Abstract
Background
Intramedullary (IM) fixation has been described as a reliable method of treatment for certain fracture patterns but has not been widely adopted into practice. The purpose of this study was to evaluate the literature comparing IM fixation to other forms of treatment for metacarpal fractures.
Methods
A systematic review was performed to identify studies investigating the treatment of metacarpal fractures using IM fixation. Inclusion and exclusion criteria were predetermined. Two reviewers independently identified appropriate articles for review based on the criteria. Primary outcome measures were range of motion (ROM) (Styf et al., Rev Chir Orthop Reparatrice Appar Mot 74(Suppl 2):268–270, 2008) and complications. Secondary outcomes included loss of reduction, grip strength, Disabilities of arm, shoulder and hand (DASH) scores, radiographic measures and pain scores.
Results
Eight studies were eligible for review. Studies were of level II–IV evidence, and captured a total of 435 patients. The ROM post-operatively was found to be greater in the IM group in half of the studies. IM fixation trended toward higher complication rates in one study, but no differences were statistically significant. IM fixation fared similarly or superiorly to its competitor in each of the secondary outcomes. A formal meta-regression analysis was not possible given the heterogeneity of studies.
Conclusions
IM fixation may have a role in the treatment of certain metacarpal fractures. No conclusive recommendations can be made based on the available studies included in this literature search. Further study of this technique and its applications using high level evidence is warranted.
Keywords: Intramedullary fixation, Metacarpal fractures, Systematic review
Introduction
Metacarpal fractures are among the most commonly treated upper extremity injuries in adults, and represent about 10 % of all fractures [4]. Metacarpal fractures are most often caused by axial loads applied to the hand, frequently with the wrist flexed [10]. The usual etiologies are a direct blow during fisticuffs, or a fall [4]. Indirect torsional forces can also result in metacarpal fracture [10]. Young men have the highest incidence of metacarpal fractures, which has been estimated to be greater than 250 per 100 000 for persons between the ages of 15–24 [8].
Kuntscher et al. first described intramedullary (IM) [29] fixation of long bones in 1939 [18, 21]. They reported that IM fixation decreased infection rates, shortened hospital stays, and allowed for rapid return to function. The IM technique for metacarpal fractures was first described by Lord [23], a military surgeon, in 1957. The interest in the topic was borne from the desire to return injured military personnel to full duty as soon as possible. Lord remarked that the technique allowed for immediate return to duty, which pleased the employer. Foucher et al. [14] built on the technique by introducing the “bouquet” method in 1975, which introduces three Kirschner wires (K-wire) longitudinally into the medullary in a divergent fashion. Bouquet osteosynthesis gained popularity through Europe thereafter [13]. Since Foucher’s report, there have been many articles that have described variations of the technique, with successful results [1, 3, 5, 6, 9, 12, 17, 19, 22, 24, 29].
A number of retrospective and case series studies have investigated the effectiveness of IM fixation for treating metacarpal fractures, and reported favorable results [6, 13, 20, 22, 24, 29]. It has been shown to be technically straightforward, have relatively short operative times, and is associated with low complication rates. The purpose of the present systematic review is to compare the best evidence of IM fixation of metacarpal fractures with other treatment modalities, both surgical and non-surgical.
Methods
Search Strategy
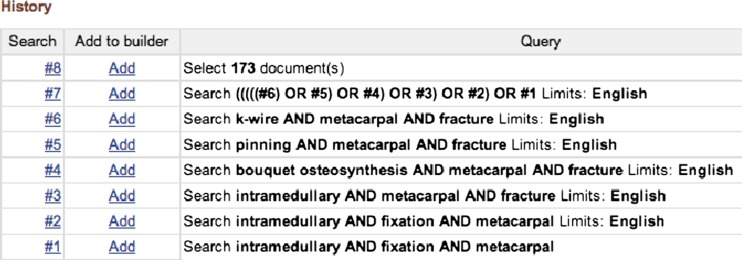
A literature search was conducted with the help of a professional librarian. The following databases were searched: Cochrane Library, MEDLINE, and EMBASE. The key words used were a combination of “metacarpal”, “fracture”, “intramedullary”, “K-wire”, “bouquet osteosynthesis”, and “pinning”. Results were limited to English articles, published before April 2012. An example of the search strategy is shown in Fig. 1. Primary outcome measures were range of motion (ROM) [34] and complication rates. Secondary outcomes include loss of reduction, grip strength, DASH (Disability of arm, shoulder and arm questionnaire) scores, radiographic measures, operating room (OR) times, visual analog scale [2] pain scores, along with any author conclusions.
Fig. 1.
PubMed search history
Article Eligibility
All the retrieved articles’ titles were scanned by two independent reviewers (J.C. and P.D.) and then abstracts and subsequently manuscripts were reviewed in detail based on relevance. To be included for full review, the article must have met the following criteria: treatment of metacarpal fractures using IM fixation and a comparative study design of another treatment modality surgical or non-surgical. Articles were excluded for meeting any of the following criteria: study designs that include case reports, abstracts, conference proceedings, and letters to the editor; studies of thumb metacarpals; animal studies; pediatric studies; gunshot wounds; locked IM fixation (although not excluded when being compared to unlocked IM fixation); biomechanical studies; and studies of intra-articular fractures.
Data Extraction and Analysis
The level of agreement between authors executing the search was evaluated statistically. To this end, a kappa score was calculated to assess inter-rater reliability by comparing articles included and excluded by the two authors responsible for the search (J.C. and P.D.). The following was extracted from each article: author, year, sample size of each group, study model, follow-up duration, study results and authors’ recommendations. The results of the studies were qualitatively assessed. Each article was assigned a level of evidence based on the American Society of Plastic Surgeons Evidence Rating Scale for Therapy [15].
Results
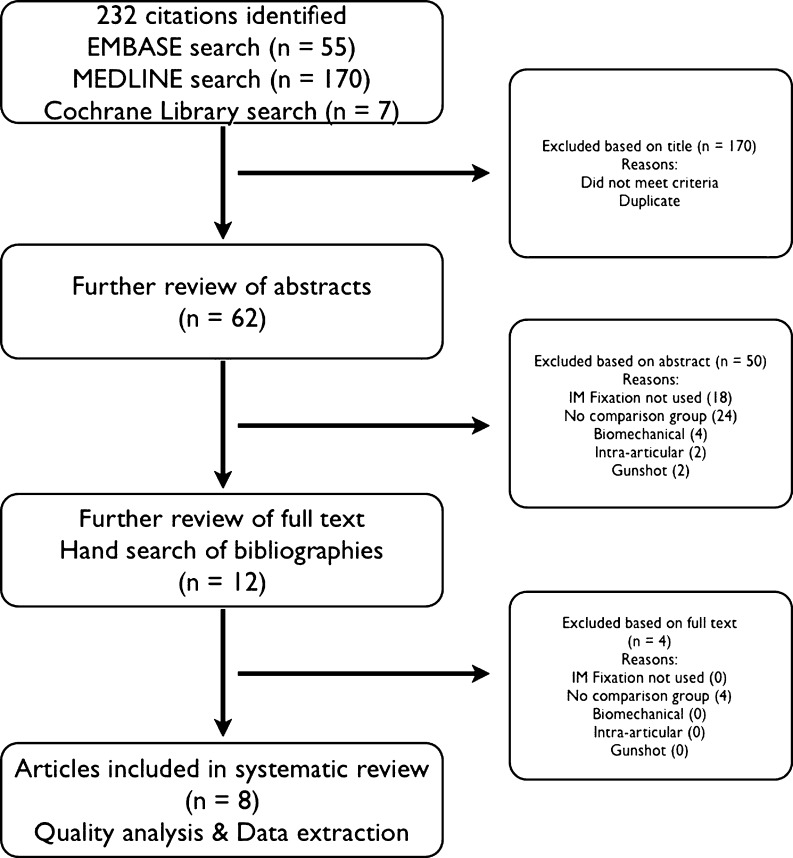
The literature search results are summarized in Fig. 2. The literature search yielded 232 potential studies and after applying the inclusion and exclusion criteria, a total of eight articles were included in this review [11, 16, 26, 27, 30, 33, 35, 36]. A kappa score of 93 % was calculated, which indicates a high inter-rater reliability. A single article meeting our inclusion criteria was discovered during the manuscript review process, and was also included in the study [31].
Fig. 2.
Outline of systematic literature search
A total of 502 patients received treatment for a metacarpal fracture, 233 of which were treated with IM fixation, and 269 were treated either conservatively or with another form of surgical fixation. A formal meta-analysis was not performed because of significant heterogeneity in inclusion and exclusion criteria, as well as evaluated outcomes. An antegrade approach was used for IM fixation in all nine studies. The study designs, inclusion/exclusion criteria, and outcome measures are summarized in Table 1.
Table 1.
American Society of Plastic Surgeons Evidence Rating Scale for Therapy
| Level of Evidence | Qualifying Studies |
|---|---|
| I | High-quality, multicenter or single-center, randomized controlled trial with adequate power; or systematic review of these studies |
| II | Lesser-quality, randomized controlled trial; prospective cohort study; or systematic review of these studies |
| III | Retrospective comparative study, case–control study, or systematic review of these studies |
| IV | Case series |
| V | Expert opinion; case report or clinical example; or evidence based on physiology, bench research, or “first principles” |
Our pre-determined primary outcomes, ROM and complication rates, were studied in nine and seven of the studies, respectively. Four (50 %) of the studies demonstrated that IM fixation resulted in greater ROM at terminal follow-up when compared with their counterpart groups [11, 16, 30, 35]. The remaining articles found no statistical difference in ROM between the groups. Differences in complication rates were not statistically significant in any of the studies, although Ozer et al. [27] found a higher complication rate in the IM fixation group (no p value reported), and Sletten at al. [31] found a difference in a subanalysis of infection rates (p = 0.05) (Table 2).
Table 2.
Selected studies
| Authors | Comparative treatment (# of patients) | Antegrade or retrograde IM fixation (# of patients) | Inclusions/exclusions | Outcome measures | Level of evidence, study design | Author conclusions |
|---|---|---|---|---|---|---|
| Facca et al. [11] | Locked plate (18) | Antegrade (20) | Inclusions: Closed, isolated, displaced 5th metacarpal neck fractures | ROM, radiographic measures, grip strength, VAS for pain, DASH, and complication rates | II, Prospective Comparative Study | IM fixation remains the reference technique for displaced fifth metacarpal neck fractures. |
| Exclusions: Recurrent, open, and/or multiple fractures (metacarpal or other) | ||||||
| Fujitani et al. [16] | Low-profile plates (15) | Antegrade (15) | Inclusions: Unstable fractures with a dorsal angulation of more than 30° or with a shortening more than 3 mm | ROM, radiographic measures, complication rates and grip strength | II, Prospective Comparative Study | Low profile PS fixation should be used for patients refusing bracing and immobilization, and that require early powerful hand strength. Whereas IM fixation should be reserved for patients desiring a less invasive procedure and where regaining full ROM was more critical. |
| Exclusions: Open fractures, under 14 years old | ||||||
| Orbay and Touhami [26] | Locking IM fixation (95) | Usually antegrade (55) | Inclusions: Significantly displaced and unstable metaphyseal or diaphyseal fractures of the metacarpal | Radiographic measures, complications, mean operating time, ROM, grip strength, VAS for pain | III, Retrospective Comparative Study | Proximal locking broadens the indications for the reliable intramedullary fixation. |
| Fractures with 100 % displacement, rotational deformity, angulation of 60° in the 5th metacarpal, or more than 45° in the 4th metacarpal, or more than 30° in the 2nd and 3rd. | ||||||
| Exclusions: articular involvement, tendon injury, open fractures with severe soft tissue loss, and pathological fractures | ||||||
| Ozer et al. [27] | Plate screw fixation (14) | Antegrade (38) | Inclusions: Age between 19 and 49 years with closed extra- articular metacarpal fractures, rotational deformity of more than 5° for shaft fractures of the proximal third and of the middle third, lateral angulation of more than 10° in index and long fingers, 20° for ring finger, and 30° for small finger for fractures of the distal third, lateral angulation of more than 60° for small finger, 40° for index, long, and ring fingers, complete displacement of the fracture with no other associated injuries (fractures of soft tissue injuries). | ROM, DASH, radiographic measures | II, Prospective Comparative Study | IM fixation should not be used in fractures of the distal third metacarpal due to the risk of penetrating the MCP joint. |
| Exclusions: High energy injuries, open and/or comminuted fractures, previous fracture same hand | ||||||
| Schädel-Höpfner et al. [30] | Retrograde Kirschner wire pinning (15) | Antegrade (15) | Inclusions: Displaced neck fractures of the 5th metacarpal, isolated fracture | ROM, grip strength, radiographic measures, DASH, VAS for pain, Steel score | III, Retrospective Comparative Study | They prefer the antegrade IM fixation over the cross-pinning method, but thought further research to better define surgical indications in metacarpal fractures was needed. |
| Exclusions: Loss to follow-up | ||||||
| Strub et al. [33] | Conservative treatment without reduction (20) | Antegrade (20) | Inclusions: Acute, closed fractures, 5th metacarpal neck, palmar displacement between 30° and 70° | ROM, radiographic measures, VAS for pain, grip strength, and complications | II, Randomized Control Trial | Treatment should be decided on an individual basis, and IM fixation may be beneficial over conservative treatment for manual laborers. |
| Exclusions: Rotational deformity greater than 10°, concomitant injuries, open fractures, intra-articular fractures, or shaft fractures | ||||||
| Winter et al. [35] | Percutaneous transverse Kirschner wires (18) | Antegrade (18) | Inclusions: Recent, isolated, closed, simple fracture of the 5th metacarpal neck, any malrotation, palmar angulation greater than 30° | VAS for pain, ROM, grip strength, radiographic measures, patient satisfaction, complications | II, Randomized Control Trial | IM fixation technique is an efficient technique that performed better than percutaneous K-wire pinning. |
| Exclusions: Open fractures, fractures extending to metacarpal shaft, articular involvement, multiple injuries, 5th metacarpal malunion, self-inflicted injuries | ||||||
| Wong et al. [36] | Percutaneous transverse Kirschner wires (29) | Antegrade (30) | Inclusions: Closed fracture, 5th metacarpal base, more than 30° angulation | ROM, grip strength, VAS for pain, complications, radiographic measures | II, Randomized Control Study | The main complications with IM fixation were Kirschner wire migration and perforation of the metacarpal head, although they stated both are avoidable. |
| Exclusions: Angular deformity less than 30°, rotational deformity less than 15°, an open fracture, concomitant hand fractures, patients who refused surgery, less than 1 year follow-up | ||||||
| Sletten et al. [31] | Transverse Kirschner wires (45) | Antegrade (22) | Inclusions: Single, extra-articular neck and shaft fractures of the 4th and 5th metacarpals treated with bouquet or transverse pinning. Volar angulation exceeding 30°. Shaft fractures were primarily treated with closed reduction and a plaster, and surgery was indicated if the | Quick DASH, VAS for pain and satisfaction, grip strength, ROM, radiographic measures | III, Retrospective Comparative Study | Patients treated with transverse or bouquet pinning for fractures of the 4th and 5th metacarpal regain good hand function, but are at risk of surgery-related complications. Due to the risk of fracture of the neighboring metacarpal after transverse pinning, the authors concluded that bouquet pinning is superior and is now the standard at their institution. |
| fracture re-dislocated to more than 20° in the plaster in the 4th metacarpal and 25–30° in the 5th metacarpal. Patients who presented with a rotational deformity of the corresponding finger were treated operatively. | ||||||
| Exclusions: Patients younger than 18 years, patients older than 50 years, patients with fractures older than 10 days at time of surgery, patients with concomitant injuries in the ipsilateral upper limb, or previous fractures of the actual hand or wrist, patients who had a history of a previous fracture of the corresponding metacarpal in the contralateral hand. |
IM intramedullary, PS plating system, ROM range of motion, VAS visual analog scale, DASH Disabilities of the arm, shoulder and hand
Our pre-selected secondary outcomes were reported with much variability among the included studies. Two of the three studies (67 %) that measured operation time found IM fixation took less time [26, 27], while the third [30] showed no difference. The four studies that used the DASH score found no statistical differences [11, 27, 30, 31]. Schädel-Höpfner et al. [30] found a statistically greater improvement in the Steel score (a grading score incorporating ROM, power, pain, and radiography [32]) 6 months postoperatively with IM fixation (p = 0.001). All articles assessed radiographic measures as an outcome and Schädel-Höpfner et al. found significantly less shortening with IM fixation (p = 0.029); the other eight studies found no statistically significant differences, although Strub et al. [33] did not run a statistical test on their radiographic data. Eight articles assessed patient grip strength at follow-up, and seven found no statistical differences. At the 3-month follow-up, Fujitani et al. [16] found that the IM fixation group had lower grip strength (p < 0.05). However, there was no difference at later follow-up. Visual analog scale for pain was used in seven studies with no difference between groups in all but one study; Schädel-Höpfner et al. [30] found IM fixation to be less painful (p = 0.026).
Discussion
The purpose of this review was to summarize the available literature comparing IM fixation with other metacarpal fracture treatments. Although there was a considerable degree of variability between study models, IM fixation was concluded to be equivalent or superior to its competitors in all included studies. However, there was a higher rate of complications in one study [27]. All articles included in the review used an antegrade approach and some variation of Foucher’s technique. Wong et al. [36] suggested that the main complications encountered when using IM fixation, namely, K-wire migration and distal perforation of the metacarpal head, can be avoided by using Foucher’s bouquet technique [36]. Two studies found IM fixation used less OR time than the control group operation [26, 27], and one study found no difference [30].
The treatment of metacarpal fractures has been extensively discussed and several guidelines are available [7, 15, 25]. Guidelines are designed to help clinical decision-making and are based on the best available evidence. Proposed surgical indications for a metacarpal fracture include significant palmar angulation, shortening greater than 2 mm, any rotational deformity, greater than 1 mm of articular surface step-off, and involvement of greater than 25 % of the articular surface [4, 7, 15]. With respect to how much palmar angulation can be tolerated, recommendations vary in the literature from 20° to 70° in the ulnar two digits and 5–10° in the index and middle digit [7, 28]. Other variables that influence management are the anatomical location of the fracture within the metacarpal, the type of fracture, surgeon experience, and patient characteristics. Exact criteria for directing treatment options have not been defined, and guidelines are not ubiquitously applicable.
K-wires can also be placed in the IM space and this may minimize the requisite immobilization period of other K-wire techniques, while conserving the technical facileness that K-wire fixation provides. IM fixation of metacarpal fractures can be done on an outpatient basis under general anesthesia [5, 6, 9, 22, 29], a regional block [3, 9, 12, 13, 22, 29], or local anesthetic [29]. A tourniquet may [9, 12, 13] or may not be applied [5, 6]. A closed reduction is performed first before the procedure. Then surgeons may choose their approach based on the site of the fracture (i.e., a proximal incision for a distal fracture or distal incision for a proximal fracture) [3, 17, 22]. Depending on whether an antegrade or retrograde approach is taken, a small incision is then made over the affected metacarpal base [1, 5, 9, 13, 14, 24] or head [6, 19, 29], respectively. The K-wires are cut to approximate the metacarpal length, and then bent according to the surgeon’s preferences, which usually involves making a small curve in the wire and sharp bends [13] at the blunt end to act as a handle [12]. An awl is used to open the medullary canal and the appropriate placement is confirmed using fluoroscopy. Imaging is routinely used for guiding K-wire insertion, although Foucher originally argued it is not necessary [14]. The number of K-wires can vary from one [1, 3] to four [9, 17], although greater than one K-wire provides better rotational stability [22]. The number of K-wires used depends on surgeon experience, size of the medullary canal, K-wire diameter, and fracture stability [1, 9]. The K-wires can be cut to lie subcutaneously [1, 22, 24], entirely within the IM canal [1, 12, 17] or with a short protruding portion to allow for easy removal [5, 6, 13, 29].
The recent evidence-based review by Friedrich and Vedder [15] suggested that IM fixation is an attractive option for metacarpal fracture treatment. IM fixation of metacarpal fractures was first introduced in 1957, and its efficacy has been demonstrated in multiple case series and observational studies [1, 3, 5, 6, 9, 12, 17, 19, 22, 24, 29]. Foucher et al. [13, 14] introduced the bouquet osteosynthesis technique in 1976. The technique is relatively quick and reproducible, while allowing for early mobilization. Rhee et al. [29] recently published a large prospective series of their modified IM fixation technique for metacarpal neck and shaft fractures with excellent functional and cosmetic results. The potential benefits of IM fixation include less total operative time, fewer days of missed work for patients, and therefore a hypothesized favorable cost/benefit ratio; however, this was not addressed in this review and should be further studied.
A major drawback of IM fixation is that it does not truly provide rigid fixation [7]. Therefore a longer period of immobilization is necessary than with PS fixation. Since patient compliance can be suboptimal in this population, there is a theoretical risk of delayed union or malunion in the patient non-compliant of immobilization protocols. However, none of the studies included in this review assessed rates of compliance. Although no regimen has been determined to be optimal [28], some period of immobilization will be necessary postoperatively after IM fixation, which requires the cooperation of the patient.
Limitations of this study were intrinsic to the retrieved articles. The quality of the evidence available is low to moderate, with the highest rated article receiving II on the American Society of Plastic Surgeons Evidence Rating Scale for Therapy [15]. Many of the studies had small sample sizes, which increases the risk of making type I or type II statistical errors. Due to the heterogeneity of the study designs and outcome measures, it was not reasonable to pool the data for a meta-analysis. Half of the articles looked only at Boxer’s fractures and thereby limits the ability to generalize these results to all metacarpal fractures [11, 30, 33, 35]. "Kirschner wire" was not included in the initial search strategy; however, upon review of the references from all included articles, and a more recent search of the online databases, no additional relevant studies were identified based on the use of Kirschner wire.
The lack of high-quality research studies available for this systematic review precludes us from making any evidence-based recommendations or conclusions on IM fixation compared to other treatment modalities. There is a need for higher-level studies to compare the various surgical and non-surgical treatment options for metacarpal fractures. The incidence of metacarpal fractures is high and thus even small benefits would be significant for the overall population.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
No experiments were conducted in this study. No humans or animals were used in its making.
Statement of informed consent
No patient information was included in this study.
Contributor Information
Joseph P. Corkum, Phone: +1-902-8028434, Email: jpc@dal.ca
Peter G. Davison, Email: peter.davison@dal.ca
Donald H. Lalonde, Email: labtrio@nbnet.nb.ca
References
- 1.Balfour GW. Minimally invasive intramedullary rod fixation of multiple metacarpal shaft fractures. Tech Hand Up Extrem Surg. 2008;12(1):43–5. doi: 10.1097/BTH.0b013e31815678ef. [DOI] [PubMed] [Google Scholar]
- 2.Bardin T, et al. Prospective study of articular involvement in patients on hemodialysis for 10 years. Rev Rhum Mal Osteoartic. 1988;55(2):131–3. [PubMed] [Google Scholar]
- 3.Blazar PE, Leven D. Intramedullary nail fixation for metacarpal fractures. Hand Clin. 2010;26(3):321–5. doi: 10.1016/j.hcl.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Bucholz, R.W. Chapter 3. The epidemiology of fractures. Rockwood and Green's fractures in adults. 7th ed. Lippincott Williams & Wilkins; Vol. 1. 2009.
- 5.Calder JD, O'Leary S, Evans SC. Antegrade intramedullary fixation of displaced fifth metacarpal fractures. Injury. 2000;31(1):47–50. doi: 10.1016/S0020-1383(99)00201-6. [DOI] [PubMed] [Google Scholar]
- 6.Chammaa RH, Thomas PB, Khalil A. Single retrograde intramedullary wire fixation of metacarpal shaft fractures. Acta Orthop Belg. 2010;76(6):751–7. [PubMed] [Google Scholar]
- 7.Chin SH, Vedder NB. MOC-PSSM CME article: metacarpal fractures. Plast Reconstr Surg. 2008;121(1 Suppl):1–13. doi: 10.1097/01.prs.0000294704.48126.8c. [DOI] [PubMed] [Google Scholar]
- 8.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908–15. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 9.Downing ND, Davis TR. Intramedullary fixation of unstable metacarpal fractures. Hand Clin. 2006;22(3):269–77. doi: 10.1016/j.hcl.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 10.Dye, T.M. Metacarpal fractures. Medscape 2012, April 29th, 2012. Available at: http:emedicine.medscape.com/article/1239721-overview.html.
- 11.Facca S, et al. Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Orthop Traumatol Surg Res. 2010;96(5):506–12. doi: 10.1016/j.otsr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Faraj AA, Davis TR. Percutaneous intramedullary fixation of metacarpal shaft fractures. J Hand Surg Br. 1999;24(1):76–9. doi: 10.1016/S0266-7681(99)90039-6. [DOI] [PubMed] [Google Scholar]
- 13.Foucher G. "Bouquet" osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am. 1995;20(3 Pt 2):S86–90. doi: 10.1016/S0363-5023(95)80176-6. [DOI] [PubMed] [Google Scholar]
- 14.Foucher G, Chemorin C, Sibilly A. A new technic of osteosynthesis in fractures of the distal 3d of the 5th metacarpus. Nouv Presse Med. 1976;5(17):1139–40. [PubMed] [Google Scholar]
- 15.Friedrich JB, Vedder NB. An evidence-based approach to metacarpal fractures. Plast Reconstr Surg. 2010;126(6):2205–9. doi: 10.1097/PRS.0b013e3181f830ad. [DOI] [PubMed] [Google Scholar]
- 16.Fujitani R, et al. Comparison of the intramedullary nail and low-profile plate for unstable metacarpal neck fractures. J Orthop Sci. 2012;17(4):450–6. doi: 10.1007/s00776-012-0223-y. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez MH, Igram CM, Hall RF., Jr Flexible intramedullary nailing for metacarpal fractures. J Hand Surg Am. 1995;20(3):382–7. doi: 10.1016/S0363-5023(05)80091-7. [DOI] [PubMed] [Google Scholar]
- 18.Itadera E, et al. Closed intramedullary fixation for metacarpal fractures using J-shaped nail. Hand Surg. 2008;13(3):139–45. doi: 10.1142/S0218810408003980. [DOI] [PubMed] [Google Scholar]
- 19.Karbelnig MJ. Fracture of the metacarpal shaft. A method of treatment. Calif Med. 1963;98:269–70. [PMC free article] [PubMed] [Google Scholar]
- 20.Kelsch G, Ulrich C. Intramedullary k-wire fixation of metacarpal fractures. Arch Orthop Trauma Surg. 2004;124(8):523–6. doi: 10.1007/s00402-004-0706-1. [DOI] [PubMed] [Google Scholar]
- 21.Kuntscher, G., Di Marknagelung von Knockenbruchen Langenbeck's Archiv far Klinische Chirugie vereinigt mit Deutsche Zeitschrift fur Chirugie, 1940. 200: p. 443–9
- 22.Liew KH, Chan BK, Low CO. Metacarpal and proximal phalangeal fractures—fixation with multiple intramedullary Kirschner wires. Hand Surg. 2000;5(2):125–30. doi: 10.1142/S0218810400000314. [DOI] [PubMed] [Google Scholar]
- 23.Lord RE. Intramedullary fixation of metacarpal fractures. J Am Med Assoc. 1957;164(16):1746–9. doi: 10.1001/jama.1957.02980160018005. [DOI] [PubMed] [Google Scholar]
- 24.Manueddu CA, Della Santa D. Fasciculated intramedullary pinning of metacarpal fractures. J Hand Surg Br. 1996;21(2):230–6. doi: 10.1016/S0266-7681(96)80104-5. [DOI] [PubMed] [Google Scholar]
- 25.McNemar TB, Howell JW, Chang E. Management of metacarpal fractures. J Hand Ther. 2003;16(2):143–51. doi: 10.1016/S0894-1130(03)80009-1. [DOI] [PubMed] [Google Scholar]
- 26.Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3):279–86. doi: 10.1016/j.hcl.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 27.Ozer K, et al. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724–31. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Poolman RW, et al. Conservative treatment for closed fifth (small finger) metacarpal neck fractures. Cochrane Database Syst Rev. 2005;3 doi: 10.1002/14651858.CD003210.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rhee SH, et al. Prospective multicenter trial of modified retrograde percutaneous intramedullary Kirschner wire fixation for displaced metacarpal neck and shaft fractures. Plast Reconstr Surg. 2012;129(3):694–703. doi: 10.1097/PRS.0b013e3182402e6a. [DOI] [PubMed] [Google Scholar]
- 30.Schadel-Hopfner M, et al. Antegrade intramedullary splinting or percutaneous retrograde crossed pinning for displaced neck fractures of the fifth metacarpal? Arch Orthop Trauma Surg. 2007;127(6):435–40. doi: 10.1007/s00402-006-0254-y. [DOI] [PubMed] [Google Scholar]
- 31.Sletten, I.N., et al., Assessment of volar angulation and shortening in 5th metacarpal neck fractures: an inter- and intra-observer validity and reliability study. J Hand Surg Eur Vol, 2012. [DOI] [PubMed]
- 32.Steel WM. Articular fractures. In: Fractures of the Hand and the Wrist. Churchill Livingstone: New York, Edinburgh, London, Melbourne; 1988. p. 55–73.
- 33.Strub B, et al. Intramedullary splinting or conservative treatment for displaced fractures of the little finger metacarpal neck? A prospective study. J Hand Surg Eur Vol. 2010;35(9):725–9. doi: 10.1177/1753193410377845. [DOI] [PubMed] [Google Scholar]
- 34.Styf J, Karlsson J, Romanus B. Intra-articular pressure of the hip joint in Legg–Calve–Perthes disease. Rev Chir Orthop Reparatrice Appar Mot. 1988;74(Suppl 2):268–70. [PubMed] [Google Scholar]
- 35.Winter M, et al. Surgical treatment of the boxer's fracture: transverse pinning versus intramedullary pinning. J Hand Surg Eur Vol. 2007;32(6):709–13. doi: 10.1016/j.jhse.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg Br. 2006;31(1):61–5. doi: 10.1016/j.jhsb.2005.06.022. [DOI] [PubMed] [Google Scholar]