Abstract
Background
We hypothesize that one-stage Integra skin coverage is an effective treatment modality for the treatment of fingertip defects.
Methods
Nine patients who sustained fingertip injuries were treated with one-stage Integra coverage. In all cases, Integra was placed directly on bone. Static two-point discrimination and the Semmes–Weinstein Monofilament Test (SWMFT) were used to determine the sensations of the affected and opposite unaffected digit. The QuickDASH, Cold Intolerance Symptom Severity (CISS), visual analog scale (VAS), and a 0–10-point pain scale were administered to assess patient function, satisfaction, and pain levels.
Results
The mean age was 53.1 years (39–61). There were 8 males and 1 female. The average area covered was 2.3 cm2 (1.0–3.2). The mean follow-up duration was 16 months (8–46). The median QuickDASH, CISS score, VAS patient satisfaction, and 0–10 pain score were 9.1 (2.3–40.9), 18 (4–30), 10 (most satisfied) (7–10), and 0 (0–3), respectively. Five patients were evaluated for their digital sensory perception. The mean static two-point discrimination was 9.6 mm for the affected digit and 4.6 mm for the opposite unaffected digit. The median SWMFT was 4.31 for the affected digit and 3.61 for the opposite unaffected digit.
Conclusion
For small soft tissue and bone defects involving the fingertip, the use of Integra without further skin grafting appears to be effective, avoids the morbidity of the donor site, and avoids a second surgery. Despite mild sensory deficits, patients were satisfied with the results and fully functional during short-term follow-up.
Keywords: Integra, Fingertip, Hand, Tissue reconstruction
Introduction
The treatment of hand trauma often draws on the knowledge of multiple surgical principles, including neurovascular repair, tendon repair, fracture fixation, and wound coverage. Integra® Bilayer Matrix Wound Dressing (BMWD) (Integra Life Sciences, Plainsboro, NJ, USA) is occasionally used in wound coverage. It consists of an acellular dermal matrix composed of bovine collagen that is covered by a layer of silicon. It is designed to act as a skin regeneration scaffold that allows the host’s cells to grow into the dermal template. Although it was initially approved by the Food and Drug Administration to treat burn injuries [4], its indications continue to expand due to numerous accounts of desirable clinical and histologic outcomes [2–5, 7, 11–13, 17, 19, 20]. Currently, its use spans multiple areas of reconstructive surgery, including soft tissue coverage following tumor excision [2–5, 7, 11–13, 17], soft tissue coverage following the repair of congenital defects [11], and traumatic loss of soft tissue [3, 12, 19, 20].
The standard method of Integra use involves two stages. It begins with initial wound coverage with the dermal matrix and is followed a few weeks later by the removal of the silicon layer and coverage with an autologous split or full thickness skin graft.
Fingertip injuries present a subset of injuries that are typically complicated by nail bed, pulp, and bone defects. We set out to investigate the effectiveness of one-stage reconstruction for fingertip injuries using Integra BMWD.
Materials and Methods
This study was approved by our institutional review board and was conducted accordingly under its protocol and guidelines. The study was a retrospective case series of adult patients who underwent skin substitute grafting with Integra following injuries to their fingertips. Outcomes were prospectively obtained either by office-based evaluations or mailed questionnaires. The fingertip was defined as the area distal to the insertion of the flexor digitorum profundus or the flexor pollicis longus and included the nail apparatus and the finger pulp (Figs. 1 and 2). Between 1 March 2007 and 1 November 2011, patients were identified from the medical records based on the current procedural codes 15170 (acellular dermal replacement, trunk, arms or legs; first 100 cm2 or less) or 15175 (acellular dermal replacement face, scalp, eyelids, mouth, neck, ears, orbits, genitalia, hand, feet, or multiple digits; first 100 cm2 or less) or by manually scanning our patient database using a keyword search, with the keyword being “Integra.” The inclusion criteria were (1) fingertip injuries and (2) a minimum time of 6 months between the surgery and the date of the research query. Patients who had complex lacerations that included a fingertip injury as well as nerve or tendon injury were included. The exclusion criteria were (1) patients younger than 18 years of age, (2) patients who underwent BMWD placement followed by split or full thickness skin grafting, and (3) patients who had mental deficiencies.
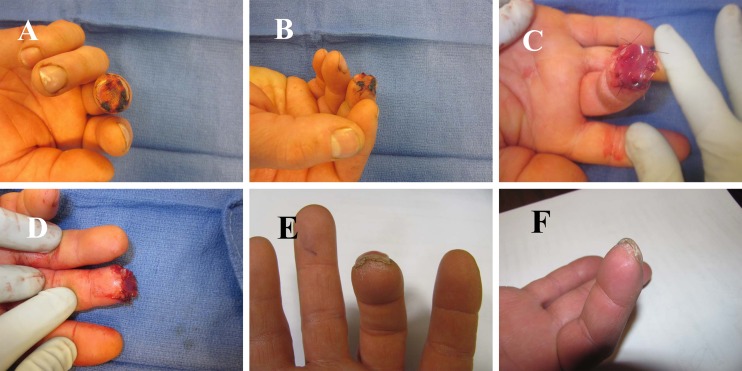
Fig. 1.
Patient #1: a middle fingertip transverse amputation with exposed bone; b oblique view of the injury; c, d Integra BMWD applied to the injury site and sutured in place with 5–0 chromic sutures; e, f 9 months following treatment, the patient demonstrates complete healing of the fingertip, with some regrowth of the fingerprint at the Integra site
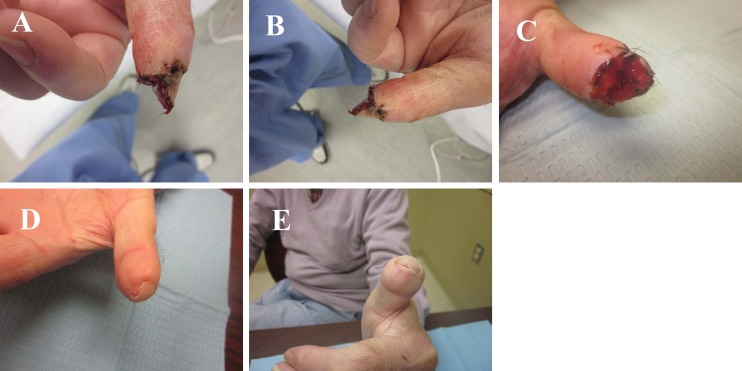
Fig. 2.
Patient #6: a, b lateral photographs demonstrating the extent of the fingertip defect after debridement of an infection; c Integra BMWD applied to the injury site and sutured in place with 5–0 chromic sutures; d, e 18 months following treatment, the fingertip is well healed; however, a hook nail deformity has developed
Nine patients (8 males and 1 female) were available for follow-up, and all patients replied to the study questionnaires, while 5 agreed to return for a physical examination. The mean age of the 9 patients was 53.1 years (39–61). Patient demographics and characteristics are presented in Table 1. Patients 4, 5, and 8 were smokers at the time of injury. No patients were diabetic. The mean follow-up duration was 16 months (8–46). Five out of 9 patients sustained fingertip amputations: 3 transverse and 2 volar oblique. Two patients sustained open distal phalangeal fracture with soft tissue loss (1 with concomitant flexor pollicis longus maceration, digital artery, and nerve injury), 1 patient sustained a fingertip degloving injury, and 1 patient sustained a pulp infection.
Table 1.
Patient demographics and characteristics
| Patient | Gender | Age (years) | Side and finger | Area grafted (cm2) | Injury mechanism | Concomitant procedures | Occupation | Complications | Follow-up duration (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 51 | Right long | 1.5 | Machine fan | None | Maintenance mechanic | None | 9 |
| 2 | Male | 39 | Right long | 1.0 | Crush injury, subsequent infection | I & D | Project manager | None | 10 |
| 3 | Male | 48 | Left thumb | 2.3 | Table saw | Repair of FPL, ulnar digital nerve | IT consultant | None | 8 |
| 4 | Male | 47 | Right long | 1.5 | Crush injury | None | Foreman laborer | None | 16 |
| 5 | Male | 61 | Left thumb | 3.0 | Table saw | Revision amputation | Electrician | None | 49 |
| 6 | Malea | 75 | Left thumb | 1.6 | Table saw, subsequent infection | None | Retired | Infection requiring I & D and IV Abx; hook nail | 18 |
| 7 | Male | 60 | Right long | 3.2 | Crush injury | Excisional debridement of open fracture | Press operator | None | 13 |
| 8 | Male | 56 | Left small | 3.2 | Fingertip infection | I & D | Plumber | None | 10 |
| 9 | Female | 41 | Left thumb | 3.2 | MVA trauma | None | Office-based work | None | 13 |
| Mean | 53.1 | 2.3 | 16 |
I & D irrigation and debridement, FPL flexor pollicis longus, IV Abx intravenous antibiotics, MVA motor vehicle accident
aUnderwent a stacking procedure
One-stage reconstruction was selected as the definitive form of treatment when the patient preferred a prompt return to activities of daily living, without the need for a secondary procedure. In addition, if a patient had significant medical comorbidities (patient #6), with pre-existing microvascular disease, it was deemed prudent to avoid flap coverage, since there was a higher risk of flap failure, and general anesthesia would have placed the patient at increased cardiac risk. Furthermore, when the distal phalangeal bone was exposed, we preferred not to shorten the bone any further in order to minimize the risk of a hook nail deformity.
The patients were surgically treated by 1 of 4 hand surgeons, under local anesthesia with monitored anesthesia care or general anesthesia when a more extensive procedure was planned. After debridement of nonviable skin, subcutaneous tissue and bone, and irrigation with antibiotic-impregnated saline, a piece of Integra was fashioned to the appropriate size and shape of the defect and secured with either 5–0 chromic sutures or 4–0 nylon sutures. At times, the Integra was pie-crusted to allow fluid egress. In all cases, the Integra was placed directly on bone. Xeroform Petrolatum Gauze (Covidien, Mansfield, MA, USA) was placed directly on the Integra, followed by a sterile dressing. At the first follow-up appointment 1 week postoperatively, the dressing was taken off. Nylon sutures were removed 10 days postoperatively, while chromic sutures were allowed to resorb. The silicon layer was allowed to fall off or was removed 3 to 4 weeks after surgery. Re-epithelialization of the defects occurred between 3 and 4 weeks, and there were no restrictions during this time period. The approximate area of the Integra graft was retrospectively recorded based on the medical record when available or the patients’ accounts. The average area of the covered defect was 2.3 cm2 (1.0–3.2). As of December 2012, a 2 × 2-in.2 sheet of Integra costs $1,978.
For patients who returned to the clinic for the purpose of the research study, fingertip sensations were assessed using both the Semmes–Weinstein Monofilament Test (Sammons Preston, Cedarburg, WI, USA) and a two-point static discrimination test using a Disk-Criminator, and then compared to the contralateral digit. Patient function was assessed using the Quick Disabilities of the Arm Shoulder and Hand survey (QuickDASH). The Cold Intolerance Symptoms Severity (CISS) score was used to assess cold intolerance. Pain was assessed using the 0–10-point ordinal pain scale (0 = no pain and 10 = worst pain possible). Patient satisfaction with the treatment was assessed using the visual analog scale (VAS).
A paired t test was used to compare numerical data for 2 groups. The Wilcoxon signed ranks test was used to compare ordinal data. p values less than 0.05 were considered statistically significant.
Results
The mean static two-point discrimination of the affected finger was 9.6 mm, while it was 4.6 mm for the opposite unaffected finger (p = 0.024). The median SW of the affected finger was 4.31, while it was 3.61 for the opposite unaffected digit (p = 0.125; Table 2). One patient developed an early infection, followed by a hook nail deformity 18 months after treatment. There were no other complications. Patient-rated outcomes were available for all 9 patients. The median QuickDASH, CISS score, VAS patient satisfaction, and 0–10 pain score were 9.1 (2.3–40.9), 18 (4–30), 10 (most satisfied) (7–10), and 0 (0–3), respectively, and are presented in Table 3.
Table 2.
Patient-rated outcomes at final follow-up and worker’s compensation status
| Patient | 0–10 pain score | Satisfaction VAS | QDASH | CISS | Workman’s compensation claim |
|---|---|---|---|---|---|
| 1 | 0 | 10 | 4.5 | 18 | Yes |
| 2 | 0 | 10 | 18.2 | 23 | No |
| 3 | 0 | 10 | 2.3 | 4 | No |
| 4 | 1 | 10 | 18.2 | 16 | Yes |
| 5 | 0 | 10 | 25.0 | 30 | Yes |
| 6 | 0 | 9 | 9.1 | 14 | No |
| 7 | 0 | 7 | 9.1 | 18 | No |
| 8 | 2 | 10 | 2.3 | 18 | Yes |
| 9 | 3 | 10 | 40.9 | 22 | No |
| Median | 0 | 10 | 9.1 | 18 |
Table 3.
Sensory findings of patients treated with Integra coverage
| 2-Point static discrimination (mm) | Semmes–Weinstein monofilament test | ||||||
|---|---|---|---|---|---|---|---|
| Patient | Affected digit | Unaffected, opposite digit | p | Patient | Affected digit | Unaffected, opposite digit | p |
| 1 | 11 | 4 | 0.024 | 1 | 4.31 | 2.83 | 0.125 |
| 2 | 11 | 3 | 2 | 4.31 | 2.83 | ||
| 3 | 10 | 4 | 3 | 4.31 | 3.61 | ||
| 4 | 4 | 4 | 4 | 3.61 | 3.61 | ||
| 5 | 12 | 8 | 5 | 3.84 | 3.61 | ||
| Mean | 9.6 | 4.6 | Median | 4.31 | 3.61 | ||
Discussion
The purpose of this study was to determine the effectiveness of one-stage Integra coverage for fingertip defects. Numerous studies have analyzed the utility of Integra for the reconstruction of hand and finger injuries. To date, all have employed two-stage reconstructive procedures, which have consisted of an initial procedure to place the Integra, followed several weeks later by autologous skin grafting. The results have been promising and consistent.
Taras et al. used two-stage grafting to reconstruct digital injuries with exposed bone, joint, tendon, or hardware in 21 digits [19]. The area of Integra application ranged from 1 to 12 cm2, for the largest single site. Twenty of 21 digits demonstrated complete incorporation of the dermal matrix, and following autografting, 16 of 20 digits demonstrated complete incorporation. Similarly, using two-stage reconstruction, Weigert et al. treated 15 patients with exposed tendon or bone hand wounds and followed them up for at least 10 months [20]. The area of the exposed structures ranged from 0.5 to 9.1 cm2. They reported that the use of Integra achieved durable, functional, and aesthetic coverage in 13 of 15 patients. Carothers et al. also reported staged stacking of Integra for the treatment of a large soft tissue defect in the palm of a patient who underwent wide excision of an acral myxoinflammatory fibroblastic sarcoma [5]. They reported placement of the dermal matrix directly on the median nerve and flexor tendons and noted graft incorporation and excellent functional recovery without the development of tendon adhesions.
One-stage reconstruction with Integra is the same as healing by secondary intention since the healing process relies on both wound contraction and re-epithelialization. Burd and Wong used one-stage reconstruction in 10 patients who underwent excision of cutaneous head and neck lesions [4]. The largest lesion that was excised was 2.9 cm × 2.0 cm. They reported that all wounds were fully healed within 6 weeks. In our series of patients, the area that was grafted was rather small, averaging 2.2 cm2, and so it is not surprising that the fingertips healed. The inherent ability of the skin to regenerate and epithelialize is an attribute that could be exploited to treat small fingertip injuries with one-stage reconstruction, in select cases. It avoids a second surgery and decreases donor site morbidity.
Integra is more expensive than zinc or primary wound healing, but it potentially accelerates wound recovery as it provides a barrier to the external environment and may therefore minimize infection. Historical results indicate that conservative treatment with dressing changes yields acceptable outcomes [8, 9, 18], but we postulate that the matrix allows for the host’s cell to create or produce a more “bulky” or “full” subdermal bed upon which the skin may epithelialize. Further, some would hesitate to treat open wounds with exposed bone with conservative measures and would opt for revision amputation or flap coverage. Since one could place Integra directly on bone, it may obviate the need for revision amputation and further shortening of the phalanx.
It is important to note that flap reconstruction offers an alternative option for the treatment of fingertip injuries. Several variants of flap coverage have been described including cross finger [6], thenar [15], and pedicle flaps [14]. These techniques are technically more challenging than one-stage placement of Integra and, in the case of thenar and cross finger flaps, require a secondary procedure. It is unclear if flap coverage will result in superior sensory outcomes compared to one-stage Integra reconstruction, since no studies have directly compared these 2 treatment modalities. When analyzing the outcomes of our patients, all were fully functional and satisfied with their treatment despite mild sensory deficits (Tables 2 and 3). With time, the sensory deficits in our patients may or may not improve. Histological studies have revealed that peripheral nerves do in fact grow into Integra following two-stage reconstructive procedures [1, 13]. At a mean follow-up duration of 47 months, Moiemen et al. were able to identify nerve fiber regeneration in the lower reticular dermis of roughly half the patients that they studied [13].
To assess cold intolerance, we utilized the CISS questionnaire, which has previously been validated [10, 16]. In our series, although some patients did complain of cold sensitivity, none surpassed the suggested cutoff score of 30 for a normal population, which suggests that the symptoms experienced were not severe enough to significantly impact their lives (Table 3).
The limitations of this study include the small number of patients, but the results seem to be highly consistent. The retrospective methodology exposed our patients at times to recall bias when reporting the size of their initial defect, potentially underestimating, or overestimating the true size of the lesion. Also, our patient population may not be representative of the general population because a high proportion were laborers with little interest in cosmetic appearance and probably a high pain threshold. It is also possible that only the patients satisfied with the treatment returned for evaluation, resulting in selection bias.
Overall, one-stage reconstruction is a technically simple procedure and appears to be a safe and effective form of treatment for select injuries, as it limits donor site morbidity and the need for a second surgery. A comparative cost–benefit analysis may be useful to further define the utility of Integra in one-stage reconstructive procedures for fingertip defects.
Acknowledgments
We would like to thank Mrs. Mary Goff for her assistance with data acquisition. Funding was received from the Hand Rehabilitation Foundation.
Conflict of interest
None of the authors have any conflicts of interest to declare.
References
- 1.Anderson JR, Fear MW, Phillips JK, Dawson LF, Wallace H, Wood FM, et al. A preliminary investigation of the reinnervation and return of sensory function in burn patients treated with INTEGRA®. Burns. 2011;37:1101–1108. doi: 10.1016/j.burns.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Askari M, Cohen MJ, Grossman PH, Kulber DA. The use of acellular dermal matrix in release of burn contracture scars in the hand. Plast Reconstr Surg. 2011;127:1593–1599. doi: 10.1097/PRS.0b013e31820a6511. [DOI] [PubMed] [Google Scholar]
- 3.Azzena B, Amabile A, Tiengo C. Use of acellular dermal regeneration template in a complete finger degloving injury: case report. J Hand Surg. 2010;35A:2057–2060. doi: 10.1016/j.jhsa.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Burd A, Wong PS. One-stage Integra reconstruction in head and neck defects. J Plast Reconstr Aesthet Surg. 2010;63:404–409. doi: 10.1016/j.bjps.2008.11.105. [DOI] [PubMed] [Google Scholar]
- 5.Carothers JT, Brigman BE, Lawson RD, Rizzo M. Stacking of a dermal regeneration template for reconstruction of a soft-tissue defect after tumor excision from the palm of the hand: a case report. J Hand Surg. 2005;30A:1322–1326. doi: 10.1016/j.jhsa.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Cohen BE, Cronin ED. An innervated cross-finger flap for fingertip reconstruction. Plast Reconstr Surg. 1983;72:688–697. doi: 10.1097/00006534-198311000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Cuadra A, Correa G, Roa R, Pineros JL, Norambuena H, Searle S, et al. Functional results of burned hands treated with Integra®. J Plast Reconstr Aesthet Surg. 2012;65:228–234. doi: 10.1016/j.bjps.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Holm A, Zachariae L. Fingertip lesions. An evaluation of conservative treatment versus free skin grafting. Acta Orthop Scand. 1974;45:382–392. doi: 10.3109/17453677408989160. [DOI] [PubMed] [Google Scholar]
- 9.Ipsen T, Frandsen PA, Barfred T. Conservative treatment of fingertip injuries. Injury. 1987;18:203–205. doi: 10.1016/0020-1383(87)90138-0. [DOI] [PubMed] [Google Scholar]
- 10.Irwin MS, Gilbert SE, Terenghi G, Smith RW, Green CJ. Cold intolerance following peripheral nerve injury. Natural history and factors predicting severity of symptoms. J Hand Surg. 1997;22B:308–316. doi: 10.1016/s0266-7681(97)80392-0. [DOI] [PubMed] [Google Scholar]
- 11.Jung JJ, Woo AS, Borschel GH. The use of Integra® bilaminar dermal regeneration template in apert syndactyly reconstruction: a novel alternative to simplify care and improve outcomes. J Plast Reconstr Aesthet Surg. 2012;65:118–121. doi: 10.1016/j.bjps.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 12.Katrana F, Kostopoulos E, Delia G, Lunel GG, Casoli V. Reanimation of thumb extension after upper extremity degloving injury treated with Integra. J Hand Surg. 2008;33E:800–802. doi: 10.1177/1753193408096021. [DOI] [PubMed] [Google Scholar]
- 13.Moiemen N, Yarrow J, Hodgson E, Constantinides J, Chipp E, Oakley H, et al. Long-term clinical and histological analysis of Integra dermal regeneration template. Plast Reconstr Surg. 2011;127:1149–1154. doi: 10.1097/PRS.0b013e31820436e3. [DOI] [PubMed] [Google Scholar]
- 14.Ni F, Appleton SE, Chen B, Wang B. Aesthetic and functional reconstruction of fingertip and pulp defects with pivot flaps. J Hand Surg Am. 2012;37:1806–1811. doi: 10.1016/j.jhsa.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Rinker B. Fingertip reconstruction with the laterally based thenar flap: indications and long-term functional results. Hand. 2006;1:2–8. doi: 10.1007/s11552-006-0001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruijs AC, Jaquet JB, Daanen HA, Hovius SE. Cold intolerance of the hand measured by the CISS questionnaire in a normative study population. J Hand Surg. 2006;31B:533–536. doi: 10.1016/j.jhsb.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Smock ED, Barabas AG, Geh JL. Reconstruction of a thumb defect with Integra following wide local excision of a subungual melanoma. J Plast Reconstr Aesthet Surg. 2010;63:e36–e37. doi: 10.1016/j.bjps.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Söderberg T, Nyström A, Hallmans G, Hultén J. Treatment of fingertip amputations with bone exposure. A comparative study between surgical and conservative treatment methods. Scand J Plast Reconstr Surg. 1983;17:147–152. doi: 10.3109/02844318309013111. [DOI] [PubMed] [Google Scholar]
- 19.Taras JS, Sapienza A, Roach JB, Taras JP. Acellular dermal regeneration template for soft tissue reconstruction of the digits. J Hand Surg. 2010;35A:415–421. doi: 10.1016/j.jhsa.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Weigert R, Choughri H, Casoli V. Management of severe hand wounds with Integra® dermal regeneration template. J Hand Surg. 2011;36E:185–193. doi: 10.1177/1753193410387329. [DOI] [PubMed] [Google Scholar]