Abstract
Traditional outcome measures such as long-term mortality may be of less value than symptomatic improvement in elderly patients undergoing coronary artery bypass grafting (CABG). In this systematic review, we analyse health-related quality of life (HRQOL) as a marker of outcome after CABG. We aimed to assess the role of HRQOL tools in making recommendations for elderly patients undergoing surgery, where symptomatic and quality-of-life improvement may often be the key indications for intervention. Twenty-three studies, encompassing 4793 patients were included. Overall, elderly patients underwent CABG at reasonably low risk. Our findings, therefore, support the conclusion that performing CABG in the elderly may be associated with significant improvements in HRQOL. In order to overcome previous methodological limitations, future work must clearly define and stringently follow-up this elderly population, to develop a more robust, sensitive and specialty-specific HRQOL tool.
Keywords: Coronary artery bypass grafting, Health-related quality of life, Elderly
INTRODUCTION
Ischaemic heart disease is one of the major causes of death, disability and health care resource utilization worldwide. As the population ages, an increasing number of elderly patients are undergoing surgical revascularization [1]. Elderly patients pose a significant challenge as they have a greater incidence of comorbidities impacting adversely on outcomes and thus experience higher morbidity and mortality. Coupled with the unprecedented rise in the number of elderly patients presenting as potential surgical candidates, recent advances in operative techniques and perioperative care have resulted in an increasing number of elderly patients undergoing coronary artery bypass grafting (CABG) procedures [2, 3].
CABG is very effective at relieving angina and improving survival, which are the primary indications for the operation. Traditional outcome measures assessing the quality of CABG have been morbidity and mortality. However, with improvements in perioperative care, cardiopulmonary bypass and surgical techniques, the overall mortality associated with CABG has declined despite an increasingly elderly and sicker patient cohort. Furthermore, in an ever-aging elderly population in whom surgical intervention is more often of symptomatic rather than prognostic benefit, long-term mortality has limited use as an outcome measure.
Over recent years, there has been an increasing interest in assessing health-related quality of life (HRQOL), defined as a multi-dimensional assessment of an individual's perception of the physical, psychological and social aspects of life that can be affected by a disease process and its treatment. This increasing focus on the patient's perspective has led to the development of Patient Reported Outcomes Measures (PROMS), outcomes that provide a validated evidence of health from the patient's perspective [4]. The use of PROMs can greatly enhance the assessment of quality of care, particularly HRQOL, and have great potential to transform healthcare [5]. At present, there are three broad categories of PROMs instruments: (i) generic health status, (2) condition- or population-specific and, (iii) preference-based measures. Generic health status measures (e.g. Short form [SF]-36, RAND SF-36, SF-20) aim to give a fully comprehensive assessment of HRQOL thus providing a common scoring system that may be used to compare different patient cohorts, conditions and subsequent treatments. In contrast, condition-specific measures (e.g. Seattle Angina Questionnaire [SAQ], Dukes Activity Status Index [DASI] and Rose Angina Questionnaire [RAS]) provide a precise score of health status for a given condition, rendering them more sensitive to smaller changes in HRQOL that may not be reflected in a general measures assessment [6]. Preference-based measures differ in that they provide an assessment of the effectiveness of a treatment or intervention to prevent disease based on HRQOL. The outcomes of such scoring systems are often utilized in evaluating the cost-effectiveness or cost-benefit of a given treatment or procedure. Examples of such tools include the 15D-Measure of Health-related Quality of Life and EuroQOL-5D scoring systems [7].
As a consequence of the increasing elderly population undergoing cardiac surgery, data are needed to adequately counsel patients so that their expectations are aligned with their likely outcome, particularly in terms of improvements in quality of life. In the elderly population, the assessment of quality of life after cardiac surgery has been recently appropriately described as ‘under researched research’ [8], with greater focus on mortality as a marker of surgical outcome. However, in this population where symptomatic rather than long-term prognostic improvement is more pertinent in defining operative success, HQOL may be a more important indicator of clinical outcome.
The aims of this study were to systematically review the published literature relating to HRQOL outcomes for elderly patients who have undergone CABG. First, we assess the quality of studies within the literature, highlight the different tools used in assessing HRQOL and identify predictors of poor HRQOL. Secondly, we perform comparative therapies assessment in terms of HRQOL in the elderly and demonstrate findings that confirm the potential benefits of CABG in elderly patients. Finally, we uncover the limitations of the current literature and formulate recommendations for much-needed future work in this area.
MATERIALS AND METHODS
Literature search
This study was performed in accordance with guidelines for the ‘Preferred Reporting Items for Systematic reviews and Meta-Analyses’ (PRISMA) [9].
A systematic search was carried out using MEDLINE (1950 to date), EMBASE (1980 to date) and PsycINFO (1966 to date) databases using the following MESH terms: [coronary artery bypass grafting OR cardiac surgery] AND [health related quality of life] OR [quality of life] AND [elderly] OR [aged]. The search period was 6 months with the last search date being 31 March 2012.
Eligibility criteria
Articles relating to HRQOL outcomes in elderly patients (i.e. aged ≥70) who had undergone CABG were included.
One of the greatest challenges is the lack of consensus as to the definition of elderly. There is no consistent and universally accepted age cut-off for defining the elderly. The WHO/UN have traditionally defined elderly as 60 years and over [10], and many developed countries have taken the age of retirement at 65 to define the elderly population. In the literature, its definition has been changing with time. However, most of the literature relating to CABG over the past two decades has defined elderly as those aged 70 years or older. It is interesting to note that the latest American Heart Association/American College of Cardiology guidelines now define elderly as 80 years of age [11].
All studies where full text was available in the English language were included in this review.
Studies were excluded when they reported: (a) patient groups with a mean age of ≥70 but included patients aged <70 years of age; (b) HRQOL outcomes in patients undergoing CABG and concomitant valve or other surgery.
Study selection and data collection process
Two reviewers (J.P. and L.H.) independently identified potentially relevant articles. The full text of the article was obtained and further screened for inclusion if it addressed HRQOL outcomes in elderly patients after CABG. Conflicts between reviewers were subsequently discussed until 100% agreement was achieved on the final studies to be included in the review. The inter-rater agreement reliability was calculated by consensus estimate to be 90%.
The following information was extracted from each study: First author, year of publication, research type, study population, HRQOL instrument used, timings of the follow-up, number of patients included in the study, completeness of follow-up, overall conclusions and quality of the study (Tables 1–4).
Table 1:
Generic HRQOL instruments
| Author | Study type | Patient population | Number of patients | Preoperative HRQOL assessment | Duration or follow-up | Instruments | Follow-up completion | Conclusion | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Barnett [13] | Cohort retrospective | Regional medical centre Northern Virginia, Washington DC | 383 | Yes | 1 year, annually thereafter | Medical Outcome Trust SF-20 | 26% at 1 year 18% at 2 years |
Findings suggested that elderly patients can expect postsurgical function to increase steadily during the first 2 years after surgery | 9 |
| Kallis [27] | Cohort retrospective | Cardiothoracic Unit, St George's Hospital, London | 137 | No | Mean f/u time 36 months | University of York Questionnaire | 95% | Cardiac surgery can be carried out in elderly patients with an acceptable early morbidity and mortality. Two-thirds of patients demonstrated a sustained improvement in their quality of life | 9 |
| Kurlansky [28] | Cohort retrospective | Miami Heart Research Institute, Mount Sinai Medical Center | 987 | No | Mean f/u 3.45 years | SF-36 | 98.1% | Arterial grafting confers an enhanced quality of life in the elderly | 9 |
| Murphy [30] | Cohort retrospective | Jewish Hospital, Washington University Medical Centre | 106 | No | Mean f/u time 22 months | Functional status questionnaire (FSQ) | 61% | CABG can be performed in the elderly population with a good functional outcome and improved quality of life | 8 |
Table 2:
Preference-based HRQOL instruments
| Author | Study type | Patient population | Number of patients | Preoperative HRQOL assessment | Duration or follow-up | Instruments | Follow-up completion | Conclusion | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Loponen [14] | Cohort prospective | Thoracic and Cardiovascular Department, Vaasa Central Hospital, Finland | 56 | Yes | 6 and 18 months | 15-D | 96.3% | In patients aged ≥75, the initial improvement in HRQOL returned to the preoperative levels 18 months after surgery. Expectations of improved HRQOL may have limited value in decision making for surgery for patients aged ≥75 | 9 |
| Markou [15] | Cohort retrospective | Radboud University Hospital, Netherlands | 73 | Yes | 1 year | EuroQOL | 76.3% | Elderly patients have the same improvement in their symptomatic status as younger patients. However, despite this improvement they have less benefit from CABG regarding their quality of life and physical activity | 10 |
| Sollano [31] | Cohort retrospective | Surgical cohort identified by the database maintained for the New York State Cardiac Surgery Reporting Systems | 176 | No | 3 years | EuroQOL | 64% | Performing CABG surgery in octogenarians is highly cost-effective. The QOL of the elderly who elect to undergo CABG surgery is greater than that of their cohorts and equal to that of an average 55-year old person in the general population | 8 |
| Markou [16] | Cohort prospective | Radboud University Hospital, Netherlands | 102 | Yes | 1 year | EuroQOL | – | In elderly patients undergoing CABG, the HRQOL strongly improved, particularly in respect of the mobility, pain and discomfort and anxiety domains of the EQ-5D | 10 |
Table 3:
Condition-specific HRQOL instruments
| Author | Study type | Patient population | Number of patients | Preoperative HRQOL assessment | Duration or follow-up | Instruments | Follow-up completion | Conclusion | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Conaway [17] | Cohort prospective | Mid America Heart Institute—Tertiary Centre | 138 | Yes | 1 year | SAQ | 73% | Despite slower rates of physical recovery, older patients derived similar health status benefits from CABG compared with younger patients | 9 |
| Glower [18] | Cohort retrospective | Duke University Medical Center, Durham, NC | 86 | Yes | Mean f/u duration 17 ± 17 months | Karnofsky | 88% | CABG can be offered to selected elderly patients with acceptable morbidity, mortality, marked improvement in performance status and an acceptable quality of life | 9 |
| Graham [32] | Cohort retrospective | Patient cohort selected from the Alberta provincial project for outcomes assessment in coronary heart disease (APPROACH) | 901 | No | 1 and 3 years | SAQ | 77.4% | Elderly patients undergoing revascularization have better health status at four years than those in the same age group that do not. Patients over the age of 80 who underwent CABG, had higher score than those undergoing PCI in the majority of dimensions | 8 |
| Hedeshian [19] | Cohort retrospective | Beth Israel Deaconess Medical Centre | 119 | Yes | 6 months | DASI | 86% | Functional outcomes demonstrated that older patients present for CABG at a significantly lower functional level and remain at a significantly lower functional level 6 months after CABG. However, functional improvement after CABG is not significantly different across age groups | 10 |
| Huber [20] | Cohort retrospective | Division of Cardiovascular Surgery University Hospital of Lausanne and Bern | 61 | Yes | Mean f/u length 29.6 months | Modified SAQ | 100% | A remarkable quality of life and improvement in the functional status in patients aged over 80 paired with a satisfactory medium-term survival justify early surgical intervention | 9 |
| Kamiya [33] | Cohort retrospective | Department of Surgery, Nippon Medical School, Tokyo, Japan | 28 | No | 1 and 4 years | Modified SAQ | 98.2% | The quality of life and longevity of octogenarians following extensive surgical revascularization for ischaemic coronary artery disease were satisfactory | 9 |
| Luqman [34] | Cohort prospective | Aga Khan University Hospital, Karachi, Pakistan | 31 | No | Mean f/u time 21.1 ± 6.6 months | Modified SAQ | 82% | Patients reported remarkable improvement in QOL. 90% were not or slightly disabled in their daily activity. Satisfaction with their current QOL was reported by 95% of patients | 9 |
| Wilson [21] | Cohort retrospective | Millard Fillmore Hospital, Buffalo New York | 69 | Yes | Specific timings Not specified | Karnofsky | 94.5% | Karnofsky performance status scores improved postoperatively | 7 |
Table 4:
Multiple HRQOL instruments
| Author | Study type | Patient population | Number of patients | Duration or follow-up | Preoperative HRQOL assessment | Instruments | Follow-up completion | Conclusion | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Fruitman [35] | Cohort retrospective | Queen Elizabeth II Health Centre in Halifax, Nova Scotia | 78 | Mean f/u time 15.7 ± 6.9 months | No | RAND SF-36 SAQ | 96.1% | Octogenarians can undergo cardiac surgical procedures at a reasonable risk and show remarkable improvement in their symptoms | 9 |
| Jarvinen [22] | Cohort prospective | Tampere University Hospital, Finland | 44 | 1 year | Yes | RAND-36 Karnofsky | 94.7% | Elderly patients not only have higher mortality and morbidity but derive less benefit from CABG regarding certain aspects of QOL | 10 |
| Kaiser [24] | Prospective randomized multicentre | Multicentre Swiss trial (TIME study) | 59 | 6 months and 1 year | Yes | SF-36 DASI Rose Angina Questionnaire | Not stated | QOL parameters were significantly less improved in patients with chronic angina by medical therapy vs CABG surgery | 9 |
| MacDonald [23] | Cohort prospective | Victoria General Hospital, Halifax, Nova Scotia | 100 | 3 months | Yes | RAND-36 SAQ | 75% | On average, important improvements in QOL were observed at 3 months follow-up, using both RAND 36 and SAQ | 9 |
| Artinian [29] | Cohort retrospective | Five Teaching Hospital Cardiothoracic Units, Detroit MI | 39 | 1, 3 and 6 weeks | No | Sickness Impact Profile 20-Item Symptom Inventory Beck Depression Inventory | 71% | There were no significant differences between age cohorts for any of the physical, psychological or social recovery measures. Patients over 70 years of age had recovery patterns similar to those of younger age groups | 8 |
| Jensen [25] | Prospective randomized controlled trial | Copenhagen University Hospital, Denmark | 120 | 3 months | Yes | SF-36 Major Depression Inventory | 96.5% | Both on-pump and off-pump CABG improved SF-36 scores. Depression scores remained unchanged | 9 |
| Houlind [26] | Prospective randomized controlled trial | Four centres in Denmark: DOORS | 900 | 6 months | Yes | SF-35 EuroQOL | 93% | Both on-pump and off-pump patients showed significant improvements in SF-36 and Euro-QOL scores from baseline. There was no significant difference between groups | 10 |
Quality scoring
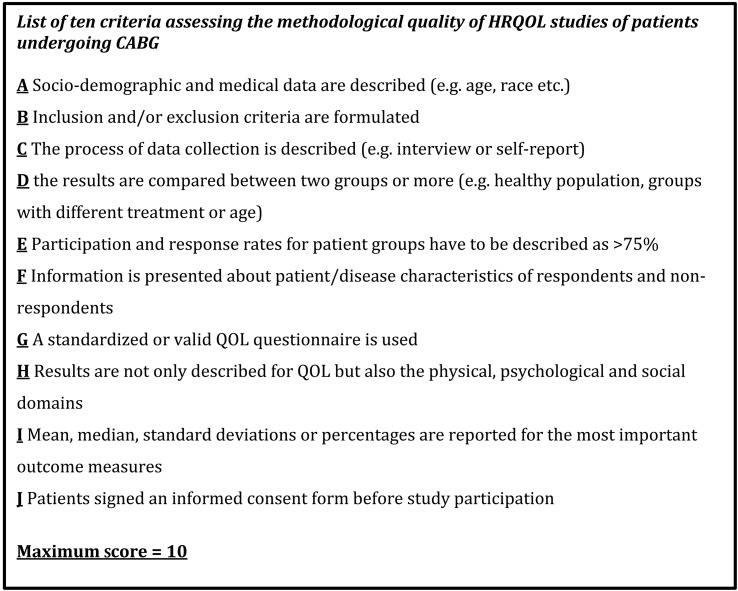
The quality of eligible studies was assessed using the criteria for assessing the methodological quality of studies in HRQOL, adapted from that previously described by Mols et al. [12] (Fig. 1). Briefly, in this modified scoring system, one point is assigned for each of a standardized checklist of 10 pre-defined criteria. Where a criterion is described inadequately or not at all, a score of zero is given, allowing the overall score to range from 0 to 10. Those studies scoring >8 were considered ‘high-quality’, a score between 5 and 8 was considered ‘moderate quality’ and <5 ‘poor quality’.
Figure 1:
Scoring criteria for quality of eligible papers: adapted from Mols et al. [4].
RESULTS
Study selection
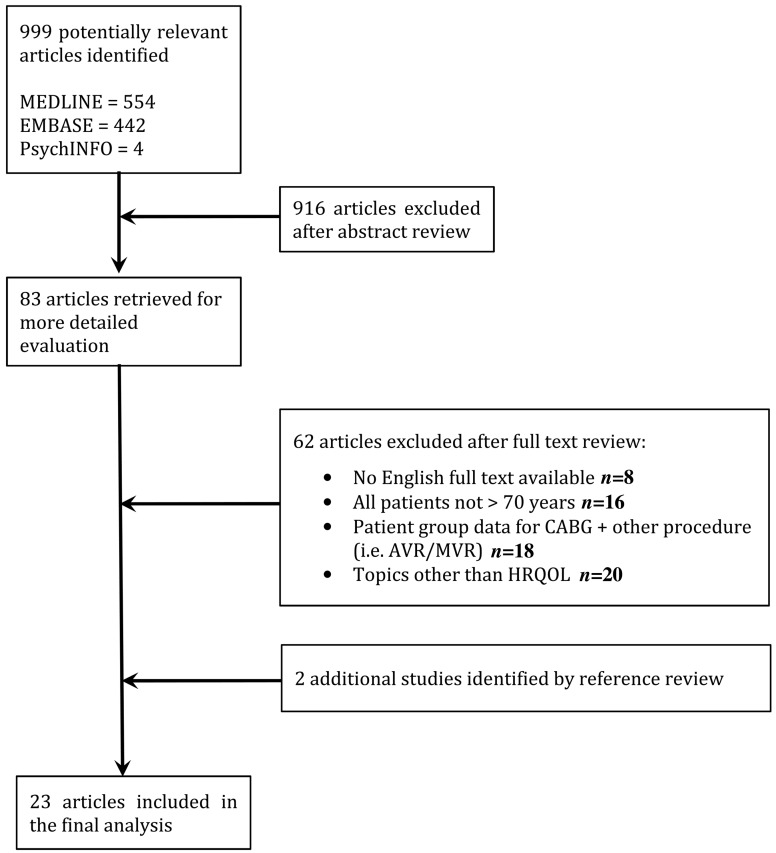
Our search identified 999 potentially relevant publications that underwent abstract review by two independent reviewers (K.B., L.H.). Nine hundred and sixteen studies were excluded following abstract review, as they did not primarily address the HRQOL outcomes in elderly patients after CABG surgery. Of the remaining 83 studies, a further 62 were excluded after a review of the full text. The reference sections of the remaining 21 studies were reviewed in an attempt to identify any further relevant studies. This identified a further two articles that fulfilled our inclusion criteria. Finally, 23 studies were included in the systematic review (Fig. 2).
Figure 2:
Flow diagram representing phases of article selection for systematic review.
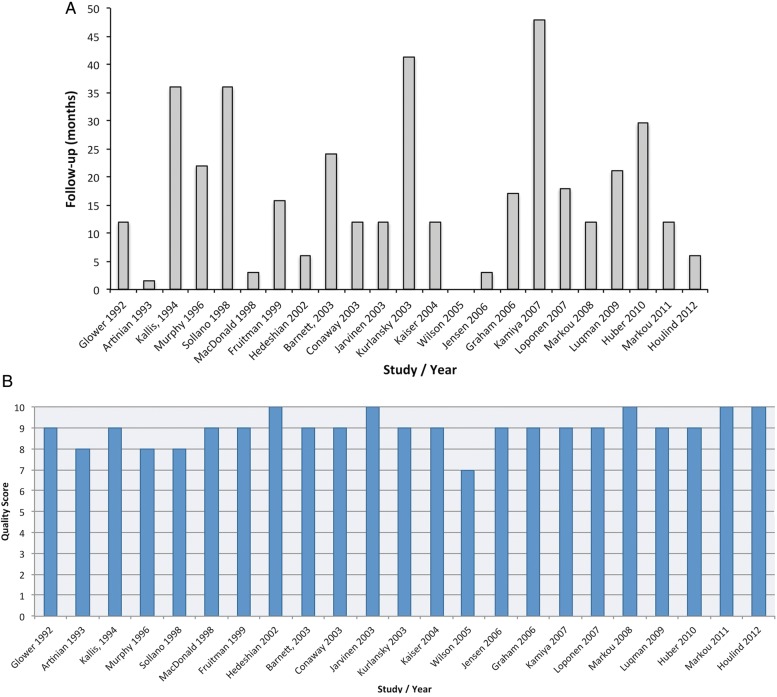
Quality of included studies
The included studies varied in quality according to the criteria used in Fig. 1 [12]. The scores of the eligible studies ranged between 0 and 10 out of a maximum of 10 (Tables 1–4, Fig. 3B). Twenty-two of the eligible studies were allocated a score of ≥8.
Figure 3:
(A) The duration of the follow-up, (B) quality score vs publication.
Study design and population
Our search identified 23 studies incorporating 4793 patients ranging from 70 to 93 years of age that assessed HRQOL outcomes in elderly patients after CABG. Study sizes varied from 28 to 987 patients. Twenty were cohort studies, and three were randomized controlled trials. Fourteen studies were carried out retrospectively and nine prospectively. Thirteen studies were conducted in the USA and North America, and the remaining in European centres. All studies were carried out at tertiary referral centres/university hospitals.
Fourteen studies assessed HRQOL both pre- and postoperatively [13–26]. None of the included studies compared findings with age-matched controls. The weighted mean age of patients included in this analysis was 80.7 ± 4.9 years.
HRQOL measures
A total of 11 different instruments were used in the 23 studies.
Generic measures were used in seven of the studies (SF-36, RAND SF-36, SF-20, York SF-12, Functional Status Questionnaire and Sickness Impact Profile) [13, 27–30].
Preference-based measures were used in four studies [14–16, 31] (15D-Measure of Health-related Quality of Life and EuroQOL-5D).
Condition-specific measures were used in 10 of the studies [17–21, 32–34] (SAQ, DASI and Rose Angina Questionnaire).
Of the 23 studies included, two used one questionnaire to assess HRQOL outcomes [13–21, 27, 30–34]. Two HRQOL questionnaires were used by six of the studies [22, 23, 25, 26, 29, 35]. One study used three HRQOL questionnaires [24].
Timings of HRQOL assessments
Fourteen of the eligible studies carried out baseline HRQOL assessments either preoperatively or during the perioperative period [13–26]. Timings of postoperative HRQOL assessments in the eligible studies varied form 6 weeks to 4 years (see Fig. 3A). Five studies performed assessments within the first 6 months [19, 23, 25, 26, 29]. Five studies performed their final postoperative assessment at 1 year, five studies between 1 and 2 years, [15–17, 22, 24] and four studies between 2 and 3 years [20, 27, 31, 32]. Two studies performed final assessments >3 years after the initial operation [28, 33]. One study did not specifically state the time of postoperative HRQOL assessment [21].
Follow-up
Patient follow-up varied between 18 and 100% within the eligible studies. Seventeen of the studies reported the follow-up of ≥75% [14–28, 32–35]. Six studies reported the follow-up of <75% [13, 17, 18, 29–31]. Information regarding patients lost to the follow-up was reported by all 23 studies. The 17 studies reporting completion of the follow-up of >75% included a total of 3892 patients. Of these, 3330 patients completed the follow-up. The weighted mean follow-up achieved by these 3330 patients was 20.95 months. The six studies reporting completion of the follow-up of <75% corresponded to a total of 928 patients. Of these 928 patients, 438 completed the follow-up. The weighted mean follow-up achieved by these 438 patients was 20.87 months.
DISCUSSION
Our systematic review has analysed 23 studies investigating HRQOL in elderly patients (age 70–93) undergoing CABG, spanning a period of two decades. These studies confirm the potential benefits of CABG in elderly patients, with the majority of studies showing that elderly patients can undergo CABG procedures at a reasonably low risk resulting in significant symptomatic and overall quality of life improvement.
We highlight the importance of considering the elderly populace as being distinct from younger cohorts, since elderly patients often do not derive the same degree of benefit in QOL as younger patients. Furthermore, in some cases such improvements have been very limited and not sustained [14, 15, 19, 22].
Impact of different techniques: off-pump vs on pump CABG
There were two studies, both Randomised controlled trials (RCTs), that investigated the effects of off-pump vs on-pump techniques for CABG on HRQOL outcomes [25, 26]. Both studies demonstrated significant improvements in HRQOL in both surgical technique groups, with no significant difference between off-pump and on-pump strategies. The follow-up period in both studies was very short, at 3 and 6 months, respectively. Further follow-up and analyses in the Danish On-pump vs Off-pump Randomization Study (DOORS) are awaited and should provide more useful insight into long-term outcomes [26].
QOL assessment tools
One of the challenges in comparing studies assessing HRQOL is the use of multiple instruments. The most commonly used HRQOL assessment tools in our analysis were the EQ-5D/EuroQOL (preference based), SAQ (condition specific) and SF-36 (generic).
A recent report was commissioned by the UK Department of Health to identify Patient Reported Outcome Measures (PROMs) that have been evaluated for patients undergoing coronary revascularization [36]. The report concluded that the EQ-5D/EuroQOL, SF-36 and SAQ HRQOL measures possessed the strongest evidence for use with patients undergoing elective CABG. This report also recommended that the Coronary Revascularisation Outcomes Questionnaire (CROQ) merited further investigation. The CROQ is a recently tool developed in the UK and has significant promise since it includes both psychological and cognitive functioning as well as unique surgery-specific items. The CROQ is intended to compare quality of life and outcomes in patients undergoing CABG and percutaneous coronary angioplasty. This tool has been evaluated in five studies investigating the outcomes of CABG and has shown responsiveness and acceptability comparable with the longstanding generic instruments SAQ and SF-36 [37]. When taking these recommendations into account, the predominant use of these three HRQOL tools by the studies within this systematic review adds strength to its findings and provides a concordance with this report.
HQOL assessment of CABG vs PCI vs medical therapy
We identified 3 studies providing a comparative therapies HRQOL assessment between medical therapy and revascularization (Percutaneous coronary intervention [PCI] or CABG). Of these, the Trial of Invasive vs Medical Treatment in Elderly patients with Chronic Angina (TIME) was the first prospective randomized treatment trial in elderly patients with chronic symptomatic coronary artery disease [38]. A subsequent on-treatment analysis of the TIME trial demonstrated that revascularized elderly patients exhibited a greater relief from angina and more significant improvements in HRQOL measures than with optimized medical therapy (OMT) [24]. Furthermore, patients undergoing CABG experienced greater symptomatic relief and reported improved quality of life at 1 year in comparison to those treated with PCI.
Graham et al. [32] showed that patients (aged 70–79) treated with PCI or CABG tended to have better crude SAQ scores than those treated medically. In patients >80 years, CABG scored significantly better than PCI, with exception of exertional capacity. This study importantly demonstrated that the benefits of surgical revascularization extend to long-term enhancement (3 years) of quality of life. Conversely, however, Kamiya et al. [33] demonstrated comparable favourable HRQOL (SAQ) scores in physical and mental satisfaction domains, across the three treatment strategies.
Valuable insights into the effects of surgical revascularization on HRQOL can be obtained from large-scale RCTs of PCI vs CABG, in the non-elderly population. In the Stent or Surgery Trial, Zhang et al. [39] reported that although CABG and stent-assisted PCI dramatically improved cardiac-related health status in patients with multivessel disease at the 6- and 12-month follow-up, CABG was more effective in relieving angina, increasing physical functioning and improving quality of life during the first year after revascularization. Similarly, the SYNTAX quality of life sub-study (n = 903 PCI; 897 CABG) has shown both PCI and CABG to be associated with significant improvements in disease-specific and general health status when assessed using SAQ (disease specific), SF-36 and EQ-5D (general health status) questionnaires. CABG was also associated with a slightly greater improvement in SAQ score on the angina frequency subscale at 6 and 12 months when compared with PCI. This small but significant effect was, however, counterbalanced by improved short-term (1 month) outcomes seen in the PCI group [40].
Predicting poor quality of life
Despite the majority of studies demonstrating overall improvement in HRQOL outcomes in elderly patients undergoing CABG, a proportion of patients may not achieve such benefits and in fact may have poor outcomes. Surprisingly, only one of the studies in our review sought to analyse the predictors of postoperative quality of life. Using multivariate regression analysis, Wilson et al. [21] revealed that in octogenarians (n = 73), preoperative functional classification (New York Heart Association) and chronic renal failure were sensitive predictors of impaired quality of life after CABG. Furthermore, they also underlined the importance of family support in improving quality of life in the elderly. It is, therefore, paramount that the patient's comorbid conditions and social situation be equally considered in the decision-making process regarding therapeutic strategy for coronary artery disease.
Non-cardiac variables also appear to have a significant influence on HRQOL outcomes following CABG and potential strategies to improve HRQOL following cardiac surgery may target non-cardiac contributors. Although studies on non-cardiac contributors to HRQOL are limited in elderly patients, data taken from a younger population identify several factors such as female sex, diabetes, peripheral vascular disease, >2 days intensive care unit stay and chronic obstructive pulmonary disease to be independent predictors of low HRQOL after CABG [41]. Such findings are likely to be translatable since many of these patients will have significant coexisting comorbidities, including respiratory, musculoskeletal and cerebrovascular disease, which may impact their postoperative functional status.
Cost-effectiveness
One of the greatest challenges facing global health-care systems is the rapidly escalating cost of an increasingly aging population countered by limitation of resources and increasing drives for cost-effective treatments. The few analyses of cost-effectiveness comparing CABG surgery with medical therapy have shown that CABG is most economically attractive when applied to high-risk patients and those with severe symptoms [42–44].
Only one study in our series addressed cost-effectiveness of CABG in the elderly and correlated this with quality of life. Sollano et al. [31] demonstrated that performing CABG in octogenarians was highly cost-effective and patients who underwent CABG enjoyed a better quality of life up to 3 years after surgery, compared with age-matched control subjects.
A cost-effectiveness analysis was also performed on a subgroup of the TIME study, demonstrating invasive strategy (PCI and CABG) to be cost-effective over a 1-year observation period relative to OMT as the early increased costs of revascularization were balanced by increased private practitioner's charges and symptom-driven late revascularizations [45].
Frailty and HRQOL
Recently, there has been increasing interest in assessing the frailty of elderly patients. Frailty is an emerging concept that has no universally agreed definition, but can be considered as a biological state or syndrome of decreased resistance to environmental stressors resulting from a deterioration in multiple physiological systems [46]. Lee et al. [47] have demonstrated frailty to be a risk for postoperative complications and an independent predictor of in-hospital mortality, institutional discharge and reduced mid-term survival. They proposed that frailty screening improves risk assessment in cardiac surgery patients and may identify a subgroup of patients who may benefit from innovative processes of care. Singh et al. [48] showed that in patients >65 year after PCI, frailty, comorbidity and poor quality of life (as assessed by SF-36) are prevalent and are associated with adverse long-term outcomes. This is the only study to date that has utilized frailty and HRQOL assessments for risk stratification in elderly patients undergoing coronary revascularization and it provides strong evidence for including such geriatric assessments for improving risk stratification in this increasingly important patient population [49].
Difficulties with HRQOL assessment
The study of HRQOL as a primary outcome measure has continued to increase, resulting in a proliferation of instruments. However, interpreting HRQOL studies is a complicated task, characterized by the lack of a gold standard measure of HRQOL. Many studies are limited by inadequate reporting which significantly restricts the quality of the data and subsequent conclusions drawn.
To date, two authors in particular have attempted to overcome some of these challenges. In 2008, Koch et al. [50] published their comprehensive review of the difficulties in analysing QOL after cardiac surgery giving an overview of emerging analytical techniques. Despite this, in their 2011 synopsis of 29 studies assessing QOL after cardiac surgery, Noyez et al. [8] found several ongoing serious methodological weaknesses relating to differing study design, lack of preoperative quality of life assessment, the variability in definition and length of the follow-up. Consequently, they proposed five minimal requirements to increase the validity of postoperative quality of life studies (Table 5). Other groups such as Gill and Feinstein [51] have also developed criteria for assessment of quality of life studies and more recently, Mols et al. [12] devised their checklist, which was adopted in this review to assess study quality. Overall however, there is still an ongoing requirement for more conceptual and methodological rigour to be adopted in future quality-of-life studies.
Table 5:
Requirements to increase the validity of postoperative quality of life studies as taken from Noyez et al. [30]
| Criterion | Explanation |
|---|---|
| 1 | Clearly define the number of patients included in the study, the precise surgical intervention (e.g. CABG only vs CABG + valve) and explicitly state inclusion and exclusion criteria |
| 2 | Clear description of the number of patients with: (i) pre- and postoperative QOL information and (ii) the number of patients with complete QOL information |
| 3 | State whether the study has been performed only on patients with complete data and whether imputation methods have been used to handle the missing data |
| 4 | State the reason for missing preoperative QOL data and a comparison of demographics, comorbidity, cardiac data and risk stratification of the groups with and without preoperative QOL data |
| 5 | State the reason for missing postoperative data as described in 4 |
Study limitations
As with all systematic reviews, it is possible that this review is subject to a degree of publication bias inherent in the included studies. Overall, the small number of studies (n = 23) shown here almost all indicate a beneficial effect of CABG on HRQOL in the elderly. It is, therefore, possible that there is a tendency not to report negative effects on HRQOL after surgery, particularly given the predominantly non-randomized study design.
The definition of elderly is taken within this study to be patients age ≥70 years. However, there is a lack of universal definition of ‘elderly’ within the literature. In light of improvements in primary prevention and non-surgical management of cardiovascular disease, historical definitions taken by the WHO/UN of 60 years of age, or the retirement age of 65, no longer reflect the population of ‘elderly patients’ undergoing cardiac surgery in most centres. We have, therefore, taken the definition of ≥70 years to reflect the recent trend in reporting of the elderly population over the past decade; however, we recognize that this remains variable throughout the literature.
In this study, we chose to focus specifically upon only elderly patients who underwent isolated CABG and not include elderly patients who underwent combined CABG + valve procedures. The principal reason was that there are different pathological/disease processes involved in isolated CABG and CABG + valve patients and hence it would complicate the analysis of subsequent benefits in terms of HRQOL. We appreciate that this may have resulted in a loss of inclusion of some studies in our analysis but we preferred to maintain focus upon the effects of revascularization alone upon HRQOL in the elderly.
Within this review, 12 studies were carried out retrospectively, giving rise to potential selection bias. Eight of the included studies did not assess preoperative QOL status. Furthermore, studies undertaking single assessments of HRQOL only provide a ‘snap-shot’ of HRQOL at a specific point in time and do not detect changes over time or the consequences of new health concerns. Multiple assessments of HRQOL over time would be more likely to provide generalizable information on the impact of key variables. Another significant limitation of the cross-sectional manner by which QOL data were collected is that patients who have done badly and subsequently died may have been removed from the study sample, with no data on the patients' quality of life prior to death. In this way, death may act as a competing variable resulting in a bias towards better outcomes.
A further limitation is the small sample size of 10 of the included studies (≤100 patients), decreasing the ability to detect factors influencing HRQOL outcomes. The follow-up range varied from 26 to 100% and many studies only included data of patients who were still alive at time of the follow-up. This may be an important limitation as patients who did not survive may have had lower quality of life. Furthermore, the potential impact of lack of data from non-responders should be noted. These patients may in fact have excellent QOL; however, previous research suggests that non-responders may in fact be more ill and less willing to complete questionnaires [52, 53].
The issues of missing data due to non-compliance, patient dropout or death have been discussed in further detail by Koch et al. [50]. If the non-response is due to death, the final analysis may be biased towards better outcomes by the dropout of individuals having the poorest physical function. Statistical strategies for dealing with missing data have been developed, from simplistic techniques of non-informative imputation to more complex missing data models and multiple imputations. These tools for dealing with missing data are complicated and often require sensitivity analyses to compare the appropriateness of adopting a particular strategy. Grady et al. [54] have adopted such longitudinal modelling and multivariate analyses in reporting HRQOL after cardiac operations.
In addition to incomplete follow-up, there is currently no established optimal duration for quality of life assessment and no studies report long-term (i.e. 5-year) outcomes in the elderly population. The follow-up period of studies included in this review varied from 6 weeks to 4 years and is limited to 1 year if we consider only RCTs [24–26]. Furthermore, although Houlind et al. [26] have performed the largest study to date (n = 900), this too is limited by only the 6-month follow-up. This is important to note as the evaluation of HRQOL within the first 6 months after surgery may not produce accurate results. First, slower rehabilitation in elderly patients may adversely affect HRQOL outcomes in this period. Secondly, early beneficial effects on HRQOL seen during this limited period of observation cannot be assumed to be representative of long-term quality of life improvements. Further research is, therefore, required to determine true quality-of-life outcomes after 5 years [14]. There is also evidence that HRQOL can vary over the time of the follow-up. Yun et al. [55] demonstrated that in patients >65, physical function components of HRQOL improved following cardiac operations (majority of which were isolated CABG), peaking at 12 months, but showed small but significant decline thereafter, suggesting effects of the aging process itself or underlying disease.
CONCLUSIONS
This study demonstrates that performing CABG in the elderly is associated with significant improvements in HRQOL. The data presented here support the use of a combination of HRQOL tools to achieve a comprehensive QOL assessment in elderly patients, namely the generic SF-36, preference-based measures EQ-5D and condition-specific SAQ. There is, however, a need to develop more robust and sensitive HRQOL tools specifically for cardiac surgery, and the CROQ offers significant promise and warrants further validation. The findings presented here highlight the importance of performing frailty assessment and assessing HRQOL outcomes in the elderly population undergoing CABG. Furthermore, such tools should play an important role in surgical decision-making, comparative therapies assessment and cost-effectiveness analysis. Future development of frailty and HRQOL assessment may improve informed consent and provide an invaluable tool to surgeons counselling elderly patients about to undergo coronary surgery. Further prospective randomized trials are urgently warranted, utilizing advanced analytical techniques to assess HRQOL outcomes.
Conflict of interest: none declared.
REFERENCES
- 1.Natarajan A, Samadian S, Clark S. Coronary artery bypass surgery in elderly people. Postgrad Med J. 2007;83:154–8. doi: 10.1136/pgmj.2006.049742. doi:10.1136/pgmj.2006.049742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spencer. Bureau of the Census: Projections of the population of the United States, by age, sex and race; 1988–2080. Curr Popul Rep Ser. 1980;1018:1988–2080. 1989;1018:25. [PubMed] [Google Scholar]
- 3.Peterson ED, Jollis JG, Bebchuk JD, DeLong ER, Muhlbaier LH, Mark DB, et al. Changes in mortality after myocardial revascularization in the elderly. The national Medicare experience. Ann Intern Med. 1994;121:919–27. doi: 10.7326/0003-4819-121-12-199412150-00003. doi:10.7326/0003-4819-121-12-199412150-00003. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2:i–iv. 1–74. [PubMed] [Google Scholar]
- 5.Black N. Patient reported outcome measures could help transform healthcare. Br Med J. 2013;346:167. doi: 10.1136/bmj.f167. doi:10.1136/bmj.f167. [DOI] [PubMed] [Google Scholar]
- 6.Santo Tomas LH, Varkey B. Improving health-related quality of life in chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2004;10:120–7. doi: 10.1097/00063198-200403000-00006. doi:10.1097/00063198-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Kymes SM, Lee BS. Preference-based quality of life measures in people with visual impairment. Optom Vis Sci. 2007;84:809–16. doi: 10.1097/OPX.0b013e3181337638. doi:10.1097/OPX.0b013e3181337638. [DOI] [PubMed] [Google Scholar]
- 8.Noyez L, de Jager MJ, Markou AL. Quality of life after cardiac surgery: underresearched research. Interact CardioVasc Thorac Surg. 2011;13:511–4. doi: 10.1510/icvts.2011.276311. doi:10.1510/icvts.2011.276311. [DOI] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. doi:10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organisation Expert Committee. WHO Technical Report Series, No. 779. World Health Organization, Geneva 1989. ISBN: 9241207795. [PubMed] [Google Scholar]
- 11.Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e123–210. doi: 10.1016/j.jacc.2011.08.009. doi:10.1016/j.jacc.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41:2613–9. doi: 10.1016/j.ejca.2005.05.017. doi:10.1016/j.ejca.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Barnett SD, Halpin LS. Functional status improvement in the elderly following coronary artery bypass graft. J Nurs Care Qual. 2003;18:281–7. doi: 10.1097/00001786-200310000-00006. doi:10.1097/00001786-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Loponen P, Luther M, Wistbacka JO, Korpilahti K, Laurikka J, Sintonen H, et al. Quality of life during 18 months after coronary artery bypass grafting. Eur J Cardiothorac Surg. 2007;32:77–82. doi: 10.1016/j.ejcts.2007.03.045. doi:10.1016/j.ejcts.2007.03.045. [DOI] [PubMed] [Google Scholar]
- 15.Markou AL, van der Windt A, van Swieten HA, Noyez L. Changes in quality of life, physical activity, and symptomatic status one year after myocardial revascularization for stable angina. Eur J Cardiothorac Surg. 2008;34:1009–15. doi: 10.1016/j.ejcts.2008.08.003. doi:10.1016/j.ejcts.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Markou AL, Selten K, Krabbe PF, Noyez L. Quality of life one year post myocardial revascularization and aortic valve replacement in patients aged 70 year or older. J Cardiovasc Surg (Torino) 2011;52:601–7. [PubMed] [Google Scholar]
- 17.Conaway DG, House J, Bandt K, Hayden L, Borkon AM, Spertus JA. The elderly: health status benefits and recovery of function one year after coronary artery bypass surgery. J Am Coll Cardiol. 2003;42:1421–6. doi: 10.1016/s0735-1097(03)01052-0. doi:10.1016/S0735-1097(03)01052-0. [DOI] [PubMed] [Google Scholar]
- 18.Glower DD, Christopher TD, Milano CA, White WD, Smith LR, Jones RH, et al. Performance status and outcome after coronary artery bypass grafting in persons aged 80 to 93 years. Am J Cardiol. 1992;70:567–71. doi: 10.1016/0002-9149(92)90192-2. doi:10.1016/0002-9149(92)90192-2. [DOI] [PubMed] [Google Scholar]
- 19.Hedeshian MH, Namour N, Dziadik E, Stewart RD, Campos CT. Does increasing age have a negative impact on six-month functional outcome after coronary artery bypass? Surgery. 2002;132:239–44. doi: 10.1067/msy.2002.125388. doi:10.1067/msy.2002.125388. [DOI] [PubMed] [Google Scholar]
- 20.Huber CH, Goeber V, Berdat P, Carrel T, Eckstein F. Benefits of cardiac surgery in octogenarians—a postoperative quality of life assessment. Eur J Cardiothorac Surg. 2007;31:1099–105. doi: 10.1016/j.ejcts.2007.01.055. doi:10.1016/j.ejcts.2007.01.055. [DOI] [PubMed] [Google Scholar]
- 21.Wilson MF, Baig MK, Ashraf H. Quality of life in octagenarians after coronary artery bypass grafting. Am J Cardiol. 2005;95:761–4. doi: 10.1016/j.amjcard.2004.11.031. doi:10.1016/j.amjcard.2004.11.031. [DOI] [PubMed] [Google Scholar]
- 22.Jarvinen O, Saarinen T, Julkunen J, Huhtala H, Tarkka MR. Changes in health-related quality of life and functional capacity following coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2003;24:750–6. doi: 10.1016/s1010-7940(03)00413-5. doi:10.1016/S1010-7940(03)00413-5. [DOI] [PubMed] [Google Scholar]
- 23.MacDonald P, Stadnyk K, Cossett J, Klassen G, Johnstone D, Rockwood K. Outcomes of coronary artery bypass surgery in elderly people. Can J Cardiol. 1998;14:1215–22. [PubMed] [Google Scholar]
- 24.Kaiser C, Kuster GM, Erne P, Amann W, Naegeli B, Osswald S, et al. Risks and benefits of optimised medical and revascularisation therapy in elderly patients with angina–on-treatment analysis of the TIME trial. Eur Heart J. 2004;25:1036–42. doi: 10.1016/j.ehj.2004.02.033. doi:10.1016/j.ehj.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 25.Jensen BO, Hughes P, Rasmussen LS, Pedersen PU, Steinbruchel DA. Health-related quality of life following off-pump versus on-pump coronary artery bypass grafting in elderly moderate to high-risk patients: a randomized trial. Eur J Cardiothorac Surg. 2006;30:294–9. doi: 10.1016/j.ejcts.2006.04.015. doi:10.1016/j.ejcts.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Nielsen PH, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation. 2012;125:2431–9. doi: 10.1161/CIRCULATIONAHA.111.052571. doi:10.1161/CIRCULATIONAHA.111.052571. [DOI] [PubMed] [Google Scholar]
- 27.Kallis P, Unsworth-White J, Munsch C, Gallivan S, Smith EE, Parker DJ, et al. Disability and distress following cardiac surgery in patients over 70 years of age. Eur J Cardiothorac Surg. 1993;7:306–11. doi: 10.1016/1010-7940(93)90172-8. discussion 12 doi:10.1016/1010-7940(93)90172-8. [DOI] [PubMed] [Google Scholar]
- 28.Kurlansky PA, Williams DB, Traad EA, Carrillo RG, Schor JS, Zucker M, et al. Arterial grafting results in reduced operative mortality and enhanced long-term quality of life in octogenarians. Ann Thorac Surg. 2003;76:418–26. doi: 10.1016/s0003-4975(03)00551-4. discussion 27 doi:10.1016/S0003-4975(03)00551-4. [DOI] [PubMed] [Google Scholar]
- 29.Artinian NT, Duggan C, Miller P. Age differences in patient recovery patterns following coronary artery bypass surgery. Am J Crit Care. 1993;2:453–61. [PubMed] [Google Scholar]
- 30.Murphy SF, Nickerson NJ, Kouchoukos NT. Functional outcome in the elderly after coronary artery surgery. Medsurg Nurs. 1996;5:107–10. [PubMed] [Google Scholar]
- 31.Sollano JA, Rose EA, Williams DL, Thornton B, Quint E, Apfelbaum M, et al. Cost-effectiveness of coronary artery bypass surgery in octogenarians. Ann Surg. 1998;228:297–306. doi: 10.1097/00000658-199809000-00003. doi:10.1097/00000658-199809000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Graham MM, Norris CM, Galbraith PD, Knudtson ML, Ghali WA. Quality of life after coronary revascularization in the elderly. Eur Heart J. 2006;27:1690–8. doi: 10.1093/eurheartj/ehl038. doi:10.1093/eurheartj/ehl038. [DOI] [PubMed] [Google Scholar]
- 33.Kamiya M, Takayama M, Takano H, Murai K, Hinokiyama K, Ochi M, et al. Clinical outcome and quality of life of octogenarian patients following percutaneous coronary intervention or surgical coronary revascularization. Circ J. 2007;71:847–54. doi: 10.1253/circj.71.847. doi:10.1253/circj.71.847. [DOI] [PubMed] [Google Scholar]
- 34.Luqman Z, Ansari J, Siddiqui FJ, Sami SA. Is urgent coronary artery bypass grafting a safe option in octogenarians? A developing country perspective. Interact CardioVasc Thorac Surg. 2009;9:441–5. doi: 10.1510/icvts.2009.204156. doi:10.1510/icvts.2009.204156. [DOI] [PubMed] [Google Scholar]
- 35.Fruitman DS, MacDougall CE, Ross DB. Cardiac surgery in octogenarians: can elderly patients benefit? Quality of life after cardiac surgery. Ann Thorac Surg. 1999;68:2129–35. doi: 10.1016/s0003-4975(99)00818-8. doi:10.1016/S0003-4975(99)00818-8. [DOI] [PubMed] [Google Scholar]
- 36.Makintosh ACC, Fitzpatrick R. A structured review of patient-reported outcome measures used in elective procedures for coronary revascularisation. Report to the Department of Health. University of Oxford 2010. http://phi.uhce.ox.ac.uk/pdf/ElectiveProcedures/PROMs_Oxford_Elective%20Cardiac_012011.pdf. (1 November 2012, date last accessed) [Google Scholar]
- 37.Schroter S, Lamping DL. Coronary revascularisation outcome questionnaire (CROQ): development and validation of a new, patient based measure of outcome in coronary bypass surgery and angioplasty. Heart. 2004;90:1460–6. doi: 10.1136/hrt.2003.021899. doi:10.1136/hrt.2003.021899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trial of invasive versus medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomised trial. Lancet. 2001;358:951–7. doi: 10.1016/S0140-6736(01)06100-1. doi:10.1016/S0140-6736(01)06100-1. [DOI] [PubMed] [Google Scholar]
- 39.Zhang Z, Mahoney EM, Stables RH, Booth J, Nugara F, Spertus JA, et al. Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: one-year results from the stent or surgery trial. Circulation. 2003;108:1694–700. doi: 10.1161/01.CIR.0000087600.83707.FD. doi:10.1161/01.CIR.0000087600.83707.FD. [DOI] [PubMed] [Google Scholar]
- 40.Cohen DJ, Van Hout B, Serruys PW, Mohr FW, Macaya C, den Heijer P, et al. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011;364:1016–26. doi: 10.1056/NEJMoa1001508. doi:10.1056/NEJMoa1001508. [DOI] [PubMed] [Google Scholar]
- 41.Dunning J, Waller JR, Smith B, Pitts S, Kendall SW, Khan K. Coronary artery bypass grafting is associated with excellent long-term survival and quality of life: a prospective cohort study. Ann Thorac Surg. 2008;85:1988–93. doi: 10.1016/j.athoracsur.2008.02.024. doi:10.1016/j.athoracsur.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 42.Smith LR, Milano CA, Molter BS, Elbeery JR, Sabiston DC, Jr, Smith PK. Preoperative determinants of postoperative costs associated with coronary artery bypass graft surgery. Circulation. 1994;90(5 Pt 2):II124–8. [PubMed] [Google Scholar]
- 43.Weinstein MC, Stason WB. Cost-effectiveness of coronary artery bypass surgery. Circulation. 1982;66(5 Pt 2):III56–66. [PubMed] [Google Scholar]
- 44.Wong JB, Sonnenberg FA, Salem DN, Pauker SG. Myocardial revascularization for chronic stable angina. Analysis of the role of percutaneous transluminal coronary angioplasty based on data available in 1989. Ann Intern Med. 1990;113:852–71. doi: 10.7326/0003-4819-113-11-852. doi:10.7326/0003-4819-113-11-852. [DOI] [PubMed] [Google Scholar]
- 45.Claude J, Schindler C, Kuster GM, Schwenkglenks M, Szucs T, Buser P, et al. Cost-effectiveness of invasive versus medical management of elderly patients with chronic symptomatic coronary artery disease. Findings of the randomized trial of invasive versus medical therapy in elderly patients with chronic angina (TIME) Eur Heart J. 2004;25:2195–203. doi: 10.1016/j.ehj.2004.09.013. doi:10.1016/j.ehj.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 46.Lally F, Crome P. Understanding frailty. Postgrad Med J. 2007;83:16–20. doi: 10.1136/pgmj.2006.048587. doi:10.1136/pgmj.2006.048587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee DH, Buth KJ, Martin BJ, Yip AM, Hirsch GM. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation. 2010;121:973–8. doi: 10.1161/CIRCULATIONAHA.108.841437. doi:10.1161/CIRCULATIONAHA.108.841437. [DOI] [PubMed] [Google Scholar]
- 48.Singh S, Bailey KR, Noheria A, Kullo IJ. Frailty across the spectrum of ankle-brachial index. Angiology. 2012;63:229–36. doi: 10.1177/0003319711413457. doi:10.1177/0003319711413457. [DOI] [PubMed] [Google Scholar]
- 49.Chaudhry SI, Gill TM. Geriatric assessment to improve risk stratification in older patients undergoing coronary revascularization. Circ Cardiovasc Qual Outcomes. 2011;4:491–2. doi: 10.1161/CIRCOUTCOMES.111.962647. doi:10.1161/CIRCOUTCOMES.111.962647. [DOI] [PubMed] [Google Scholar]
- 50.Koch CG, Khandwala F, Blackstone EH. Health-related quality of life after cardiac surgery. Semin Cardiothorac Vasc Anesth. 2008;12:203–17. doi: 10.1177/1089253208323411. doi:10.1177/1089253208323411. [DOI] [PubMed] [Google Scholar]
- 51.Gill TM, Feinstein AR. A critical appraisal of the quality of quality-of-life measurements. JAMA. 1994;272:619–26. doi:10.1001/jama.1994.03520080061045. [PubMed] [Google Scholar]
- 52.Hays RD, Anderson RT, Revicki D. Assessing reliability and validity of measurement in clinical trials. In: Staquet MJ, Hays RD, Fayers PM, editors. Quality of life assessment in clinical trials: methods and practice. Oxford, England: Oxford University Press; 1998. pp. 169–82. [Google Scholar]
- 53. Bert Spilker (Ed). Quality of life and pharmacoeconomics in clinical trials (2nd edn). Philadelphia, New York, Lippincott-Raven Publishers, 1996. [Google Scholar]
- 54.Grady KL, Lee R, Subacius H, Malaisrie SC, McGee EC, Jr, Kruse J, et al. Improvements in health-related quality of life before and after isolated cardiac operations. Ann Thorac Surg. 2011;91:777–83. doi: 10.1016/j.athoracsur.2010.11.015. doi:10.1016/j.athoracsur.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 55.Yun KL, Sintek CF, Fletcher AD, Pfeffer TA, Kochamba GS, Mahrer PR, et al. Time related quality of life after elective cardiac operation. Ann Thorac Surg. 1999;68:1314–20. doi: 10.1016/s0003-4975(99)00675-x. doi:10.1016/S0003-4975(99)00675-X. [DOI] [PubMed] [Google Scholar]