Abstract
Enhancing the functioning of parents, teachers, juvenile justice authorities, and other health and mental heal professionals who direct children and adolescents to services is a major mental health services concern. The Gateway Provider Model is an elaborated testable subset of the Network-Episode Model (NEM; B. A. Pescosolido & C. A. Boyer, 1999) that synthesizes it with Decision (D. H. Gustafson, et al., 1999) and organizational theory (C. Glisson, 2002; C. Glisson & L. James, 1992, 2002). The Gateway Provider Model focuses on central influences that affect youth’s access to treatment, i.e., the individual who first identifies a problem and sends a youth to treatment (the “gateway provider”); and the need those individuals have for information on youth problems and relevant potential resources. Preliminary studies by the authors and other applicable studies (D. Carise & O. Gurel, 2003) show that providers’ perception of need, and their knowledge of resources, and their environment are related to the decision to offer or refer to services, supporting key aspects of the Model.
Keywords: service access, providers, service theory, youth, mental health
To reduce the gap between need and service access for children and adolescents with mental health problems, one must understand what determines or influences service use (Burns et al., 1995). Improvement in modeling youth’s access could uncover intervention points to improve their service access. A variety of models and theories purport to explain the receipt of health and mental health services. These include the “Behavioral Model” (Andersen, 1968, 1995); the Health Belief Model and Children’s Health Belief Model (Becker & Maiman, 1975; Bush & Iannotti, 1990; Janz & Becker, 1984); the Theory of Reasoned Action (Fishbein & Azjen, 1975); and, specifically for mental health services, the Network-Episode Model (NEM; Pescosolido, 1992; Pescosolido, Gardner, & Lubell, 1998), and the Children’s NEM (Costello, Pescosolido, Angold, & Burns, 1998). There are also more qualitatively oriented models, largely inductive and derived from patients and family member’s narratives of their illness experiences (e.g., Kleinman’s 1980 explanatory model of illness).
Although empirical studies using these models (largely the Andersen model) have explained some of the variance in service outcomes, none has emerged as thoroughly explanative. Typically, tests of Andersen’s model explain approximately 20% of the variance in service use (Mechanic, 1979; Phillips, Morrison, Andersen, & Aday, 1998). This poor explanatory power could be attributed to its focus on client variables. The NEM rose as an attempt to shift away from the individualistic and static focus on primarily client need and services seen in Andersen’s (1995) Behavioral Model, to a more community-based and process-oriented understanding of health service use (Costello et al., 1998).
The low percentage of explained variance in the one tested model and the continued need to explain variance indicates that important elements shaping the response to mental health problems still must be examined. In particular, those elements that would lend themselves to developing interventions to enhance service access remain to be identified as barriers or facilitators in the help-seeking process. An examination of the current state of knowledge about youth service access reveals potential factors that constitute a testable model: the Gateway Provider Model.
Youth usually do not seek services or treatment on their own. In line with the basic tenets of the NEM, youth tend to be directed to services by their parents, teachers, juvenile justice authorities, and other adults (Alegria et al., 1991; Bickman, Heflinger, Northrup, Sonnischsen, & Schilling, 1998; Burns & Friedman, 1990; Costello et al., 1998; Landsverk, 1995; Saunders, Resnick, Hoberman, & Blum, 1994; Wells et al., 1988), all of whom might be considered gateway providers (Flisher et al., 1997). These “gateway providers” might be informal (family or friends) or formal providers (mental health specialists or nonspecialists from primary health, child welfare, juvenile justice, or education) (Mechanic, Angel, & Davies, 1991). These lay and professional individuals’ knowledge and awareness of services and assessment of youth’s symptoms, diagnosis, and impairment are essential in recommending/suggesting services for youth (Costello et al., 1988; Horwitz, Leaf, Leventhal, Borsyth, & Speechley, 1992; Stiffman, Chen, Elze, Dorè, & Cheng, 1997). Because youth are minors, guardian permission is needed to access many services and insurance. Also, youth, even more than adults, may need the advice, encouragement, and guidance of others in their social network (informal gateway providers such as parents) in order to seek services (Landsverk, 1995). After family and friends, providers from formal nonspecialty sectors (social services, education, juvenile justice, primary health care) often have the first official service contact with the youth, identify the problem, provide some immediate services, and/or refer the youth to psychiatric or specialty mental health services. Even when these providers cannot offer direct mental health services, their actions in referral, consultation, and liaison qualify as quality care in so far as they help youth access mental health services (Creed, Gownsunkur, Russell, & Kincey, 1990; Hammer, Strain, & Lyons, 1991; Hatfield, Harrington, & Mohamad, 1996; Hoge & Howenstine, 1997; Lourie & Katz-Leavy, 1991; Vanstraelen & Cottrell, 1994).
The research literature consistently demonstrates low rates of identification and recognition on the part of potential gateway providers (Burns, Costello, Angold, Tweed, Stangl, Former, & Erklani, 1995; Commander, Dharan, Odell, & Surtees, 1997; Costello et al., 1988; Earls, Robins, Stiffman, & Powell, 1989; Srebnik, Cauce, & Baydar, 1996). Even when formal gateway providers are physicians or professionally trained others, they often do not recognize need (e.g., Costello et al., 1988; Earls et al., 1989; Goldberg & Huxley, 1980; Stiffman, Cheng, Chen, & Dorè, 1995; Stiffman, Dore´, Cunningham, & Earls, 1995). General practitioners, pediatricians, and primary health care providers consistently overlook 46–86% of existing mental health problems and diagnoses (Armstrong, Bird, Fry, & Armstrong, 1992; Burns et al., 1995; Commander et al., 1997; Costello et al, 1995; Creed et al., 1990; Earls et al., 1989; Farmer & Griffiths, 1992; Goldberg, 1984; Hammer et al., 1991; Horwitz et al., 1992). Whether gateway providers offer services depends on their recognition of need and their knowledge of such predisposing factors as culture, and the economic and environmental situation of the client (Costello, et al., 1988; Horwitz, et al., 1992; Zahner & Daskalakis, 1997).
However, gateway providers’ decisions are not only based on perceived need. Consistent with Andersen’s concept of perceived availability (Andersen, 1968), research has demonstrated the importance of gateway providers’ knowledge of the service system in obtaining services for their children (Bickman et al., 1998; Stiffman et al., 2000, 2001). Thus, even when need is identified and gateway providers decide that a youth should receive services; the actual or perceived lack of available mental health services and treatments presents barriers to actual service provision.
Organizational factors particularly, might influence the behavior of professional providers. Although there are only a few published studies on the influence of organizational factors on provider behavior (Glisson, 2002; Glisson & James, 1992, 2002), there are a number of conceptual articles indicating how provider environment might also shape gateway providers’ actions on behalf of youth (Hoge & Howenstine, 1997; Mechanic, 1979; Schorr, 1997). Social science research on provider environment in mental health care has concentrated on interorganizational relationships within and across service systems (Glisson & James, 1992, 2002); area characteristics (such as availability, accessibility, and cultural behaviors; McLafferty & Broe, 1990); social network mechanisms (such as linking functions of gateway providers; Gater et al., 1991; Goldberg & Huxley, 1980; Pescosolido, 1992); state and federal policies (Small, 1991); and legal constraints (English, 1986). These critical dimensions of environment fall into multiple dimensions that can be conceptualized broadly as the psychological impact of the environment on the individual (James, James, & Ashe, 1990), and the structure or culture of the organization (Kopelman, Brief, & Guzzo, 1990). These studies have focused on measurement and definitional issues (Ashkanasy, Broadfoot, & Falkus, 2000; Cooke & Szumal, 1993; Glisson & James, 2002). Although relatively few also include a study of provider behavior, the articles have consistently commented on the role of structural and psychological climate variables in influencing provider behavior (Brown & Leigh, 1996; Glisson & Hemmelgarn, 1998; Moos & Moos, 1998). Most recently, Glisson (2002) presented a conceptual model of organizational context that explicitly posits that organizational properties (culture and structure) influence provider individual and shared perceptions (psychological and organizational climate, respectively). His conceptual model states that, in turn, these perceptions influence work performance. The Gateway Provider Model recognizes both the organizational impact on provider behavior, and how its impact is joined by such important factors as recognition of need and knowledge of resources.
Although research has not examined the front line gateway providers’ connections to an integrated system, evaluations of system level interventions demonstrate a disjuncture between system level changes and clinical outcomes. Thus, system level changes may be too removed from gateway providers to affect their actions (Salzer & Bickman, 1997). But other factors may be at work. Pescosolido (1996) has suggested that focusing simply on the system-individual levels fails to capture the many mechanisms that link the two, including how system change (such as increased interorganizational linkages and communication) impacts front line providers.In a similar vein, Hohmann (1999) has suggested that the lack of positive effects may be due to the failure to examine processes.
A major mental health services concern, therefore, is to identify the factors associated with enhancing the quality of the functioning of gateway providers in mental health services. The New Freedom Commission on Mental Health (2003), the National Research Council (1995), and others (Glisson & Hemmelgarn, 1998) identified research on referral decisions as a major priority. The Gateway Provider Model provides a framework for this area of research.
THEORETICAL FRAMEWORK
The Gateway Provider Model
The Gateway Provider Model represents a synthesis and elaboration of two existing models useful for understanding critical elements of the route to care (Stiffman et al., 2000, 2001). One important feature of the NEM (Pescosolido, 1992; Pescosolido & Boyer, 1999) is its focus on the kinds of individuals who become involved in responding to a child’s mental health or drug problems. Specifically, the NEM suggests that members of the community and the treatment system can work together or in opposition to affect the provision of care and outcomes. Both the individuals’ social network in the community, and the culture and climate produced by treatment networks, result in treatment decisions that may or may not reflect the best options for clients (Pescosolido, 1992, 1996). Second, Decision theory (Albert, 1978; Chapman & Sonnenberg, 2000; Eddy, 1996) can be used to elaborate the NEM by clarifying how the provider decision-making process concerning services can be understood as a rationally based decision. The process links knowledge of resources to perceived need in deciding to provide a relevant and appropriate service. The Gateway Provider model draws insights from the NEM to understand which treatment and community interface factors need to be explicitly considered in the treatment decisions, whereas Decision theory describes the selection and matching process of those considerations in any intervention.
The NEM
The Children’s version of the NEM (Costello, Pescosolid et al., 1998) draws from the general idea that there are key individuals who come together to affect the response to children’s mental health problems. As demonstrated in a series of studies (e.g., Alegria, et al., 1991, 2002), the first persons in the “treatment” system are often not mental health specialists. Thus, the pathways that children travel into and through the mental health service system can be shaped by the gateway provider’s knowledge, attitudes, and preferences. Too often, however, these “gateway providers’ knowledge of resources and preferences may not reflect the actual resources available or best practices.” Thus, the NEM points to three important factors that need to be considered in an intervention. First, the initial contact person (i.e., the gateway provider) in the treatment system can play a critical role in shaping the child’s pathway through the system; affect their experiences in care, and potentially their outcomes. Second, unless the factors that are implicitly used in deciding on treatment options are made explicit, providers may draw from organizational routines and tacit knowledge, resulting in suboptimal decisions. Third, even with the development of an intervention designed to replace this informal decision-making process, it is important to understand if and how providers’ resource knowledge and organizational context support or hinder the care for the children and families involved.
In sum, the NEM suggests that interventions may be explicitly designed to affect the usual (and sometimes not-optimal) choices that occur in intervention settings. Although the NEM is sometimes misinterpreted as eliminating the need to consider rational choice-based theories, it is more accurately seen as a framework for examining how providers and families can move from a “business-as-usual,” culturally-based approach to the onset of mental health problems into a rational choice-based approach (Pescosolido, 1992). However, because the NEM focuses on the more usual way that individuals respond, rather than the factors that come into play when individuals shift into a rational choice-based mode of response, it does not offer an understanding of the factors that should be directly considered in the development of the intervention. This is where the inclusion of Decision theory in the Getaway Provider Model produces a new guiding approach. The Gateway Provider Model draws insight from theNEMto understand what environmental factors may affect provider behavior and from Decision Theory to suggest what factors providers could or should consider in making their treatment decisions.
Decision Theory
Decision theory is a group of related constructs that seek to describe how to choose a course of action when faced with alternatives and variable amount of knowledge about outcomes of alternatives (Raiffa, 1968, Resnik, 1987). The goal of a decision is to choose the best option available. To do that one must generate a list of options and evaluate the outcomes of each relative to one another (Edwards & Fasolo, 2001). To make decisions, a human must be able to input, output, store, and manipulate information, which humans can only do with limited amounts of data at any one time (Simon, 1990). Many studies have shown that, when there are multiple options, individuals cannot weigh them all (Albert, 1978). Decision theory clarifies which factors should be considered explicitly in the provider’s decision-making process (Chapman & Sonnenberg, 2000; Eddy, 1996).
Gateway providers, who first recognize the need of the individual in need, must delineate a set of choice options by paring down the cues and the referral options to those most relevant and productive (Gustafson et al., 1999). This occurs whether the provider is a parent or a professional. In fact, it occurs for all decisions, not only service decisions. To make a service decision, the gateway provider must weigh the youth’s needs with detailed information about various treatment and referral options. Many communities literally have thousands of potential referral options, about which any one individual can know only a few. Yet quality care demands choosing themost appropriate treatment or referral. In this era of computers and handheld devices, physicians are often aided in such decisions by computerized software concerning drug treatments and drug interactions. The medical literature supports the need and effectiveness of these forms of decision support systems (e.g., Gerbert, Bronstone, Maurer, Hofmann, & Berger, 1999; Gustafson et al., 1999; Kvedar, 2000). Despite this, little has been extrapolated concerning the need for decision support systems related to referrals, nonmedication treatments, or their use by gateway providers.
The Testable Synthesis: The Gateway Provider Model
Drawing from the NEM and Decision theory, the Gateway Provider Model focuses on three central influences that affect the treatment children receive. First, it incorporates the NEM concept of the key role of the individual, often not in the mental health system or not even a formal provider, who initiates or directs the trajectory of treatment. This person is referred to as the gateway provider. Second, it recognizes, from Decision theory, that if providers are given more information than is embedded in their provider networks, and, if that information can be narrowed to only a relevant subset based on identified client needs, providers may offer better and more consistent advice, options, assistance, and referrals. This would then improve the quality of care offered to clients. Third, as illustrated in the organizational literature (Glisson, 2002), providers’ attitudes, impressions of support for treatment, and system burden can facilitate or hinder the implementation of new approaches in treatment systems.
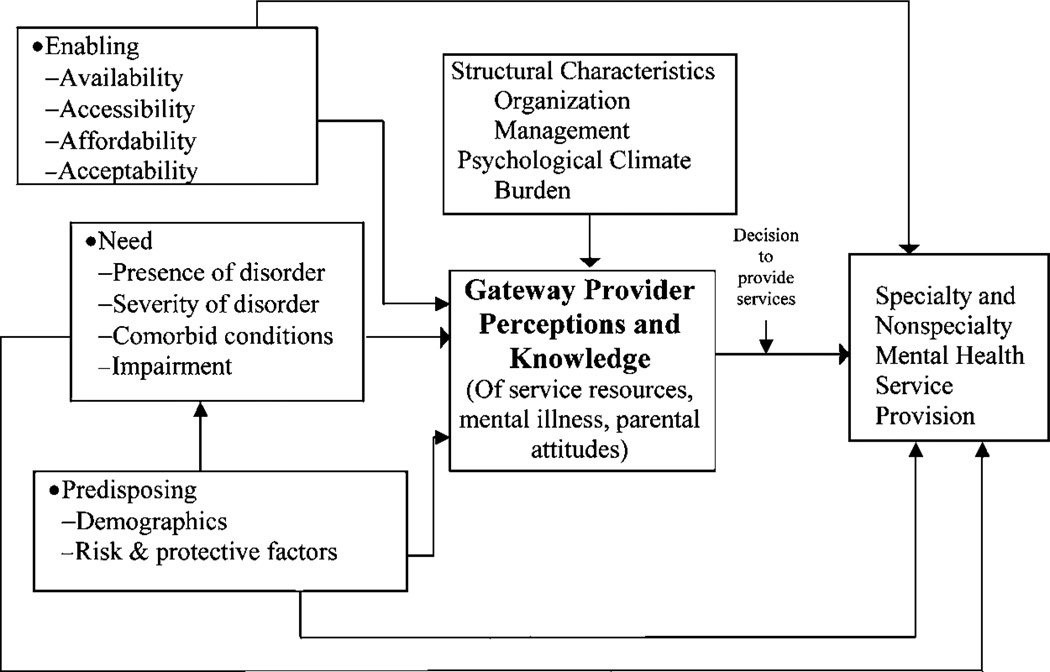
Figure 1 illustrates the Gateway Provider Model as it synthesizes the NEM and the Decision-making models, and adds organizational dimensions. The model in Figure 1 shows that client need, enabling and predisposing factors contribute directly to service use. However, as Pescosolido posits, the gateway provider perceptions of those factors mediate their impact on service use. In turn, as the organizational literature postulates, gateway provider perceptions and knowledge are influenced by the structural and systemic characteristics of their environment. Together, the gateway provider’s perceptions, knowledge, and environment influence their decision-making surrounding service provision. Decision making theory is applicable to the link between perception and services, as it explains how providers must pick, from the range of known services, those services that are relevant to the provider’s perception of the client’s problems. A wider range of known services assures more likelihood that a relevant service can be found and provided.
Fig. 1.
Gateway provider service framework.
Preliminary Research Support for the Gateway Provider Model
This model has received support from three prior studies by one of the authors, and by the TECH study (Carise & Gurel, 2003). Stiffman’s studies attempt to clarify the relationship between need and mental health service use, by examining the role of providers in moderating the gap between youth’s need for services and their receipt of services. These studies used the core variables of need and provider context, as posited in the latest version of the Andersen model, and the provider perception of need, as posited in the NEM. The central hypothesis for the analyses theorized that provider perceptions were influenced more by their own personal factors (knowledge and training) and work environment (the organizational predisposing and enabling factors of burden and resource knowledge) than by client problems. Youth self reported mental health and provider training were posited to contribute to service provision directly and through their influence on providers’ perceptions of youth’s mental health and provider knowledge of resources.
The first study was known as the Gateways and Pathways Project (GAPP) and funded by NIMH (Stiffman et al., 2000, 2001). Interviews with youth who were involved with St. Louis public health, juvenile justice, child welfare, or education service sectors revealed that 282 youth had received some services from 533 providers. Interviews with 222 providers focused on their reports of youth service need, service use, and provider’ knowledge and behavior. Structural Equation Modeling (SEM) tested elements of the gateway provider model (Hatcher, 1994). The model explained 55% of the variance in service provision, derived from provider perception of need (.54), provider knowledge of resources (.26), and provider burden (−.14). There were no direct paths from youth self report of mental health or provider training to services. The study clearly demonstrated, through the nonsignificant relationship between youth’s self reported mental health and service provision, that service provision was not based on clients’ self-reported problems. Instead, service provision appeared to be based primarily on provider assessment and provider knowledge of resources.
The second study used to test the Gateway Provider Model is currently in the field, with three waves of data and provider interviews completed. The American Indian Multisector Help Inquiry (AIM-HI) is a NIDA-funded study of service use and drug-use information in two American Indian populations, one urban and one reservation-based. A sample of 401 youth (about 200 from each area, aged 12–19) was first interviewed in person in 2001 (Stiffman, Striley, Brown, Limb, & Ostmann, 2003). Similar to the GAPP study, youth were asked to name those individuals who helped them with their mental health and addictions problems in the last year. The AIM-HI study included professional providers, like the GAPP study, but also added informal providers and traditional healers. Interviews with 190 providers, who offered services to 212 youth, revealed that their knowledge of resources was significantly correlated with any service provision (R2 = .45) (Stiffman et al., 2002). It was associated with direct provision at a somewhat lower level (R2 = .34) than with referral or recommendations (R2 = .47). Further, knowledge of resources was significantly associated with provider perception of mental health problems (R2 = .19). Multiple regressions showed that 23% of the variance in referred or recommended services was predicted by provider perception of mental health problems (14% unique) and by provider knowledge of resources (5% unique).
The third study focused largely on Decision theory’s assumption that improved information, accompanied by the means to narrow relevant subsets of information would aid appropriate decision making. This brief quality of care pilot gave five child welfare workers a handheld device preprogrammed with youth assessment questions keyed to over 1,000 local resources (Stiffman, Foster, Hamburg, & Dore, 2003). In a 2-month pilot, those workers with such a device, as opposed to those without the device, increased their identification of both youth and parent problems and increased their service actions (primary referrals) on the part of both youth and their parents.
The TECH study findings actually led to the ideas for the handheld study discussed above. The TECH study found that, when addiction providers used laptops that contained assessment devices and information about resources and treatment planning, there was “(a) a better match between the needs of patients and the services they receive and (b) a higher number of services delivered to patients.” (Carise & Gurel, 2003, p. 187).
The results of all the above studies followed the general pattern of the Gateway Provider Model posited in Fig. 1. The tests of the Gateway Provider Model, one using structural equation modeling to examine the joint contribution of youth and provider perspectives on the provision of services and the other using multivariate regression from only the provider perspective, explained 55 and 23%, respectively, of the variance in services. Further, an intervention to increase assessment of need and decisions concerning choosing relevant resources did increase need identification and referral actions. Critical to the decision to offer services in all the studies was the providers’ perception of need and knowledge of resources.
DISCUSSION
The Gateway Provider Model, when tested in a manner consistent with Pescosolido (Pescosolido, 1996; Pescosolido & Boyer, 1999) and Hohmann’s (Hohmann, 1999) inclusion of provider variables, explains substantial portions of the variance in service provisions. Also, as a subset of the NEM, it is much simpler. Unique to the Gateway Provider Model is the focus on a testable subset of the NEM variables, including client need, and organizational context, providers’ knowledge and perception and the inclusion of Decision theory principles. The largest predictor of service provision is the providers’ perception of youth mental health; their knowledge of resources is a close second. The more knowledge of mental health resources the provider has, the more likely he/she is to provide services. Also, the use of computerized aids providing knowledge of resources and then in narrowing the resources to those relevant according to an assessment, increased service provision by nonspecialist professionals. However, this relationship is far from perfectly explained by those two variables.
Consistent with Glisson’s conceptual proposals (Glisson & James, 1992) the organizational context of provider burdens explains additional variance in service provision. The greater the burdens (i.e. caseload), the less likely a provider is to offer services. Unfortunately, none of the studies supporting the Gateway Provider Model specifically measured the key theoretical organizational variables presumed to also influence provider behavior: culture, climate, and interorganizational linkages (Glisson, 2002). The studies’ findings, however, did support the inclusion of Decision theory and organizational theory in the Gateway Provider Model, as knowledge and burden both explained variance in service provision. Further studies better specifying the organizational context of professional gateway providers is clearly indicated.
The strong and direct role of gateway provider assessments and knowledge supports the NEM’s hypothesis that providers play a key role in determining service access for youth (Costello et al., 1998; Bickman et al., 1998; Burns & Friedman, 1990). The results show that any formulation of a model or heuristic for mental health services must include the pivotal role of gateway providers. Such a role goes far beyond a simple assessment of objective need, and operates independently of individuals’ assessment of their own need for service. Although further tests of the utility of this model in other settings and with other populations are required, clearly no model of service use can ignore the role of gateway providers. The provider’s assessment of the youth’s mental health problems, rather than the youth’s self-reported problems, is related to both direct provision of services and referral or recommendation to other services. Gateway providers may be more likely to both identify youth’s problems and refer youth to services when two pieces of information are in place: (1) knowledge of community resources available to youth; and (2) knowledge of brief, accurate screening devices. It is possible that gateway providers are reluctant to even identify problems if they know of no resources to serve the problem.
The studies we discussed also indicate why policies that enhance resource connectivity at the administrative or financial level, such as those instituted under the NIMH Child and Adolescent Service System Project (CAASP) movement (Lourie & Katz-Leavy, 1991), may not have been as effective as planned in increasing youth’s access to service. Unless the knowledge of those linkages and services get translated into the provider level they may not impact service use (Friedman, 1986).
Further, the testing of decision-making devices (Carise & Gruel, 2003; Stiffman et al., 2000; Stiffman et al., 2001) support the idea that decision-making surrounding service provision is based on selecting a narrow range of appropriate services from the providers wider range of known services. These studies demonstrate that decision-making aids that provide more information concerning service availability and help providers narrow that information to a smaller relevant appropriate range will enhance the decision to provide services. With the advent of web-based sources, such decision-making aids might become publicly available to informal providers (i.e., parents or friends) from their homes, as well as be provided by agencies to formal providers.
In sum, policies that enhance provider connections with and knowledge of other resources would likely affect service provision. Child welfare, juvenile justice, education and health care targeting youth should consider establishing mutual relationships. Gateway providers who know the service community may be more likely to both identify youth problems and refer youth to needed services. If provider knowledge of and contact with mental health resources can be enhanced, their ability tomake quality care decisions in offering services will increase.
REFERENCES
- Albert DA. Decision theory in medicine: A review and critique. Health and Society. 1978;56(3):362–401. [PubMed] [Google Scholar]
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, et al. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatric Services. 2002;53(12):1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alegria M, Robles R, Freeman DH, Vera M, Jimenez AL, Rios C, et al. Patterns of mental health utilization among island Puerto Rican poor. American Journal of Public Health. 1991;81:875–879. doi: 10.2105/ajph.81.7.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. Behavioral model of family’s use of health services: Research series, 25. Chicago, IL: University of Chicago, Center for Health Administration Studies; 1968. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Armstrong D, Bird J, Fry J, Armstrong P. Perspectives of psychological problems in general practice: A comparison of general practitioners and psychiatrists. Family Practice. 1992;9(2):173–176. doi: 10.1093/fampra/9.2.173. [DOI] [PubMed] [Google Scholar]
- Ashkanasy NM, Broadfoot LE, Falkus S. Questionnaire measures of organizational culture. In: Ashkanasy NM, Wilderom CPM, Peterson MF, editors. Handbook of organizational culture and climate. Thousand Oaks, CA: Sage; 2000. pp. 131–146. [Google Scholar]
- Becker MH, Maiman LA. Sociobehavioral determinants of compliance with health and medical care recommendations. Medical Care. 1975;13(1):10–24. doi: 10.1097/00005650-197501000-00002. [DOI] [PubMed] [Google Scholar]
- Bickman L, Heflinger CA, Northrup D, Sonnischsen S, Schilling S. Long term outcomes to family caregiver empowerment. Journal of Child and Family Studies. 1998;7:269–282. [Google Scholar]
- Brown SP, Leigh TW. A new look at psychological climate and its relationship to job involvement, effort, and performance. Journal of Applied Psychology. 1996;81:358–368. doi: 10.1037/0021-9010.81.4.358. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Friedman RM. Examining the research base for child mental health services and policy. Journal of Mental Health Administration. 1990;17:87–98. doi: 10.1007/BF02518583. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EMZ, et al. Children’s mental health service use across service sectors. Health Affairs. 1995;14:147–159. doi: 10.1377/hlthaff.14.3.147. [DOI] [PubMed] [Google Scholar]
- Bush PJ, Iannotti RJ. A children’s health belief model. Medical Care. 1990;28(1):69–83. doi: 10.1097/00005650-199001000-00008. [DOI] [PubMed] [Google Scholar]
- Carise D, Gurel O. Benefits of integrating technology with treatment: The DENS Project. In: Sorenson J, Rawson R, Guydish J, Zweben J, editors. Drug abuse treatment through collaboration: Practice and research partnerships at work. Washington, DC: American Psychological Association; 2003. pp. 181–195. [Google Scholar]
- Chapman GB, Sonnenberg FA. Decision making in health care: Theory, psychology, and applications. New York: Cambridge University Press; 2000. [Google Scholar]
- Commander MJ, Dharan SP, Odell SM, Surtees PG. Access to mental health care in an inner-city health district. II: Association with demographic factors. British Journal of Psychiatry. 1997;170:317–320. doi: 10.1192/bjp.170.4.317. [DOI] [PubMed] [Google Scholar]
- Cooke RA, Szumal JL. Using the organizational culture inventory to understand the operating cultures of organizations. In: Ashkanasy NM, Wilderom CPM, Peterson MF, editors. Handbook of organizational culture and climate. Thousand Oaks, CA: Sage; 1993. pp. 147–162. [Google Scholar]
- Costello EJ, Burns BJ, Angold A, Leaf PJ. How can epidemiology improve mental health services for children and adolescents? Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(6):1106–1115. doi: 10.1097/00004583-199311000-00002. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Burns BJ, Costello AJ, Edelbrock C, Dulcan M, Brent D. Service utilization and psychiatric diagnosis in pediatric primary care: The role of the gatekeeper. Pediatrics. 1988;82(3/2):435–441. [PubMed] [Google Scholar]
- Costello EJ, Pescosolido BA, Angold A, Burns BJ. A family network-based model of access to child mental health services. Research in Community and Mental Health: Social Networks and Mental Illness. 1998;9:165–190. [Google Scholar]
- Creed F, Gownsunkur J, Russell E, Kincey J. General practitioner referral rates to district psychiatry and psychology services. British Journal of General Practice. 1990;40:450–454. [PMC free article] [PubMed] [Google Scholar]
- Earls FJ, Robins LN, Stiffman AR, Powell J. Comprehensive health care for high-risk adolescents: An evaluation study. American Journal of Public Health. 1989;79:999–1005. doi: 10.2105/ajph.79.8.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy DM. Clinical decision making from theory to practice: A collection of essays from the Journal of the American Medical Association. Sudbury, MA: Jones and Bartlett; 1996. [Google Scholar]
- Edwards W, Fasolo B. Decision technology. Annual Review of Psychology. 2001:581–605. doi: 10.1146/annurev.psych.52.1.581. [DOI] [PubMed] [Google Scholar]
- English A. Adolescent health care: Barriers to access: Consent, confidentiality, and payment. Clearinghouse Review, Summer. 1986:481–490. [Google Scholar]
- Farmer AE, Griffiths H. Labeling and illness in primary care: Comparing factors influencing general practitioners’ and psychiatrists’ decisions regarding patient referral to mental illness services. Psychological Medicine. 1992;22:717–723. doi: 10.1017/s0033291700038150. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Azjen I. Belief, attitude, intention and behavior. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Flisher AJ, Kramer RA, Grosser RC, Alegria M, Bird HR, Bourdon KH, et al. Correlates of unmet need for mental health services children and adolescents. Psychological Medicine (QER) 1997;27:1145–1154. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Friedman RM. Major issues in mental health services for children. Sixth annual meeting of the American College of Mental Health Administration, (San Diego, California) Administration in Mental Health. 1986;14(1):6–13. [Google Scholar]
- Gater R, De Almeida B, Sousa E, Barrientos G, Caraveo C, Chandrashekar C, et al. The pathways to psychiatric care: A cross-cultural study. Psychological Medicine. 1991;21:761–744. doi: 10.1017/s003329170002239x. [DOI] [PubMed] [Google Scholar]
- Gerbert B, Bronston A, Maurer T, Hofmann R, Berger T. Decision support software to help primary care physicians triage skin cancer: A pilot study. Archives of Dermatology. 1999;135:187–192. doi: 10.1001/archderm.136.2.187. [DOI] [PubMed] [Google Scholar]
- Glisson C. The organizational context of children’s mental health services. Clinical Child and Family Psychology Review. 2002;5(4):233–253. doi: 10.1023/a:1020972906177. [DOI] [PubMed] [Google Scholar]
- Glisson C, Hemmelgarn A. The effects of organizational climate and interorganizational coordination on the quality and outcomes of children’s service systems. Child Abuse and Neglect. 1998;22(5):401–421. doi: 10.1016/s0145-2134(98)00005-2. [DOI] [PubMed] [Google Scholar]
- Glisson C, James L. The interorganizational coordination of services to children in state custody. Administration in Social Work. 1992;16(3/4):65–79. doi: 10.1300/j147v16n03_05. [DOI] [PubMed] [Google Scholar]
- Glisson C, James L. The cross-level effects of culture and climate in human service teams. Journal of Organizational Behavior. 2002;23(6):1099–1379. [Google Scholar]
- Goldberg D. The recognition of psychiatric illness by non-psychiatrists. Australian and New Zealand Journal of Psychiatry. 1984;18:128–133. doi: 10.3109/00048678409158781. [DOI] [PubMed] [Google Scholar]
- Goldberg DP, Huxley P. The pathway to psychiatric care. London: Tavistock Press; 1980. [Google Scholar]
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F. Impact of a patient-centered, computer-based health information/support system. American Journal of Preventative Medicine. 1999;16(1):1–9. doi: 10.1016/s0749-3797(98)00108-1. [DOI] [PubMed] [Google Scholar]
- Hammer JS, Strain JT, Lyons JS. Health service delivery and research outcomes of a common departmental structure for psychiatric consultation-liaison and social work services at a university hospital. General Hospital Psychiatry. 1991;13:95–105. doi: 10.1016/0163-8343(91)90020-w. [DOI] [PubMed] [Google Scholar]
- Hatcher L. A step by step approach to using the SAS System for factor analysis and structural equations modeling. Cary, NC: SAS Institute, Inc; 1994. [Google Scholar]
- Hatfield B, Harrington R, Mohamad H. Staff looking after children in local authority residential units: The interface with child mental health professionals. Journal of Adolescence. 1996;19:127–139. doi: 10.1006/jado.1996.0013. [DOI] [PubMed] [Google Scholar]
- Hoge MA, Howenstine RA. Organizational development strategies for integrating mental health services. Community Mental Health Journal. 1997;33:175–187. doi: 10.1023/a:1025044225835. [DOI] [PubMed] [Google Scholar]
- Hohmann AA. A contextual model for clinical mental health effectiveness research. Mental Health Services Research. 1999;1:83–91. [Google Scholar]
- Hollingshead AB. Four factor index of social status. New York: Wiley; 1975. [Google Scholar]
- Horwitz SM, Leaf PJ, Leventhal JM, Borsyth B, Speechley KN. Identification and management of psychosocial and developmental problems in community-based, primary care pediatric practices. Pediatrics. 1992;89:480–485. [PubMed] [Google Scholar]
- James LR, James LA, Ashe DK. The meaning of organizations: The role of cognition and values. In: Schneider B, editor. Organizational climate and culture. San Francisco: Jossey Bass; 1990. pp. 40–84. [Google Scholar]
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Patients and healers in the context of culture: An exploration of the borderline between anthropology, medicine and psychiatry. Berkeley, CA: University of California Press; 1980. [Google Scholar]
- Kopelman RE, Brief AP, Guzzo RA. The role of climate and culture in productivity. In: Schneider B, editor. Organizational climate and culture. San Francisco: Jossey-Bass; 1990. pp. 282–318. [Google Scholar]
- Kvedar JC. Decision support is changing health care. Archives of Dermatology. 2000;136:249. doi: 10.1001/archderm.136.2.249. [DOI] [PubMed] [Google Scholar]
- Landsverk J. Design and assessment issues in conducting longitudinal outcome studies of children in welfare systems. In: Vecchiato T, editor. Social research methods for the evaluation of social services. Padua: Fondazione Emanuela Zancan; 1995. pp. 52–65. [Google Scholar]
- Lourie IS, Katz-Leavy J. New directions for mental health services for families and children. Families in Society: The Journal of Contemporary Human Services. 1991 May;:277–285. [Google Scholar]
- McLafferty S, Broe D. Patient outcomes and regional planning of coronary care services: A location-allocation approach. Social Sciences and Medicine. 1990;30(3):297–304. doi: 10.1016/0277-9536(90)90185-u. [DOI] [PubMed] [Google Scholar]
- Mechanic D. Correlates of physician utilization: Why do major multivariate studies of physician utilization find trivial psychosocial and organizational effects? Journal of Health and Social Behavior. 1979;20:387–396. [PubMed] [Google Scholar]
- Mechanic D, Angel R, Davies L. Risk and selection processes between the general and the specialty mental health sectors. Journal of Health and Social Behavior. 1991;32:49–64. [PubMed] [Google Scholar]
- Moos RH, Moos BS. The staff workplace and the quality and outcome of substance abuse treatment. Journal of Studies on Alcohol. 1998;59:43–51. doi: 10.15288/jsa.1998.59.43. [DOI] [PubMed] [Google Scholar]
- New Freedom Commission on Mental Health. Achieving the promise: Transforming mental health care in America. Rockville, MD: 2003. Final Report; DHHS Pub. No SMA-03-3832. [Google Scholar]
- Pescosolido BA. Beyond rational choice: The social dynamics of how people seek help. American Journal of Sociology. 1992;97:1096–1138. [Google Scholar]
- Pescosolido BA. Bringing the “Community” into utilization models. Research in the Sociology of Health Care. 1996;13A:171–197. [Google Scholar]
- Pescosolido BA, Boyer CA. How do people come to use mental health services? Current knowledge and changing perspectives. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social contexts, theories, and systems. New York: Cambridge University Press; 1999. pp. 392–411. [Google Scholar]
- Pescosolido BA, Gardner CB, Lubell KM. How people get into mental health services: Stories of choice, coercion and “muddling through” from “first-timers.”. Social Science and Medicine. 1998;46(2):275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: Assessing environmental and provider-related variables in the behavioral model of utilization. Health Services Research. 1998;33(3):571–596. [PMC free article] [PubMed] [Google Scholar]
- Raiffa H. Decision analysis: Introductory lectures on choices under uncertainty. Oxford: England Addison-Wesley; 1968. [PubMed] [Google Scholar]
- Resnik MD. Choices: An introduction to decision theory. Minneapolis, MN: University of Minnesota Press; 1987. [Google Scholar]
- Salzer MS, Bickman L. Delivering effective children’s services in the community: Reconsidering the benefits of system interventions. Applied and Preventive Psychology. 1997;6:1–13. [Google Scholar]
- Saunders S, Resnick M, Hoberman HM, Blum R. Formal help-seeking behavior of adolescents identifying themselves as having mental health problems. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(5):718–728. doi: 10.1097/00004583-199406000-00013. [DOI] [PubMed] [Google Scholar]
- Schorr LB. Common purpose. New York: Doubleday; 1997. [Google Scholar]
- Simon HA. Invariants of human behavior. Annual review of psychology. 1990;41:1–19. doi: 10.1146/annurev.ps.41.020190.000245. [DOI] [PubMed] [Google Scholar]
- Small MA. Obstacles and advocacy in children’s mental health services: Managing the Medicaid maze. Behavioral Sciences and the Law. 1991;9:179–188. doi: 10.1002/bsl.2370090207. [DOI] [PubMed] [Google Scholar]
- Srebnik D, Cauce AM, Baydar N. Help-seeking pathways for children and adolescents. Journal of Emotional and Behavioral Disorders. 1996;4(4):210–220. [Google Scholar]
- Stiffman AR, Brown E, Striley C, Limb G, Nelson J, Pescarino R. Youths’ treatment needs and access: contrasts in African American and American Indian experiences. San Diego, CA: Oral Presentation at Society of Social Work Research Conference; 2002. [Google Scholar]
- Stiffman AR, Chen YW, Elze D, Dorè P, Cheng LC. Adolescents’ and providers’ perspectives on the need for and use of mental health services. Journal of Adolescent Health. 1997;21(5):335–342. doi: 10.1016/S1054-139X(97)00046-3. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Cheng LC, Chen YW, Dorè P. Social workers as gatekeepers of mental health services for teens; Washington, DC. Paper presented at the annual meeting of the American Public Health Association; October 30-November 3.1995. [Google Scholar]
- Stiffman AR, Dorè P, Cunningham RM, Earls F. Person and environment in HIV risk behavior change between adolescence and young adulthood. Health Education Quarterly. 1995;22(2):233–248. doi: 10.1177/109019819502200209. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Foster K, Hamburg K, Dore P. IMPROVE: A software program to improve assessments and multisector referrals; Tampa, FL. Oral presentation at the annual research conference of The Research and Training Center for Children’s Mental Health.2003. [Google Scholar]
- Stiffman AR, Hadley-Ives E, Dore P, Polgar M, Horvath VE, Striley C, et al. Youths’ access to mental health services: The role of providers’ training, resource connectivity, and assessment of need. Mental Health Services Research. 2000;2:141–154. doi: 10.1023/a:1010189710028. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Striley CW, Brown E, Limb G, Ostmann E. American Indian youth: Southwestern urban and reservation youth’s need for services and whom they turn to for help. Journal of Child and Family Studies. 2003;12:319–333. [Google Scholar]
- Stiffman AR, Striley CW, Horvath V, Hadley-Ives E, Polgar M, Elze D, et al. Organizational context and provider perception as determinants of mental health service use. The Journal of Behavioral Health Services and Research. 2001;28(2):1–17. doi: 10.1007/BF02287461. [DOI] [PubMed] [Google Scholar]
- Vanstraelen M, Cottrell D. Child and adolescent mental health services: Purchasers’ knowledge and plans. BMJ. 1994;309:259–261. doi: 10.1136/bmj.309.6949.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KB, Golding JM, Hough RI, et al. Factors affecting the probability of youth of general and medical health and social/community services for Mexican Americans and non-Hispanic Whites. Medical Care. 1997;26:441–452. doi: 10.1097/00005650-198805000-00001. [DOI] [PubMed] [Google Scholar]
- Zahner GEP, & Daskalakis C. Factors associated with mental health, general health, and school-based service use for child psychopathology. American Journal of Public Health. 1997;87(9):1440–1448. doi: 10.2105/ajph.87.9.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]