiation dose
The mean scanned length for set S, set M and set L was of 15.9±1.3, 30.1±2.6 and 40.5±3.9 cm, respectively. The mean DLP was 142.8±0.9, 271.1±1.9 and 364.9±2.8 mGy cm, respectively. The reduction in DLP reached thus was 61% and 26%, respectively, for set S and set M, compared with set L.
DISCUSSION
The results of our study suggest that (1) pelvic focused acquisition is at risk of missing alternative diseases and not visualising the appendix, (2) the appendix visualisation rate is similar to restricted abdominal coverage acquisition and with the entire abdomen and pelvis coverage, (3) reducing the scanned range from the diaphragmatic crus to the upper aspect of the pubis probably does not impair the diagnosis of acute appendicitis nor for alternative diseases and (4) the restricted abdominal coverage is reduced by approximately 25% compared with that of the entire abdomen and pelvis, with subsequent DLP reduction within the same order of magnitude. In addition, our study, involving only experienced readers, confirms their influence in providing the correct diagnosis, particularly that of alternative diseases [16,22,23]. This study is important because it shows that coverage from diaphragmatic crus to pubis, but not focused on pelvis only, can be recommended in adults suspected of appendicitis, no diagnosis being susceptible to be missed owing to z-axis coverage restriction.
Overscanning beyond the region of interest is an important source of unnecessary radiation, which could be reduced by restricting a scan zone to a more focused region [5,7,24,25]. In patients suspected of acute appendicitis (pelvic and even appendiceal), focused CT acquisitions have high diagnostic performance with sensitivity ranging from 83% to 100% [2,9,10,12,13]. However, we showed that the probability of achieving a correct alternative diagnosis is lower when scanning the pelvis only rather than the entire abdomen and pelvis. This confirms the major drawback of focused pelvic acquisition is missing alternative diseases by ignoring the upper abdomen [8,14]. In addition, our study shows that the visualisation of the appendix is less frequent with pelvic focused CT than with other acquisitions. Although the lack of visualisation of the appendix with CT reliably excludes acute appendicitis if secondary inflammatory changes are absent, the visualisation of a normal appendix strengthens the reader’s confidence in a truly normal finding [26,27]. Therefore, the appendix should be included in the scan length. Moreover, even if the rate of appendix visualisation was not statistically significantly different between scan lengths among patients with a definite diagnosis of acute appendicitis, it was not visible on pelvic focused CT in 4% of patients, which is unacceptable in clinical practice. Conversely, our study shows that the visualisation of the appendix is not statistically different between the restricted abdominal coverage and the entire abdomen and pelvis acquisition. But more importantly, we showed that the probability of giving the correct alternative diagnosis was similar between these two scan lengths; all alternative diagnoses—even a lower chest disease—are detectable on the restricted abdominal coverage. With this coverage, acquisition length is reduced by approximately 25% compared with coverage of the entire abdomen and pelvis. Dose reduction would be within the same order of magnitude even with the AEC device switched on—the automatic modulation of tube current being of low amplitude on the upper abdomen on which our coverage is mostly restricted. This restricted abdominal coverage has the additional advantage of protecting breasts and testes from direct radiation. Radiologists should, however, be aware that with helical CT, the planned scan range is substantially extended at both ends owing to the side effect of data interpolation. This extension of scan length, known as overranging, means that any organ positioned just outside the image volume could be fully exposed to radiation [28,29]. We did not take this effect into account because it is affected by many factors, including collimation, pitch, manufacturer and type of scanner. The latest generation of CT scanners are now equipped with overrange dose-reducing innovations, such as dynamic beam collimators, which abolish this effect [28,29]. Having said that, the effect of overranging on testes located several centimetres away from the lower limit of our restricted abdominal coverage is probably negligible. Dose reduction should, however, be considered in young patients only, and elder patients such as those included in our study sample could need a thorough imaging protocol rather than a radiation saving protocol. Nevertheless, as compared with young adults, patients older than 65 years present more frequently a cause of symptoms other than acute appendicitis and are thus an appropriate model for investigating diseases alternative to acute appendicitis [14].
Our study has several limitations. First, patients were primarily enrolled in two previous prospective studies, with an interval of several years. However, the acquisition protocols as well as the CT scanners were identical, and images were read by other radiologists than those in our previous studies. Furthermore, we used at that time a four-row CT scanner, which could be considered as outdated equipment. However, reducing the z-axis is the easiest way to reduce the dose whatever the CT equipment. In addition, our examinations were reconstructed with thin slice thicknesses and intervals, the appendiceal visualisation rate and the reader confidence in its diagnosis being both increased with slice thicknesses lower than 5 mm [30]. Second, the examinations were performed without any oral or IV contrast but several studies have reported high diagnostic performance with unenhanced CT as compared with enhanced CT, even for alternative diseases [16,18–20]. Third, our patient pool was rather small, but even with this group, we detected statistically significant differences between coverages, in particular between pelvic focused coverage and our two other coverages. Fourth, our restricted abdominal coverage was, for the purpose of this study, based on a virtual scout view, and we were therefore unable to evaluate the effect of the variability in inspiratory levels (i.e. lung volumes) between the acquisition of the scout view and that of the CT axial images [5]. Such variability could be avoided by appropriate respiratory instructions and coaching as recommended for thoracic CT examinations [31]. Finally, we calculated dose reduction by multiplying DLP by the percentage of z-axis reduction. DLP reflects the tube output but does not estimate the radiation risk of exposed radiosensitive organs (breasts, lungs, oesophagus, stomach and colon for the upper abdomen and bladder, rectum and ovaries for the lower pelvis). As discussed above, we could not evaluate the effect of AEC, probably of low amplitude on the upper abdomen where our coverage was the most restricted.
In summary, in adults suspected of acute appendicitis, pelvic focused coverage is at risk of not covering the appendix and is insufficient for diagnosing alternative diseases. Conversely, restricted coverage from the diaphragmatic crus to the upper aspect of the pubis could be recommended, in particular in young patients, since it could preserve the performance in diagnosing acute appendicitis as well as alternative diseases with approximately 25% radiation dose reduction.
REFERENCES
- 1.Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology 2000;215:337–48 [DOI] [PubMed] [Google Scholar]
- 2.Wise SW, Labuski MR, Kasales CJ, Blebea JS, Meilstrup JW, Holley GP, et al. Comparative assessment of CT and sonographic techniques for appendiceal imaging. AJR Am J Roentgenol 2001;176:933–41 10.2214/ajr.176.4.1760933 [DOI] [PubMed] [Google Scholar]
- 3.Johnson PT, Horton KM, Mahesh M, Fishman EK. Multidetector computed tomography for suspected appendicitis: multi-institutional survey of 16-MDCT data acquisition protocols and review of pertinent literature. J Comput Assist Tomogr 2006;30:758–64 [DOI] [PubMed] [Google Scholar]
- 4.O'Malley ME, Halpern E, Mueller PR, Gazelle GS. Helical CT protocols for the abdomen and pelvis: a survey. AJR Am J Roentgenol 2000;175:109–13 10.2214/ajr.175.1.1750109 [DOI] [PubMed] [Google Scholar]
- 5.Liao EA, Quint LE, Goodsitt MM, Francis IR, Khalatbari S, Myles JD. Extra Z-axis coverage at CT imaging resulting in excess radiation dose: frequency, degree, and contributory factors. J Comput Assist Tomogr 2011;35:50–6 10.1097/RCT.0b013e3181f5a652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, Steele SR, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg 2008;248:557–63 10.1097/SLA.0b013e318187aeca [DOI] [PubMed] [Google Scholar]
- 7.Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, et al. Strategies for CT radiation dose optimization. Radiology 2004;230:619–28 10.1148/radiol.2303021726 [DOI] [PubMed] [Google Scholar]
- 8.Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Raptopoulos V. Right lower quadrant pain and suspected appendicitis: nonfocused appendiceal CT–review of 100 cases. Radiology 2000;217:159–63 [DOI] [PubMed] [Google Scholar]
- 9.Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology 1997;202:139–44 [DOI] [PubMed] [Google Scholar]
- 10.Wijetunga R, Tan BS, Rouse JC, Bigg-Wither GW, Doust BD. Diagnostic accuracy of focused appendiceal CT in clinically equivocal cases of acute appendicitis. Radiology 2001;221:747–53 [DOI] [PubMed] [Google Scholar]
- 11.Rao PM, Rhea JT, Novelline RA. Sensitivity and specificity of the individual CT signs of appendicitis: experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr 1997;21:686–92 [DOI] [PubMed] [Google Scholar]
- 12.Hershko DD, Awad N, Fischer D, Mahajna A, Guralnik L, Israelit SH, et al. Focused helical CT using rectal contrast material only as the preferred technique for the diagnosis of suspected acute appendicitis: a prospective, randomized, controlled study comparing three different techniques. Dis Colon Rectum 2007;50:1223–9 [DOI] [PubMed] [Google Scholar]
- 13.Jacobs JE, Birnbaum BA, Macari M, Megibow AJ, Israel G, Maki DD, et al. Acute appendicitis: comparison of helical CT diagnosis focused technique with oral contrast material versus nonfocused technique with oral and intravenous contrast material. Radiology 2001;220:683–90 [DOI] [PubMed] [Google Scholar]
- 14.Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology 2012;265:733–42 10.1148/radiol.12120614 [DOI] [PubMed] [Google Scholar]
- 15.Keyzer C, Tack D, De Maertelaer V, Bohy P, Gevenois PA, Van Gansbeke D. Comparison of low-dose and standard-dose unenhanced multidetector row CT in patients with suspected acute appendicitis. Radiology 2004;232:164–72 [DOI] [PubMed] [Google Scholar]
- 16.Keyzer C, Cullus P, Tack D, De Maertelaer V, Bohy P, Gevenois PA. MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol 2009;193:1272–81 10.2214/AJR.08.1959 [DOI] [PubMed] [Google Scholar]
- 17.Menke J. Comparison of different body size parameters for individual dose adaptation in body CT of adults. Radiology 2005;236:565–71 10.1148/radiol.2362041327 [DOI] [PubMed] [Google Scholar]
- 18.Lane MJ, Liu DM, Huynh MD, Jeffrey RB, Jr, Mindelzun RE, Katz DS. Suspected acute appendicitis: nonenhanced helical CT in 300 consecutive patients. Radiology 1999;213:341–6 [DOI] [PubMed] [Google Scholar]
- 19.Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose i.v. contrast-enhanced CT scans. AJR Am J Roentgenol 2009;193:96–105 10.2214/AJR.08.1237 [DOI] [PubMed] [Google Scholar]
- 20.Paulson EK, Coursey CA. CT protocols for acute appendicitis: time for change. AJR Am J Roentgenol 2009;193:1268–71 10.2214/AJR.09.3313 [DOI] [PubMed] [Google Scholar]
- 21.Random.org [homepage on the Internet]. Dublin, Ireland: Randomness and Integrity Services Limited [accessed 25 May 2011] Available from: http://www.random.org/integers/ [Google Scholar]
- 22.Bankier AA, De Maertelaer V, Keyzer C, Gevenois PA. Pulmonary emphysema: subjective visual grading versus objective quantification with macroscopic morphometry and thin-section CT densitometry. Radiology 1999;211:851–8 [DOI] [PubMed] [Google Scholar]
- 23.Lee SY, Coughlin B, Wolfe JM, Polino J, Blank FS, Smithline HA. Prospective comparison of helical CT of the abdomen and pelvis without and with oral contrast in assessing acute abdominal pain in adult emergency department patients. Emerg Radiol 2006;12:150–7 10.1007/s10140-006-0474-z [DOI] [PubMed] [Google Scholar]
- 24.Campbell J, Kalra MK, Rizzo S, Maher MM, Shepard JA. Scanning beyond anatomic limits of the thorax in chest CT: findings, radiation dose, and automatic tube current modulation. AJR Am J Roentgenol 2005;185:1525–30 10.2214/AJR.04.1512 [DOI] [PubMed] [Google Scholar]
- 25.Kalra MK, Maher MM, Toth TL, Kamath RS, Halpern EF, Saini S. Radiation from “extra” images acquired with abdominal and/or pelvic CT: effect of automatic tube current modulation. Radiology 2004;232:409–14 10.1148/radiol.2322031151 [DOI] [PubMed] [Google Scholar]
- 26.Ganguli S, Raptopoulos V, Komlos F, Siewert B, Kruskal JB. Right lower quadrant pain: value of the nonvisualized appendix in patients at multidetector CT. Radiology 2006;241:175–80. 10.1148/radiol.2411050191 [DOI] [PubMed] [Google Scholar]
- 27.Nikolaidis P, Hwang CM, Miller FH, Papanicolaou N. The nonvisualized appendix: incidence of acute appendicitis when secondary inflammatory changes are absent. AJR Am J Roentgenol 2004;183:889–92 10.2214/ajr.183.4.1830889 [DOI] [PubMed] [Google Scholar]
- 28.Schilham A, van der Molen AJ, Prokop M, de Jong HW. Overranging at multisection CT: an underestimated source of excess radiation exposure. Radiographics 2010;30:1057–67 10.1148/rg.304095167 [DOI] [PubMed] [Google Scholar]
- 29.van der Molen AJ, Geleijns J. Overranging in multisection CT: quantification and relative contribution to dose–comparison of four 16-section CT scanners. Radiology 2007;242:208–16 10.1148/radiol.2421051350 [DOI] [PubMed] [Google Scholar]
- 30.Johnson PT, Horton KM, Kawamoto S, Eng J, Bean MJ, Shan SJ, et al. MDCT for suspected appendicitis: effect of reconstruction section thickness on diagnostic accuracy, rate of appendiceal visualization, and reader confidence using axial images. AJR Am J Roentgenol 2009;192:893–901 [DOI] [PubMed] [Google Scholar]
- 31.Bankier AA, O'Donnell CR, Boiselle PM. Quality initiatives. Respiratory instructions for CT examinations of the lungs: a hands-on guide. Radiographics 2008;28:919–31 10.1148/rg.284085035 [DOI] [PubMed] [Google Scholar]