Abstract
Objective of present study is to evaluate the possible role of clopidogrel in improving glycemic indices and oxidative stress in patients with type 2 diabetes.
This study was performed on 42 uncontrolled type 2 diabetic patients at the specialized center for Endocrinology and Diabetes, Al-Rasafa Directorate of Health, Baghdad. All of the patients were treated with (glibenclamide 5 mg at morning) and randomized into two groups: the first group includes 22 patients treated with clopidogrel tablets (75 mg/day) for 2 months; the second group includes 20 patients treated with a placebo formula (sodium bicarbonate 200 mg/day) for the same period. Treatment with clopidogrel produced significant improvement (P < 0.05) in fasting serum glucose (FSG), fasting serum insulin level, quantitative insulin sensitivity check index (QUICKI); and oxidative stress markers: serum malondialdehyde (MDA) and serum reduced glutathione (GSH) compared to their baseline levels. There was significant elevation (P < 0.05) in both FSG and fasting serum insulin and the MDA level with significant reduction (P < 0.05) in QUICKI of placebo group compared to their baseline levels. However, clopidogrel produced significant elevation (P < 0.05) in AST and ALT levels but placebo formula caused no significant alteration (P > 0.05) in the serum levels of these two enzymes.
In conclusion the treatment with clopidogrel improved glycemic indices and reduced oxidative stress in patients with type 2 diabetes.
Keywords: Clopidogrel, Glycemic indices, Malondialdehyde, Reduced glutathione, Type 2 diabetes
1. Introduction
Type 2 diabetes accounts for about 90–95% of those with diabetes. Previously it was known as non-insulin dependent diabetes or adult onset diabetes. It involves insulin resistance and relative insulin deficiency as seen in type 1 diabetes (Flower, 2007). Insulin resistance is strongly associated with obesity and physical inactivity, and several mechanisms mediating this interaction have been identified. A number of circulating hormones, cytokines, and metabolic fuels, such as free fatty acids (FFA) originate in the adipocytes and modulate insulin action. An increased mass of stored triglyceride, especially visceral or deep subcutaneous adipose depot, leads to large adipocytes that are themselves resistant to the ability of insulin to suppress lipolysis; this results in increased release and circulating level of FFA and glycerol, both of which aggravate insulin resistance in skeletal muscle and liver (Stumvoll et al., 2005). These FFA can influence insulin signaling pathway by activating of several serine/thionine kinases, reducing the tyrosine phosphorylation on insulin receptor substrate (IRS) and impairing IRS/phospho-inositide-3-kinase pathway (Kowalska, 2007; White, 2002). Recently, several groups provided strong evidence to support the concept of adipose tissue as an endocrine organ producing cytokines which modulate glucose homeostasis (Saltiel and Kahn, 2001). Tumor necrosis factor alpha (TNF-α) is a cytokine produced by adipocytes that may contribute to the development of insulin resistance in obesity. TNF-α can impair insulin action on glucose metabolism and increase lipolysis. At the molecular level, TNF-α increases serine phosphorylation of IRS-1 and down regulates GLUT-4 expression, thereby contributing to insulin resistance (Saltiel and Kahn, 2001; Kahn and Flier, 2000).
Oxidative stress plays a central role in the onset of diabetes mellitus as well as in the development of vascular and neurological complications of the disease. The source of oxidative stress is a cascade of reactive oxygen species (ROS) leaking from mitochondria and this process has been associated with the onset of type 1 diabetes via the apoptosis of pancreatic B-cells and the onset of type 2 diabetes via insulin (Phillips et al., 2004). Hyperglycemia in diabetic patients leads via several mechanisms that, include increased polyol pathway flux increased intracellular advanced glycation end product formation, activation of protein kinase C (PKC) and increased hexoseamine pathway flux, to multiple biochemical squeal aimed to an increased production of ROS (Bonnefont-Rousselet, 2002).
Clopidogrel is a potent antiplatelet drug which belongs to thioenpyridine derivatives. It selectively inhibits the binding of ADP to its platelets receptor and the subsequent ADP mediated activation of the glycoprotein GP11b/111a complex, thereby inhibiting platelet aggregation (Richter et al., 2004). Type 2 diabetes is a state of increased plasma coagulability. The platelet aggregatability is increased and fibrinolytic capacity is reduced. Antiplatelet therapy, notably use of aspirin, has been shown to be effective in reducing cardiovascular events, but clopidogrel has been appeared to be more potent than aspirin in reducing cardiovascular events in patients with type 2 diabetes (Mooradian, 2003). The protective effects of clopidogrel on oxidant damage in a rat model of acute ischemia have been studied. The results of this study revealed that clopidogrel prevents the increase in MDA level and the decrease in GSH level and SOD activity caused by the ischemia–reperfusion in both tissue and plasma samples (Kanko et al., 2005). MDA is known as the main parameter showing the level of lipid peroxidation process induced by oxidative stress. The primary antioxidative enzyme, SOD and GSH, powerful antioxidants are among the first line of defense mechanism against oxidative stress (Cheeseman and Slater, 1993). Clopidogrel also reduces levels of serum hs-CRP and TNF-α in patients with non-ST segment elevation acute coronary syndrome. Elevated levels of markers for inflammation (such as CRP and TNF-α) have been associated with increased risk for first and recurrent cardiovascular events (Chen et al., 2006). Clopidogrel is considered not just an antiplatelet agent but a drug with pleiotropic effects, which contribute to its long term benefit (Angiolillo et al., 2006).
2. Materials and methods
2.1. Chemicals
Glucose, AST and ALT are measured using kits supplied by Randox, UK. Mogrel® (Clopidogrel 75 mg) tablets are purchased from Mission, India. Insulin ELISA kits provided by DRG International Inc., USA.
2.2. Patients and control subjects
This study was performed on 42 uncontrolled type 2 diabetic patients at the specialized center for Endocrinology and Diabetes, Al-Rasafa Directorate of Health – Baghdad (24 males and 18 females) with age range (40–68 years), and with mean duration of diabetes of 5 years.
The selected patients attended the medical center from November 2007 to May 2008 during their periodic visit seeking for medical advice concerning their diet modification, weight reduction and drug prescription. The diabetic patients were selected by a senior physician and those patients were diagnosed as diabetic according to the American Diabetes Association Criteria [fasting plasma glucose ⩾126 mg/dL (7.0 mmol/L) or 2 h plasma glucose after oral glucose tolerance test ⩾200 mg/dL (11.1 mmol/L)] (American Diabetic Association, 2008). All the selected patients have no other prominent pathological disorders like hypertension and IHD. The patients were already treated with ordinary hypoglycemic agent glibenclamide, but with poor glycemic control as evidenced by the abnormal values of fasting plasma glucose.
Patient’s selection and enrollment in the study after their agreement was performed according to the following exclusion criteria:
-
1.
Patients with chronic disease like liver, kidney disorder and cardiovascular complications, or acute infections.
-
2.
Patients with pregnancy or breast feeding are excluded.
-
3.
Patients with history of alcohol consumption are excluded.
-
4.
Patients with history of active pathological bleeding such as peptic ulcer and intracranial hemorrhage.
-
5.
Patients on insulin therapy or maintained on any type of anti-oxidant drugs or aspirin.
The selected patients were divided randomly into two groups:
-
1.
Clopidogrel group: included 22 patients (14 males and 8 females) treated with antiplatelet agent clopidogrel bisulfate in a dose of one tablet (75 mg) ingested once daily for 2 months in addition to the routinely used oral hypoglycemic agent (glibenclamide 5 mg in the morning).
-
2.
Placebo group B: included 20 patients (10 males and 10 females) were treated with placebo capsules containing sodium bicarbonate (Liu et al., 1997) in a dose of one capsule 200 mg ingested once daily for 2 months duration, in addition to the routinely used oral hypoglycemic agent (glibenclamide 5 mg at morning). Sixteen healthy control subjects (7 male and 9 females) with the same age range of patients were selected to evaluate the normal values of the studied parameters (Fig. 1).
Figure 1.
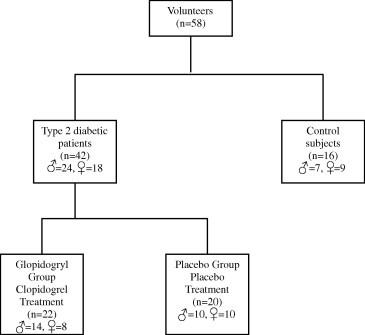
Distribution of volunteers included in the study.
All patients received their treatment for 2 months duration, and blood samples were collected from them at the beginning of the study (baseline samples) and after 2 months of starting treatment to measure the possible change in the studied parameters (see Table 1).
Table 1.
Characteristics of control subjects and type 2 diabetic patients.
| Variable | Type 2 diabetic patient | Healthy control subjects |
|---|---|---|
| Number | 42 | 16 |
| Gender (male/female) | 24/18 | 7/9 |
| Age (years) | 52.04 ± 7.31 | 48.19 ± 6.76 |
| BMI (kg/m2) | 28.28 ± 3.68 | 27.07 ± 3.52 |
| FSG (mmol/L) | 9.10 ± 2.87 | 4.87 ± 0.63 |
| Systolic blood pressure (mmHg) | 120.64 ± 0.70 | 120.00 ± 1.21 |
| Diastolic blood pressure (mmHg) | 80.45 ± 0.74 | 70.75 ± 0.68 |
The data are expressed as mean ± SD.
BMI = body mass index; FSG = fasting serum glucose.
2.3. Samples collection and preparation
After 12 h fasting, blood samples were collected from all subjects by vein puncture (10 mL), before starting drug treatment (as baseline sample) and then after 2 months of treatment to follow the changes in the studied parameters.
The blood was collected in plane tubes and after clotting was centrifuged at 3000 rpm for 10 min to obtain serum. Fresh serum was used for the measurement of MDA (biomarker of lipid peroxidation) and GSH (a biomarker of antioxidant system). The remaining serum was stored frozen at −20 °C until analysis was performed.
2.4. Measurement of serum glucose level
Glucose was determined by enzymatic oxidation in the presence of glucose oxidase (Barham and Trinder, 1972).
2.5. Determination of serum insulin level
The insulin ELISA kit is a solid phase-enzyme-linked immunosorbent assay based on the sandwich principle (Flier et al., 1979). The microtiter wells are coated with monoclonal antibody directed toward a unique antigenic site on human insulin molecule. An aliquot of patient’s sample containing endogenous insulin is incubated in the coat well with enzyme conjugate, which is an anti-insulin antibody conjugated with biotin. After incubation the unbound conjugate is washed off. During the second incubation step streptavidin–peroxidase enzyme complex binds to biotin–anti-insulin antibody. The mount of bound horseradish peroxidase (HRP) complex is proportional to the concentration of insulin in the sample. Having added the substrate solution, the intensity of color developed is proportional to the concentration of insulin in the patient sample with running proper standards of insulin. Absorbance was measured spectrophotometrically at 450 nm. The results were expressed as μIU/mL. Serum insulin levels were determined for the diabetic patients and control subjects.
2.6. Estimation of insulin sensitivity
Insulin sensitivity was determined using the quantitative insulin sensitivity check index (QUICKI) which is calculated from fasting plasma glucose (FPG) and fasting plasma insulin (FPI) using the following formula (Katz et al., 2000):
2.7. Assessment of lipid peroxidation
Determination of lipid peroxidation performed by estimation of MDA, the degradative by-product of peroxidized lipid after reaction with thiobarbituric acid (TBA) to form MDA-TBA2 complex, a red chromophore that can be analyzed spectrophotometrically depending on the method of Beuge and Aust (1978). The procedure includes the addition of 1 mL of TBA reagent [0.375 g TBA, 15 g trichloroacetic acid (TCA) and 2.1 mL of 11.9 N hydrochloric acid, up to 100 mL distilled water] to 0.5 mL of serum. After mixing, the mixture was heated in water bath at 95 °C for 15 min, cooled and centrifuged at 3000 rpm in cooled centrifuge for 10 min. Light absorbance of clear supernatant was determined at 535 nm. The MDA concentration is calculated using a molar absorptivity coefficient of 1.56 × 105 M−1 cm−1. The results were expressed as μmol/L.
2.8. Serum glutathione determination
Serum reduced glutathione (GSH) content was determined according to the method of Ellman (1959), that included the addition of 0.5 mL of serum to equal volume of 4% sulfosalicylic acid and centrifuged in cooled centrifuge for the precipitation of protein, then 0.5 mL of clear supernatant was added to 4.5 mL of 5,5-dithiobis-(2-nitrobenzoic acid), DTNB reagent [0.1 mM of DTNB in 0.1 M phosphate buffer, pH 8]. The absorbance of the solution is measured at 412 nm after 2 min. Serum glutathione concentration is calculated using a molar absorptivity coefficient of 13,600 M−1 cm−1. The final results were expressed as μmol/L.
2.9. Determination of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) activities in serum
The activities of AST and ALT were calculated calorimetrically according to the method of Reitman (Reitman and Frankel, 1957).
2.10. Statistical analysis
The results were expressed as mean ± standard error of mean (SEM) or percent of changes. Student’s t-test was used to examine the degree of significance. P values less than 0.05 were considered significant. The statistical analysis was performed using Microsoft Excel 2003.
3. Results
3.1. Effect of treatment with clopidogrel on fasting serum glucose, serum insulin level and quantitative insulin sensitivity check index (QUICKI)
Results presented in Table 2 revealed that the levels of fasting serum glucose (FSG) in diabetic patients (clopidogrel group and placebo group) were significantly elevated (P < 0.05) over those of controls during the treatment period.
Table 2.
Effect of 2 months treatment with clopidogrel or with placebo on glycemic control markers (FSG, insulin level and insulin sensitivity) in diabetic patients taking glibenclamide.
| Control (n = 16) | Clopidogrel group (n = 22) | Placebo group (n = 20) | |
|---|---|---|---|
| FSG (mmol/L) | |||
| Baseline | 4.875 ± 0.159 | 9.705 ± 0.743⁎,a | 8.415 ± 0.418⁎,a |
| After 60 days | 7.495 ± 0.532⁎,b | 9.33 ± 0.575⁎,b | |
| % Change | −22.77 | 10.87 | |
| Serum insulin level (mIU/mL) | |||
| Baseline | 7.177 ± 0.950 | 11.76 ± 1.00⁎,a | 13.838 ± 0.943⁎,a |
| After 60 days | 8.981 ± 0.514b | 15.277 ± 1.254⁎,b | |
| % Change | −23.63 | 10.4 | |
| Insulin sensitivity (QUIKI) | |||
| Baseline | 0.364 ± 0.006 | 0.295 ± 0.007⁎,a | 0.304 ± 0.003⁎,a |
| After 60 days | 0.326 ± 0.005⁎,b | 0.298 ± 0.004⁎,b | |
| % Change | 10.51 | −1.97 | |
Data are expressed as mean ± SEM.
n = Number of subjects or patients.
Non-identical superscripts (a, b) within the same group represent significant difference (P < 0.05), by paired t-test.
P < 0.05 with respect to control group, by unpaired t-test.
In patients treated with clopidogrel for 2 months, there was significant decrease in FSG level (P < 0.05) compared with baseline value (7.495 ± 0.532 vs. 9.705 ± 0.743). The patients of placebo treated group showed significant increase in FSG level after 2 months of treatment with placebo formula compared with baseline value (9.33 ± 0.575 vs. 8.415 ± 0.418). Table 2 demonstrated that the significant decline in FSG level after 2 months of clopidogrel treatment, as compared to baseline level, occurred with remarkable percentage of decline in FSG level (22.77%), while in the placebo treated group, significant increase in FSG level occurred after 2 months of placebo therapy, and the percentage of increase was 10.87%.
Determination of serum insulin levels (Table 2) showed that there were significant elevations (P < 0.05) in the baseline value of insulin levels in clopidogrel treated group over those of controls. In placebo treated group the serum insulin levels were significantly elevated (P < 0.05) over those of controls at the baseline and after 2 months of treatment. There were significant decreases in insulin level (P < 0.05) after treatment compared with baseline value in clopidogrel treated group (8.981 ± 0.515 vs. 11.76 ± 1.00), with percentage of decline (−23.63%), while in placebo treated group, there were significant increase in insulin level after treatment compared with baseline value (15.277 ± 1.254 vs. 13.838 ± 0.943) and percentage of increment (10.4%).
The values of QUICKI (Table 2) were significantly different (P < 0.05) in diabetic patients (clopidogrel group and placebo group) as compared to controls at the baseline and after 2 months of treatment. In clopidogrel treated group, there was significant elevation in QUICKI values (P < 0.05) as compared with baseline value (0.326 ± 0.005 vs. 0.295 ± 0.007) and percentage of increase (10.51%). In placebo treated group, there was significant decrease in baseline value (0.298 ± 0.004 vs. 0.304 ± 0.003) and the percentage of decline was 1.97%.
3.2. Effect of treatment with clopidogrel on oxidative stress markers
A significantly higher (P < 0.05) level of MDA was detected in diabetic patients as compared to control during the treatment period (Table 3). In patients treated with clopidogrel, there was a significant reduction in MDA level after 2 months of treatment compared with the baseline value (2.09 ± 0.14 vs. 2.38 ± 0.18). In placebo treated group, there was a significant increase (P < 0.05) in the MDA level after 2 months of treatment compared with baseline value (2.31 ± 0.13 vs. 2.02 ± 0.14). In clopidogrel group, a 12.18% decrease in MDA level was reported and 14.36% increase in MDA level was observed in placebo group.
Table 3.
Effect of 2 months treatment with clopidogrel and with placebo on oxidative stress markers (MDA and GSH) in diabetic patients taking glibenclamide.
| Control (n = 16) | Clopidogrel group (n = 22) | Placebo group (n = 20) | |
|---|---|---|---|
| Serum MDA (μmol/L) | |||
| Baseline | 1.086 ± 0.01 | 2.38 ± 0.18⁎,a | 2.02 ± 0.14⁎,a |
| After 60 days | 2.09 ± 0.14⁎,b | 2.31 ± 0.13⁎,b | |
| % Change | −12.18 | 14.36 | |
| Serum GSH (μmol/L) | |||
| Baseline | 0.273 ± 0.004 | 0.153 ± 0.01⁎,a | 0.186 ± 0.018⁎,a |
| After 60 days | 0.205 ± 0.006⁎,b | 0.169 ± 0.008⁎,a | |
| % Change | 34.53 | −9.19 | |
Data are expressed as mean ± SEM.
n = Number of subjects or patients.
Non-identical superscripts (a, b) within the same group represent significant difference (P < 0.05), by paired t-test.
P < 0.05 with respect to control group, by unpaired t-test.
Regarding reduced glutathione (GSH) level in serum, Table 3 showed that levels of GSH were significantly lower than those of controls during the treatment period. A significant elevation (P < 0.05) in GSH level after 2 months of treatment with clopidogrel compared with baseline value had been demonstrated (0.205 ± 0.006 vs. 0.153 ± 0.01).In patients treated with placebo formula, there was no significant change in GSH level after 2 months of treatment compared with baseline value (0.169 ± 0.003 vs. 0.186 ± 0.018). In clopidogrel group, a 34.5% increase in GSH level was reported; while in placebo group, −9.19% decrease was observed.
3.3. Effect of treatment with clopidogrel on AST and ALT activities in serum
The data presented in Table 4 showed that in clopidogrel group patients there was a significant elevation (2.2%, P < 0.05) in the level of AST after 2 months of treatment with clopidogrel compared with the baseline value (23.23 ± 0.33 vs. 22.73 ± 0.42). However, the level of AST was significantly higher after treatment compared to control. In placebo group there was no significant change (P > 0.05) in the level of AST after the treatment period and levels of AST do not show significant change compared to control group at base line and after 2 months of treatment (Table 4).
Table 4.
Effect of 2 months treatment with clopidogrel and with placebo on hepatic function markers (AST and ALT) in diabetic patients taking glibenclamide.
| Control (n = 16) | Clopidogrel group (n = 22) | Placebo group (n = 20) | |
|---|---|---|---|
| AST (U/L) | |||
| Baseline | 21.37 ± 1.32 | 22.73 ± 0.42a | 22.7 ± 0.40a |
| After 60 days | 23.23 ± 0.33⁎,b | 22.75 ± 0.37a | |
| % Change | 2.2 | 0.22 | |
| ALT (U/L) | |||
| Baseline | 17.813 ± 0.42 | 18.14 ± 0.43a | 18.15 ± 0.30a |
| After 60 days | 19.27 ± 0.40b | 18.4 ± 0.36a | |
| % Change | 6.23 | 1.38 | |
Data are expressed as mean ± SEM.
n = Number of subjects or patients.
Non-identical superscripts (a, b) within the same group represent significant difference (P < 0.05), by paired t-test.
P < 0.05 with respect to control group, by unpaired t-test.
Regarding ALT, there was a significant elevation in the level of ALT in clopidogrel group after 2 months of treatment compared with the baseline value (19.27 ± 0.4 vs. 18.14 ± 0.43) The levels of ALT in both groups (clopidogrel and placebo) at base line level and after treatment were not different significantly (P > 0.05) compared to control group (Table 4).
4. Discussion
The present study investigated the effect of clopidogrel on glycemic indices in type 2 diabetic patients treated with oral hypoglycemic agent (glibenclamide). Significant reduction in FSG was reported in patients treated with clopidogrel in addition to the currently used oral hypoglycemic agent as compared to the baseline FSG level (Table 2). Significant reduction in serum insulin level and improvement of insulin sensitivity (QUICKI) was also observed in clopidogrel treated group after 2 months of treatment. These results could indicate that clopidogrel has glucose lowering effect and the FSG level in placebo treated group significantly elevated after the same course of treatment. This study also shows significant increase in insulin level and significant decrease in insulin sensitivity were also observed in placebo treated group (Table 2). Whereas there is a significant correlation between obesity and insulin resistance (Kahn and Flier, 2000) it is not yet clear how obesity leads to insulin resistance. On the other hand, growing evidences suggest that insulin sensitivity of the whole body is modulated by a large number of factors secreted by the adipose tissue, which include insulin resistance-inducing factors such as, free fatty acids, TNF-α, IL-6 and resistin, as well as insulin sensitizing factors such as adioponectin (Havel, 2004; Pittas et al., 2004). Del Aguila et al. have planned an experimental study to determine whether TNF-α decreases insulin responsiveness at the cellular level. Their study data suggested that increases in TNF-α may cause insulin resistance in skeletal muscle by inhibiting IRS-1 and IRS-2 mediated PI3 kinase activation, leading to impaired insulin-stimulated glucose uptake (Del Aguila et al., 1999). Clopidogrel is a potent oral antiplatelet agent that has the ability to suppress TNF-α production (Dunzendorfer et al., 2002; Al-Bahrani et al., 2007), and there is substantial evidence that therapy with clopidogrel leads to reduction in serum levels of inflammatory markers including TNF-α across the spectrum of atherothrombotic disease (Steinhubl et al., 2007). The mechanism of glucose lowering activity of clopidogrel is not clear but it could be explained on the basis of clopidogrel inhibitory effect on TNF-α production and this might cause improvement in insulin sensitivity, increase in glucose utilization by peripheral tissue and suppressed hepatic glucose production.
The present study clearly showed that the parameters of oxidative stress were significantly elevated in type 2 diabetic patients, represented by the increased levels of serum MDA compared to controls (Table 3). Most of clopidogrel treated patients in this study demonstrated significant reduction in the serum MDA level. In placebo treated group the serum MDA levels were significantly elevated after the same course of placebo treatment. These results suggest that clopidogrel has antioxidant effect and they are compatible with some studies shown below. In patients with symptomatic coronary artery disease, treatment with clopidogrel improved systemic endothelial function of nitric oxide bioavailability and reduced oxidative stress. Enhanced production of oxygen derived free radicals lead to impaired nitric oxide bioavailability and, therefore, reducing oxidative stress may be an important mechanism by which clopidogrel exerts its beneficial effect on nitric oxide bioavailability (Heitzer et al., 2006). There is growing evidence that excessive generation of highly reactive free radicals, largely due to hyperglycemia, causes oxidative stress, which further exacerbates the development and progression of diabetes and its complication (Johansen et al., 2005). The protective effect of clopidogrel on oxidant damage in a rat model of acute ischemia was demonstrated. It has been observed that ischemia–reperfusion injury caused by free radical production (increase MDA level with a decrease in GSH level) and pretreatment with clopidogrel prevented these changes (Kanko et al., 2005). Clopidogrel increases the perfusion of tissue by decreasing platelet and leukocyte adhesion and reducing blood viscosity (Pasqualini et al., 2002). Furthermore, platelet aggregation due to increased permeability in major organs during reperfusion was reported to be prevented by clopidogrel (Jeffrey et al., 1999), thus the inhibition of platelet aggregation by preventing endothelial and leukocyte dysfunction might one of the mechanisms of the drug to prevent the oxidative injury (Dunzendorfer et al., 2002). Moreover the active metabolite of clopidogrel has sulfhydryl group (thiol, SH group); the possibility of chemical modification of SH group has an important regulative role. It is able to connect with compounds containing sulfur to produce sulfane sulfurs. The later compounds contain a labile highly reactive sulfur atom at reduced oxidation state and they have significant antioxidant property (Iciek and Wodek, 2001). This may suggest the mechanism responsible for the antioxidant effect of clopidogrel in this study.
It is found in the present study that serum GSH level was shown to be significantly reduced in type 2 diabetic patients compared to controls (Table 3). Clopidogrel causes significant elevation in the serum GSH level after 2 months of treatment while in the placebo treated group there is no significant change in the level of GSH after the same course of placebo therapy. These results demonstrate that the drug improves the antioxidant defense system represented by elevated GSH levels and hence reduces the increased oxidative stress in diabetic patients. Although the exact mechanism of this effect is not clearly understood, the results of this study suggest the mediation of inhibited free radical production as one way behind clopidogrel antioxidant (Kanko et al., 2005).
Table 4 showed that clopidogrel treatment resulted in a significant elevation in AST after 2 months while treatment with placebo formula resulted in non-significant changes. Regarding ALT, significant elevation was observed after treatment with clopidogrel while in placebo treated group there was no significant change. Individuals with type 2 diabetes have a higher incidence of liver function test abnormalities than individuals who do not have diabetes and chronic mild elevation of transaminases is frequently found in type 2 diabetic patient (Harris, 2005). The most common cause of elevated transaminases in diabetic patients is the excess intracellular fatty acid found in insulin resistant state which is known to be directly toxic to hepatocytes. Putative mechanisms include cell membrane disruption at high concentration, mitochondrial dysfunction, toxin formation and activation and inhibition of key steps in the regulation of metabolism and other potential explanation for elevated transaminases in insulin resistant state is oxidative stress (Neuschwander-Tetri and Caldwell, 2003). In this study the baseline levels of both AST and ALT of diabetic patients groups did not differ significantly from those of control. Since clopidogrel is activated by hydrolysis in the liver to produce active and inactive metabolites, so it is necessary to observe the hepatic function during the clopidogrel treatment to detect any changes in the integrity of hepatocytes through measuring AST and ALT activities. From the above resulted results, it is found that clopidogrel caused significant elevations in the level of AST and ALT but this elevation remained within the reference limited during the treatment period.
5. Conclusion
-
1.
The adjuvant use of clopidogrel with oral hypoglycemic agents (glibenclamide) increases insulin sensitivity and improves glycemic homeostasis after short term of treatment.
-
2.
The mechanism responsible for the clopidogrel induced improvement of insulin sensitivity and glycemic control in type 2 diabetic patients could possibly be related to antioxidant activity of clopidogrel and suppression of TNF-α production, which is an important cause of insulin resistance.
Acknowledgments
The authors would like to express appreciations to Dr. Rassmyoa Hadi, Dr. Meada H. Mansour and the clinical laboratory personnel at the specialized center for Endocrinology and Diabetes for their generous help during study.
References
- Al-Bahrani A., Taha S., Shaath H. TNF-α and IL-8 in acute stroke and the modulation of these cytokines by antiplatelet agents. Curr. Neurovasc. Res. 2007;4:31–37. doi: 10.2174/156720207779940716. [DOI] [PubMed] [Google Scholar]
- American Diabetic Association Diagnosis and classification of diabetes mellitus. Diabetic Care. 2008;31:S55–S60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- Angiolillo D.J., Fernadezortiz A., Bernardo E. Clopidogrel withdrawal is associated with proinflammatory and prothrombotic effect in patient with diabetes and coronary artery disease. Diabetes. 2006;55:780–784. doi: 10.2337/diabetes.55.03.06.db05-1394. [DOI] [PubMed] [Google Scholar]
- Barham D., Trinder P. An improved colour reagent from the determination of blood glucose by the oxidative system. Analyst. 1972;97:142–145. doi: 10.1039/an9729700142. [DOI] [PubMed] [Google Scholar]
- Beuge J.A., Aust S.D. Microsomal lipid peroxidation. Meth. Enzymol. 1978;51:302–310. doi: 10.1016/s0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- Bonnefont-Rousselet D. Glucose and reactive oxygen species. Curr. Opin. Clin. Nutr. Metab. Care. 2002;5:561–568. doi: 10.1097/00075197-200209000-00016. [DOI] [PubMed] [Google Scholar]
- Cheeseman K.M., Slater T.F. An introduction of free radical biochemistry. Br. Med. Bull. 1993;49:481–493. doi: 10.1093/oxfordjournals.bmb.a072625. [DOI] [PubMed] [Google Scholar]
- Chen Y.G., Xu F., Zhang Y. Effect of aspirin plus clopidogrel on inflammatory markers in patients with NSTEACS. Chin. Med. J. 2006;119:32–36. [PubMed] [Google Scholar]
- Del Aguila L.F., Claffey K.P., Kirman J.P. TNF-α impairs insulin signaling and insulin stimulation of glucose uptake in C2C12 muscle cells. Am. J. Physiol. 1999;276:849–855. doi: 10.1152/ajpendo.1999.276.5.E849. [DOI] [PubMed] [Google Scholar]
- Dunzendorfer S., Reinisch C.M., Kaneider N.C. Inhibition of plasma-dependent monocyte chemokinesis and cytokine-triggered endothelial activation for neutrophil transmigration by administration of clopidogrel in man. Acta Med. Austriaca. 2002;29:100–106. doi: 10.1046/j.1563-2571.2002.02015.x. [DOI] [PubMed] [Google Scholar]
- Ellman G.L. Tissue sulfahydryl group. Arch. Biochem. Biophys. 1959;82:70–77. doi: 10.1016/0003-9861(59)90090-6. [DOI] [PubMed] [Google Scholar]
- Flier J.S., Kahn C.R., Roth J. Receptor, anti-receptor antibodies and mechanisms of insulin resistance. New Engl. J. Med. 1979;300:413–419. doi: 10.1056/NEJM197902223000808. [DOI] [PubMed] [Google Scholar]
- Flower M.J. Classification of diabetes. Not all hyperglycemia is the same. Clin. Diab. 2007;25:74–76. [Google Scholar]
- Harris E.H. Elevated liver function tests in type 2 diabetes. Clin. Diab. 2005;23:115–119. [Google Scholar]
- Havel P.J. Update on adipocyte hormone regulation of energy balance and carbohydrate/lipid metabolism. Diabetes. 2004;26:2442–2450. doi: 10.2337/diabetes.53.2007.s143. [DOI] [PubMed] [Google Scholar]
- Heitzer T., Rudolph V., Schwedhelm E. Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease. ATNB. 2006;26:1648–1652. doi: 10.1161/01.ATV.0000225288.74170.dc. [DOI] [PubMed] [Google Scholar]
- Iciek M., Wodek L. Biosynthesis and biological properties of compounds containing highly reactive, reduced sulfane sulfur. Pol. J. Pharmacol. 2001;53:215–225. [PubMed] [Google Scholar]
- Jeffrey T., Michael E., Garry L. The role of glutamine in skeletal muscle ischemia/reperfusion injury in the rat hind limb model. Am. J. Surg. 1999;178:147–150. doi: 10.1016/s0002-9610(99)00148-8. [DOI] [PubMed] [Google Scholar]
- Johansen J.S., Harris A.K., Rychly D.J. Oxidative stress and the use of antioxidant in diabetes: linking basic science to clinical practice. Cardiovasc. Diabetol. 2005;4:5–16. doi: 10.1186/1475-2840-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn B.B., Flier J.S. Obesity and insulin resistance. J. Clin. Invest. 2000;106:473–481. doi: 10.1172/JCI10842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanko M., Maral H., Akbas M.H. Protective effects of clopidogrel on oxidant damage in a rat model of acute ischemia. Tohoku J. Exp. Med. 2005;205:133–139. doi: 10.1620/tjem.205.133. [DOI] [PubMed] [Google Scholar]
- Katz A., Nambi S.S., Mather K., Baron A.D., Follmann D.A., Sullivan G., Quoun M.J. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J. Clin. Endocrinol. Metab. 2000;85:2402–2410. doi: 10.1210/jcem.85.7.6661. [DOI] [PubMed] [Google Scholar]
- Kowalska I. Role of adipose tissue in the development of vascular complications in type 2 DM. Diab. Res. Clin. Pract. 2007;78:S14–S22. [Google Scholar]
- Liu L., Leech J.A., Urch R.B. Invivo salicylate hydroxylation: a potential biomarker for assessing acute ozone exposure and effects in humans. Am. J. Respir. Cirt. Care Med. 1997;156:1405–1412. doi: 10.1164/ajrccm.156.5.9610105. [DOI] [PubMed] [Google Scholar]
- Mooradian A.D. Cardiovascular in type 2 DM. Arch. Intern. Med. 2003;163:33–40. doi: 10.1001/archinte.163.1.33. [DOI] [PubMed] [Google Scholar]
- Neuschwander-Tetri, Caldwell B.A. Non-alcoholic steatohepatitis: a summary of AASLD single topic conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- Pasqualini L., Proi M., Lombardini R. A human model of platelet leukocyte adhesion interaction during controlled ischemia in patients with peripheral vascular disease. J. Clin. Pathol. 2002;55:946–950. doi: 10.1136/jcp.55.12.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M., Catanae R.N., Cheema T. Increased breath biomarker of oxidative stress in DM. Clin. Chim. Acta. 2004;344:189–194. doi: 10.1016/j.cccn.2004.02.025. [DOI] [PubMed] [Google Scholar]
- Pittas A.G., Joseph N.A., Greenberg A.S. Adipocytokines and insulin resistance. J. Clin. Endocrinol. Metab. 2004;89:447–452. doi: 10.1210/jc.2003-031005. [DOI] [PubMed] [Google Scholar]
- Reitman S., Frankel S. A colorimetric method for determination of serum glutamic oxaloacetic and glutamic pyruvic transaminases. Am. J. Clin. Pathol. 1957;28:56–63. doi: 10.1093/ajcp/28.1.56. [DOI] [PubMed] [Google Scholar]
- Richter J., Murdter T.E., Heinkele G. Potent mechanism based inhibition of human CYP2B6 by clopidogrel and ticlopidine. J. Pharmacol. Exp. Ther. 2004;308:189–197. doi: 10.1124/jpet.103.056127. [DOI] [PubMed] [Google Scholar]
- Saltiel A.R., Kahn C.R. Insulin signaling and the regulation of glucose and lipid metabolism. Nature. 2001;414:799–806. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- Steinhubl S.R., Badimon J.J., Bhatt D.L. Clinical evidence for anti-inflammatory effects of antiplatelet therapy in patients with atherothrombotic disease. Vas. Med. 2007;12:113–122. doi: 10.1177/1358863X07077462. [DOI] [PubMed] [Google Scholar]
- Stumvoll M., Goldestien B., Van T. Type of 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365:9. doi: 10.1016/S0140-6736(05)61032-X. [DOI] [PubMed] [Google Scholar]
- White M.F. IRS proteins and the common path to diabetes. Am. J. Physiol. Endocrinol. Metab. 2002;283:E413–E422. doi: 10.1152/ajpendo.00514.2001. [DOI] [PubMed] [Google Scholar]


