Abstract
Purpose
Many clinical studies and systematic reviews have compared the short-term (2 year) outcomes of ACL reconstruction with hamstring and patellar tendon autograft. Few differences have been observed, with the exception of increased kneeling pain with patellar tendon grafts. The goal of this systematic review is to determine where there are differences in clinical, patient reported, or radiographic outcomes based on graft choice at a minimum of 5 years after ACL reconstruction.
Methods
A systematic review was performed to identify all prospective outcome studies comparing patellar tendon and hamstring autograft ACL reconstruction with minimum follow-up of at least five years. Seven studies were identified and meta-analysis of select data determined to be sufficiently homogenous was performed (failure and laxity).
Results
Five randomized controlled trials and two prospective cohorts comparing hamstring and patellar tendon autografts were identified. Clinical assessment [failure rate, International Knee Documentation Committee (IKDC) class, Lachman, pivot shift, and KT 1000 testing] showed no difference between grafts. Patient-reported outcomes (Lysholm, Cincinnati, and IKDC) showed no difference. Both anterior knee pain (3/3 studies) and kneeling pain (4/4 studies) were more frequent in the patellar tendon group. However, the patient-reported outcomes in these studies were not different. Radiographic evidence of osteoarthritis was inconsistent between autograft choices.
Conclusion
This Level II systematic review demonstrates no difference in major clinical results between graft types with the exception of increased anterior knee and kneeling pain. There exists a potential for increased incidence of osteoarthritis in the patellar tendon group but increased sample size is required. These longer-term outcomes are similar to results of prior systematic reviews with two-year follow-up.
Introduction
The anterior cruciate ligament (ACL) is frequently injured and its reconstruction is among the most common procedures performed by orthopaedic surgeons. The orthopaedic literature is replete with papers reporting outcomes of ACL reconstruction and univariate analyses of factors felt to influence outcome. These hypothesized factors include patient characteristics such as meniscus or articular cartilage status at the time of reconstruction, mechanism of injury, or body mass index (BMI), as well as surgical factors such as graft choice or surgical technique.
Numerous authors have investigated the impact of autograft choice on outcome after ACL reconstruction and several authors have published systematic reviews on the subject with varying results (Table 1).[16, 24] Some favor bone-patellar tendon-bone[26] and some favor hamstring tendon,[17] while the majority note strengths and weaknesses of each graft type without concluding that one is superior.[1, 3–5, 10, 23] While many of these studies focus on prospective data, they all have minimum follow-up requirements of two years or less. A systematic review of minimum five-year follow-up after ACL reconstruction has not been reported.
Table 1.
Previous Systematic Reviews
| Level of Evidence | Minimum Follow-up | Included Studies | Conclusions | Direction | ||
|---|---|---|---|---|---|---|
| Biau | 2006 | I | 1 year | 18 Prospective randomized trials |
|
Neutral |
| Forster | 2005 | I | 2 years | 6 Prospective randomized trials |
|
Neutral |
| Freedman | 2003 | IV | 2 years | BTB data from 21 studies Hamstring data from 13 studies |
|
Neutral |
| Goldblatt | 2005 | I | 2 years | 11 Prospective controlled trials |
|
Neutral |
| Herrington | 2005 | I | 1 year | 13 Prospective controlled trials |
|
Neutral |
| Prodromos | 2005 | IV | 2 years | BTB data from 32 studies Hamstring data from 24 studies |
|
Favors Hamstrings |
| Spindler | 2004 | I | 2 years | 9 Prospective controlled studies |
|
Neutral |
| Yunes | 2001 | I | 2 years | 4 Prospective controlled studies |
|
Favors BTB |
BTB = Bone-patellar tendon-bone
The last decades have seen a significant focus on evidence based medicine, with a subsequent increase in the quality of published studies.[8] The last ten years have witnessed the publication of numerous papers detailing long-term outcomes following ACL reconstruction. Numerous authors have suggested that longer-term follow-up is required for accurate assessment of results after ACL reconstruction.[7, 21, 25] The aim of this systematic review is to determine whether graft choice affects clinical, patient-reported, and radiographic outcomes after ACL reconstruction based on published prospective comparative studies with 5-year minimum follow-up. We hypothesize that no significant differences will be noted between the two graft types.
Material and Methods
A MEDLINE literature search was performed to identify all publications from January 1, 1966 through May 1, 2009 reporting long-term outcomes of ACL reconstruction. A search for articles containing the terms “reconstruction,” “follow-up,” and either “anterior cruciate” or “ACL” yielded 1381 results. The title, abstract, and full text where necessary of these publications were reviewed and studies failing to meet inclusion and exclusion criteria outlined in Table 2 except for prospective nature were excluded. Full texts of the resulting 42 articles were obtained. Subsequent review led to the exclusion of 22 studies that were retrospective in nature, two that were duplicate publications, and one study which included patients represented at longer follow-up in another included study.
Table 2.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Prospective comparative studies comparing outcomes of primary ACL reconstruction with hamstring and patellar tendon grafts (Level I and II evidence) | Retrospective comparative studies and case series (Level III and IV evidence) |
| Five-year minimum follow-up | Less than 5-year minimum follow-up |
| Reconstruction with patellar tendon or hamstring tendon autograft | Utilization of graft tissue other than patellar tendon or hamstring tendon |
| All-arthroscopic, arthroscopic-assisted, or mini-arthrotomy technique | Open ACL reconstruction |
| Report separate outcomes based on graft type | Multi-ligament knee injury other than low grade MCL injuries |
| Inclusion of skeletally immature patients | |
| Use of allograft | |
| Animal studies | |
| In vitro studies | |
| Non-English studies | |
| Reviews without original data | |
| Inclusion of revision ACL reconstructions | |
| Use of artificial ligaments |
A search of the Embase database was then performed utilizing the same search strategy. The title and abstracts of the resulting 974 studies were reviewed and 933 papers were excluded in the same manner as in the MEDLINE search. Thirty-six of the remaining 41 articles had previously been identified in the MEDLINE search. Full text of the remaining 5 articles was obtained and 4 were excluded because they were retrospective studies.
The resulting 18 prospective studies were reviewed to identify those evaluating outcome based on autograft choice (hamstring versus bone-patellar tendon-bone) and 7 studies were identified.[11, 12, 14, 15, 18, 20, 27]
Assessment of Quality of Included Studies
A Modified Coleman Methodology Score was utilized to assess the quality of included studies.[2] This scoring system awards points for study design and size, patient selection, length and completeness of follow-up, and outcomes assessment. Points are totaled to yield a maximum of 100 points (Appendix 1).
Data Extraction
A templated EBM literature review form was utilized to assist in data collection. Extracted data included study design and follow-up, patient demographics (age, sex, and body mass index), surgical and rehabilitation technique, clinical outcome assessment [International Knee Documentation Committee (IKDC) class, Lachman, pivot shift, KT 1000 testing, and range of motion], failure rate, patient reported outcomes (Lysholm, Cincinnati, IKDC, subjective anterior knee and kneeling pain) quadriceps and hamstring strength testing, and radiographic findings (IKDC[9] or Rosenberg[19] rating scales). Radiographic evidence of osteoarthritis was defined as an IKDC score of B or worse or the presence of major Rosenberg changes. Data were extracted by two authors independently and discrepancies were resolved by consensus.[6, 22]
Statistical Analysis
Heterogeneity was qualitatively assessed by comparing the study populations, interventions, and outcomes among the included studies. In addition, statistical tests of homogeneity (chi-square testing for failures and for grouped frequency distribution of instrumented laxity) were employed to determine if any individual study findings refute the null hypothesis that the findings of the individual studies are the same. If the observed variation among studies was inconsistent with this null hypothesis (P < 0.10), then heterogeneity was assumed.
A study was withdrawn from meta-analysis of a particular outcome if that outcome was not studied or not reported adequately. A Mantel-Haenszel analysis utilizing a random effects model allowed for pooling of results by graft type, while accounting for number of subjects of individual studies. In order to ensure that the findings were robust, a sensitivity analysis was performed, varying the included studies in the meta-analysis based on study methodology (randomized study design or prospective cohort) as well as on the consistent inclusion or exclusion of clinical failures in the instrumented laxity data.
Results
Study Design and Quality
The literature review described above yielded 7 prospective (level I or II) manuscripts with at least 5-year minimum follow-up. These studies include five randomized controlled trials[11, 14, 15, 20, 27] and two prospective cohort studies[12, 18] comparing outcomes of ACL reconstruction with bone-patellar tendon-bone autografts and hamstring tendon autografts.
All studies had minimum follow-up of 5 years after reconstruction. Mean follow-up ranged from 5 to 8.5 years. Clinical follow-up was performed in all 7 studies, with a mean follow-up rate of 86%, with individual papers’ follow-up rates ranging from 67% to 100%. Instruments utilized for clinical follow-up included KT-1000 (100%), range of motion (86%), subjective measures of stability (Lachman/anterior drawer) (71%), overall IKDC score (71%), and validated patient oriented outcome scores (86 %): Lysholm score (57%), subjective IKDC score (14%), and Cincinnati score (14%). Radiographic follow-up was available in 6 studies, with a mean follow-up rate of 83%, with individual papers’ follow-up rates ranging from 58% to 100%. Modified Coleman Methodology Scores for the studies ranged from 66 to 78 (Table 3).
Table 3.
Follow-up and Quality Scores
| Author | Year | Initial Cohort | Years to Clinical Follow-up Mean (range) | Final Clinical Cohort | Clinical Evaluation | Years to Radiographic Follow-up | Final Radiographic Cohort | Modified Coleman Methodology Score |
|---|---|---|---|---|---|---|---|---|
| Ibrahim | 2005 | 110 | 6.8 (5–8) | 85 (77%) | Subjective Patient Satisfaction Lysholm Score Tegner Score Lachman/Pivot shift KT-1000 Extension deficit |
6.8 (5–8) | 85 (77%) | 66 |
| Keays | 2007 | 62 | 6 | 56 (90%) | Cincinnati knee score Lachman/Pivot shift KT-1000 Extension deficit |
6 | 56 (90%) | 68 |
| Liden | 2007 | 71 | 7.2 (5.7–9.5) | 68 (96%) | IKDC Grade - overall Lysholm Score Tegner Score Lachman KT-1000 Extension deficit |
NA | NA | 70 |
| O’Neill | 2001 | 225 | 8.5 (6–11) | 225 (100%) | IKDC Grade - overall KT-1000 |
8.5 (6–11) | 225 (100%) | 76 |
| Roe | 2005 | 180 | 7 | 120 (67%) | IKDC Grade - overall Lysholm Score Lachman/Pivot shift KT-1000 Extension deficit |
7 | 104 (58%) | 78 |
| Sajovic | 2006 | 64 | 5 | 54 (85%) | IKDC Grade - overall Lysholm Score KT-1000 Extension deficit Anterior knee pain |
5 | 54 (85%) | 71 |
| Zaffagnini | 2006 | 50 | 5 | 50 (100%) | IKDC - Subjective IKDC Grade - overall Tegner Score Pivot shift/Lachman KT-1000 Extension deficit Anterior knee pain |
5 | 50 (100%) | 75 |
Patient Demographics
Mean patient age at reconstruction was 25 years. Mean patient age in the six studies reporting it ranged from 22 to 31 years. Overall, 66% of patients were male, with the percentage in the seven studies ranging from 50% to 100%. The time from injury to ACL reconstruction varied considerably between studies. Exclusion criteria among the studies varied, but all excluded knees with multiple ligament injuries other than low-grade medial collateral ligament injuries. Demographic information is detailed in Table 4.
Table 4.
Patient Demographics
| Author | Journal | Year | Initial Cohort | Patient Age Mean (range) | Percent male | Chronicity | Method of Reconstruction | Other Selection Criteria |
|---|---|---|---|---|---|---|---|---|
| Ibrahim | Arthroscopy | 2005 | 110 | 22 (17–34) | 100% | NR* | All arthroscopic Femoral tunnel drilled through tibia | |
| Keays | AJSM | 2007 | 62 | 27 (18–38) | 71% | Mean time from injury to reconstruction 3 years | All arthroscopic for hamstring, mini- arthrotomy for BTB. Femoral tunnel drilled through tibia | Multi-ligament injuries, patients over 40, acute injuries, and patients with evidence of osteoarthritis at reconstruction excluded |
| Liden | AJSM | 2007 | 71 | 28 (15–59) | 69% | Mean time from injury to reconstruction 2.8 years | All arthroscopic Femoral tunnel drilled through tibia | Multi-ligament injuries, bilateral injuries, and revision excluded |
| O’Neill | JBJS-Am | 2001 | 225 | NR | 67% | NR | 1/3 all arthroscopic and 2/3 2-incision | Multi-ligament injuries and those under age 18 excluded |
| Roe | AJSM | 2005 | 180 | 24 (13–52) | 53% | 62% reconstructed within 12 weeks of injury | All arthroscopic Femoral tunnel drilled through anteromedial portal | Patients with multi-ligament injuries, chondral injuries, meniscal pathology involving more than 2/3 of the meniscus, contralateral knee injury, or radiographic abnormality excluded |
| Sajovic | AJSM | 2006 | 64 | 25 (14–46) | 50% | Mean time from injury to reconstruction 2.0 years | All arthroscopic | Patients with multi-ligament injuries, abnormal radiographs, previous meniscal surgery, or subsequent contralateral rupture excluded |
| Zaffagnini | KSSTA | 2006 | 50** | 31 (22–49) | 62% | Mean time from injury to reconstruction 0.8 years | All arthroscopic Femoral tunnel drilled through tibia | Patients with PCL injury, meniscal or cartilage injury, non-athletes, prior knee surgery, and age over 50 were excluded |
NR = not reported
Study also included an extra-articular reconstruction group that was excluded from this analysis
Surgical and Rehabilitation Technique
All studies utilized autograft for ACL reconstruction performed using all endoscopic, arthroscopic-assisted, or two incision mini-arthrotomy techniques. Fixation of all patellar tendon grafts was with interference screw. Hamstring fixation was variable, with staple, interference screw, and endobutton techniques all utilized (Table 5). Six studies reported details of their rehabilitation protocol. Four (67%) allowed immediate full weight bearing[12, 14, 18, 20]. One author allowed immediate partial weight bearing and full weight bearing at 2 weeks[27] while one allowed full weight bearing after 2–3 days.[11] Postoperative extension bracing was utilized by 2 authors (33%) for time periods ranging from 1–3 weeks.[12, 20]
Table 5.
Surgical Technique
| Author | Year | Surgical Approach | Method of Drilling Femoral Tunnel | Proximal Fixation | Proximal Fixation | Distal Fixation | Distal Fixation |
|---|---|---|---|---|---|---|---|
| BTB* | Hamstring | BTB | Hamstring | ||||
| Ibrahim | 2005 | All endoscopic | Transtibial | Interference screw | Endobutton | Interference screw | Screw and washer or staple |
| Keays | 2007 | Mini-arthrotomy | Independent | Interference screw | Interference screw | Interference screw | Interference screw |
| Liden | 2007 | All endoscopic | Transtibial | Interference screw | Interference screw | Interference screw | Interference screw |
| O’Neill | 2001 | 2/3 Arthroscopic-assisted 2-incision, 1/3 All endoscopic | 2/3 Independent 1/3 Transtibial |
Interference screw | 2 staples | Interference screw | 2 staples |
| Roe | 2005 | All endoscopic | Transtibial | Interference screw | Interference screw | Interference screw | Interference screw |
| Sajovic | 2006 | All endoscopic | Independent | Interference screw | Interference screw | Interference screw | Interference screw |
| Zaffagnini | 2006 | All endoscopic | Transtibial | Interference screw | Endobutton | Interference screw | Interference screw |
BTB = bone-patellar tendon-bone
Clinical Outcome Assessment
Clinical outcomes of the two graft types were compared in each of the seven studies outlined above. No study showed significant differences in overall IKDC score, manual stability, KT-1000 testing, or extension deficit between the patellar tendon and hamstring groups. Data are shown in Table 7.
Table 6.
Clinical Outcome Measures
| Author Year | Clinical Failure
|
Clinical Failure
|
Overall IKDC A or B
|
Overall IKDC A or B
|
Normal Lachman
|
Normal Lachman
|
Normal Pivot
|
Normal Pivot
|
KT-1000 within 2–4 mm of contra- lateral
|
KT-1000 within 2–4 mm of contra- lateral
|
No extension deficit
|
No extension deficit
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BTB | Ham | BTB | Ham | BTB | Ham | BTB | Ham | BTB | Ham | BTB | Ham | |
|
| ||||||||||||
| Ibrahim 2005 | NR | NR | 35/40 (88 %) | 38/45 (84 %) | 35/40 (88 %) | 39/45 (87 %) | 35/40 (88 %) | 38/45 (84%) | 35/40 (88 %) | 38/45 (84 %) | 28/40 (70 %) | 37/45 (82 %) |
|
| ||||||||||||
| Keays 2007 | 0/29 (0%) | 1/27 (3.7%) | 29/29* (100 %) | 25/25* (100 %) | 29/29* (100 %) | 25/25* (100 %) | 23/27# (85 %) | 18/22# (82 %) | 29/29* (100 %) | 25/25* (100 %) | ||
|
| ||||||||||||
| Liden 2007 | 2/32 (6.2%) | 2/36 (5.6%) | 15/31* (48 %) | 17/34* (50 %) | 30/31* (97 %) | 32/34* (94 %) | NR | NR | NR | NR | 24/31* (77 %) | 27/34* (79 %) |
|
| ||||||||||||
| O’Neill 2001 | 9/150 (6.0%) | 6/75 (8.0%) | 141/150 (94 %) | 67/75 (89 %) | NR | NR | NR | NR | 121/150 (81 %) | 56/75 (75 %) | NR | NR |
|
| ||||||||||||
| Roe 2005 | 4/90 (4.4%) | 9/90 (10%) | 50/59# (85 %) | 54/61# (89 %) | 45/59# (76 %) | 50/61# (82 %) | 49/59# (83 %) | 50/61# (82 %) | 44/59# (74 %) | 49/61# (80 %) | 51/59# (86 %) | 55/61# (90 %) |
|
| ||||||||||||
| Sajovic 2006 | 1/30 (3.3%) | 1/31 (3.2%) | 25/26# (97 %) | 27/28# (97 %) | 22/26# (85 %) | 22/28# (79 %) | 21/26# (81 %) | 23/28# (83 %) | 21/26# (81 %) | 24/28# (85 %) | NR | NR |
|
| ||||||||||||
| Zaffagnini 2006 | NR | NR | 19/25 (76 %) | 18/25 (72 %) | 22/25 (88 %) | 16/25 (64 %) | 23/25 (92 %) | 18/25 (72 %) | 18/25 (72 %) | 15/25 (60 %) | 20/25 (80 %) | 18/25 (72 %) |
Clinical Failures Excluded
Clinical Failures and Contralateral Ruptures Excluded
NR = Not Reported
Table 7.
Patient-Reported Outcome Measures
| Author | Year | Patient Reported Score
|
Patient Reported Score
|
Anterior Knee Pain
|
Anterior Knee Pain
|
Kneeling Pain
|
Kneeling Pain
|
|---|---|---|---|---|---|---|---|
| BTB | Ham | BTB | Ham | BTB | Ham | ||
|
| |||||||
| Ibrahim | 2005 | Lysholm 92 | Lysholm 93 | 10/40 (25%) | 3/45 (6.6%) | NR | NR |
|
| |||||||
| Keays* | 2007 | Cincinnati 92 | Cincinnati 94 | NR | NR | NR | NR |
|
| |||||||
| Liden* | 2007 | Lysholm 91 | Lysholm 80 | NR | NR | 13/31 (42%) | 10/34 (29%) |
|
| |||||||
| O’Neill | 2001 | NR | NR | NR | NR | NR | NR |
|
| |||||||
| Roe# | 2005 | Lysholm 93 | Lysholm 93 | 24/63 (38%) | 9/64 (14%) | 34/63 (54%) | 13/64 (20%) |
|
| |||||||
| Sajovic | 2006 | Lysholm 92 | Lysholm 92 | NR | NR | 5/26 (19%) | 5/28 (17%) |
|
| |||||||
| Zaffagnini | 2006 | Subjective IKDC 82 | Subjective IKDC 76 | 9/25 (36%) | 3/25 (12%) | 18/25 (72%) | 11/25 (44%) |
Ipsilateral Ruptures Excluded
Ipsilateral and Contralateral Ruptures Excluded
NR = Not Reported
Graft failure Rate
Graft failure rate was reported in five studies, none of which demonstrated a difference in failure rate between graft types.
Patient-Reported Outcomes
Six studies utilized validated patient-reported outcome scores including Lysholm, Cincinnati, and IKDC in outcome assessment. None demonstrated significant differences between graft types. The three studies reporting anterior knee pain showed a higher incidence in the patellar tendon group (range 25–36%) than the hamstring tendon group (range 7–14%). Similarly, kneeling pain was reported in four studies with three reporting more kneeling pain in the patellar tendon group. The patient-reported outcomes in the studies that reported anterior knee and kneeling pain were not different (Table 8).
Table 8.
Radiographic Outcome Measures
| Joint | Author | Year | Follow-up (Years) | Level of Evidence | Radiographic Grading Scale | Radiographic Evidence of OA
|
Radiographic Evidence of OA
|
Significance |
|---|---|---|---|---|---|---|---|---|
| BTB Number (Percent) | Ham Number (Percent) | |||||||
|
| ||||||||
| Tibiofemoral | Ibrahim | 2005 | 6.8 | I | NR | 6/40 (15%) | 8/45 (18%) | p = 0.73 |
|
| ||||||||
| Keays | 2007 | 6 | II | NR | 18/29 (62%) | 9/27 (33%) | p = 0.02 | |
|
| ||||||||
| O’Neill | 2001 | 8.5 | I | IKDC | 14/150 (9%) | 12/75 (16%) | p = 0.2 | |
|
| ||||||||
| Roe | 2005 | 7 | II | IKDC | 24/53 (45%) | 7/51 (14%) | p = 0.002 | |
|
| ||||||||
| Sajovic | 2006 | 5 | I | IKDC | 9/26 (35%) | 4/28 (14%) | p = 0.075 | |
|
| ||||||||
| Zaffagnini | 2006 | 5 | I | Rosenberg | 0/25 (0%) | 1/25 (4%) | p = 0.9 | |
|
| ||||||||
| Patellofemoral | Ibrahim | 2005 | 6.8 | I | NR | 8/40 (20%) | 3/45 (7%) | p = 0.068 |
|
| ||||||||
| Keays | 2007 | 6 | II | NR | 12/29 (41%) | 8/27 (30%) | p = 0.2 | |
|
| ||||||||
| Roe | 2005 | 7 | II | IKDC | 8/53 (15%) | 2/51 (4%) | p = 0.053 | |
|
| ||||||||
| Sajovic | 2006 | 5 | I | IKDC | 7/26 (27 %) | 3/28 (11%) | p = 0.12 | |
|
| ||||||||
| Any# | Keays | 2007 | 6 | II | NR | 21/29 (72%) | 12/27 (44%) | p = 0.03 |
|
| ||||||||
| Roe | 2005 | 7 | II | IKDC | 28/53 (53%) | 8/51 (16%) | p < 0.001 | |
|
| ||||||||
| Sajovic | 2006 | 5 | I | IKDC | 13/26 (50%) | 5/28 (18%) | p = 0.012 | |
NR = Not Reported
Any = Evidence of osteoarthritis noted in either the patellofemoral or tibiofemoral compartments or both
Strength Testing
Isokinetic strength test results were reported in two studies.[12, 15] Keays et al noted nearly full strength of both quadriceps and hamstrings compared to the contralateral side in both groups. O’Neill noted a deficit of at least 10% of quadriceps strength in 34% of patients in the BTB groups and 13% of patients in the hamstring group. A similar deficit in hamstring strength was noted in 10% of patients in the BTB groups and 19% of patients in the hamstring group.
Radiographic Evaluation
Six of the above studies described the rate of development of radiographic evidence of osteoarthritis with a patellar tendon graft versus a hamstring graft. All six compare the rates of tibiofemoral osteoarthritis,[11, 12, 15, 18, 20, 27] four compare the rates of patellofemoral arthritis,[11, 12, 18, 20] and three present sufficient data to allow comparison of the rate of osteoarthritis in either location.[12, 18, 20]
A minority of studies (2/6) showed a significantly increased rate of tibiofemoral osteoarthritis in the patellar tendon group[12, 18] and four showed no difference in tibiofemoral osteoarthritis between groups.[11, 15, 20, 27] All four studies comparing rates of patellofemoral osteoarthritis noted higher rates of osteoarthritis in the patellar tendon group but none demonstrated a statistically significant difference.[11, 12, 18, 20] However, all three studies that allowed calculation of the rate of development of osteoarthritis in either location demonstrated a significantly increased rate in the patellar tendon group.[12, 18, 20, 27] Rates of osteoarthritis in each location by graft type in each study are shown in Table 9.
Assessment of Heterogeneity
Statistical tests of homogeneity supported the null hypothesis that the findings of these seven individual studies were the same with respect to clinical failure rate and instrumented laxity (P > 0.10). Remaining outcome measures demonstrated significant heterogeneity and were not subjected to meta-analysis.
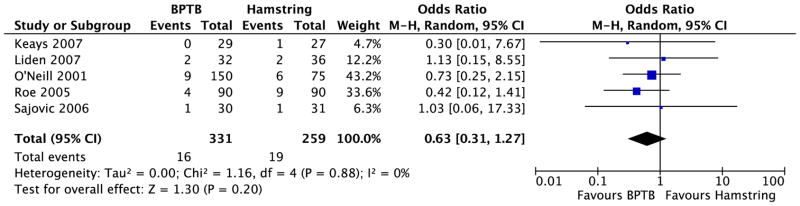
Meta-analysis of Graft Failures
Graft failures were reported in five of the seven studies identified for this review.[12, 14, 15, 18, 20] Failure was defined by clinical exam in the five studies without specific criteria reported. The clinical failures from these five studies were pooled by graft type, and the meta-analysis (Figure 1) estimates an odds ratio of 0.63 favoring bone-patellar tendon-bone [95% CI of 0.31 to 1.27, P = 0.20].
Figure 1.
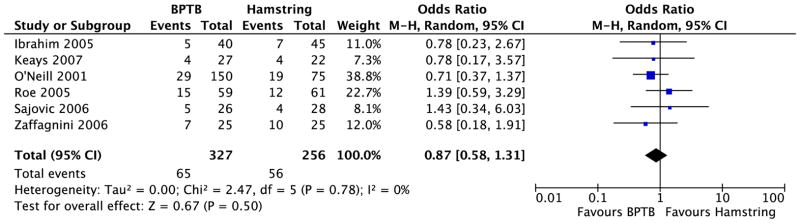
Meta-analysis of Instrumented Laxity
Six studies reported the grouped frequency distribution of instrumented laxity.[11, 12, 15, 18, 20, 27] The instrumented laxity results of these six studies were pooled by graft type, and the meta-analysis of instrumented laxity more than 5 mm (Figure 2) estimates an odds ratio of 0.87 favoring bone-patellar tendon-bone [95% CI of 0.58 to 1.31, P = 0.50]. Of note, when clinical failures are consistently included in the instrumented laxity data, the funnel plot assumes the characteristic funnel shape. In that setting, the meta-analysis of instrumented laxity more than 5 mm estimates an odds ratio of 0.78 favoring bone-patellar tendon-bone [95% CI of 0.53 to 1.16, P = 0.22].
Figure 2.
Discussion
The most important finding of our study is the absence reproducible differences in clinical assessment, instrumented laxity, or patient-reported outcomes based on autograft choice. Thus we reach a similar conclusion to those of numerous two-year systematic reviews that no reproducible difference exists between autograft choices and confirm that at minimum of five years these results are maintained. Based on this longer-term follow-up, both autografts should be considered equivalent.
Both anterior knee pain and kneeling pain were evaluated in a minority of studies but were consistently worse with bone-patellar tendon-bone grafts. However, anterior knee pain in patients in these studies was not assessed using a validating tool for assessing anterior knee pain such as the Kujala score.[13] It is interesting to note that in each study reporting increased anterior knee pain or kneeling pain in the patellar tendon group, the patient-reported outcomes and clinical assessments did not differ between groups. Further research utilizing validated measures is needed as to the cause of anterior knee pain following ACL reconstruction. Currently available data suggest that patients whose occupation, recreation, or religion requires repetitive kneeling, a hamstring graft should be considered.
The papers included in this review are inconsistent in regard to the influence of graft choice on the development of osteoarthritis. Two of the six papers strongly link the development of osteoarthritis with the use of patellar tendon grafts while the other four do not. It should be noted that the two studies which demonstrated this effect were not randomized. In both papers, consecutive cohorts are compared. It is possible that other unknown differences in the patient populations, surgical environment, or rehabilitation contributed to the increased osteoarthritis in the patellar tendon group. All papers evaluating the effect of graft choice on the development of patellofemoral osteoarthritis had a p value between 0.05 and 0.20. It is likely that these studies were underpowered to detect a difference. The three studies that allowed for comparison of rates of osteoarthritis in either location showed a statistically and clinically significant increased rate with patellar tendon grafts.
If an increased patellofemoral osteoarthritis rate with patellar tendon grafts is shown in future studies, this may represent the technique of graft harvest and suggest that extreme care be taken during harvest to avoid chondral injury. Reasons for increased tibiofemoral osteoarthritis are less clear, but may be related to the increased rate of postoperative stiffness reported by some authors utilizing patellar tendon grafts. Regardless of the etiology of the effect, it might be advisable to avoid patellar tendon grafts in patients who already exhibit early signs of osteoarthritis. Future studies with multivariable analysis are needed to identify modifiable risk factors for osteoarthritis following ACL reconstruction.
The strengths of this study are the prospective nature and relatively long-term follow-up of the papers included in the analysis. To our knowledge, no previously published systematic review of the influence of autograft choice on outcome after ACL surgery has had such rigid inclusion and exclusion criteria. The included studies are all level I or II data with at least five-year minimum follow-up and thus provide a high level of evidence for analysis for clinical decision making.
The weaknesses of this study are the heterogeneous outcomes evaluated in each study and lack of validated instruments for anterior knee or kneeling pain. However, these weaknesses do not preclude a systematic review. Further standardization of rehabilitation, utilization of a blinded clinical examiner, and use of additional validated patient-reported outcome measure would improve the strength of conclusions and meta-analysis. Similarly, there remains no universally applied, validated outcome measure for rotational stability following ACL reconstruction, forcing us to rely on the quite subjective pivot-shift examination. Additionally, this study suffers from a weakness inherent to all assessments of relatively long-term outcome data: the data presented above represents surgical instrumentation and techniques that are at least five years old and may not entirely represent current practice. Finally, the strict inclusion criteria for this review have led to the collection of data from a relatively small number of papers selected from numerous studies addressing outcome after ACL reconstruction. The findings of this study thus reflect only this relatively small amount of data.
Conclusion
Data from prospective studies with minimum five-year follow-up indicate that the choice of bone-patellar tendon-bone autograft versus hamstring autograft does not significantly influence clinical outcome at minimum five-year follow-up. Radiographic data is more inconsistent with respect to evidence of osteoarthritis following autograft ACL reconstruction. Both anterior knee pain and kneeling pain occurred more frequently in patellar tendons but the patient-reported outcomes were not different. These findings are consistent with previous two-year systematic reviews and meta-analysis which fail to consistently demonstrate the superiority of one autograft type over the other. Thus, both should be considered the current standard for ACL reconstruction.
Supplementary Material
Acknowledgments
The authors would like to thank Lynn Cain for editorial assistance.
Footnotes
Conflict of Interest Statement
The authors report no conflict of interest related to this work.
References
- 1.Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006;332:995–1001. doi: 10.1136/bmj.38784.384109.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 3.Forster MC, Forster IW. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee. 2005;12:225–230. doi: 10.1016/j.knee.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 5.Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21:791–803. [Google Scholar]
- 6.Greenhalgh T. How to Read a Paper: The Basics of Evidence Based Medicine. 2. London: BMJ Publishing Group; 2001. [Google Scholar]
- 7.Hanypsiak BT, Spindler KP, Rothrock CR, Calabrese GJ, Richmond B, Herrenbruck TM, Parker RD. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36:671–677. doi: 10.1177/0363546508315468. [DOI] [PubMed] [Google Scholar]
- 8.Hanzlik S, Mahabir RC, Baynosa RC, Khiabani KT. Levels of evidence in research published in The Journal of Bone and Joint Surgery (American Volume) over the last thirty years. J Bone Joint Surg Am. 2009;91:425–428. doi: 10.2106/JBJS.H.00108. [DOI] [PubMed] [Google Scholar]
- 9.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 10.Herrington L, Wrapson C, Matthews M, Matthews H. Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee. 2005;12:41–50. doi: 10.1016/j.knee.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412–417. doi: 10.1016/j.arthro.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007;35:729–739. doi: 10.1177/0363546506298277. [DOI] [PubMed] [Google Scholar]
- 13.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 14.Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-Year follow-up. Am J Sports Med. 2007;35:740–748. doi: 10.1177/0363546506298275. [DOI] [PubMed] [Google Scholar]
- 15.O’Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament. A follow-up report. J Bone Joint Surg Am. 2001;83-A:1329–1332. doi: 10.2106/00004623-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am. 2007;89:1542–1552. doi: 10.2106/JBJS.F.01292. [DOI] [PubMed] [Google Scholar]
- 17.Prodromos CC, Joyce BT, Shi K, Keller BL. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21:1202. doi: 10.1016/j.arthro.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 18.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337–1345. doi: 10.1177/0363546504274145. [DOI] [PubMed] [Google Scholar]
- 19.Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479–1483. [PubMed] [Google Scholar]
- 20.Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34:1933–1940. doi: 10.1177/0363546506290726. [DOI] [PubMed] [Google Scholar]
- 21.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446–452. doi: 10.1177/03635465000280040201. [DOI] [PubMed] [Google Scholar]
- 22.Spindler KP, Kuhn JE, Dunn W, Matthews CE, Harrell FE, Dittus RS. Reading and reviewing the orthopaedic literature: a systematic, evidence-based medicine approach. J Am Acad Orthop Surg. 2005;13:220–229. doi: 10.5435/00124635-200507000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 24.Vavken P, Dorotka R. A systematic review of conflicting meta-analyses in orthopaedic surgery. Clin Orthop Relat Res. 2009;467:2723–2735. doi: 10.1007/s11999-009-0765-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu WH, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30:845–850. doi: 10.1177/03635465020300061501. [DOI] [PubMed] [Google Scholar]
- 26.Yunes M, Richmond JC, Engels EA, Pinczewski LA. Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: A meta-analysis. Arthroscopy. 2001;17:248–257. doi: 10.1053/jars.2001.21242. [DOI] [PubMed] [Google Scholar]
- 27.Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060–1069. doi: 10.1007/s00167-006-0130-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


