Abstract
Background
The diagnosis and validation of thoracic outlet syndrome/brachial plexopathy (TOS) remains a difficult challenge for surgeons, neurologists, and radiologists. This is due to the fact that the responses of standard elevated arm stress tests can be considered somewhat subjective and can vary. Therefore, non-vascular TOS cases are presently diagnosed clinically, and any objective diagnosis has been controversial.
Methods
This is a technique paper describing the use of dynamic neuromusculoskeletal ultrasound to assist in the diagnosis of thoracic outlet/brachial plexus pathology. We propose a new way to observe the brachial plexus dynamically, so that physical verification of nerve compression between the anterior and middle scalene muscles can be clearly made at the onset of clinical symptoms. This gives a way to objectively identify clinically significant brachial plexus compression.
Results
Dynamic testing can add objective analysis to tests such as the elevated arm stress tests and can correlate the onset of symptoms with plexus compression between the anterior and middle scalene muscles. With this, the area of pathologic compression can be identified and viewed while performing the dynamic testing. If compression is seen and the onset of symptoms ensues, this is a positive confirmatory test for the presence of TOS and a clinically significant disease.
Conclusions
This paper offers a simple, objective, and visual diagnostic test that can validate the presence or absence of brachial plexus compression during arm elevation in patients with brachial plexus injury and thoracic outlet syndrome.
Electronic supplementary material
The online version of this article (doi:10.1007/s11552-013-9523-8) contains a video, which is available to authorized users.
Keywords: Thoracic outlet syndrome, Brachial plexus, Neuromusculoskelatal ultrasound, Diagnostic ultrasonography, Roos test, Adson test, Brachial plexopathy diagnosis
Background and Purpose
Here we present a clear-cut, objective, and visual diagnostic test which can validate the presence or absence of brachial plexus compression during arm elevation in patients with brachial plexus injury and thoracic outlet syndrome (TOS).
The diagnosis and validation of TOS/brachial plexopathy remains a challenge for surgeons, neurologists, and radiologists. Controversy over the methods dates back to the early 1900s, when Adson described his test for TOS as being positive when it showed a loss of pulse and the onset of dysesthesia with arm abduction in the elevated posture [6–19].
In the 1960s, Roos demonstrated operatively that TOS could be present without loss of pulse, that most cases of TOS are neurogenic in nature and that the vascular type is not as common. Consequently, the Roos test and other elevated arm stress tests were developed [17, 30]. However, the results of these tests have been considered somewhat subjective in that patient response is needed and responses can vary.
Doppler vascular studies can identify the 5 % of TOS cases that are vascular but nonvascular cases cannot be diagnosed by this method. Further electrical studies with nerve conduction and electromyelographic testing, for example, EMG/NCV studies, are not reliable in most areas, with some believing that the diagnosis can be made only by testing the lateral antebrachial cutaneous nerve and the medial antebrachial cutaneous nerve, the sensory branches leading from the brachial plexus to the medial and lateral arm [33, 11]; and others believing that conductions across the plexus from Erb's point to the axilla could document the pathology [12, 24]. Because of a lack of other objective findings, some neurologists question the diagnosis unless atrophy is present [26].
MRI studies are useful for identifying cases with static compression, tumors, and aneurysm pathology and can identify nerve changes in some cases. Unfortunately, dynamic testing cannot be undertaken with MRI and, in addition to being expensive [7], the clarity of nerve images is less than optimal, especially with suboptimal coils [22, 8, 23].
These diagnostic challenges often leave clinicians with the problem of how to address pain and dysfunction in those patients who obviously have pathology, but do not present with objective documentable evidence. In such cases, highly complex surgery and other intensive medical treatments, with substantial possible complications, are difficult to justify [18, 3, 27, 16].
Differential diagnoses include cervical disk disease, shoulder dysfunction, carpal tunnel syndrome, and other peripheral neuropathies [13]. Ultrasound is used to visualize these nerve structures and the surrounding anatomy in real time, and although this technique has been used dynamically [9], in most cases of nerve pathology it is still used as a static study [32, 2, 10–25].
Ultrasound has been used for the dynamic evaluation of ligament and tendon structures and these techniques can be applied to entrapment neuropathies with equally reproducible and clinically useful results [29–5].
This paper addresses the diagnosis of TOS using neuromusculoskeletal (NMSK) ultrasound. Specifically, we investigate the brachial plexus and its relationship to the anterior and middle scalene and to other surrounding tissues. The nerves themselves can be visualized well using cross-sectional and longitudinal views, allowing swelling of the nerves and nerve compression to be identified. More importantly, the brachial plexus itself can be localized and visually evaluated at its point of tenderness and tested for positive tinel’s sign. Along with this, dynamic testing can be performed to reproduce the elevated arm stress tests and correlate the onset of symptoms with brachial plexus compression between the anterior and middle scalene muscles. This allows us to identify the area of pathology and compression and view the actual anatomy while performing the dynamic testing. If compression is observed and the onset of symptoms ensues, this is a positive test for the presence of TOS and clinically significant disease.
Using ultrasound, we can validate that there is compression of the actual brachial plexus when elevating the arm past 90°. This is an objective test that can be correlated with the onset of symptoms in the diagnosis of TOS.
Materials and Methods
All examinations were performed by the lead author using the technique described to duplicate the positions of dynamic stress on the structures of the brachial plexus.
A Sonosite M-MSK system and HFL50 15-6mHz transducer (Sonosite, Bothell, WA, USA) were used for all examinations. Comparison studies were done on all patients to evaluate the opposite side to be certain that the pathology was consistent with the clinical disease. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Dynamic Neuromusculoskeletal Ultrasound Plexus Testing
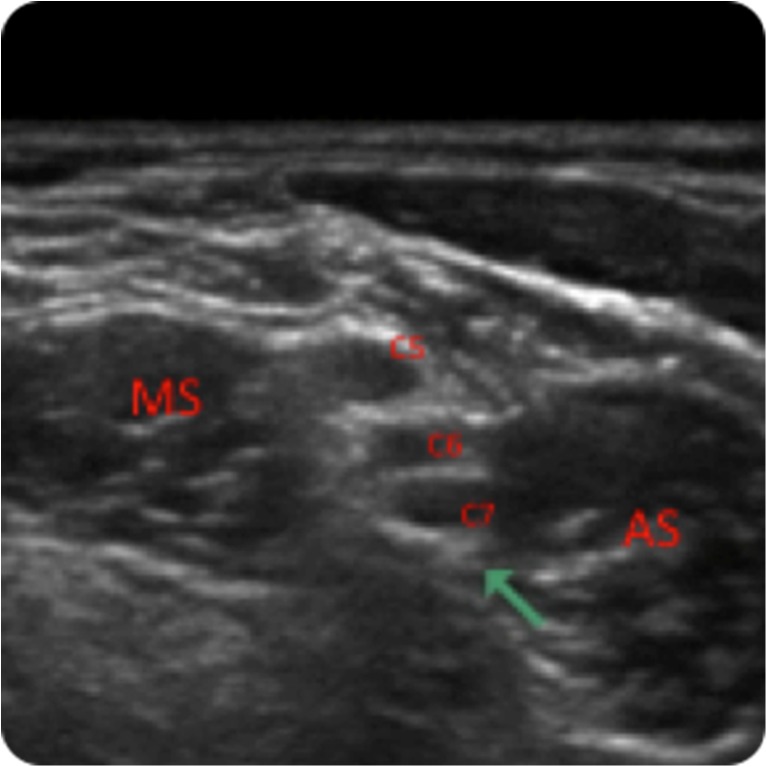
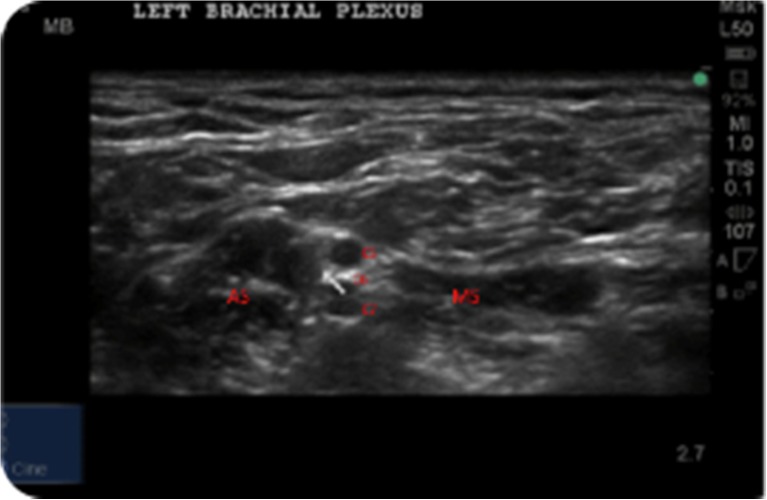
The examination essentially “visualizes” the dynamic internal anatomy of the brachial plexus at the thoracic outlet when performing the standard and accepted diagnostic tests for TOS, such as the Roos, Adsons, Wrights, and elevated arm stress tests. The cross-sectional anatomy can be visualized as shown above (Fig. 1).
Fig. 1.
Ultrasound image. AS anterior scalene, MS middle scalene, and C5−7 nerve roots of the brachial plexus
In the presence of clinical TOS, the anterior scalene (AS) compresses the structures of the brachial plexus (C5, C6, and C7) in the thoracic outlet between the anterior and middle scalene (MS) muscles during examination with standard elevated arm stress testing [1].
Depending upon the amount of elasticity in the scalene muscles, the dimensions of that particular thoracic outlet, and the amount of scarring, variable degrees of compression, or none at all, may occur to the plexus. This compression and narrowing of the thoracic outlet can be clearly demonstrated using the technique described below, which visualizes the compression of the nerves in the thoracic outlet when the arm is elevated. This is shown below in the clinical case examples of normal testing as well as the dynamic videos that show compression of the brachial plexus with arm abduction.
As we will demonstrate, in normal individuals, a negative test causes no compression and the nerves of the brachial plexus can still be visualized with arm elevation. The contour and patency of the thoracic outlet is maintained with no symptoms.
In positive tests, where scarring, deformity of the anterior or middle scalene, the presence of aberrant bands or constricting perineural tissue is present, compression of the brachial plexus nerve structures is evident. This can be seen in the case examples below where the C5, C6, and C7 nerve roots compress and disappear with compression between the anterior and middle scalene muscles. When accompanied by clinical symptoms of numbness or tingling, this is considered a positive test.
The NMSK ultrasound dynamic testing validates the presence or absence of actual brachial plexus compression by the added visual demonstration of nerve compression with the onset of clinical symptoms.
Ultrasound Technique
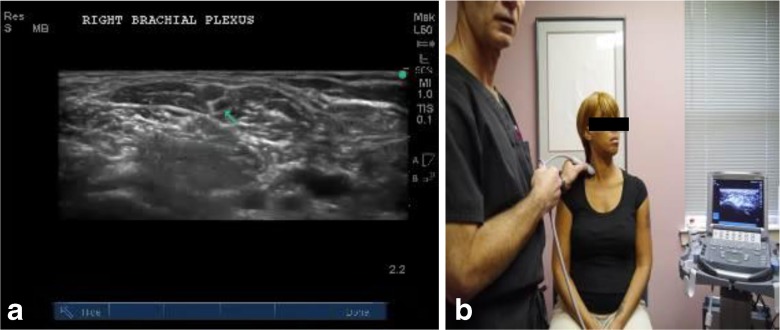
The ultrasound examination for dynamic testing of the brachial plexus for compression is performed with the patient in a seated position. Initially, the arm is in neutral, resting in the patient's lap or on a pillow. The probe is placed in the supraclavicular fossa, and the subclavian artery is identified (Fig. 2). Color Doppler is used to ensure vascular flow.
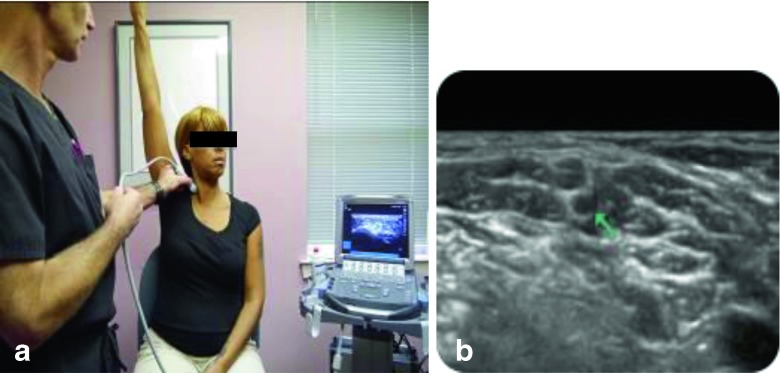
Fig. 2.
a Ultrasound image. b Patient and operator showing ultrasound scan position
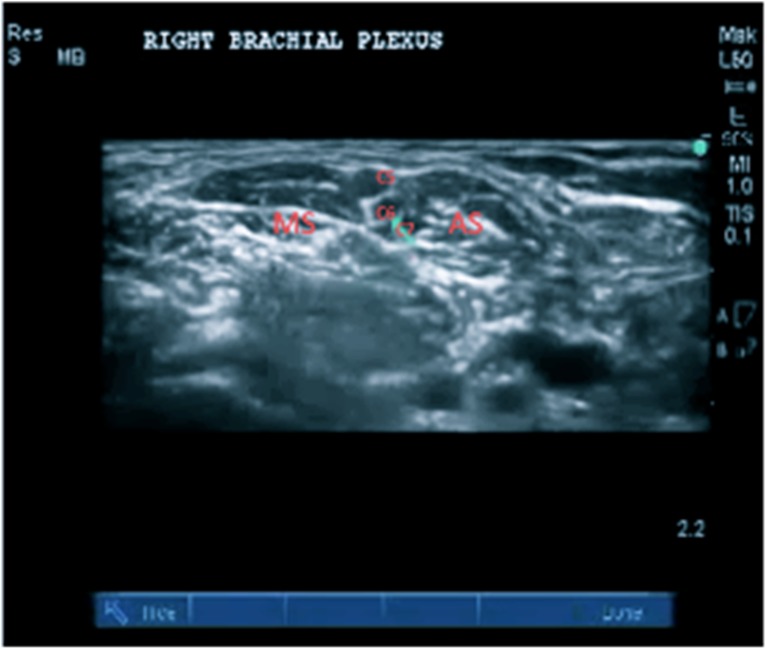
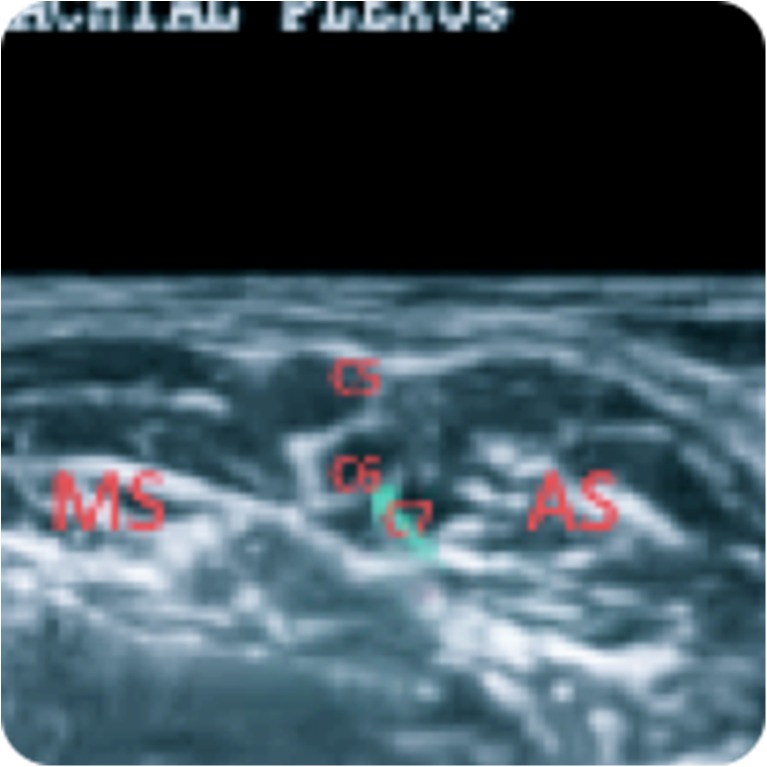
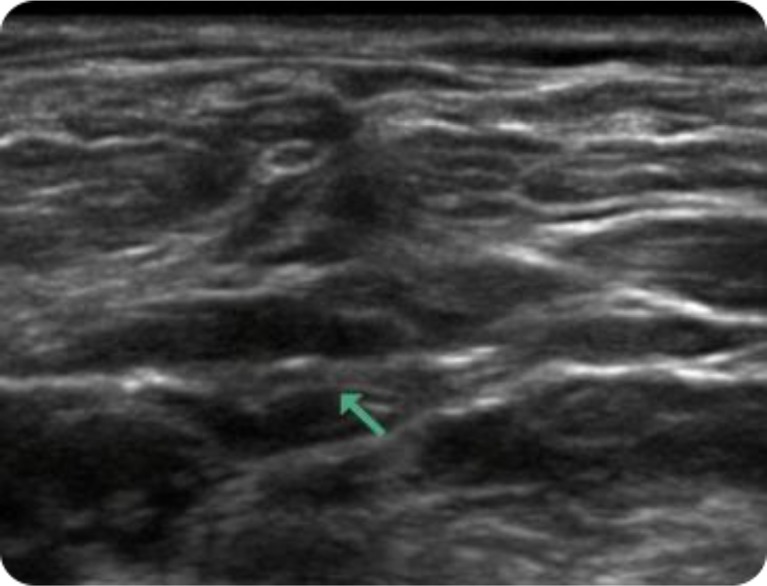
Figures 3 and 4 above show the sonographic anatomy of the brachial plexus as seen on the screen and a zoomed-in version detailing the anatomy before testing; AS, anterior scalene; MS, middle scalene, and the C5, C6, and C7 nerves in cross-section.
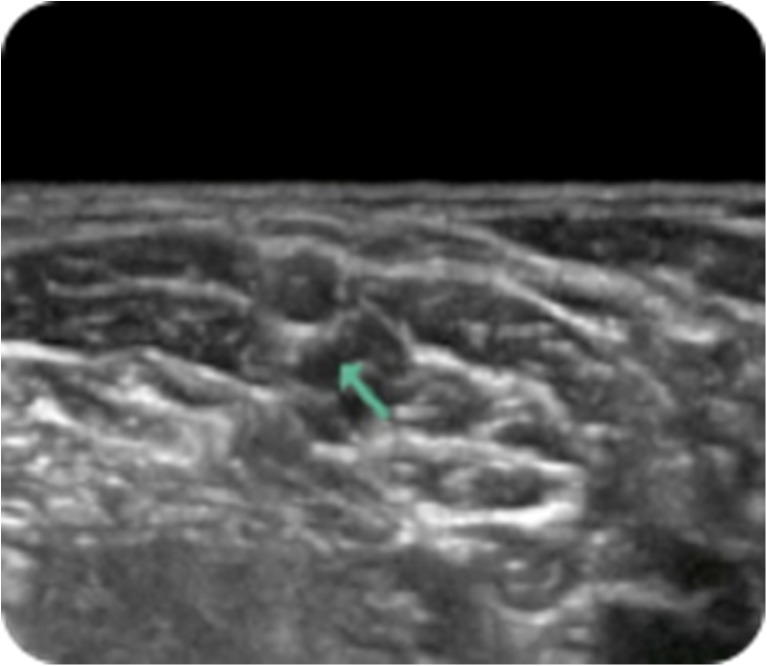
Fig. 3.
Ultrasound image of the normal pre-test anatomy. C5–7 are shown under the green arrow
Fig. 4.
Ultrasound image zoomed in view
Generally, above and just posterior to the artery, the nerves of the brachial plexus can be identified. This is essentially the same approach utilized for performing a supraclavicular nerve block [10]. The anterior and middle scalene muscles are visible surrounding the brachial plexus (see Figs. 3 and 4). The quality of these muscles can be evaluated at this time. Severe scarring about the brachial plexus and scalene deformities can also be identified. The brachial plexus is then viewed isolating the upper, middle, and lower trunks and the nerve roots labeled above (C5, C6, and C7). Longitudinal views should then also be obtained for completeness.
Next, the arm is allowed to hang down by the patient’s side (Fig. 5). Static views to image the plexus under the stress of the arm weight only are taken. The three hypoechoic circles of the brachial plexus are indicated by the green arrow as shown in Fig. 6.
Fig. 5.
Ultrasound scan position arm at side
Fig. 6.
Ultrasound image normal plexus
Next, the patient is instructed to abduct the arm directly to the side with the palm facing towards the floor (Fig. 7). The arm is then abducted through the active range of abduction as best the patient can perform. The plexus should be visualized throughout the motion and but most importantly at 90, 130, and 150° of abduction.
Fig. 7.
Ultrasound scan position with the arm at a 90° abduction
The contour of the brachial plexus nerves and the maintenance or narrowing of the interval is continuously evaluated through the dynamic testing, reproducing the posture of the elevated arm stress testing through the full range of motion. Compression of the brachial plexus and the onset of clinical symptoms with narrowing or obliteration of the interval is considered a positive scan.
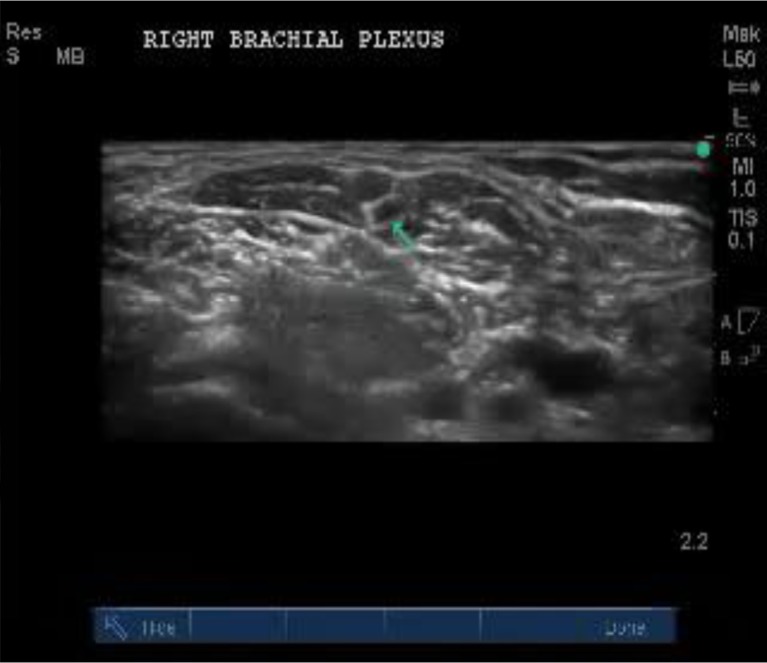
Figure 8 shows a negative dynamic test for compression. Note the C5, C6, and C7 nerve roots at the green arrow remain visualized and uncompressed with full arm abduction.
Fig. 8.
a Ultrasound scan position with arm raised. b Corresponding image showing no brachial plexus compression
If the opposite side is asymptomatic, a comparison evaluation of the normal side is helpful in confirming a positive test, although in patients with bilateral pathology, this may not be possible.
Criteria for a Positive Dynamic Compression Test
A positive test is indicated by a decrease in the interscalene interval with abduction and brachial plexus compression with loss of surrounding soft tissue space, accompanied by either a compressed brachial plexus or obliteration of the visualized nerves. This is similar to findings on MRI with compression of the cord by a disk herniation or bulge.
It is clinically relevant that the nerves are compressed and clinical symptoms occur. This is significant in that the interscalene interval is highly variable, since the nerves of the brachial plexus, in utero, actually grow through scalene muscle mass and essentially create what become the anterior and middle scalene muscles. This anatomy is different in every individual; consequently, surgical findings and clinical presentation of brachial plexus injury can be highly variable [26].
During the stress test, what is being measured clinically with elevation is whether abduction of the arm results in compression or impingement of the nerves themselves, which is not present in the non-stressed posture. Furthermore, it is necessary that the compression be associated with the onset of clinical symptoms, along with a documented change in either the contour or width of the space; this is then a positive clinical neuromusculoskeletal dynamic stress test evaluation.
In some cases, with repeat dynamic testing, a change in the plexus morphology is seen after a positive test with increased hypoechogenicity of the plexus nerves and hyperechogenic appearance of the surrounding tissue. Perineural edema is commonly seen in the operating room, and is visible on ultrasound scans, proximal to the area of nerve compression. This is caused by vascular compromise, specifically in the vaso vasorum. These changes are similar in dynamic testing and may also be helpful in confirming pathologic objective changes in the nerves after stress examinations produce compression.
Results
Clinical Case Examples
Static images are presented to first familiarize the reader with normal and pathologic anatomy and then dynamic video testing of several cases is presented to show the actual compression that occurs during live motion testing.
Patient DR has symptoms on the right but testing shows no entrapment of the brachial plexus before and after dynamic testing and before stress testing of the normal brachial plexus. Figure 9 shows the three normal round or ovoid hypoechoic structures (green arrow); these are the trunks of the brachial plexus with no impingement surrounded by the anterior and middle scalene muscles.
Fig. 9.
Ultrasound image shows normal brachial plexus anatomy in a symptomatic patient at rest
A negative or normal stress test is shown in Fig. 10, with normal maintenance of the plexus interval and continued visualization of the round or ovoid hypoechoic structures of the brachial plexus under the green arrow.
Fig. 10.
Ultrasound image shows normal brachial plexus anatomy during a negative dynamic stress test
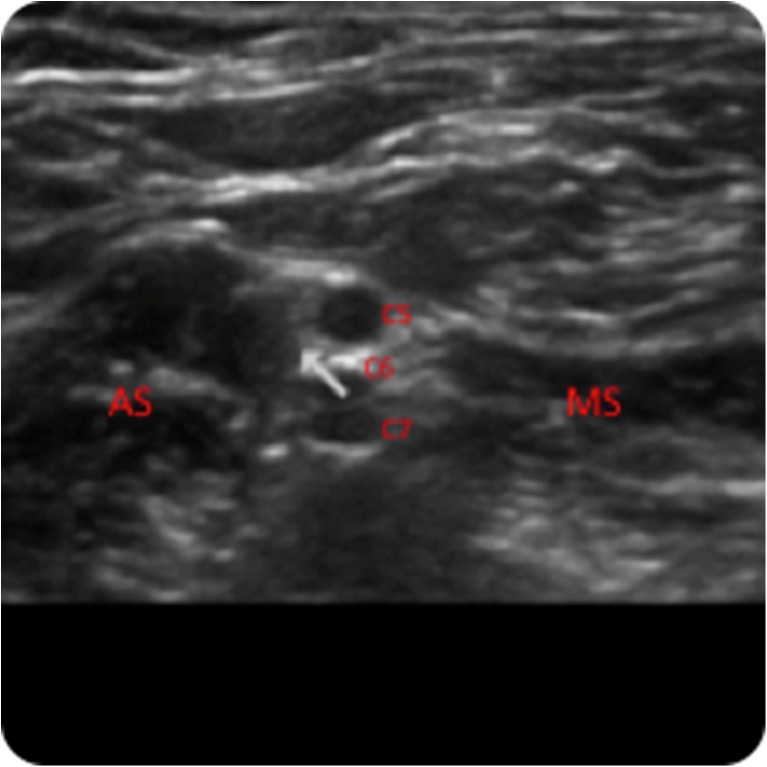
The next example is patient MB, a 47-year-old male with post-traction injury to the left arm reporting complaints of numbness and tingling in the left arm with elevation and reaching activity. EMG/NCV studies show brachial plexus injury on the left and not on the right.
Pre-dynamic stress testing of the left brachial plexus shows three normal round or ovoid hypoechoic structures (Fig. 11, below white arrow), which are the trunks of the brachial plexus with no impingement surrounded by the anterior and middle scalene muscles.
Fig. 11.
Normal Ultrasound image in a symptomatic patient at rest
Below is the same patient (MB) after completing a positive scan, with the arm in abduction during dynamic stress testing. Note the complete disappearance of the three round hypoechoic structures (C5, C6, and C7) of the brachial plexus compared with the pre-stress study. This indicates compression between the anterior and middle scalene muscles. This is also a positive dynamic NMSK ultrasound test for brachial plexus compression (Figs. 12, 13, and 14).
Fig. 12.
Ultrasound image magnified no compression
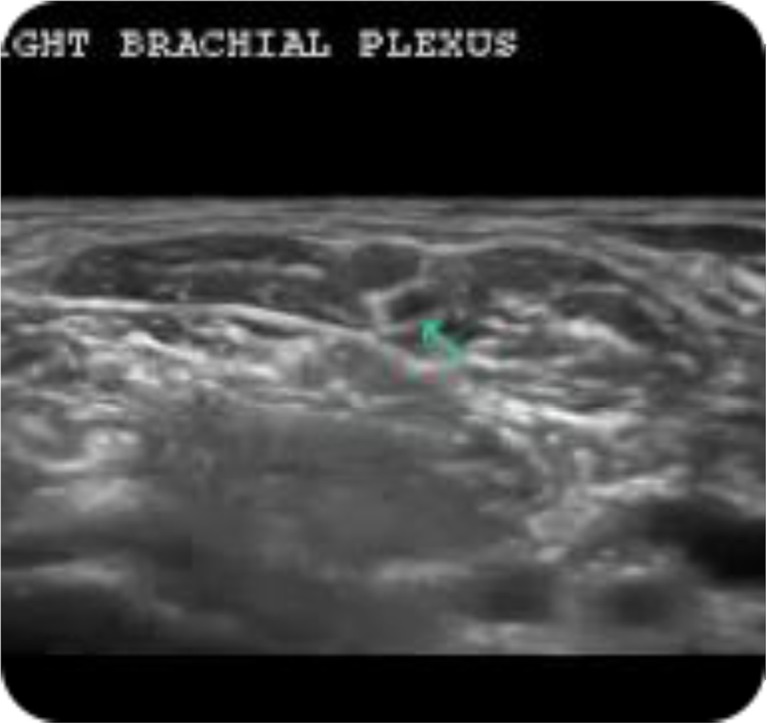
Fig. 13.
Ultrasound image of positive dynamic NMSK ultrasound test for brachial plexus compression
Fig. 14.
Ultrasound image of magnified positive scan showing compression at the green arrow
The attached dynamic video studies demonstrate live motion studies of dynamic stress testing for further clarification.
First, a normal brachial plexus dynamic neuromusculoskeletal ultrasound stress test is shown. This is what a normal brachial plexus with no compression looks like during initial scanning and through a normal dynamic stress test.
Next we see a case study with bilateral testing. The image on the right side of the screen is normal and is first shown as a still before the video motion study.
Immediately following this are two dynamic studies of the injured brachial plexus in the same patient. This demonstrates compression with stress testing in comparison with a normal brachial plexus. These two positive scans clearly demonstrate what we would see on a positive dynamic stress test.
The final video is another positive stress test in a different patient with compression of the nerve roots between the anterior and middle scalene muscles during elevated arm stress testing.
Discussion
The current approach for treatment of patients with brachial plexus injury is conservative treatment. Surgery is necessary in only about 5 % of patients and with major risk of complications such as paralysis of the facial nerve, laryngeal nerve or arm, phrenic nerve injury, hemothorax, pneumothorax, bleeding, and even death, a conservative approach is reasonable. Furthermore, 50 % of patients show no improvement 6 months after surgery and some experience degradation due to recurrent scarring [30, 19, 15, 14].
With this in mind, therapy, activity modification, and pain management become essential components of the treatment plans for patients reporting pain [20]. One of the primary issues encountered with TOS patients is how to explain the exact cause of their symptoms. Understanding the dynamics and physiology of brachial plexus nerve compression is often very difficult for patients to grasp. It can be an eye-opening experience for patients when they can actually visualize compression of the brachial plexus with the onset of clinical symptoms during the dynamic test. Patients understand almost immediately why they are experiencing numbness when they place their arms in an overhead position or reach out away from the body. The exact amount of abduction they can clinically tolerate can also be determined, which provides patients with a better idea of what they are capable of doing without aggravating the problem. It can also help them to determine the extent of their vocational and avocational abilities, and which activities may need modifications. This can help to direct therapy in that we know when the onset of symptoms will occur, both during therapeutic nerve sliding exercises as well as in lifestyle modifications. Furthermore, we can identify the areas of significant scarring and whether this is a more intermittent compression or fixed perineural scar tissue, allowing the use of modalities such as ultrasound, iontophoresis, and massage to address the clinical symptoms.
Concerning work-related problems, this information allows workplace adaptation and ergonomic changes to be instituted to allow patients to perform maximally and yet stay within their physical limits. They will also be able to identify aggravating factors. In medicolegal cases, it allows clear documentation of injury and validates legitimate pathology, which helps rule out suggestions of malingering.
Another benefit is the correlation of these findings with distal nerve studies, ultrasound, and EMG/NCV. These benefits, along with appropriate scanning of the cervical spine, can help determine whether a patient suffers from double crush syndrome and rule out any associated multilevel compression neuropathies.
In conclusion, we have described here a technique for dynamic neuromusculoskeletal ultrasound to assist in the diagnosis of TOS/brachial plexopathy. This technique provides a new, dynamic way to look at the brachial plexus, by which physical verification of nerve compression can be clearly identified at the onset of clinical symptoms, providing an objective corroboration of clinically significant brachial plexus compression. Prior to this, diagnosis of non-vascular TOS cases was primarily clinical and attempts to objectify the diagnosis have been fraught with controversy. Further clinical trials will be required to determine the accuracy and clinical utility of this new technique and to define the presence of thoracic outlet compression in clinically symptomatic individuals.
Electronic supplementary material
(MOV 92975 kb)
Acknowledgments
Statement of Human and Animal Rights
The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Conflicts of Interest Statement
The authors have no conflicts of interest, commercial associations, or intent for financial gain regarding this research.
Statement of Informed Consent
Informed consent has been obtained for cited clinical participants.
Contributor Information
Scott M. Fried, Email: askdoctorscott@gmail.com
Levon N. Nazarian, Email: Levon.Nazarian@jefferson.edu
References
- 1.Atasoy E. Thoracic outlet syndrome: Anatomy. Hand Clin. 2004;20:7–14. doi: 10.1016/S0749-0712(03)00078-7. [DOI] [PubMed] [Google Scholar]
- 2.Blankstein A. Ultrasound in the diagnosis of clinical orthopedics: The orthopedic stethoscope. World J Orthop. 2011;2(2):13–24. doi: 10.5312/wjo.v2.i2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooke R. Thoracic outlet syndrome: Aspects of diagnosis in the differential diagnosis of hand–arm vibration syndrome. Occup Med. 2003;53:331–336. doi: 10.1093/occmed/kqg097. [DOI] [PubMed] [Google Scholar]
- 4.Demondion X, Herbinet P, Boutry N, et al. Sonographic mapping of the normal brachial plexus. Am J Neuroradiol. 2003;24:1303–1309. [PMC free article] [PubMed] [Google Scholar]
- 5.DeSmet A, Winter T, Best T, et al. Dynamic sonography with valgus stress to assess elbow ulnar collateral ligament injury in baseball pitchers. Skeletal Radiol. 2002;31:671–676. doi: 10.1007/s00256-002-0558-0. [DOI] [PubMed] [Google Scholar]
- 6.Erdoğan A. A hand surgeon's further experience with thoracic outlet compression syndrome. J Hand Surgery. 2010;35(9):1528–1538. doi: 10.1016/j.jhsa.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 7.Grechenig W, Mayr J, Peicha G, et al. Subluxation of the ulnar nerve in the elbow region: Ultrasonographic evaluation. Acta Radiol. 2003;44(6):662–664. doi: 10.1080/02841850312331287789. [DOI] [PubMed] [Google Scholar]
- 8.Haber H, Sinis N, Haerle M, et al. Brachial plexus traction injuries. AJR Am J Roetgenol. 2006;186(6):1787–1791. doi: 10.2214/AJR.04.1861. [DOI] [PubMed] [Google Scholar]
- 9.Haun D, Cho C, Kettner N. Normative cross-sectional-area of the C5–C8 nerve roots using ultrasonography. Ultrasound Med Biol. 2010;36(9):1422–1430. doi: 10.1016/j.ultrasmedbio.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 10.Hems T, Birch R, Carlstedt T. The role of magnetic resonance imaging in the management of traction injuries of the adult brachial plexus. J Hand Surg Br. 1999;24B:550–555. doi: 10.1054/jhsb.1999.0234. [DOI] [PubMed] [Google Scholar]
- 11.Kothari MJ, Macintosh K, Heistand M, Logigian EL. Medial antebrachial cutaneous sensory studies in the evaluation of neurogenic thoracic outlet syndrome. Muscle Nerve. 1998;21:647–649. doi: 10.1002/(SICI)1097-4598(199805)21:5<647::AID-MUS13>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 12.Leffert R. Thoracic outlet syndrome and the shoulder. Clin Sports Med. 1983;2:439–452. [PubMed] [Google Scholar]
- 13.Leffert R. Thoracic outlet syndromes. Hand Clin. 1992;8:285–297. [PubMed] [Google Scholar]
- 14.Leffert R. The conundrum of thoracic outlet surgery. Tech Should Elb Surg. 2002;3:262–270. doi: 10.1097/00132589-200212000-00005. [DOI] [Google Scholar]
- 15.Leffert R. Complications of surgery for thoracic outlet syndrome. Hand Clin. 2004;20:91–98. doi: 10.1016/S0749-0712(03)00084-2. [DOI] [PubMed] [Google Scholar]
- 16.Leffert R, Perlmutter G. Thoracic outlet syndrome: Results of 282 transaxillary first rib resections. Clin Orthop Relat Res 1999:66–79. [PubMed]
- 17.Levin D, Nazarian L, Miller T, et al. Sono-graphic detection of lateral epicondylitis of the elbow. Radiology. 2005;237:230–234. doi: 10.1148/radiol.2371040784. [DOI] [PubMed] [Google Scholar]
- 18.Liu J, Tahmoush A, Roos D, et al. Shoulder-arm pain from cervical bands and scalene muscle anomalies. J Neurol Sci. 1995;128:175–180. doi: 10.1016/0022-510X(94)00220-I. [DOI] [PubMed] [Google Scholar]
- 19.Machleder H, Moll F, Verity M. The anterior scalene muscle in thoracic outlet compression syndrome: Histochemical and morphometric studies. Arch Surg. 1986;121:1141–1144. doi: 10.1001/archsurg.1986.01400100047009. [DOI] [PubMed] [Google Scholar]
- 20.MacKinnon S. Thoracic outlet syndrome. Ann Thorac Surg. 1994;58:287–289. doi: 10.1016/0003-4975(94)92194-6. [DOI] [PubMed] [Google Scholar]
- 21.Martinoli C, Bianchi S, Santacroce E, et al. Brachial plexus sonography: A technique for assessing the root level. AJR Am J Roetgenol. 2002;179:699–702. doi: 10.2214/ajr.179.3.1790699. [DOI] [PubMed] [Google Scholar]
- 22.Nazarian L. Top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI musculoskeletal imaging. AJR Am J Roetgenol. 2008;190:1621–1626. doi: 10.2214/AJR.07.3385. [DOI] [PubMed] [Google Scholar]
- 23.Ochi M, Ikuta Y, Watanabe M, et al. The diagnostic value of MRI in traumatic brachial plexus injury. J Hand Surg. 1994;19B:55–59. doi: 10.1016/0266-7681(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 24.Passero S, Paradiso C, Giannini F, Cioni R, Burgalassi L, Battistini N. Diagnosis of thoracic outlet syndrome. Relative value of electrophysiological studies. Acta Neurol Scand. 1994;90:179–185. doi: 10.1111/j.1600-0404.1994.tb02702.x. [DOI] [PubMed] [Google Scholar]
- 25.Peer S, Bodner G, Meirer R, Willeit J, Piza-Katzer H. Examination of postoperative peripheral nerve lesions with high-resolution sonography. AJR Am J Roetgenol. 2001;177:415–419. doi: 10.2214/ajr.177.2.1770415. [DOI] [PubMed] [Google Scholar]
- 26.Roos D. Thoracic outlet syndrome is underdiagnosed. Muscle Nerve. 1999;22:126–129. doi: 10.1002/(SICI)1097-4598(199901)22:1<126::AID-MUS21>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 27.Ruiz A. The influence of arm abduction on the anatomic relations of infraclavicular brachial plexus: An ultrasound study. Barcelona: University of Barcelona; 2008. [DOI] [PubMed] [Google Scholar]
- 28.Sanders R, Hammond S. Etiology and pathology. Hand Clin. 2004;20:23–26. doi: 10.1016/S0749-0712(03)00079-9. [DOI] [PubMed] [Google Scholar]
- 29.Shafighi M, Gurunluoglu R, Ninkovic M, et al. Ultrasonography for depiction of brachial plexus injury. J Ultrasound Med. 2003;22:631–634. doi: 10.7863/jum.2003.22.6.631. [DOI] [PubMed] [Google Scholar]
- 30.Spinner R, Amadio P. Compressive neuropathies of the upper extremity. Clin Plast Surg. 2003;30:155–173. doi: 10.1016/S0094-1298(02)00103-7. [DOI] [PubMed] [Google Scholar]
- 31.Stuart R, Koh E, Breidahl W. Sonography of peripheral nerve pathology. AJR Am J Roetgenol. 2004;182:123–129. doi: 10.2214/ajr.182.1.1820123. [DOI] [PubMed] [Google Scholar]
- 32.Thallaj A. Sonoanatomy of the brachial plexus with single broad band-high frequency (L17-5 Mhz) linear transducer. The Internet Journal of Anesthesiology 2007;11(2).
- 33.Veilleux M, Stevens JC, Campbell JK. Somatosensory evoked potentials: Lack of value for diagnosis of thoracic outlet syndrome. Muscle Nerve. 1988;11:571–575. doi: 10.1002/mus.880110608. [DOI] [PubMed] [Google Scholar]
- 34.Yang W, Chui P, Metreweli C. Anatomy of the normal brachial plexus revealed by sonography and the role of sonographic guidance in anesthesia of the brachial plexus. AJR Am J Roetgenol. 1998;171:1631–1636. doi: 10.2214/ajr.171.6.9843302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(MOV 92975 kb)