Abstract
We report a case of granulations that complicated subglottic stent placement and completely destroyed vocal folds with luminal stent obstruction. A microbial aetiology significantly contributed to the occurrence of granulations associated with mechanical irritation. The granulations were successfully resected using a digital AcuBlade laser system, a new generation of CO2 laser used in otorhinolaryngology, particularly in vocal cord disease. It permitted a precise control of the scan line between vocal fold and granulation for several reasons. The scan line was completely electronic and integrated in the scanner. The sweep in speed was constant and the energy distribution was uniform along the entire length of the time. The interpulse pause was of ∼1 ms, allowing the tissue cooling with reduction of thermal spread and quicker healing support. The result was the radical excision of granulations without injuring vocal folds. The respiratory function was restored and no other treatments such as arytenoidectomy or cordectomy associated with the alteration of phonatry function were required. No intraoperative or/and postoperative complications were registered and the patient was discharged 7 days after the procedure.
Keywords: Subglottic stenosis, Granulation, Air way stent, Laser resection, Vocal fold
INTRODUCTION
Despite several techniques are reported, the endoscopic treatment of granulation after stent placement just below the vocal cords is challenging. Herein, we report the use of digital AcuBlade™ robotic microsurgery system (Lumenis, Rome, Italy), a new generation of CO2, laser to remove huge vocal folds granulations after subglottic stent placement.
CLINICAL CASE
A 47-year old man with post-intubation subglottic stenosis was dilated without success in another hospital; tracheostomy was then performed for respiratory failure and referred to our attention. Because the patient was unfit for surgery, the stenosis was dilated using rigid bronchoscopy and a Montgomery T-tube was placed. Unfortunately, the patient re-developed stenosis following the removal of the T tube after 9 months.
A rigid bronchoscopy was performed under general anaesthesia. A subglottic stenosis located 1.5 cm from the vocal folds was found. The stenosis was redilated and a silicone Dumon stent (length: 60 mm, width: 17 mm) inserted in a standard manner at 1 cm from the vocal folds. After 2 weeks, the stent migrated under the stenosis. It was re-placed just below the vocal folds to avoid further migration and to preserve phonation. The patient was discharged 3 days later. In the first 5 months after the procedure, he underwent large-drop aerosol treatment and repeated bronchoscopy aspiration. The aspiration was stopped at the time of the summer holidays for ∼2 months. In this period, the patient complained of progressive symptoms: bad breath, difficult phonation and airway obstruction. He was re-admitted on the assumption that the stent had migrated further. Endoscopy showed the stent in situ but the vocal folds completely covered by huge granulations (Fig. 1A) obstructing the stent (Fig. 1B).
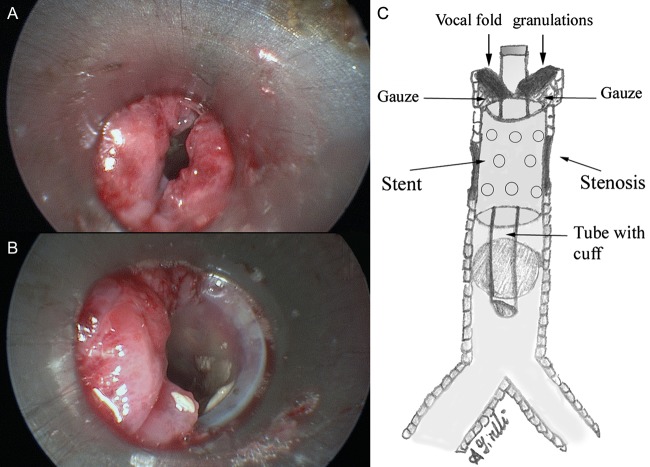
Figure 1:
Rigid bronchoscopy showed the presence of bilateral huge granulations that completely covered vocal folds (A). Under granulations, the stent resulted to be in site but its lumen was partially obstructed by granulation (B). The patient was intubated with a small laser-safe endo-tracheal tube which passed through the stent. To preserve the stent from thermal injury, a gauze was placed around the orotracheal tube under granulations (C).
Probably, mucus accumulation in the stent due to the lack of aspiration supported bacterial colonization. Then, the stent infection and the mechanical irritation promoted granulation growth.
The patient was intubated with a small laser-safe endo-tracheal tube which passed through the stent. The granulations were ablated using the AcuBlade system through the suspended laryngoscope and with an operative microscope. To preserve the stent from laser thermal injury, a gauze was placed under the granulation (Fig. 1C). After the procedure, the vocal folds seemed to be normal and the luminal stent free (Fig. 2A). The patient was extubated the day after; bronchoscopy showed normal function of the vocal folds. The stent was in situ with normal patency; bacterial culture resulted negative for stent colonization. The patient was afebrile, having normal phonation and breathing. He was discharged 7 days after the procedure. Three months later, bronchoscopy showed normal vocal folds with stent patency (Fig. 2B).
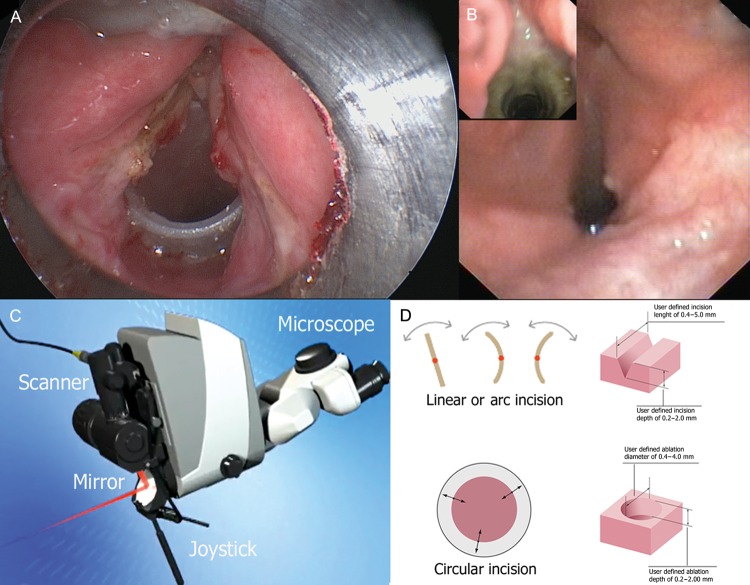
Figure 2:
The granulations were completely resected, and after the procedure the vocal folds seemed to be normal and the luminal stent free (A). Endoscopic view showed patent glottic lumen at 3-month follow-up (B). AcuBlade™ connected with an operative microscope is reported in (C). The scanner is a device connected between the laser arm and the micromanipulator. By a computer-guided system of rotating mirrors, the scanner allows the beam to sweep a given surface with extreme rapidity. Scan patterns enable incision (linear or arc-incision) and ablation (circle) using parameters proposed by laser-controlling software. The incision line can be rotated to the right or left with joystick (D).
DISCUSSION
When the proximal end of the silicon stent is placed just below the vocal folds, granulation tissue may occasionally grow around the tip and disturb the ventilation. Its treatment is reported in a number of papers using different techniques [1, 2]. The digital AcuBlade laser system is commonly used in otorhinolaryngology, especially in vocal cord disease, but no papers have addressed its use in such an issue.
AcuBlade™ is a scanning micromanipulator system that combines the ability to contour the laser beam (scanning micromanipulator technology) with the addition of laser setting automation. The micromanipulator yields the smallest possible beam diameter presently available, i.e. 250 µm for a local length of 400 nm. The scanner is a device connected between the laser arm and the micromanipulator. By a computer-guided system of rotating mirrors, the scanner allows the beam to sweep a given surface with extreme rapidity (Fig. 2C). Scan patterns enable ablation (circle) and incision (linear or arc-incision). The incision length (0.4–5.0 mm) and depth (0.2–2 mm) or ablation diameter (0.4–4.0 mm) are programmable (Fig. 2D). The software-calculated penetration depth is based on the average absorption of the CO2 laser by living soft tissues. According to the desired length and penetration, the software calculates the required power and pulse duration for the single pulse mode [3]. However, the surgeon can modify the parameter proposed by laser-controlling software in any case.
In the presented case, the laser setting used was a linear-incision of 2 mm beam length with 2 mm penetration; the ultrapulsed wave was used in a continued pulse mode with a 400-mm focal length; the power was 10 W with a pulse duration of 0.5 s. Similar values were proposed by Remacle et al. [3, 4] for resecting the nodules of vocal folds. During the procedure, it was mandatory to maintain the tissue in the same dissection plane, in order not to deviate from the desired incision. AcuBlade permitted a precise control of the scan line between vocal fold and granulation for several reasons. The scan line was completely electronic and integrated in the scanner. The sweep in speed was constant and the energy distribution was uniform along the entire length of the time. The interpulse pause was of ∼1 ms, allowing tissue cooling with reduction of thermal spread and quicker healing support [3]. The result was the radical excision of granulations without injuring the vocal folds. The respiratory function was restored and no other treatments such as arytenoidectomy or cordectomy associated with the alteration of phonatry function were required. No intraoperative or/and postoperative complications were registered. However, we preferred having the patient under observation for several days (7 days) to prevent an emergency admission in case of complications.
Good results are reported applying laser surgery to vocal cords granulation [1]. However, subglottic stenosis is an area that offers poor access to the linearly transmitted CO2 laser. This may be associated with several complications such as thermal injury, scar formation and airway restenosis [1, 5]. To avoid thermal spread, cold-knife surgery may be used despite haemorrhages and a lack of uniform dissections are potential complications in non-expert hands. The microdebrider has achieved enormous success in granulation stenosis, laryngeal papillomas and endobronchial tumour [1, 2], which are different lesions compared with the present case.
Finally, AcuBlade may be used in treating vocal folds granulation after stent placement in the subglottic area. In expert hands, it allows the complete resection of granulation, preserving phonation conversely, to other procedures such as arytenoidectomy or cordectomy.
Acknowledgement
The authors thank Giovanni Galluccio for his assistance during the treatment of the present case.
Conflict of interest: none declared.
REFERENCES
- 1.Hsieh MJ, Liu YH, Yueh YS, Ko PJ. Use of microdebrider in glottic stenosis following airway stenting. Eur J Cardiothorac Surg. 2006;30:388–90. doi: 10.1016/j.ejcts.2006.04.041. [DOI] [PubMed] [Google Scholar]
- 2.Pasquale K, Wiatrak B, Woolley A, Lewis L. Microdebrider versus CO2 laser removal of recurrent respiratory papillomas: a prospective analysis. Laryngoscope. 2003;113:139–43. doi: 10.1097/00005537-200301000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Remacle M, Lawson G, Nollevaux MC, Delos M. Current state of scanning micromanipulator applications with the carbon dioxide laser. Ann Otol Rhinol Laryngol. 2008;117:239–44. doi: 10.1177/000348940811700401. [DOI] [PubMed] [Google Scholar]
- 4.Remacle M, Hassan F, Cohen D, Lawson G, Delos M. New computer-guided scanner for improving CO2 laser-assisted microincision. Eur Arch Otorhinolaryngol. 2005;262:113–9. doi: 10.1007/s00405-004-0746-8. [DOI] [PubMed] [Google Scholar]
- 5.Ossoff RH, Werkhaven JA, Dere H. Soft-tissue complications of laser surgery for recurrent respiratory papillomatosis. Laryngoscope. 1991;101:1162–64. doi: 10.1288/00005537-199111000-00004. [DOI] [PubMed] [Google Scholar]