Abstract
Purpose
To describe women’s condom use patterns over time and assess predictors of dual method use 12 months after initiating hormonal contraceptives.
Methods
We conducted a prospective cohort study among women aged 15–24 years initiating oral contraceptive pills, patch, ring, or depot medroxyprogesterone and attending public family planning clinics. Participants completed questionnaires at baseline and 3, 6, and 12 months after enrollment. We used multivariable logistic regression to assess baseline factors associated with dual method use at 12 months among 1,194 women who were sexually active in the past 30 days.
Results
At baseline, 36% were condom users, and only 5% were dual method users. After initiation of a hormonal method, condom use decreased to 27% and remained relatively unchanged thereafter. Dual method use increased to a peak of 20% at 3 months but decreased over time. Women who were condom users at baseline had nearly twice the odds of being a dual method user at 12 months compared with nonusers (adjusted odds ratio [AOR] = 2.01, 95% CI: 1.28–3.14). Women who believed their main partner thought condoms were “very important,” regardless of perceived sexually transmitted infection risk or participant’s own views of condoms, had higher odds of dual method use (AOR = 2.89, 95% CI: 1.47–5.71).
Conclusions
These results highlight a potential missed opportunity for family planning providers. Providers focus on helping women initiate hormonal methods, however, they may improve outcomes by giving greater attention to method continuation and contingency planning in the event of method discontinuation and to the role of the partner in family planning.
Keywords: Dual method, Contraception, Adolescent, Young adult, Condoms, Sexually transmitted diseases, Depot medroxyprogesterone acetate, Oral contraceptives, Contraceptive patch, Vaginal ring
Between 1996 and 2006, pregnancy rates among teenaged women (aged 15–19 years) in the United States decreased by nearly 33%, yet as of 2006 (the most recent year for which data are available) an estimated 82% of these were unintended [1–3]. Sexually experienced teens and young adults have unintended pregnancy rates more than twice the national figure (69 per 1,000) for sexually active women of childbearing age, with the highest rates (162 per 1,000) among 18–19 year olds [4]. In addition to disproportionately high rates of unintended pregnancy, women aged 15–24 years also experience high rates of sexually transmitted infections (STIs). Although comprising only 25% of the sexually active population, teens and young adults are responsible for more than half of gonorrhea infections and nearly 75% of chlamydia infections [5]. Unintended pregnancy and STIs remain high, despite widespread use of contraceptives. Between 2006 and 2010, more than 86% of never-married female teens and 93% of never-married male teens had used a contraceptive method at last sex. Of this, condom use accounted for 75% and 52% by men and women, respectively [1].
Dual method use, defined as the use of a contraceptive method plus condoms, has been promoted as an effective way to mitigate the burden of both unintended pregnancy and STIs in teens and young adults. Although the prevalence of dual method use among teens has been found to be as high as 20%, when young adults are included, dual method use is as low as 8.3% [1,6]. Our understanding of factors associated with increased dual method use is very limited. Much of the prior research on dual method use has been cross-sectional, which is inadequate to assess the temporal relationship between factors that might contribute to dual method use [7–10]. In addition, few studies have been designed to analyze continued condom use at the time that women initiate hormonal contraception. Finally, many prior studies have been hampered by methodological flaws, including small sample sizes [7,9–12], differing lengths of follow-up for women using different methods [12], inconsistent definitions of dual method use including ineffective methods such as abstinence or withdrawal [7], and inconsistent definitions of discontinuation (discontinuation of condoms or the hormonal method), limiting the inferences to be drawn and generalizability of this prior research [13].
We examined condom use patterns over time in a large cohort of high-risk young women initiating hormonal contraception, including relatively newer contraceptive methods not previously studied: the transdermal patch and the vaginal ring. Additionally, we sought to identify predictors of dual method use over a 1-year period to inform strategies for increasing dual method use.
Materials and Methods
Subjects
Data for this study were collected as part of a larger study on factors associated with method discontinuation and pregnancy among adolescents and young women initiating hormonal contraception; detailed description of the study methods are described elsewhere [14]. In the original cohort, women initiating hormonal contraceptives, either the pill, patch, ring, or depot medroxyprogesterone, were recruited from four Planned Parenthood clinics in Northern California (Vallejo, Richmond, East Oakland, and Hayward) between September 2005 and July 2008. The study was designed specifically to examine newer short acting hormonal method use and therefore women using other effective methods including long acting reversible contraceptive (LARC) methods at baseline were not enrolled. Women, however, could switch to any method including LARCs over the 1-year follow-up period, although few did this. Women who presented for reproductive health care were screened consecutively. Eligibility criteria included being between 15 and 24 years old, not married, able to read English or Spanish, not pregnant (self-report) or desiring pregnancy within the next year, and able to provide written informed consent and comply with study procedures. Women could not have previously used the method they were initiating at the visit. Research staff collected data from enrolled participants via self-administered electronic questionnaires at baseline and 3, 6, and 12 months. All participants provided written informed consent. Given that minors can consent to contraceptive services in California without parental consent and that attempting to obtain parental consent could have compromised the adolescents’ guarantee of confidential services, parental consent was not required. The study was approved by the Committee on Human Research at the University of California, San Francisco.
Measures
The primary outcome measure was dual method use at 1 year. Dual method use was defined as condom use plus an effective contraceptive method. Effective contraceptive methods included the pill, patch, ring, implant, or IUD. Effective contraceptive method use was determined from questions about method used at last sex and continued use of the hormonal method initiated at baseline. Women were considered condom users if the percent of time they reported using a condom divided by the number of times they reported having sex in the past 30 days was equal to or greater than 80%. We based our definition of a condom user on evidence from a recent cohort study that demonstrated that using a proportion of protected acts (number of times a condom was used divided by the number of vaginal sex acts during a typical month in the past 3 months) was more predictive of pregnancy incidence than other measures (since last visit, at last sex, or frequency measure), although no one method was most predictive of STI/HIV incidence [15].
Independent variables considered for the analysis included those found to be associated with dual method use in previous studies as well as variables informed by the Health Belief Model, which states that individuals weigh the costs and benefits of a health-related behavior before attempting behavior change, and the Theory of Planned Behavior, which takes into account subjective norms around the behavior based on attitudes of individuals close to the person [16,17]. We grouped variables into the following categories: sociodemographic characteristics, reproductive history, and attitudes toward condom use.
Sociodemographic characteristics collected at baseline included age, neighborhood income, race and ethnicity, education, and employment status. Sexual and reproductive history measures included prior pregnancies and STIs, partner concurrency (having sex with a man other than main partner), and length of time they had sex with their main partner (0–3 months, 4–6 months, 7–12 months, >12 months, and no sex yet). Perceived STI risk in the next 3 months was measured on a Likert scale (not at all likely, a little likely, somewhat likely, very likely, don’t know). Participant’s beliefs toward condom use were derived from responses to a series of questions with answers on a Likert scale. The items were “Condoms should always be used, even if the girl uses birth control like the pill, patch, ring, or the shot” and “A girl does not need to use condoms if she gets checked at the clinic often” (responses for both questions included: strongly agree, agree, neither, disagree, and strongly disagree). Assessment of the attitudes of the woman and her partner toward condoms was obtained from the following questions: “How important do you think it is for your main partner to use condoms when he has sex with you? FOR HIM is it…” and “How important is it for YOU to use condoms when you have sex with your main partner?” (responses included: not at all important, somewhat important, very important, and don’t know). For women who reported condom use at last sex, reason for condom use was also asked (responses included: STI prevention, pregnancy prevention, both, or don’t know).
Data analysis
Analysis was limited to the subset of women from the original study cohort who reported having sex in the past 30 days at baseline. Women were divided into those who were condom users at baseline and those that were not. Comparisons between condom users and non-condom users at baseline were made using chi-square analyses. Bivariate analyses (chi-square) were conducted using sociodemographic, reproductive history, and attitude variables at baseline to model dual method use at 12 months. Multivariable logistic regression was used to examine factors associated with dual method use at 12 months. Variables chosen for the multivariable model were based on results from bivariate analyses (p < .05), potential confounders, prior research, and Health Belief Model/Theory of Planned Behavior. Attrition analyses were conducted comparing baseline characteristics including sociodemographics and reproductive history between those lost to follow-up and those who remained in the study. Two separate sensitivity analyses were done for the multivariable model, the first assuming those lost to follow-up were dual method users and the second assuming they were not. Statistical significance level was set to p < .05. All analyses were conducted using STATA 11 (Stata Corporation, College Station, TX).
Results
Of the 1,387 women enrolled at baseline in the cohort, we excluded 193 subjects for the following reasons: 134 women had not had sex in the past 30 days and 59 women were missing data on predictor variables. This resulted in 1,194 women who were eligible for analysis. The cohort was racially/ethnically diverse, with 61% describing themselves as either Latina or African-American. Nearly two thirds of women were ages 15 to 19 and more than half lived in a low-income neighborhood. At baseline, 36% of women were condom users and 5% were dual method users. Condom users at baseline were more likely to have been in a monogamous relationship of shorter duration and have a main partner with positive views of condoms, with a lower likelihood of a prior pregnancy than those who did not use condoms at baseline as seen in Table 1.
Table 1.
Characteristics of participants by condom use status at baseline
| Characteristic | Total
|
Condom user
|
Non-condom user
|
|||
|---|---|---|---|---|---|---|
| N
|
% | N
|
%
|
N
|
%
|
|
| 1,194 | 432 | 36.2 | 762 | 63.8 | ||
| Sociodemographics | ||||||
| Age (years)** | ||||||
| 15–17 | 413 | 34.6 | 170 | 39.4 | 243 | 31.9 |
| 18–19 | 391 | 32.8 | 146 | 33.8 | 245 | 32.2 |
| 20–24 | 390 | 32.7 | 116 | 26.9 | 274 | 36.0 |
| Race/ethnicity (n = 1,194) | ||||||
| White | 133 | 11.1 | 59 | 13.7 | 74 | 9.7 |
| Latina | 320 | 26.8 | 105 | 24.3 | 215 | 28.2 |
| African American/black | 407 | 34.1 | 150 | 34.7 | 257 | 33.7 |
| Asian/Pacific Islander | 141 | 11.8 | 43 | 10.0 | 98 | 12.9 |
| Multiracial/other | 193 | 16.2 | 75 | 17.4 | 118 | 15.5 |
| School and employment status (n = 1,194) | ||||||
| In school or employed (full or part time) | 996 | 83.4 | 371 | 85.9 | 625 | 82.0 |
| Not working or in school | 198 | 16.6 | 61 | 14.1 | 137 | 18.0 |
| Clinic site (n = 1,194) | ||||||
| Oakland | 361 | 30.2 | 125 | 28.9 | 236 | 31.0 |
| Hayward | 312 | 26.1 | 120 | 27.8 | 192 | 25.2 |
| Vallejo | 139 | 11.6 | 49 | 11.3 | 90 | 11.8 |
| Richmond | 382 | 32 | 138 | 31.9 | 244 | 32.0 |
| Low income neighborhood (n = 1,171)a | 655 | 55.9 | 244 | 58.1 | 411 | 54.7 |
| Reproductive history | ||||||
| Method used at last sex (n = 1,190)*** | ||||||
| Pill | 82 | 6.9 | 30 | 7.0 | 52 | 6.9 |
| Patch | 56 | 4.7 | 15 | 3.5 | 41 | 5.4 |
| Ring | 12 | 1.0 | 1 | .2 | 11 | 1.4 |
| DMPA | 29 | 2.4 | 10 | 2.3 | 19 | 2.5 |
| Other effective methodb | 1 | .8 | 0 | 0 | 1 | .1 |
| None/withdrawal | 993 | 83.4 | 366 | 84.9 | 627 | 82.6 |
| Dual method users | 56 | 4.7 | 56 | 13 | 0 | 0 |
| Baseline method initiated (n = 1,194)* | ||||||
| Pill | 366 | 30.7 | 158 | 36.6 | 208 | 27.3 |
| Patch | 339 | 28.4 | 112 | 25.9 | 227 | 29.8 |
| Ring | 232 | 19.4 | 74 | 17.1 | 158 | 20.7 |
| DMPA | 257 | 21.5 | 88 | 20.4 | 169 | 22.2 |
| Prior pregnancy (n = 1,194)*** | 586 | 49.1 | 165 | 38.2 | 421 | 55.2 |
| Prior STI (n = 1,169) | 255 | 21.8 | 83 | 19.7 | 172 | 23.0 |
| Perceived STI risk in next 3 months with main partner (n = 1,194) | ||||||
| Not at all/a little likely/somewhat | 875 | 73.3 | 314 | 72.7 | 561 | 73.6 |
| Very likely | 319 | 26.7 | 118 | 27.3 | 201 | 26.4 |
| Partner concurrency (sex with man other than main partner) (n = 1,194)* | 170 | 14.2 | 47 | 10.9 | 123 | 16.1 |
| Time had sex with main partner (months) (n = 1,194)*** | ||||||
| 0–6 | 518 | 43.4 | 228 | 52.8 | 290 | 38.1 |
| 7–12 | 140 | 11.7 | 41 | 9.5 | 99 | 13.0 |
| >12 | 352 | 29.5 | 97 | 22.5 | 255 | 33.5 |
| No sex yet | 184 | 15.4 | 66 | 15.3 | 118 | 15.5 |
| Attitudes toward condom use | ||||||
| Reason for condom use at last sex (n = 459)c,** | ||||||
| Pregnancy prevention | 188 | 41 | 133 | 37.7 | 55 | 51.9 |
| STI/AIDS prevention | 12 | 2.6 | 8 | 2.3 | 4 | 3.8 |
| Both | 255 | 55.6 | 211 | 59.8 | 44 | 41.5 |
| Other | 4 | .9 | 1 | .3 | 3 | 2.8 |
| Main partner views of condoms (n = 1,008)d,*** | ||||||
| Very important | 307 | 30.5 | 204 | 56.0 | 103 | 16.0 |
| Somewhat important | 327 | 32.4 | 115 | 31.6 | 212 | 32.9 |
| Not at all important | 321 | 31.8 | 43 | 11.8 | 278 | 43.2 |
| Don’t know | 53 | 5.3 | 2 | .5 | 51 | 7.9 |
| Believes should always use condoms, even if on birth control (n = 1,187)*** | ||||||
| Strongly agree | 419 | 35.3 | 185 | 43.1 | 234 | 30.9 |
| Agree | 417 | 35.1 | 132 | 30.8 | 285 | 37.6 |
| Neither | 212 | 17.9 | 70 | 16.3 | 142 | 18.7 |
| Disagree | 119 | 10 | 33 | 7.7 | 86 | 11.3 |
| Strongly disagree | 20 | 1.7 | 9 | 2.1 | 11 | 1.5 |
DMPA = depot medroxyprogesterone; STI = sexually transmitted infection.
p < .05,
p < .01,
p < .001.
Defined as living in a zip code where the proportion of families living below the federal poverty level is greater than the national average.
Includes one woman who reported using a once-monthly injectable contraceptive.
Asked of those who used a condom at last sex.
Asked only of those with a main partner.
Contraceptive and condom use over time was dynamic with women experiencing dramatic changes in both as represented in Figure 1. After initiation of hormonal methods at baseline, overall condom use (condoms only or with a contraceptive method) dropped from 36% to 27% by 3 months. During the same period, dual method use increased from 5% to a peak of 20%. Over the 12 months, as women discontinued hormonal methods, there was a substantial decrease in dual method use, an increase in condom only use, and little change in overall condom use. Among condom users at baseline who discontinued condom use after initiating an effective method and were no longer using that method at 1 year, 46% switched back to condoms.
Figure 1.
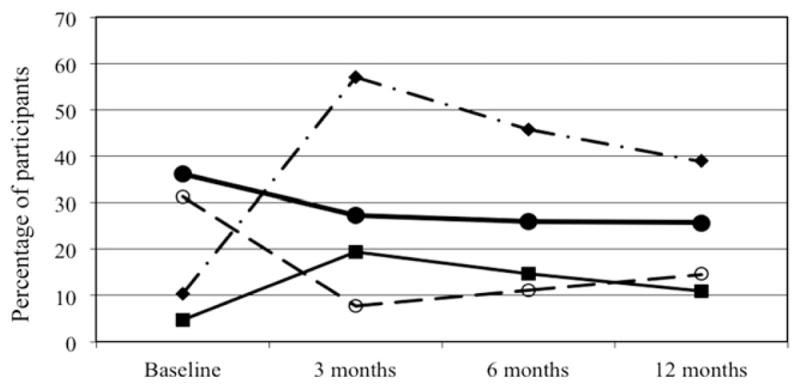
Condom use over time with the initiation of hormonal methods.
 Hormonal methods only.a
Hormonal methods only.a
 Overall condom use.b
Overall condom use.b
 Dual method use.
Dual method use.
 Condom only. aAlso includes small percentage of women (1.8%) using other effective methods (intrauterine devices, implants). bIncludes condom only and dual method use.
Condom only. aAlso includes small percentage of women (1.8%) using other effective methods (intrauterine devices, implants). bIncludes condom only and dual method use.
In the bivariate analysis of factors associated with dual method use at 12 months, being a consistent condom user at baseline was associated with an odds ratio (OR) of 2.4 (95% CI: 1.6–3.6). Type of hormonal method chosen at baseline was not significantly associated with dual method use nor was a prior pregnancy or history of an STI. Women who said their partner thought condoms were “very important” or did not know how their partners felt about condom use were more likely to be dual method users than women who said their partner thought condoms were “not at all important” (OR 3.5, 95% CI: 1.9–6.3 and 2.5, 95% CI: 1.3–4.8, respectively). In the multivariable model (adjusted for age, race/ethnicity, clinic site), both baseline condom use and main partner’s views of condoms remained significant. Those who thought it was “very likely” that they would get an STI in the next 3 months were significantly less likely to be dual method users at 1 year (OR .5, 95% CI: .3–.99), as seen in Table 2.
Table 2.
Predictors of dual method use at 12 months
| Variable | Unadjusted OR (95% CI)a N = 1,018 |
Adjusted OR (95% CI)b N = 1,012 |
|---|---|---|
| Baseline condom use | ||
| <80% of time | 1 (reference) | 1 (reference) |
| ≥80% of time | 2.40 (1.62–3.58)*** | 2.01 (1.28–3.14)** |
| Prior sexually transmitted infectionc | 1.35 (.93–1.96) | 1.55 (.94–2.55) |
| Prior pregnancy | 1.11 (.75–1.65) | 1.18 (.73–1.88) |
| Perceived STI risk in next 3 months | ||
| Not at all/a little/somewhat likely | 1 (reference) | 1 (reference) |
| Very likely | .89 (.56–1.42) | .54 (.30–.99)* |
| Partner concurrency (other than main) | .77 (.42–1.41) | .73 (.38–1.40) |
| Main partner views of condoms | ||
| Not at all important | 1 (reference) | 1 (reference) |
| Somewhat important | 1.65 (.86–3.20) | 1.55 (.78–3.10) |
| Very important | 3.45 (1.88–6.34)*** | 2.89 (1.47–5.71)** |
| Don’t know | 2.45 (1.25–4.81)* | 2.99 (1.35–6.64)** |
| Believes should always use condoms, even if on birth controld | ||
| Strongly disagree | 1 (reference) | 1 (reference) |
| Disagree | .29 (0.05–1.72) | .48 (.07–3.13) |
| Neither | .91 (019–4.27) | 1.54 (.30–7.78) |
| Agree | .93 (.20–4.24) | 1.41 (.29–6.89) |
| Strongly agree | .97 (.21–4.41) | 1.07 (.22–5.15) |
p < .05,
p < .01,
p < .001.
n = 1,018 as 176 women were missing data for dual method use at 12 months.
Adjusted for age, race/ethnicity, and clinic site.
Individuals who were missing on STI history were categorized as missing as to include in multivariable analysis.
n = 1,012 because of missing data.
To determine whether those lost to follow-up may have affected our results, we conducted sensitivity analyses that demonstrated that predictors of dual method use did not differ significantly when those lost to follow-up were assumed not to be dual method users. When those lost to follow-up were considered dual users however, only condom use at baseline remained a significant predictor of dual method use (data not shown).
Discussion
This study highlights the dynamic nature of the tradeoff between hormonal methods and condom use in women initiating hormonal contraception as well as the influence of the male partner on dual method use longitudinally. A tradeoff is a phenomenon whereby women initially use condoms, begin a hormonal contraceptive, and subsequently discontinue condom use. This was observed in the current study when, as women initiated a range of effective hormonal contraceptives, dual method use increased; however, overall condom use suffered as a result. This finding is consistent with the tradeoff between condom use and hormonal methods demonstrated in a prior study [18]. The longitudinal nature of this study allowed us to follow condom use over time as women initiated and later discontinued hormonal contraception. By 12 months, the modest gains in dual method use were diminished. What is important about this study is that we were able to demonstrate that not only did women trade off condoms for hormonal methods, but as they discontinued the hormonal methods, more than half (54%) failed to resume condom use, resulting in an ultimate tradeoff of condoms for no method. This outcome is far from ideal. Given the realities of the tradeoff between condoms and hormonal contraception, the use of condoms, not only for STI protection but also as a backup method when hormonal contraception is discontinued, should be underscored. Additionally, with the understanding that many women discontinue these hormonal methods over time, promotion of long-acting reversible contraception, including copper and progestin-releasing IUDs and implants, is essential.
Overall condom use decreased by nearly one third from baseline to 12 months, and although hormonal method discontinuation was significant, there was a net gain in effective hormonal contraceptive use. It should be noted that even on the most fertile day, the risk of a woman becoming pregnant is less than half her risk of acquiring gonorrhea from an infected partner [19]. At the same time, the risk of an STI only exists when a partner is infected, whereas the risk of pregnancy (although varying in likelihood throughout a woman’s cycle) is present with virtually all partners. Therefore, one might argue that it is possible for a subset of women, those in committed monogamous relationships for instance, the tradeoff may be justified. Unfortunately, we know from multiple studies that adolescents and young adults often underestimate their risk of STIs [20,21]. Of note, having a high perceived risk of an STI in the next 3 months was independently associated with reduced odds of being a dual method user. Although it is counterintuitive, we speculate that other factors influence contraceptive behaviors. In particular, gender-based power may explain why even though women know they are at high risk, they have less agency in their relationships to negotiate condom use and therefore have lower odds of dual method use [22].
Because of small sample size and the observational design of the study, we were unable to compare STI acquisition rates among those that made the tradeoff compared with those that did not. Although a recent analysis of a randomized intervention to increase dual method use also failed to find a significant difference in biologic outcomes (STI and unintended pregnancy incidence), the study found that those with the highest level of adherence had the lowest incidence of STIs and unintended pregnancy [23]. Further studies are needed to assess STI acquisition in the setting of initiation of hormonal methods.
Our results also highlight the strong influence that a woman’s main partner has on her decision to be a dual method user, irrespective of her own views about dual method use. This again may be related to the concept of relationship power imbalance and its impact on a woman’s ability to negotiate condom use. Many of the associations observed in prior studies (age, African-American race, type of hormonal method initiated, partner concurrency, prior pregnancy, and STIs) were not observed in our bivariate models. Partner’s attitude toward condom use, in addition to condom use at baseline, were the only other significant predictors after controlling for numerous other factors. This is consistent with findings from previous research and highlights the importance of recognizing the role of the partner in contraceptive choice [9,12,24]. Providers should inquire about partner attitudes about condom use and work with women to develop techniques to address this component of the decision around dual method use. Interestingly, women who reported they didn’t know their partner’s attitudes about condoms were also more likely to report dual method use, suggesting that as long as partners do not actively voice opposition to condoms, women are more likely to use them along with another method. The need for the involvement of the partner in family planning was emphasized in a recent study of adult women attending public family planning clinics, which found that nearly two thirds of respondents were interested in some form of partner involvement in their reproductive health planning [25]. It is clear from our findings that the role of the partner is significant and that women do not make contraceptive decisions in isolation. Providing couples-centered counseling may represent a way to improve contraceptive, and more specifically, dual method use.
Our study has limitations that affect the interpretation of the data. Although our follow-up rate was high at 88%, there were some differences in women who were lost to follow-up. Women with follow-up data were more likely to be in school or working full time than those who were lost to follow-up, indicating that our final study population may have been lower risk. However, our sensitivity analysis demonstrated that even if none of those who were lost to follow-up were dual method users, our results would be the same. The data were obtained by self-report, which is susceptible to social desirability bias; however, the majority of the data was collected by computer, which has been shown to improve reliability for sensitive questions [26]. This study included a diverse group of women from urban and suburban public family planning clinics in Northern California; it may not be generalizable to other populations but this population represents an important demographic as they are at high risk for experiencing unintended pregnancy and STIs.
Despite these limitations, this study provides a dynamic view of condom use among women initiating hormonal methods and identifies key factors that could be addressed during family planning visits to improve dual method use among women.
These results highlight a potential missed opportunity for family planning providers. With a focus on getting women to initiate hormonal methods for pregnancy prevention, it is unclear whether ample attention is given to method continuation and contingency planning in the event of method discontinuation. Increasing dual method use is challenging as both hormonal contraceptive use and condom use are complex behaviors with multiple mediating factors that many women may have difficulty negotiating; that being said, it is crucial that providers stress the importance of dual method use.
IMPLICATIONS AND CONTRIBUTION.
In our efforts to increase the use of hormonal contraceptives, condom use suffers and contraceptive continuation is not optimal. This study highlights the large need for effective interventions to improve long-term condom and contraceptive use among adolescent and young adult women and their partners.
Acknowledgments
T.R.R. currently receives grant support from Teva Pharmaceutical Industries for research work on Plan B and Plan B OneStep emergency contraception. This study was supported by the National Institute of Child Health and Human Development grants R01 HD045480 and K24 HD057086-02. Additionally, this project was supported by NIH/NCRR/OD UCSF-CTSI grant number TL1 RR024129. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Results do not necessarily represent the views of Planned Parenthood Federation of America, Inc. Findings from this study were reported in poster format at the American College of Obstetricians and Gynecologists Annual Clinical Meeting in Washington, D.C., and the National Predoctoral Clinical Research Training Program Meeting in St. Louis, MO in 2011. The authors thank Cynthia Harper and Jody Steinauer for their advice on the analysis and reviewing early drafts of this article.
References
- 1.Martinez GM, Copen CE, Abma JC. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing. 2006–2010 National Survey of Family. Growth Vital Health Stat. 2011;23:1–44. [PubMed] [Google Scholar]
- 2.The DCR report: Section A - Unplanned pregnancy in the United States among all women. [Accessed April 16, 2011];The National Campaign to Prevent Teen and Unplanned Pregnancy. Available at: www.thenationalcampaign.org/resources/dcr/NATC_DCRreport.pdf.
- 3.Finer LB, Zolna MR. Unintended pregnancy in the United States: Incidence and disparities, 2006. New York: Guttmacher Institute; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finer LB. Unintended pregnancy among U.S. adolescents: Accounting for sexual activity. J Adolesc Health. 2010;47:312–4. doi: 10.1016/j.jadohealth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2009. Atlanta: CDC; 2010. [Google Scholar]
- 6.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat. 2010;23:1–44. [PubMed] [Google Scholar]
- 7.Crosby RA, DiClemente RJ, Wingood GM, et al. Correlates of using dual methods for sexually transmitted diseases and pregnancy prevention among high-risk African-American female teens. J Adolesc Health. 2001;28:410–4. doi: 10.1016/s1054-139x(00)00210-x. [DOI] [PubMed] [Google Scholar]
- 8.Pazol K, Kramer MR, Hogue CJ. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep. 2010;125:208–17. doi: 10.1177/003335491012500209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riehman KS, Sly DF, Soler H, et al. Dual-method use among an ethnically diverse group of women at risk of HIV infection. Fam Plann Perspect. 1998;30:212–7. [PubMed] [Google Scholar]
- 10.Roye CF. Condom use by Hispanic and African-American adolescent girls who use hormonal contraception. J Adolesc Health. 1998;23:205–11. doi: 10.1016/s1054-139x(97)00264-4. [DOI] [PubMed] [Google Scholar]
- 11.Darney PD, Callegari LS, Swift A, et al. Condom practices of urban teens using Norplant contraceptive implants, oral contraceptives, and condoms for contraception. Am J Obstet Gynecol. 1999;180:929–37. doi: 10.1016/s0002-9378(99)70664-2. [DOI] [PubMed] [Google Scholar]
- 12.Sangi-Haghpeykar H, Posner SF, Poindexter AN., III Consistency of condom use among low-income hormonal contraceptive users. Perspect Sex Reprod Health. 2005;37:184–91. doi: 10.1363/psrh.37.184.05. [DOI] [PubMed] [Google Scholar]
- 13.Cushman LF, Romero D, Kalmuss D, et al. Condom use among women choosing long-term hormonal contraception. Fam Plann Perspect. 1998;30:240–3. [PubMed] [Google Scholar]
- 14.Raine TR, Foster-Rosales A, Upadhyay UD, et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117:363–71. doi: 10.1097/AOG.0b013e31820563d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minnis AM, van der Straten A, Gerdts C, Padian NS. A comparison of four condom-use measures in predicting pregnancy, cervical STI and HIV incidence among Zimbabwean women. Sex Transm Infect. 2010;86:231–5. doi: 10.1136/sti.2009.036731. [DOI] [PubMed] [Google Scholar]
- 16.Lopez LM, Tolley EE, Grimes DA, Chen-Mok M. Theory-based interventions for contraception. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD007249.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Rimer BK, Glanz K. Theory at a Glance: A guide for Health Promotion Practice. Washington, DC: National Institutes of Health, National Cancer Institute; 2005. [Google Scholar]
- 18.Ott MA, Adler NE, Millstein SG, et al. The trade-off between hormonal contraceptives and condoms among adolescents. Perspect Sex Reprod Health. 2002;34:6–14. [PubMed] [Google Scholar]
- 19.Cates W, Jr, Steiner MJ. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach? Sex Transm Dis. 2002;29:168–74. doi: 10.1097/00007435-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Ford CA, Jaccard J, Millstein SG, et al. Perceived risk of chlamydial and gonococcal infection among sexually experienced young adults in the United States. Perspect Sex Reprod Health. 2004;36:258–64. doi: 10.1363/psrh.36.258.04. [DOI] [PubMed] [Google Scholar]
- 21.Ethier KA, Kershaw T, Niccolai L, et al. Adolescent women underestimate their susceptibility to sexually transmitted infections. Sex Transm Infect. 2003;79:408–11. doi: 10.1136/sti.79.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tschann JM, Adler NE, Millstein SG, et al. Relative power between sexual partners and condom use among adolescents. J Adolesc Health. 2002;31:17–25. doi: 10.1016/s1054-139x(01)00418-9. [DOI] [PubMed] [Google Scholar]
- 23.Peipert JF, Zhao Q, Meints L, et al. Adherence to dual method contraceptive use. Contraception. 2011;84:252–8. doi: 10.1016/j.contraception.2011.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harvey SM, Henderson JT, Branch MR. Protecting against both pregnancy and disease: predictors of dual method use among a sample of women. Women Health. 2004;39:25–43. doi: 10.1300/J013v39n01_02. [DOI] [PubMed] [Google Scholar]
- 25.Zolna MR, Lindberg LD, Frost JJ. Couple-focused services in publicly funded family planning clinics: Identifying the need, 2009. New York: Guttmacher Institute; 2011. [Google Scholar]
- 26.Langhaug LF, Cheung YB, Pascoe SJ, et al. How you ask really matters: randomized comparison of four sexual behaviour questionnaire delivery modes in Zimbabwean youth. Sex Transm Infect. 2011;87:165–73. doi: 10.1136/sti.2009.037374. [DOI] [PubMed] [Google Scholar]


