Abstract
The CALAXO® osteoconductive interference screw was recalled in August 2007 due to reports of increased numbers of postoperative complications associated with screw swelling and prominence leading to the need for surgical debridement. This study reviews complications associated with CALAXO® screw use in a consecutive cohort of patients undergoing anterior cruciate ligament reconstruction surgery by the senior author at our institution. Over a 12 month period, 226 CALAXO® interference screws, either of 20mm length or 25mm length, were implanted in 112 patients, and postoperative complications were noted. The 25mm tibial screw was over 5 times (RR 5.2, 95% CI 1.8 to 15.3) more likely to be prominent than the 20mm screw (p-value = 0.002). Four surgical debridements were required in the 25mm tibial screw group; none were required in the 20mm group. We hypothesize that the inability to bury the longer screw length into the bone tunnel is associated with postoperative complications associated with the CALAXO® screw.
Introduction
The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments in the body and is necessary for knee stability in the pursuit of cutting and change of direction activities. In the year 2000, estimates reveal that approximately 175,000 ACL reconstructions were performed with surgical expenditure costs exceeding 2 billion dollars.(1) A portion of these costs can be attributed to graft fixation devices implanted at the time of surgery.
In August 2006, the CALAXO® 25mm length osteoconductive interference screw, composed of polylactide carbonate (PLC), was introduced. This screw became the standard fixation for an all-biologic construct in ACL reconstruction surgeries performed at our institution. Standard patellar tendon (PT) graft bone blocks were approximately 20mm in length, and per operative protocol, screws were not inserted past the bone block in an attempt to avoid potential graft laceration or intra-articular placement. Thus by definition a 25mm screw would be on average approximately 5mm proud from the final position of the bone block. Later CALAXO® 20mm length screws became available allowing further screw burial within the tibial tunnel and improved final position.
In August 2007, the CALAXO® screw was pulled from the market due to reports of increased numbers of postoperative complications associated with screw swelling and prominence. This occurred from 2 to 36 weeks after implantation often necessitating open surgical debridement. The purpose of this manuscript is to retrospectively review postoperative complications associated with use of the CALAXO® screw in a consecutive cohort of patients undergoing ACL reconstruction surgery using PT grafts and followed for at least 36 weeks postoperatively.
Methods
Through retrospective database review, we identified 113 ACL reconstructions performed at our institution by the senior author (KPS) from August 2006 to August 2007. During this time period, 226 CALAXO® interference screws were implanted in 112 consecutive patients undergoing ACL reconstruction surgery (111 unilateral, 1 bilateral). All surgeries were performed using PT grafts (79 ipsilateral autografts, 34 allografts). An arthroscopic rear-entry technique was used with femoral and tibial interference bone fixation achieved with CALAXO® screws (116 screws of 20mm length, 110 screws of 25mm length). Per operative protocol, the screws were not placed beyond PT graft bone blocks and therefore often could not be countersunk into the bone. All patients followed the same postoperative Multicenter Orthopaedic Outcomes Network (MOON) ACL reconstruction rehabilitation program and were tracked in the clinic of the senior author (KPS). All chart documented complications were reviewed with specific attention directed towards screw prominence which was defined by patient reports of a bump or mass overlying the tibial or femoral tunnels. Confidence intervals were calculated using the binomial exact method, and screw lengths were compared with Fisher’s exact test.
Results
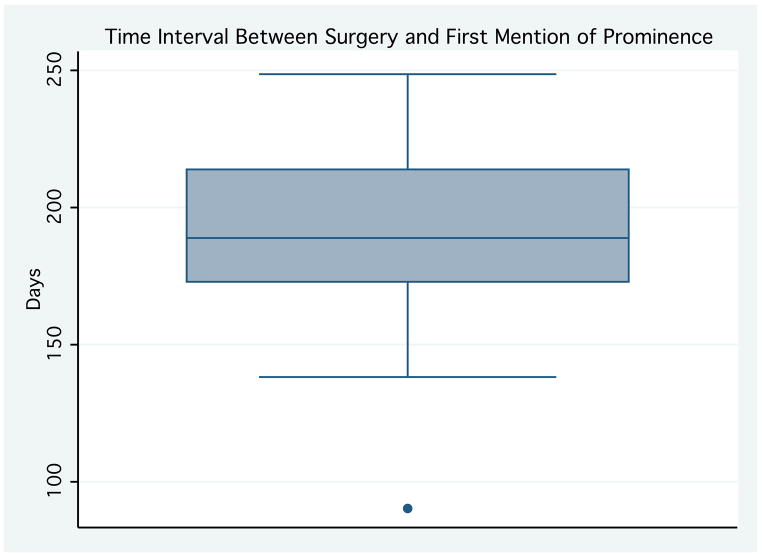
Postoperative data were available for review on all 112 patients identified at the outset of the study. Of the 226 screws implanted, 18 prominences were noted in the postoperative period (Table 1). The median time interval from surgery to first notation of screw prominence was 189 days (range 90–249 days) (Figure 1).
Table 1.
Recorded prominences are listed by screw size and time to prominence with notation of cases requiring surgical debridement.
| Screw Size (mm) | Time to Prominence (days) |
|---|---|
| TIBIAL SCREWS | |
| 9 × 25 | 238 |
| 10 × 25 | 198 |
| 7 × 20 | 215 |
| 8 × 25* | 176 |
| 9 × 25* | 181 |
| 10 × 25* | 182 |
| 8 × 25 | 233 |
| 8 × 25* | 174 |
| 7 × 20 | 195 |
| 8 × 25 | 192 |
| 7 × 25 | 139 |
| 8 × 25 | 188 |
| 9 × 25 | 250 |
| 9 × 20 | 236 |
| 9 × 20 | 173 |
| FEMORAL SCREWS | |
| 8 × 25 | 154 |
| 10 × 25 | 91 |
| 9 × 25 | 209 |
Indicates surgical debridement required
Figure 1.
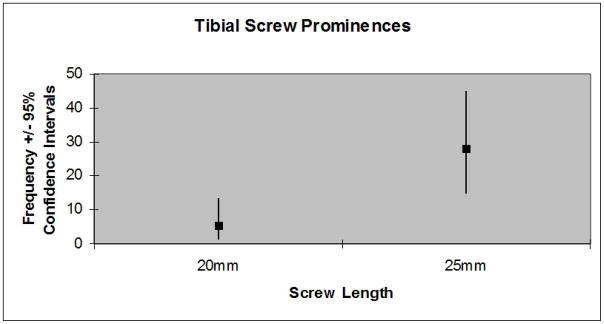
With the 20mm screws, 0/42 (0%) femoral screw prominences and 4/74 (5.4%; 95% CI 1.5–13.3%) tibial screw prominences were noted. With the 25mm screws, 3/71 (4.2%) femoral screw prominences and 11/39 (28.2%; 95% CI 15.0–44.9%) tibial screw prominences were noted (Figure 2). Four surgical debridements were required in the 25mm tibial screw group; none were required in the 20mm group. The 25mm tibial screw was over 5 times (RR 5.2, 95% CI 1.8 to 15.3) more likely to be prominent than the 20mm screw (p-value = 0.002). Further, the 20mm tibial screw never required surgical debridement. No intra-articular infections or cases of fixation failure were noted. There were approximately 2 graft failures noted which occurred as a result of reinjury following return to sports.
Figure 2.
Intraoperative findings in the cases requiring surgical debridement revealed a bulbous prominence extruding from the tunnel. The screws could not be removed with the driver but had to be extracted utilizing rongeurs. At the time of removal, the screws had a consistency of white chalk or paste.
Discussion
Interference screws, classically made of metal, are utilized to secure the bone plugs in PT grafts within the femoral and tibial tunnels. In cases of re-injury, metal interference screws can result in the presence of significant artifact during magnetic resonance imaging (MRI) sequences making accurate interpretation difficult. This has led to a shift away from the use of metal screws with an emphasis instead upon MRI compatible materials. In cases of revision surgery, removal of residual implants can necessitate a two-stage procedure requiring bone grafting of the persistent bone tunnels. Recent industry focus has been upon the development of biodegradable osteoconductive interference screws which are MRI compatible and can potentially allow for single stage revision surgery if necessary.
Several Level I or II studies exist in the literature comparing biodegradable interference screws with metallic fixation devices.(2–6) Drogset et al. and Kaeding et al. compared biodegradable screw with metallic screw fixation in PT graft ACL reconstructions and found clinically similar results in patient reported outcomes as well as instrumented laxity measurements.(2–3) Laxdal et al. also found no clinically significant differences in biodegradable screw versus metallic screw fixation in hamstring graft ACL reconstructions.(4) Buelow et al. and Ma et al. compared femoral and tibial biodegradable interference screws with femoral endobuttons and metallic tibial fixation devices and again found no clinically significant differences.(5–6)
Studies exist in the published literature analyzing degradation and tissue replacement properties of biodegradable implants.(7–8) Numerous biomaterials have been manufactured, including polyglycolic acid (PGA), poly-L-lactic acid (PLLA), and poly-D,L-lactide-co-glycolide (PDLG), each of which have been shown to degrade over time but exhibit poor restoration of trabecular bone. This lack of bone replacement can leave behind cavities complicating revision procedures. Numerous reviews and case reports have been published describing local foreign body reactions to biodegradable implants ranging from painless papules to draining sinuses to extensive osteolytic lesions.(9–14) Although effective clinically, these biodegradable implants are not ideal and do result in postoperative complications. The CALAXO® screw, utilizing PLC, attempts to combine biodegradable properties of PDLG with calcium carbonate, an osteoconductive agent, in an attempt to stimulate ingrowth of trabecular bone. This combination has been compared with PLLA in an ovine model resulting in similar fixation strength. However, the PLC resulted in complete resorption with replacement by trabecular bone within as little as 12 months following surgery.(15)
Post-market surveillance of the CALAXO® screw reveals similar complication rates as compared to previously utilized biomaterials. Although the majority of patients have excellent clinical outcomes, screw-related complications have been reported leading to recall and removal of the implant from clinical use.(16) In our series of patients, no graft failures as a result of screw complications were noted. The prominence incidence of 5.4% associated with the 20mm screw length is comparable to previously reported adverse events with other biomaterials.(10) The prominence incidence of 28.2% associated with the 25mm length tibial screw is likely due to a combination of biomaterial degradation properties and surgical protocol. With our operative technique, the screws were not placed beyond the bone block to avoid potential graft laceration and maximize the bone-screw interface for fixation. Although this technique was followed regardless of screw length, the 25mm screw was over 5 times more likely to be prominent than the 20mm screw. This finding correlates with previously published material showing larger implant surface area as a risk factor for adverse tissue responses.(10)
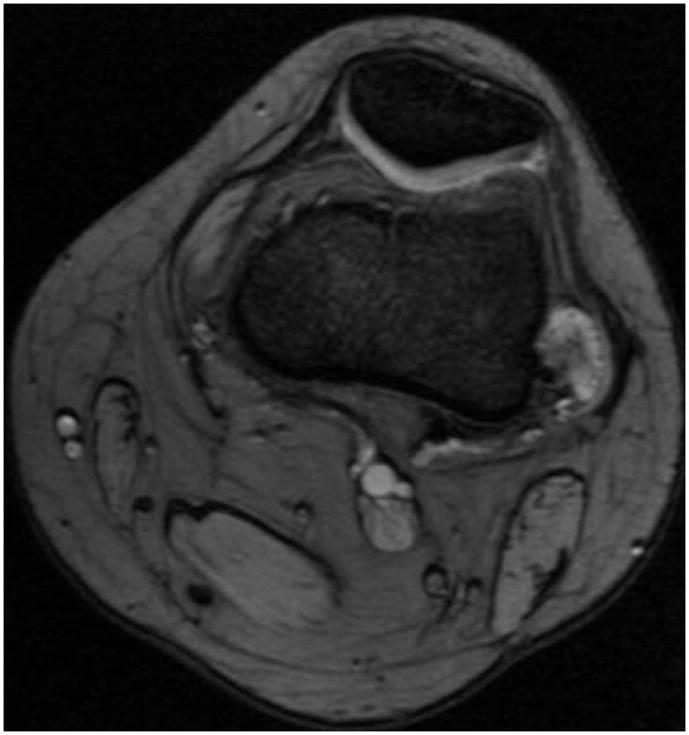
MRI follow-up illustrates the underlying clinical scenario. In cases in which the PT graft length permitted, the screw was countersunk into cortical bone. Imaging of the distal femur in the postoperative setting reveals partial screw resorption without evidence of protrusion beyond the lateral cortical bone margin (Figure 3A–B). In cases in which the screw could not be countersunk, postoperative imaging reveals partial resorption with an encapsulated protrusion beyond the cortical bone with resulting palpable prominence (Figure 4A–B).
Figure 3.
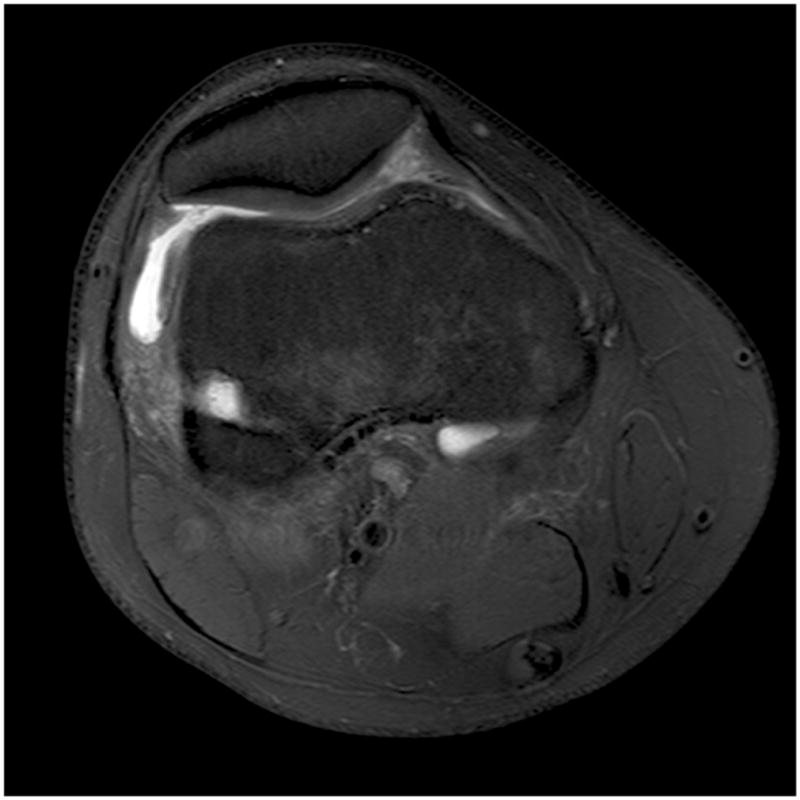

Figure 4.
Conclusions
In this cohort of patients, more postoperative screw-related complications were associated with use of the 25mm screw than with the 20mm screw. The inability to bury the longer screw length into bone combined with screw degradation properties might play a role in the postoperative complications associated with use of the CALAXO® screw.
References
- 1.Gottlob CA, Baker CL, Jr, Pellissier JM, et al. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. [PubMed] [Google Scholar]
- 2.Drogset JO, Grøntvedt T, Tegnander A. Endoscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws: a prospective randomized study of the clinical outcome. Am J Sports Med. 2005;33:1160–1165. doi: 10.1177/0363546504272264. [DOI] [PubMed] [Google Scholar]
- 3.Kaeding C, Farr J, Kavanaugh T, Pedroza A. A prospective randomized comparison of bioabsorbable and titanium anterior cruciate ligament interference screws. Arthroscopy. 2005;21:147–151. doi: 10.1016/j.arthro.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 4.Laxdal G, Kartus J, Eriksson BI, et al. Biodegradable and metallic interference screws in anterior cruciate ligament reconstruction surgery using hamstring tendon grafts: prospective randomized study of radiographic results and clinical outcome. Am J Sports Med. 2006;34:1574–1580. doi: 10.1177/0363546506288014. [DOI] [PubMed] [Google Scholar]
- 5.Buelow JU, Siebold R, Ellermann A. A prospective evaluation of tunnel enlargement in anterior cruciate ligament reconstruction with hamstrings: extracortical versus anatomical fixation. Knee Surg Sports Traumatol Arthrosc. 2002;10:80–85. doi: 10.1007/s00167-001-0267-6. [DOI] [PubMed] [Google Scholar]
- 6.Ma CB, Francis K, Towers J, et al. Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy. 2004;20:122–128. doi: 10.1016/j.arthro.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Böstman OM, Laitinen OM, Tynninen O, et al. Tissue restoration after resorption of polyglycolide and poly-laevo-lactic acid screws. J Bone Joint Surg Br. 2005;87:1575–1580. doi: 10.1302/0301-620X.87B11.16520. [DOI] [PubMed] [Google Scholar]
- 8.Pihlajamäki H, Böstman O, Tynninen O, et al. Long-term tissue response to bioabsorbable poly-L-lactide and metallic screws: an experimental study. Bone. 2006;39:932–937. doi: 10.1016/j.bone.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 9.Böstman O, Pihlajamäki H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials. 2000;21:2615–2621. doi: 10.1016/s0142-9612(00)00129-0. [DOI] [PubMed] [Google Scholar]
- 10.Böstman OM, Pihlajamäki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res. 2000;372:216–227. [PubMed] [Google Scholar]
- 11.Böstman OM, Pihlajamäki HK. Late foreign-body reaction to an intraosseous bioabsorbable polylactic acid screw. A case report. J Bone Joint Surg Am. 1998;80:1791–1794. doi: 10.2106/00004623-199812000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Busfield BT, Anderson LJ. Sterile pretibial abscess after anterior cruciate reconstruction from bioabsorbable interference screws: a report of 2 cases. Arthroscopy. 2007;23:911.e1–4. doi: 10.1016/j.arthro.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 13.Martinek V, Friederich NF. Tibial and pretibial cyst formation after anterior cruciate ligament reconstruction with bioabsorbable interference screw fixation. Arthroscopy. 1999;15:317–320. doi: 10.1016/s0749-8063(99)70042-3. [DOI] [PubMed] [Google Scholar]
- 14.Walton M, Cotton NJ. Long-term in vivo degradation of poly-L-lactide (PLLA) in bone. J Biomater Appl. 2007;21:395–411. doi: 10.1177/0885328206065125. [DOI] [PubMed] [Google Scholar]
- 15.Walsh WR, Cotton NJ, Stephens P, et al. Comparison of poly-L-lactide and polylactide carbonate interference screws in an ovine anterior cruciate ligament reconstruction model. Arthroscopy. 2007;23:757–765. doi: 10.1016/j.arthro.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Dujardin J, Vandenneucker H, Bellemans J. Tibial cyst and intra-articular granuloma formation after anterior cruciate ligament reconstruction using polylactide carbonate osteoconductive interference screws. Arthroscopy. 2008;24:238–242. doi: 10.1016/j.arthro.2007.11.009. [DOI] [PubMed] [Google Scholar]