Abstract
Background
The purpose of this study was to assess the extent to which a supplemental radiographic view increases accuracy and confidence ratings when determining screw placement in volar plating of distal radius fractures for evaluators of different specialties and experience levels.
Methods
Thirty-four distal radius fractures treated with volar plate fixation were imaged using standard AP and lateral, and supplemental lateral tilt views. Each case was then evaluated for penetration of distal screw tips into the articular space. Sixty-five physicians then completed a two-phase analysis and survey of these cases. In the first phase, presentation consisted only of AP and lateral views; in the second, the lateral tilt view was added. Participants were asked to determine whether distal screws penetrated the joint and rate their confidence in the determination. Assessments were scored for correctness; changes in accuracy and confidence levels between phases were analyzed using paired t tests. Comparisons between groups were performed by ANOVA.
Results
Supplementation increased accuracy and confidence in all position, specialty, and experience groups. Confidence scores were significantly higher following evaluation of three views versus two views. Residents exhibited the greatest improvements in accuracy and confidence. For first-phase (standard view) assessments, accuracy scores were significantly better for attendings with less than 10 years post-fellowship experience than those with more.
Conclusions
A supplemental view of the distal radius combined with AP and lateral views significantly improves the ability of all evaluators, regardless of specialty or training level, to correctly assess placement of fixation screws. The greatest improvements are seen for resident trainees.
Keywords: Distal radius fracture, Volar plate, Fixation screw, Arthrodesis, Intra-articular, Tilt radiography, Fluoroscopy, Hardware placement, Postoperative evaluation, DVR plate
Introduction
Treating distal radius fractures with open fixation has become more popular in recent years [3]. Volar radial plates have been particularly favored, as volar placement reduces risk of extensor tendon damage often seen with dorsal fixation [4, 5]. However, the use of these plates poses a risk of articular penetration, since fixation requires close juxtaposition of the distal screw tips to the subchondral radial surface. Violation of the articular space can potentially result in a number of severe sequelae, including arthrosis [11].
Screw penetration of the articular space is believed to be a relatively common occurrence. A 2010 survey of 705 physicians who practice distal radius volar plate fixation found that 372 (52.7 %) believed that screw penetration of the joint occurred in 2 % or more of cases [11]. Data from previous studies supports this perception. One study examining screw placement during volar plating found intra-articular penetration of distal screws in eight of 128 cases (6.3 %), while in another report detailing cases of volar plate fixation, where complications necessitated hardware removal, three of the 28 cases (10.7 %) were due to screw tip penetration of the radiocarpal space [2, 8]. The perceived and reported frequency of this complication reinforces the importance of ensuring proper positioning of fixation screws during plate fixation.
Fluoroscopic imaging readily allows clinicians to view distal volar plate screw placement both in real time and from a variety of angles and is, thus, the preferred method for verifying proper positioning of hardware intraoperatively [11]. However, assessments of screw position during postoperative follow-up are often accomplished with the standard, static x-ray views: AP and lateral [8, 9, 11]. The irregular geometry of the distal radius coupled with the splayed arrangement of distal plate screws complicates attempts to visualize and evaluate screw position using only standard views and can result in incorrect assessments of articular screw penetration.
Previous work demonstrates that tilted-plane radiographic images, or images acquired with the arm inclined from the horizontal axis, allow for better visualization of surgical hardware placement when examined alongside standard AP and lateral views [1, 6]. Prior studies have also examined the diagnostic value of different radiological views to supplement AP and lateral views [1, 5, 6, 10]. However, there is a paucity of information with regards to how the advantages conferred by nonstandard radiological views translate to performance improvement for assessors when evaluating extra-articular placement of fixation screws. There is also no specific data on improvements in physicians of different specialties, or levels of training and experience.
This study examines the extent to which an additional, inclined radiographic view can improve accuracy and confidence of proper distal screw placement during volar plating of the distal radius. It further examines whether the advantages conferred by a third radiographic view differs between physicians of different specialties or experience levels.
Methods
Case Selection and Classification
Thirty-four distal radius fractures that had been internally fixed with DVR plates (Hand Innovations, Miami, FL, USA) placed through a flexor carpi radialis (FCR) approach were selected from the practice of one physician on the basis of static films obtained during the first postoperative visit. Cases were selected based on plate type and the presence of clear AP, lateral, and 30° tilted lateral radiographic views. Screw positioning outside the articular space had been confirmed for each case by live, rotational dynamic mini c-arm fluoroscopy both intraoperatively and during the first postoperative follow-up. This method, while not infallible in assessing the joint space, is noninvasive and has an approximate receiver operating characteristic area under curve (ROC-AUC) of 0.95 for a single pass compared to the gold standard of arthroscopy [10]. A panel of three physicians (one board-certified orthopedic hand surgeon, one surgical resident, and one orthopedic surgery resident) then categorized the assessment difficulty of each case by consensus as “easy” (n = 11), “intermediate” (n = 13), or “difficult” (n = 10) based on the clarity of the films and the angulation of the distal screws with respect to the articular surface.
Two-Phase Assessment of Radiographs
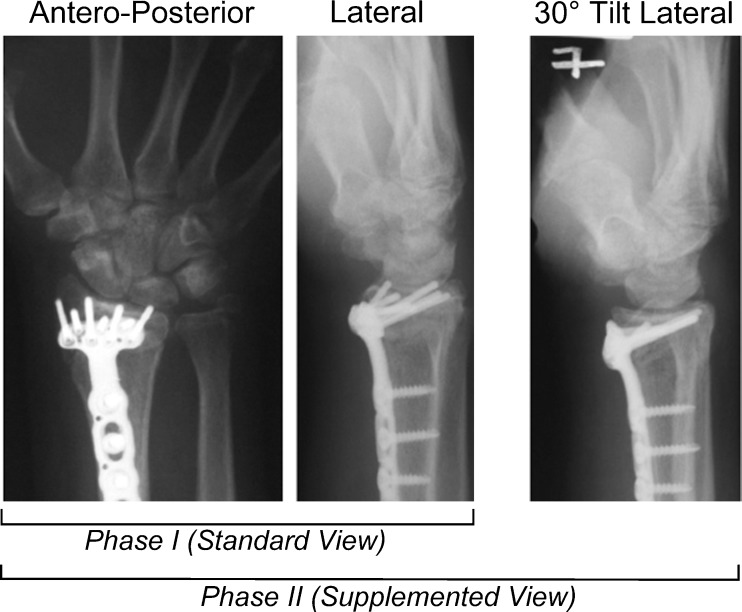
Sixty-five physicians including general orthopedists, hand surgeons, and radiologists at the attending and resident levels participated in a two-phase assessment battery in which they evaluated the postoperative radiographs from the 34 distal radius fractures. During each phase, cases were presented in random order. Participants were asked to determine if the distal fixation screws had penetrated the joint space (scoring: 0 = in joint; 1 = outside joint) and to rate the confidence in their answer on a scale of 1 to 5 (1 = not confident; 5 = extremely confident). In the first phase, cases were presented using two views: AP and lateral. During the second, or three-view phase, a 30° tilted lateral view was added to the two standard images (Fig. 1) [10]. Evaluators' assessments of screw positions for each phase were then scored. For each evaluator, overall accuracy scores were determined out of a possible 34 points (i.e., 1 point per correctly assessed case) or out 11, 13, and 10 for “easy,” “intermediate,” and “difficult” cases, respectively. The corresponding confidence rating in each determination was also recorded and summed for all cases and each for each difficulty category. Summed accuracy and confidence scores were used for subsequent statistical analyses.
Fig. 1.
Example of a single case as presented in the first and second phases of evaluation. Phase I presentation consists of two views (the standard AP and lateral); phase II comprises three views (standard views supplemented with a 30° tilt lateral view). In this case, the accuracy for all evaluators in assessing screw placement increased from 59.6 % in Phase I to 92.3 % in Phase II
Statistical Analyses
The mean and standard deviations of accuracy and confidence scores for each phase were calculated for the defined evaluator groups. The resulting data was examined in four ways: (1) combined performance of all evaluators, (2) comparison of all evaluators stratified by position (i.e., residents versus attendings), (3) comparison of all evaluators stratified by specialty (radiology, general orthopedics, and orthopedic hand surgery), and (4) comparison of fellow- and attending-level evaluators stratified by years of experience post-fellowship (two groups, cutoff level = 10 years). For these analyses, correct determination of screw placement and associated confidence scores were analyzed via paired t test; statistical significance was determined using a cutoff of p = 0.05. All p values were two sided. Accuracy and confidence score comparisons between groups were performed via ANOVA.
Results
Demographics
Of 65 physicians, there were 38 attendings, one fellow, and 26 residents. The mean age was 39.4 ± 10.7 years; mean experience was 6.6 ± 10.2 years. Attendings had a mean of 11.0 ± 11.1 years post-fellowship experience. By specialty, there were 17 radiologists, 30 general orthopedists, and 18 fellowship-trained hand surgeons (Table 1).
Table 1.
Demographic data of survey group
| Variable | Mean | SD | Frequency | Percent |
|---|---|---|---|---|
| Age (years) | 39.4 | 10.7 | ||
| Specialty | ||||
| Radiologist | 17 | 26.2 | ||
| General orthopedics | 30 | 46.2 | ||
| Orthopedic Hand Surgeon | 18 | 27.7 | ||
| Experience (years) | 6.6 | 10.2 | ||
| Experience post-fellowship (years; n = 39)a | 11.0 | 11.1 | ||
aYears of experience post-fellowship excludes residents
Overall Performance
For all cases, the 30° tilted lateral view improved evaluator accuracy scores from 19.98 to 26.34 points (58.8 to 77.5 %). Confidence ratings also rose significantly (18.7 points; p < 0.001). The additional view significantly increased correct assessments in all difficulty categories for all evaluators, with the greatest improvement for the 10 “difficult” cases (Table 2).
Table 2.
Accuracy scores and confidence ratings for all evaluators
| First phase—two images: mean ± SD | Second phase—three images: mean ± SD | Difference | p | |
|---|---|---|---|---|
| Correct score | All evaluators (n = 65) | |||
| All cases | 19.98 ± 4.51 | 26.34 ± 4.02 | +6.36 (18.7 %) | <0.001 |
| Easy | 9.49 ± 1.09 | 10.02 ± 0.91 | +0.53 (4.9 %) | <0.001 |
| Intermediate | 7.66 ± 2.22 | 9.48 ± 1.84 | +1.82 (14.0 %) | <0.001 |
| Difficult | 2.83 ± 2.04 | 6.85 ± 2.14 | +4.02 (40.2 %) | <0.001 |
| Confidence rating | ||||
| All cases | 115.6 ± 17.39 | 134.29 ± 17.83 | +18.69 | <0.001 |
| Easy | 42.43 ± 6.16 | 47.78 ± 5.50 | +5.35 | <0.001 |
| Intermediate | 41.66 ± 7.14 | 49.31 ± 7.03 | +7.65 | <0.001 |
| Difficult | 31.51 ± 5.84 | 37.20 ± 6.45 | +5.69 | <0.001 |
Performance by Position
When assessed by evaluator position (i.e., residents and attendings; the fellow was excluded from this portion of the study), the additional view yielded a significant increase in overall accuracy. Resident accuracy rose from 19.12 to 26.62 points (56.2 to 78.3 %). A significant improvement was observed for all difficulty categories with the greatest being a 51.5 percentage point increase improvement in “difficult” cases (an increase from 22.3 to 73.8 % correct). Resident confidence also increased significantly overall and within each category. Attendings exhibited significant overall accuracy improvement, increasing from 20.79 to 26.26 points (61.1 to 77.2 %) correct between phases. When stratified by case difficulty, significant improvements occurred in all three categories with the greatest change in “difficult” cases. Here, attendings realized a 32.4 percentage point accuracy increase with supplementation, from 32.9 to 65.3 % correct. Attendings' overall and category confidence ratings also increased. When accuracy and confidence for residents and attendings were compared, a significant difference was seen in first-phase assessment. Attendings exhibited significantly higher scores than residents for “difficult” cases. Otherwise, there were no differences (Table 3).
Table 3.
Accuracy scores and confidence ratings for evaluators by position
| First phase—two images: mean ± SD | Second phase—three images: mean ± SD | Difference | p | |
|---|---|---|---|---|
| Correct score | Residents (n = 26) | |||
| All cases | 19.12 ± 3.99 | 26.62 ± 3.89 | +7.50 (22.1 %) | <0.001 |
| Easy | 9.38 ± 1.06 | 9.96 ± 0.92 | +0.58 (5.2 %) | 0.008 |
| Intermediate | 7.50 ± 1.96 | 9.27 ± 1.61 | +1.77 (13.6 %) | <0.001 |
| Difficult | 2.23 ± 1.75 | 7.38 ± 2.04 | +5.15 (51.5 %) | <0.001 |
| Confidence rating | ||||
| All cases | 113.69 ± 18.03 | 132.27 ± 20.22 | +18.68 | <0.001 |
| Easy | 41.12 ± 6.70 | 46.65 ± 6.65 | +5.53 | <0.001 |
| Intermediate | 40.73 ± 7.19 | 48.69 ± 7.08 | +7.96 | <0.001 |
| Difficult | 31.85 ± 5.30 | 36.92 ± 7.41 | +5.07 | 0.001 |
| Correct score | Attendings (n = 38) | |||
| All cases | 20.79 ± 4.64 | 26.26 ± 4.15 | +5.52 (16.1 %) | <0.001 |
| Easy | 9.63 ± 1.05 | 10.05 ± 0.93 | +0.42 (3.9 %) | 0.016 |
| Intermediate | 7.87 ± 2.35 | 9.68 ± 1.96 | +1.81 (14 %) | <0.001 |
| Difficult | 3.29 ± 2.13 | 6.53 ± 2.18 | +3.24 (32.4 %) | <0.001 |
| Confidence rating | ||||
| All cases | 116.84 ± 17.30 | 136.24 ± 15.95 | +19.4 | <0.001 |
| Easy | 43.45 ± 5.71 | 48.79 ± 4.29 | +5.34 | <0.001 |
| Intermediate | 42.21 ± 7.22 | 49.92 ± 7.05 | +7.71 | <0.001 |
| Difficult | 31.18 ± 6.28 | 37.53 ± 5.84 | +6.35 | <0.001 |
The one fellow was excluded from the above analysis
Performance by Specialty
Separating performance data by specialty (radiology, general orthopedics, and orthopedic hand surgery) yielded significant accuracy improvements for almost all groups within combined and separate difficulty levels. The only exception was orthopedic hand surgeons, whose accuracy in evaluating “easy” cases was unchanged. For all specialties, the greatest improvements occurred in “difficult” cases. Confidence ratings for all groups increased significantly between phases, both overall and by difficulty level (Table 4). ANOVA revealed no differences in accuracy or confidence between groups (data not shown).
Table 4.
Accuracy scores and confidence ratings for evaluators by specialty
| First phase—two images: mean ± SD | Second phase—three images: mean ± SD | Difference | p | |
|---|---|---|---|---|
| Correct score | Radiology (n = 17) | |||
| All cases | 19.65 ± 5.10 | 26.82 ± 4.60 | +7.17 (21.1 %) | <0.001 |
| Easy | 9.41 ± 1.12 | 10.12 ± 0.60 | +0.71 (6.5 %) | 0.018 |
| Intermediate | 7.71 ± 2.66 | 9.88 ± 2.03 | +2.17 (16.7 %) | <0.001 |
| Difficult | 2.53 ± 2.15 | 6.82 ± 2.79 | +4.29 (42.9 %) | <0.001 |
| Confidence rating | ||||
| All cases | 118.53 ± 16.02 | 134.24 ± 15.63 | +15.71 | <0.001 |
| Easy | 42.06 ± 5.66 | 47.24 ± 5.29 | +5.21 | <0.001 |
| Intermediate | 43.06 ± 6.28 | 49.24 ± 5.85 | +6.18 | <0.001 |
| Difficult | 33.41 ± 5.97 | 37.76 ± 6.00 | +4.35 | 0.029 |
| Correct score | General orthopedics (n = 30) | |||
| All cases | 19.87 ± 4.61 | 26.17 ± 4.14 | +6.30 (18.6 %) | <0.001 |
| Easy | 9.50 ± 1.11 | 9.97 ± 1.03 | +0.47 (4.2 %) | 0.014 |
| Intermediate | 7.57 ± 2.16 | 9.10 ± 1.83 | +1.53 (11.8 %) | <0.001 |
| Difficult | 2.80 ± 2.11 | 7.10 ± 1.94 | +4.30 (43.0 %) | <0.001 |
| Confidence rating | ||||
| All cases | 112.93 ± 19.59 | 132.27 ± 21.37 | +19.34 | <0.001 |
| Easy | 41.90 ± 6.70 | 47.10 ± 6.47 | +5.20 | <0.001 |
| Intermediate | 40.37 ± 8.07 | 48.90 ± 7.98 | +8.53 | <0.001 |
| Difficult | 30.67 ± 6.61 | 36.27 ± 7.59 | +5.60 | <0.001 |
| Correct score | Orthopedic hand surgery (n = 18) | |||
| All cases | 20.50 ± 3.93 | 26.17 ± 3.38 | +5.67 (16.7 %) | <0.001 |
| Easy | 9.56 ± 1.10 | 10.00 ± 0.97 | +0.44 (4.1 %) | 0.134* |
| Intermediate | 7.77 ± 1.99 | 9.72 ± 1.64 | +1.95 (14.9 %) | 0.001 |
| Difficult | 3.17 ± 1.86 | 6.44 ± 1.82 | +3.27 (32.7 %) | <0.001 |
| Confidence rating | ||||
| All cases | 117.28 ± 14.78 | 137.72 ± 12.96 | +20.44 | <0.001 |
| Easy | 43.67 ± 5.83 | 49.44 ± 3.50 | +5.77 | <0.001 |
| Intermediate | 42.50 ± 6.20 | 50.06 ± 6.67 | +7.56 | <0.001 |
| Difficult | 31.11 ± 3.89 | 38.22 ± 4.66 | +7.11 | <0.001 |
*Not significant
Performance of Fellow- and Attending-Level Evaluators by Post-fellowship Experience
Stratifying the 38 attendings and one fellow by number of year, post-fellowship experience (i.e., those with less than 10 years versus 10 years or more) revealed significant improvements for both groups. Those with less experience showed a 14.4 percentage point increase in accuracy scores. Attendings with more experience exhibited an 18.6 percentage point increase. Confidence ratings also increased significantly for both experience groups for all cases and within each level of difficulty. The largest accuracy increase occurred for “difficult” cases. Evaluators with less experience showed a 32.5 percentage point increase, while those with more experience exhibited a 33.3 percentage point increase. Significant improvements were also seen in “intermediate cases” for both groups. “Easy” case accuracy did not increase in either group (Table 5). Comparing performance between groups revealed nearly no difference in accuracy scores or confidence ratings (data not shown). However, overall accuracy during the first phase for the group with less experience was significantly higher than that of the group with more (Table 5).
Table 5.
Accuracy scores and confidence ratings for postresidency evaluators by years of experience
| First phase—two images: mean ± SD | Second phase—three images: mean ± SD | Difference | p | |
|---|---|---|---|---|
| Correct score <10 years (n = 24) | ||||
| All cases | 21.92 ± 3.81 | 26.83 ± 3.75 | +4.91 (14.4 %) | <0.001 |
| Easy | 9.75 ± 1.03 | 10.13 ± 0.95 | +0.38 (3.4 %) | 0.095* |
| Intermediate | 8.42 ± 2.06 | 9.71 ± 2.10 | +1.29 (9.9 %) | 0.001 |
| Difficult | 3.75 ± 1.78 | 7.00 ± 1.62 | +3.25 (32.5 %) | <0.001 |
| Confidence rating | ||||
| All cases | 112.96 ± 18.73 | 137.17 ± 15.65 | +24.21 | <0.001 |
| Easy | 42.25 ± 6.66 | 48.83 ± 4.20 | +6.58 | <0.001 |
| Intermediate | 40.71 ± 7.68 | 50.42 ± 6.61 | +9.71 | <0.001 |
| Difficult | 30.00 ± 6.27 | 37.92 ± 6.19 | +7.92 | <0.001 |
| Correct score ≥10 years (n = 15) | ||||
| All items | 18.87 ± 5.22 | 25.20 ± 4.59 | +6.33 (18.6 %) | <0.001 |
| Easy | 9.40 ± 1.06 | 9.93 ± 0.88 | +0.53 (4.8 %) | 0.056* |
| Intermediate | 7.00 ± 2.51 | 9.47 ± 1.85 | +2.47 (19.0 %) | <0.001 |
| Difficult | 2.47 ± 2.42 | 5.80 ±2.70 | +3.33 (33.3 %) | <0.001 |
| Confidence rating | ||||
| All items | 121.27 ± 14.79 | 134.47 ± 16.32 | +13.20 | 0.002 |
| Easy | 44.33 ± 5.21 | 48.53 ± 4.50 | +4.20 | <0.001 |
| Intermediate | 44.07 ± 6.19 | 49.13 ± 7.64 | +5.06 | 0.005 |
| Difficult | 32.87 ± 5.90 | 36.80 ± 5.14 | +3.93 | 0.046 |
*Not significant
Discussion
This study highlights the importance of supplemental radiographic views for increasing the accuracy and confidence of clinical evaluators tasked with ensuring the proper positioning of radial volar plate screws in the postoperative period. When static radiography must be employed due the unavailability of a fluoroscope,we found that supplemental lateral tilt imaging can significantly increase evaluator accuracy and confidence in assessment. Our data further indicate that improved performance can be observed regardless of the evaluator's position, specialty, or post-fellowship experience, particularly for cases where the radiographic evaluation is challenging.
Our investigation also reveals clinician populations for whom supplementary tilted lateral imaging confers particular benefits. In evaluating “difficult” cases, mean resident accuracy following the introduction of the supplemental image rose approximately threefold (2.23 ± 1.75 to 7.38 ± 2.04; Table 3). This increase represented the largest observed improvement in accuracy between the first and second evaluation phases for any of the examined groups. This result is largely intuitive; residents generally have less experience reading radiographs than their more senior counterparts and are, thus, comparatively more prone to error when presented with limited information on a challenging case.
The marked improvement in the accuracy of resident evaluations for difficult cases given the added lateral tilt view strongly indicates acquisition of this view for clinic-based follow-up assessments of radial volar plating. Our data also revealed that for all cases, attending-level physicians with fewer than 10 years of post-fellowship experience were significantly more accurate in identifying screw position from the two standard orthogonal views than their more experienced counterparts. This may relate to that fact that volar plate fixation of distal radius fractures came into broad favor relatively recently. It is, thus, possible that this disparity in baseline evaluation accuracy is due to less experienced physicians having more direct exposure to the technique during the course of their training.
While the results of this study strongly suggest that additional static views should be standard for postoperative assessment, the type of view(s) that would provide the most useful information is still a matter of debate. Though we found appreciable improvements by employing a tilted lateral view to supplement the AP and lateral views, the proportion of correct assessments for all evaluators and for each of the evaluator subgroups ranged between 74.1 and 78.9 %; this corresponds to approximately 20–25 % of cases yielding assessment errors. It would, thus, be important to identify more informative radiographic views.
A number of previous studies have addressed the informative value of nonstandard radiographic vantages of the distal radius in assessing distal volar plate screw placement. Tilted lateral views have been previously scrutinized; prior cadaveric work indicated that while the 30° tilted lateral view we selected for this study was best suited for imaging radial-side distal plate screws, tilt views obtained at more acute angles of inclination (15 and 23°) provided clearer visualization of ulnar screws [10]. A second, retrospective study analyzed lateral tilt radiographs obtained by using the patient's uninjured contralateral fist as a pedestal for positioning the plated wrist for radiography. The authors reported that images suitable for analyzing distal screw arrangement were obtained in this fashion 96 % of the time, even though the angle of forearm inclination (as estimated in an uninjured control group) varied between 15 and 23° [6].
Augmenting standard views with images obtained in various degrees of pronation and supination have also been purported to improve the resolution of fixation screws. One study reported that in evaluating 48 cases of volar plate distal radius fixation, a 45° pronated view, in combination with 10° tilt AP and 20° tilt lateral views, increased evaluator confidence in determining screw position over the standard orthogonal views from 0 to 100 %, although the number and positions of evaluators was not specified [9]. Another study indicated that varying degrees of supination from lateral allowed for better imaging of the two radial distal screws, while pronation facilitated clearer views of ulnar screws [5]. Apart from changes in inclination or pronation/supination, recent work suggests that tangential radiographic views (i.e., obtained with the wrist in at least 70° flexion and the x-ray beam oriented roughly sagittal) are of great value in ruling out screw penetration of the dorsal radial cortex, particularly in the third and fourth dorsal compartments [7]. While our study did not specifically seek out the most informative radiographic view(s) for assessing screw penetration of the joint, a modified version of the tangential imaging technique may prove useful for visualizing the radiocarpal space. Alternatively, a view that incorporates both inclined tilt and pronation or supination may be of particular informative value.
Our work confirms the previously reported benefits of additional radiographic views to supplement the AP and lateral views when verifying proper volar plate fixation from static images. However, this study goes beyond prior work to systematically test image supplementation in a large and diverse population of clinical evaluators. In doing this, we reveal that significant improvements in accuracy and confidence are evident in physicians of varied expertise and levels of experience. Our analyses also identify groups for whom this additional information is particularly helpful; as a group, resident trainees stand to gain the greatest magnitude of improvement in both accuracy and confidence in their determinations. Though additional work is needed to identify the optimal supplementary view or views for volar plate screw placement, we show that even nonoptimal views confer significant positive changes in assessment quality. This, in turn, reduces the risk of complications from improper hardware placement.
Acknowledgments
Conflict of interest
None.
References
- 1.Boyer MI, Korcek KJ, Gelberman RH, et al. Anatomic tilt x-rays of the distal radius: an ex vivo analysis of surgical fixation. J Hand Surg Am. 2004;29(1):116–122. doi: 10.1016/j.jhsa.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Gyuricza C, Carlson MG, Weiland AJ, et al. Removal of locked volar plates after distal radius fractures. J Hand Surg Am. 2011;36(6):982–985. doi: 10.1016/j.jhsa.2011.03.032. [DOI] [PubMed] [Google Scholar]
- 3.Koval KJ, Harrast JJ, Anglen JO, et al. Fractures of the distal part of the radius. The evolution of practice over time. Where's the evidence? J Bone Joint Surg. 2008;90(9):1855–1861. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 4.Lutsky K, Boyer MI, Steffen JA, et al. Arthroscopic assessment of intra-articular distal radius fractures after open reduction and internal fixation from a volar approach. J Hand Surg Am. 2008;33(4):476–484. doi: 10.1016/j.jhsa.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 5.MaschkeSD EPJ, Schub D, et al. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand. 2007;2(3):144–150. doi: 10.1007/s11552-007-9038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matullo KS, Dennison DG. Lateral tilt wrist radiograph using the contralateral hand to position the wrist after volar plating of distal radius fractures. J Hand Surg Am. 2010;35(6):900–904. doi: 10.1016/j.jhsa.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Ozer K, Wolf JM, Watkins B, et al. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am. 2012;37(5):963–967. doi: 10.1016/j.jhsa.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 8.Pace A, Cresswell T. Use of articular wrist views to assess intra-articular screw penetration in surgical fixation of distal radius fractures. J Hand Surg Am. 2010;35(6):1015–1018. doi: 10.1016/j.jhsa.2010.03.041. [DOI] [PubMed] [Google Scholar]
- 9.Smith DW, Henry MH. The 45 pronated oblique view for volar fixed-angle plating of distal radius fractures. J Hand Surg Am. 2004;29(4):703–706. doi: 10.1016/j.jhsa.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Soong M, Got C, Katarincic J, et al. Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am. 2008;33(10):1720–1723. doi: 10.1016/j.jhsa.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Tweet ML, Calfee RP, Stern PJ. Rotational fluoroscopy assists in detection of intra-articular screw penetration during volar plating of the distal radius. J Hand Surg Am. 2010;35(4):619–627. doi: 10.1016/j.jhsa.2009.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]