Abstract
OBJECTIVE
Requiring a pelvic examination before prescribing oral contraception poses an unnecessary barrier to contraceptive access. Medical guidelines have outlined the safety of oral contraception provision without a pelvic examination, yet little is known about the practices of clinicians providing reproductive health care. Our purpose was to investigate clinicians′ requirements for pelvic examination and what may account for practice differences.
METHODS
We administered a mailed survey to a national probability sample of obstetrician–gynecologists (ob-gyns), family medicine physicians, and advanced practice nurses specializing in obstetrics and gynecology and women′s health or family medicine in 2008–2009 (N = 1,196), with a response rate of 65.3%
RESULTS
Nearly one third of ob-gyns and family medicine physicians reported always requiring a pelvic examination when prescribing oral contraception (ob-gyns 29%; family medicine 33%). A higher proportion of advanced practice nurses in primary care (45%) and a markedly lower percentage of advanced practice nurses in reproductive health (17%) reported always requiring the examination. In adjusted analyses, older clinicians were more likely to require the pelvic examination (odds ratio [OR] 1.03, P<.01) and clinicians serving a higher proportion of Medicaid patients more likely (OR 1.62, P<.05). Providers in private practice were more than twice as likely as those working in family-planning or community clinics to require pelvic examinations (OR 2.30, P<.01).
CONCLUSION
One third of clinicians we surveyed require pelvic examinations before provision of oral contraceptives, despite guidelines indicating they are unnecessary and research suggesting they can pose a barrier to contraceptive access.
Hormonal oral contraception can safely be prescribed without a pelvic examination, according to the World Health Organization1 and the American College of Obstetricians and Gynecologists (the College).1,2 Weight, blood pressure, and health history are required before prescription of hormonal contraception, whereas screening for sexually transmitted infections (STIs) and cancer are not needed to evaluate patients for initiation of oral contraceptive use for pregnancy prevention.3 In the United States, oral contraception is the most common reversible contraceptive method, used by more than one quarter of women using contraception (28.0%),4 and the requirement for a pelvic examination poses a barrier to access for some women.5,6 Negative perceptions of the examination such as fear, embarrassment, and pain, and health care avoidance owing to concerns about the pelvic examination have been documented.5,7
Specialists in obstetrics and gynecology provide more reproductive health care to women than any other physician type, but family medicine physicians and other general practitioners also provide such care.8–10 Women also make reproductive health care visits to advanced practice nurses, including certified nurse midwives.11 Variation in practice settings, clinical training, billing mechanisms, and patient populations could contribute to differences in pelvic examination practices related to oral contraception provision. The current study investigates clinicians’ requirements for pelvic examination and what may account for practice differences.
MATERIALS AND METHODS
We surveyed a national probability sample of physicians in obstetrics and gynecology and family medicine and advance practice nurses. These clinicians provide the majority of primary reproductive health care to women.9 The sampling frame was limited to nurses and physicians working in the United States. Physicians were identified using the American Medical Association’s Physician Masterfile, a comprehensive database of nearly 1 million physicians and residents that includes members and nonmembers of the American Medical Association. The database is updated weekly. Stratified probability samples of 600 eligible physicians (ie, not retired, not in residency, spend majority of time in direct patient care) specializing in family medicine and 600 physicians specializing in obstetrics and gynecology or gynecology alone were drawn. Nurses were identified using a national database of nurse practitioners and advanced practice nurses (Verispan), which contains more than 143,000 advanced practice nurses and is updated monthly. Stratified samples of 600 advanced practice nurses specializing in obstetrics and gynecology, family planning, or women’s health and 600 advanced practice nurses specializing in family medicine were drawn to allow comparisons within and across these clinician subgroups. In total, 1,200 physicians and 1,200 advanced practice nurses were selected with replacement using a random number generator to select participants from each clinician-type strata. Duplicate names in the sample (n=29) were excluded from the mailing.
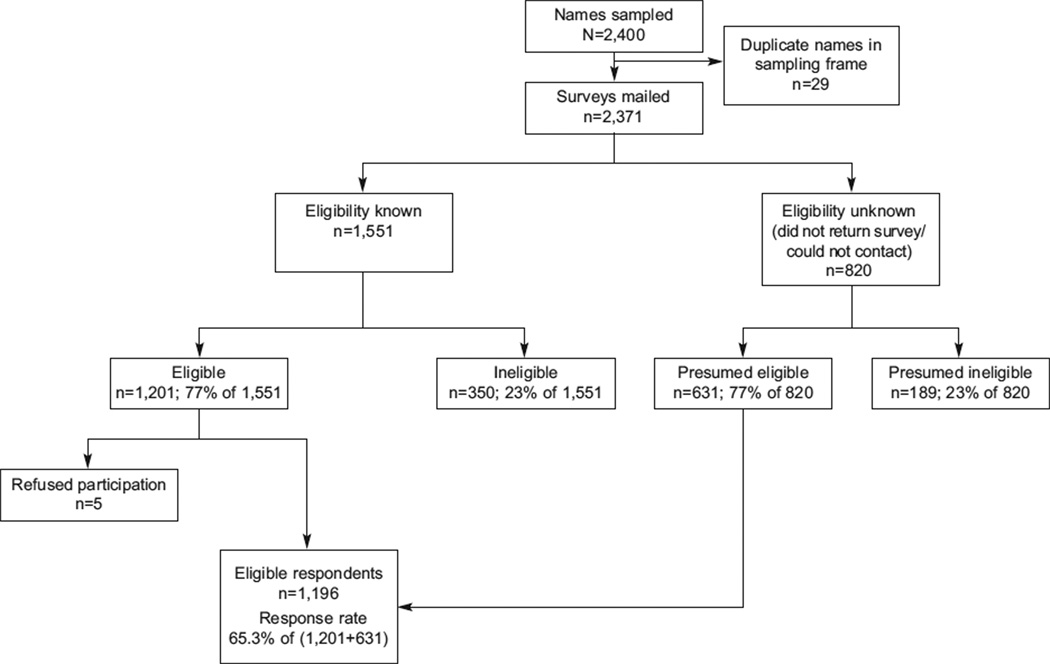
Clinicians were first sent a letter introducing the study, followed by a survey and cover letter, postagepaid return envelope, and $20 in cash mailed by U.S. Priority Mail. A reminder postcard was mailed 1 week later, and a second copy of the survey and postagepaid return envelope was sent by first class mail 3 weeks later if the original survey had not yet been returned. If mail was returned as undeliverable, research staff used online state nursing and medical boards, directories, and search engines to locate current information. After the final mailing, recruitment efforts were made by phone. Data were collected from September 2008 through February 2009. Of the 2,371 clinicians surveyed, 350 were ineligible: 123 nonrespondents were identified as ineligible in the process of telephone follow-up, and 227 respondents were not eligible based on screening questions in the survey (ie, do not provide direct patient care or do not see family-planning or STI patients). The response rate was calculated by subtracting ineligible clinicians and adjusting for an estimated proportion of eligible participants among unknown respondents (Fig. 1). There were 1,196 eligible respondents. The analytic sample for the study (N= 1,196) excludes 32 clinicians with missing data on the dependent variable. The study protocol was approved by the Committee on Human Research at the University of California, San Francisco.
Fig. 1.
Mailed and returned surveys. We assumed that the proportion of providers eligible was the same for providers of known and unknown eligibility and calculated the response rate accordingly. The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 6th ed. Deerfield (IL): The American Association for Public Opinion Research; 2009.
An original questionnaire with closed-ended questions was developed for the survey, informed by 31 qualitative interviews with providers conducted during an earlier phase of the study12,13 and using items validated in other studies.
The dependent variable was based on a single question asking clinicians, “Do you require a pelvic examination when prescribing oral contraceptives to your patients?” with the response options “never,” “sometimes,” “usually,” and “always.” A dichotomous variable was constructed to compare clinicians who always require the pelvic examination to those with other practices.
To define practice setting, clinicians were asked where they work the majority of the time. To assess the patient population served, clinicians were asked to indicate approximately how many of their patients are Medicaid recipients, uninsured, Hispanic or Latino, African American, and teenage females. The response categories were “none,” “some,” “half,”“most,” or “all,” and these were dichotomized to compare those with half or more to those with less than half of patients in the category. In addition, a variable describing patient populations as half or more minority (Hispanic or Latino, African American) was created by combining responses from the two individual items.
Population density was based on an item from the survey asking whether the location of the respondent’s clinical practice was a city, a suburban community or large town, a small town, or a rural area. The item was coded “urban,” “suburban,” or “rural,” where rural included those in a small town. Region was defined using standard U.S. census bureau classifications for states. Clinician characteristics measured included age, sex, race or ethnicity, and whether they had received training in family planning. Finally, we examined two patient scenarios that were presented to clinicians, a 16-year-old and a 24-year-old, to ascertain the clinical tests they would provide in office visits.
Stratification design were applied in all analyses to account for disproportionate sampling. The characteristics of the clinicians in our sample and their practice settings were described and differences tested with the design-based Pearson χ2 test for overall categorical differences and the adjusted Wald test for mean differences. A logistic regression model testing the independent effect of clinical specialty on the likelihood of requiring a pelvic examination, adjusted for clinician and practice setting characteristics then was computed. Finally, we evaluated how the clinical screening and prevention activities recommended by clinicians differed depending on their pelvic examination requirements. For the hypothetical patient cases, we examined how preventive screening practices related to cervical cancer and STI prevention co-vary with pelvic examination practices, using the design-based Pearson χ2 test. Stata 11.1 was used for all analyses.
RESULTS
The response rate was 65.3%; higher than response rates found in more recent national surveys of clinicians.14–17 Responders and nonresponders did not differ by region. However, younger clinicians, females, ob-gyns, and advanced practice nurses were more likely to respond to the survey than family medicine physicians.
Differences in the personal characteristics and practice settings of the different clinician types are described in Table 1. Fewer than half of ob-gyn and family medicine physicians were women, whereas nearly all advanced practice nurses were women. A greater proportion of physicians were nonwhite compared with advanced practice nurses. Few ob-gyns reported working in clinics (3.8%, 95% confidence interval [CI] 2.2–6.4)–instead, ob-gyns reported working in private practice settings (80.8%). In contrast, more than one third (36.1%, 95% CI 31.2–41.3) of advanced practice nurses in obstetrics and gynecology or women’s health reported working in community and family-planning clinics and less than half in private practices (42.3%, 95% CI 37.3–47.6). Reflecting these differences, the patient populations seen by the different types of clinicians varied. Overall, physicians were far less likely to see teenage, minority, uninsured, and Medicaid-insured patients compared with advanced practice nurses, with advanced practice nurses in obstetrics and gynecology or women’s health seeing the highest proportion of these patients.
Table 1.
Characteristics of Clinicians and Differences in Pelvic Examination Requirements by Clinician Type (N = 1,164)
| Variable | MD Ob-Gyn (n=345) |
MD Family Medicine (n=259) |
APN Ob-Gyn or Women’s Health (n=352) |
APN Family Medicine (n=208) |
|---|---|---|---|---|
| Always require pelvic examination for OC prescription | 29.0 (24.4–34.0) | 32.8 (27.4–38.8) | 16.5 (13.0–20.7) | 44.7 (38.1–51.6) |
| Clinician characteristics | ||||
| Mean age (y) | 49.3 (48.2–50.4) | 46.8 (45.7–48.0) | 50.7 (49.7–51.8) | 48.0 (46.7–49.4) |
| Mean age nonrespondents (y) | 53.3 ±11.1 | 49.7±10.0 | 53.0±12.5 | 50.8±10.2 |
| White (non-Hispanic) race or ethnicity | 71.9 (66.8–76.4) | 74.3 (68.6–79.3) | 87.7 (83.8–90.8) | 88.4 (83.3–92.1) |
| Female | 44.5 (39.5–49.9) | 40.9 (35.1–47.0) | 99.2 (97.4–99.7) | 94.2 (90.1–96.7) |
| Nonrespondents female (%) | 37.8 | 31.0 | 96.7 | 90.1 |
| Training in family planning | 89.8 (86.1–92.6) | 84.2 (79.2–88.1) | 97.2 (94.8–98.4) | 83.6 (77.9–88.0) |
| Practice characteristics | ||||
| Practice setting | ||||
| Private | 80.8 (76.2–84.6) | 77.9 (72.4–82.6) | 42.3 (37.3–47.6) | 57.1 (50.2–63.7) |
| Community or family-planning clinic | 3.8 (2.2–6.4) | 8.1 (5.4–12.2) | 36.1 (31.2–41.3) | 22.9 (17.7–29.2) |
| Hospital-based | 15.5 (12.0–19.7) | 14.0 (10.2–18.8) | 21.6 (17.6–26.2) | 20.0 (15.1–26.1) |
| Practice location | ||||
| Urban | 39.9 (34.9–45.2) | 32.1 (26.6–38.0) | 50.1 (44.9–55.4) | 41.6 (35.0–48.4) |
| Suburban | 44.6 (39.4–47.9) | 33.6 (28.1–39.6) | 29.1 (24.6–34.1) | 24.6 (19.2–31.0) |
| Rural | 15.5 (12.0–19.7) | 34.4 (28.8–40.4) | 20.8 (16.8–25.4) | 33.8 (27.7–40.6) |
| Patient population characteristics | ||||
| At least half of patients are female teenagers | 11.7 (8.7–15.5) | 9.3 (6.3–13.5) | 31.2 (26.6–36.3) | 19.0 (14.2–25.0) |
| At least half of patients are minority race or ethnicity | 28.5 (24.0–33.5) | 21.7 (17.1–27.2) | 42.9 (37.8–48.1) | 38.4 (31.9–45.2) |
| At least half of patients are uninsured | 4.1 (2.4–6.8) | 5.4 (3.2–9.0) | 27.3 (22.9–32.2) | 21.6 (16.4–27.8) |
| At least half of patients use Medicaid | 25.1 (20.8–29.9) | 13.2 (9.6–18.0) | 41.1 (36.0–46.4) | 36.9 (30.6–43.7) |
| At least half of patients at risk for STIs, HIV, or both | 59.7 (54.4–64.8) | 47.5 (41.5–53.6) | 83.0 (78.7–86.5) | 72.6 (66.1–78.2) |
APN, advance practice nurse; OC, oral contraception; STI, sexually transmitted infection; HIV, human immunodeficiency virus.
Data are % (95% confidence interval) or mean±standard deviation unless otherwise specified.
Differences were tested using the design-based Pearson χ2 test for categorical variables or the adjusted Wald test for mean differences.
All overall tests by clinician specialty are statistically significant (P<.001).
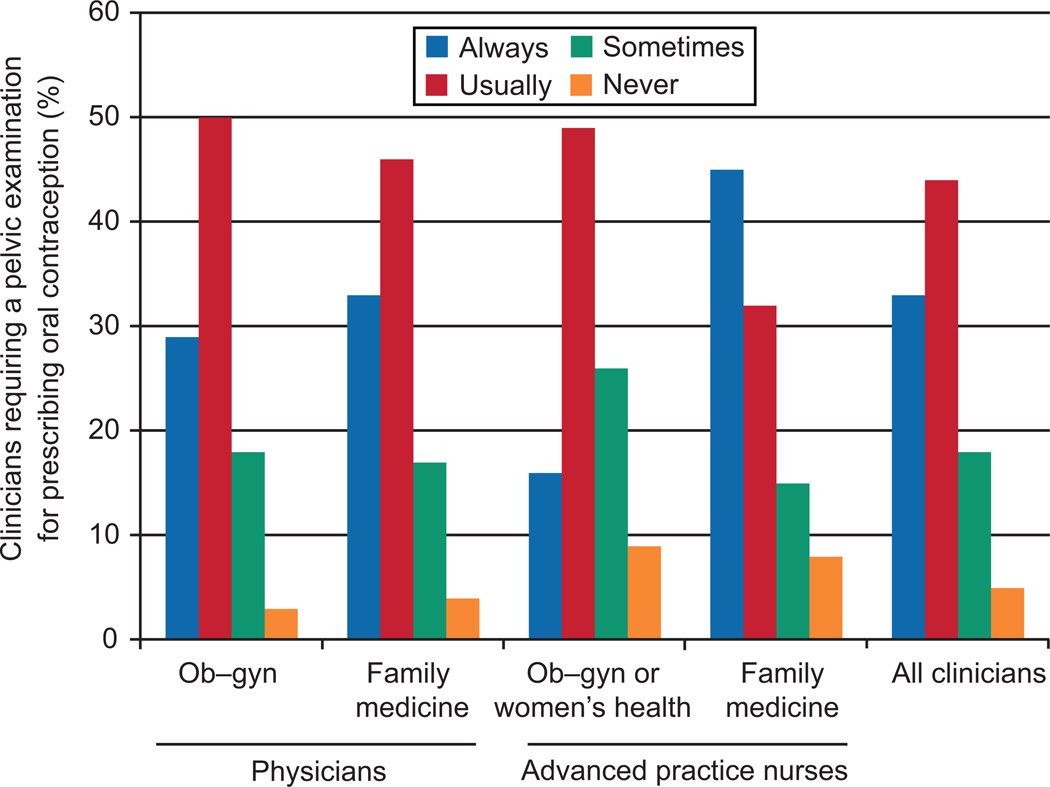
One third of all clinicians (33%, 95% CI 30.0–36.2) reported they always require a pelvic examination when prescribing oral contraception and nearly half usually require it (44%, 95% CI 40.8–47.3) (Fig. 2). There were differences by clinician type. Whereas a similar proportion of ob-gyn physicians (29.0%, 95% CI 24.4–34.0) and family medicine physicians (32.8%, 95% CI 27.4–38.8), reported that they always require a pelvic examination when prescribing oral contraception, advanced practice nurses specializing in reproductive health were least likely to require the examination (16.5%, 95% CI 13.0–20.7), and the highest proportion requiring the examination were advanced practice nurses in primary care (44.7%, 95% CI 38.1–51.5).
Fig. 2.
Requirement of a pelvic examination for oral contraception by clinician type (N = 1,164).
Results from multivariable logistic regression (Table 2) showed that advanced practice nurses specializing in obstetrics, gynecology, and women’s health were significantly less likely than ob-gyn physicians to require the pelvic examination (OR 0.59; 95% CI 0.39–0.90). Older clinicians were also more likely to require pelvic examinations (OR 1.03; 95% CI 1.01– 1.04). Clinical practice setting and patient population characteristics were significantly associated with requiring a pelvic examination for oral contraception. Clinicians in private practice were twice as likely as those in community and family-planning clinics to report always requiring a pelvic examination (OR 2.30; 95% CI 1.28–4.13). Clinicians from the South (OR 1.70; 95% CI 1.10–2.62) and those reporting that half or more of their patients are insured by Medicaid (OR 1.62; 95% CI 1.11–2.37) were also more likely to always require pelvic examinations for oral contraception.
Table 2.
Requirement of a Pelvic Examination for Oral Contraception, Unadjusted and Adjusted Logistic Regression Odds Ratios (n=1,120)
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Clinician characteristics | ||
| Specialty | ||
| MD Ob-gyn | Referent | Referent |
| MD family medicine | 1.20 (0.84–1.70) | 1.51 (1.03–2.21)* |
| APN Ob-gyn/women’s health | 0.48 (0.34–0.70)† | 0.59 (0.39–0.90)* |
| APN family medicine | 1.98 (1 38–2.84)† | 2.38 (1.58–3.59)† |
| Age (y) | 1.03 (1.01–1.04)† | 1.03 (1.01–1.04)‡ |
| White (non-Hispanic) | 0.74 (0.53–1.05) | 0.70 (0.47–1.04) |
| Female | 0.77 (0.57–1.03) | NA |
| Training in family planning | 0.83 (0.79–1.84)* | 1.06 (0.65–1.70) |
| Practice characteristics | ||
| Main clinical practice setting | ||
| Community or family-planning clinic | Referent | Referent |
| Private practice | 1.54 (1.01–2.34)* | 2.30 (1.28–4.13)‡ |
| Hospital-based | 1.26 (0.75–2.12) | 1.59 (0.87–2.92) |
| Rural practice location | 1.03 (0.75–1.42) | 0.84 (0.57–1.23) |
| Region | ||
| West | Referent | Referent |
| Midwest | 1.44 (0.93–2.23) | 1.39 (0.87–2.21) |
| Northeast | 1.31 (0.82–2.10) | 1.13 (0.68–1.89) |
| South | 1.98 (1.33–2.94)‡ | 1.70 (1.10–2.62)* |
| Patient population | ||
| At least half of patients are teenage girls | 0.83 (0.56–1.24) | 0.96 (0.61–1.53) |
| At least half of patients are minority race or ethnicity | 1.42 (1.05–1.94)* | 1.16 (0.81–1.68) |
| At least half of patients use Medicaid | 1.42 (1.05–1.94)* | 1.62 (1.11–2.37)* |
| At least half of patients are uninsured | 1.21 (0.79–1.84) | 1.53 (0.90–2.63) |
| At least half of patients at risk for STIs or HIV or both | 0.80 (0.59–1.07) | 0.78 (0.56–1.09) |
| Design-based Wald test, F (17,1100) | 4.57† | |
APN, advance practice nurse; NA, clinician sex cannot be included in the adjusted model because nearly all advance practice nurses are female; STIs, sexually transmitted infections.
P<.05.
P<.001.
P<.01.
Results from the two patient vignettes show that clinicians who require a pelvic examination for oral contraceptives are also less likely to adhere to current guidelines for women’s reproductive health care promoted by the College and the American Cancer Society,2,18,19 particularly for the adolescent patient (Table 3). The first patient is a 16-year-old female adolescent, never married, nulliparous, sexually active for the past year, and seeing a 22-year-old man for the past 6 months with inconsistent condom use. The second is a young adult woman making a contraceptive visit. She is 24 years old, unmarried, nulliparous, and has a new sexual partner. Those requiring a pelvic examination for oral contraception were more likely to recommend a Pap test and a human papillomavirus test in a visit with the 16-year-old patient, and to recommend a human papillomavirus test for the 24-year-old patient—recommendations that do not conform to current guidelines (the HPV test is not recommended for primary screening before age 30).18,20 Conversely, those requiring the pelvic examination for oral contraceptives were slightly less likely to recommend a chlamydia test for both patients despite guidelines recommending that all women ages 16–24 receive the test.21
Table 3.
Differences in the Clinical Preventive Services Provided to Hypothetical Patients According to Oral Contraception Pelvic Examination Requirements (n=1,136)
| Adolescent Patient Pelvic Examination Always Required for Oral Contraception |
Young Adult Patient Pelvic Examination Always Required for Oral Contraception |
|||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Clinician would provide for this patient | ||||
| Chlamydia test | 93.7 | 96.5* | 85.0 | 90.7† |
| Gonorrhea test | 89.7 | 92.2 | 82.4 | 85.3 |
| Human papillomavirus test | 58.2 | 47.8‡ | 60.0 | 48.8‡ |
| Pap test | 90.5 | 74.2§ | 92.1 | 93.0 |
Data are %.
Adolescent patient: age 16, nulliparous, unmarried, sexual partner of 6 months (age 22), sometimes uses condoms.
Young adult patient: age 24, nulliparous, unmarried, reason for visit contraception, new sexual partner.
Design-based Pearson χ2 test:
P<.1;
P<.05;
P<.01;
P<.001.
DISCUSSION
Clinicians specializing in reproductive health care are more likely than generalist clinicians to adhere to longstanding guidelines recognizing the safety and value of oral contraception provision without the requirement for a pelvic examination, yet nearly one third of ob-gyns ascribe to a pelvic examination requirement. Improvements in access to contraception occur when a pelvic examination is not a prerequisite, as shown in a demonstration project in which more effective methods were adopted by women who deferred the pelvic examination.6 Requiring a pelvic examination for asymptomatic women before dispensing contraception poses an unnecessary medical hurdle before a critical and time sensitive medication.3 When given the option of deferring pelvic examinations, many women choose to do so and value the opportunity to initiate contraceptive use more quickly.6,22 Furthermore, those opting to forgo a pelvic examination are no more likely to be at increased risk of cervical cancer, and those at highest risk make return visits for screening.23
Research literature on provider practices related to contraceptive provision and the pelvic examination is sparse, but our findings are consistent with a prior survey of a smaller sample of ob-gyns who used clinical vignettes to assess pelvic examination requirements.24 Younger physicians and those more closely adhering to American Cancer Society clinical guidelines for cervical cancer screening were more likely to allow a refill of an oral contraceptive prescription without Pap testing. However, the study had limited power to examine other factors associated with practices and included only ob-gyn physicians. The consistent finding with regard to clinician age suggests the need for targeted continuing education, particularly with older clinicians in private practice who are the furthest from their medical training and perhaps from professional networks and incentives for updating protocols.
The necessity of pelvic examinations for optimal reimbursement of a visit may partly explain clinicians’ practice patterns. In the absence of adequate financial incentives for contraceptive counseling as an important clinical activity in its own right, providers are incentivized to conduct a physical examination with a well-reimbursed billing code. The diffusion of clinical guidelines and mechanisms for encouraging their adoption are also uneven, resulting in different levels of knowledge and motivation to change practices.25
Our survey occurred well after the College, the American Cancer Society, and the U.S. Preventive Services Task Force guidelines were updated in 2002 and 2003 reducing the requirement for Pap tests to within 3 years of sexual intercourse or by age 21. Soon after our survey was completed, the College released new guidelines recommending screening begin at age 21, and occur every other year rather than annually until the age of 30, after which time triennial screening may be adopted for low-risk women.26 Even when STI screening is indicated, a speculum examination is not necessary; urine-based testing is preferred by patients, cost-effective, and beneficial.27–30 The pairing of pelvic examinations with oral contraceptive provision has long been a common practice, despite the potential barrier to contraception it can pose. With changing cervical cancer screening guidelines and the availability of urine-based STI screening, the requirement for a pelvic examination for oral contraceptives imposes unnecessary delays to contraceptive delivery and pregnancy risks. Despite the value of clinical preventive screening when it conforms to evidence-based guidelines, women seeking oral contraceptives do not need cancer or STI screening to safely use the medication. Notably, the clinicians requiring a pelvic examination for oral contraceptives also reported cervical cancer and STI screening practices out of step with current guidelines.
These survey data are self-reported and do not necessarily capture actual clinical practice patterns. Social desirability bias could affect responses, with clinicians indicating idealized or professionally normative practices. In addition, variation in the response to the survey by specialty and other characteristics could affect our comparisons by incurring nonresponse bias. The lowest response rate was for the clinicians with a markedly higher adherence to the pelvic examination requirement, older, male, and family medicine physicians. With a higher response rate, we might expect to see even greater divergence from evidence-based guidelines.
CONCLUSION
Because the need for contraception can arise unexpectedly and is time sensitive, a convenient and timely appointment and the opportunity to focus a visit on selecting an effective and suitable method is important. When care is sought for an emergent condition with a specific medical treatment (eg, urinary tract infections), appointments serving the presenting health need are efficiently scheduled. In contrast, in the case of pregnancy prevention, women often must wait to get an appointment for a full gynecologic examination to initiate use of the most commonly used form of contraception. The variation in clinician practices we identified suggests a need for more effective dissemination of guidelines related to oral contraception provision.
Acknowledgments
Supported by NIH/NICHD R01 HD046027. Dr. Henderson’s effort also was supported by an NIH/NICHD Mentored Research Scientist Development Award in Population Research (K01HD054495) and resources from NIH/NCRR/OD UCSF-CTSI (KL2 RR024130).
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial Disclosure
Dr. Harper is an investigator on a research grant through the university from Teva Pharmaceuticals to study Plan B One-Step emergency contraception. The other authors did not report any potential conflicts of interest.
REFERENCES
- 1.World Health Organization. Selected practice recommendations for contraceptive use. 2nd ed. Geneva: WHO; 2004. Available at http://whqlibdoc.who.int/publications/2004/9241562846.pdf. Retrieved June 16, 2010. [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists. Guidelines for women’s health care: a resource manual. 3rd ed. Washington, DC: American College of Obstetricians and Gynecologists; 2007. [Google Scholar]
- 3.Stewart FH, Harper CC, Ellertson CE, Grimes DA, Sawaya GF, Trussell J. Clinical breast and pelvic examination requirements for hormonal contraception: current practice vs evidence. JAMA. 2001;285:2232–2239. doi: 10.1001/jama.285.17.2232. [DOI] [PubMed] [Google Scholar]
- 4.Mosher WD, Jones J. National Center for Health Statistics (U.S.). Use of contraception in the United States: 1982–2008. Hyattsville (MD): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; [Google Scholar]
- 5.Kahn JA, Chiou V, Allen JD, Goodman E, Perlman SE, Emans SJ. Beliefs about Papanicolaou smears and compliance with Papanicolaou smear follow-up in adolescents. Arch Pediatr Adolesc Med. 1999;153:1046–1054. doi: 10.1001/archpedi.153.10.1046. [DOI] [PubMed] [Google Scholar]
- 6.Harper C, Balistreri E, Boggess J, Leon K, Darney P. Provision of hormonal contraceptives without a mandatory pelvic examination: the first stop demonstration project. Fam Plann Perspect. 2001;33:13–18. [PubMed] [Google Scholar]
- 7.Fiddes P, Scott A, Fletcher J, Glasier A. Attitudes towards pelvic examination and chaperones: a questionnaire survey of patients and providers. Contraception. 2003;67:313–317. doi: 10.1016/s0010-7824(02)00540-1. [DOI] [PubMed] [Google Scholar]
- 8.Leader S, Perales P. Provision of primary-preventive health care services by obstetrician-gynecologists. Obstet Gynecol. 1995;85:391–395. doi: 10.1016/0029-7844(94)00411-6. [DOI] [PubMed] [Google Scholar]
- 9.Scholle SH, Chang JC, Harman J, McNeil M. Trends in women’s health services by type of physician seen: data from the 1985 and 1997–98 NAMCS. Women’s Health Issues. 2002;12:165–177. doi: 10.1016/s1049-3867(02)00139-1. [DOI] [PubMed] [Google Scholar]
- 10.Henderson JT, Weisman CS. Women’s patterns of provider use across the lifespan and satisfaction with primary care coordination and comprehensiveness. Med Care. 2005;43:826–833. doi: 10.1097/01.mlr.0000170422.73033.eb. [DOI] [PubMed] [Google Scholar]
- 11.Frost JJ. Trends in US women’s use of sexual and reproductive health care services, 1995–2002. Am J Public Health. 2008;98:1814–1817. doi: 10.2105/AJPH.2007.124719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harper CC, Henderson JT, Schalet A, Becker D, Stratton L, Raine TR. Abstinence and teenagers: prevention counseling practices of health care providers serving high-risk patients in the United States. Perspect Sex Reprod Health. 2010;42:125–132. doi: 10.1363/4212510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henderson JT, Raine T, Schalet A, Blum M, Harper CC. “I wouldn’t be this firm if I didn’t care”: preventive clinical counseling for reproductive health. Patient Educ Couns 2010. 2010 Jun 15; doi: 10.1016/j.pec.2010.05.015. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hauptman PJ, Swindle J, Hussain Z, Biener L, Burroughs TE. Physician attitudes toward end-stage heart failure: a national survey. Am J Med. 2008;121:127–135. doi: 10.1016/j.amjmed.2007.08.035. [DOI] [PubMed] [Google Scholar]
- 15.Lawrence RE, Curlin FA. Physicians’ beliefs about conscience in medicine: a national survey. Acad Med. 2009;84:1276–1282. doi: 10.1097/ACM.0b013e3181b18dc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kahn JM, Asch RJ, Iwashyna TJ, Haynes K, Rubenfeld GD, Angus DC, et al. Physician attitudes toward regionalization of adult critical care: a national survey. Crit Care Med. 2009;37:2149–2154. doi: 10.1097/CCM.0b013e3181a009d0. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence RE, Curlin FA. Autonomy, religion and clinical decisions: findings from a national physician survey. J Med Ethics. 2009;35:214–218. doi: 10.1136/jme.2008.027565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saslow D, Runowicz CD, Solomon D, Moscicki AB, Smith RA, Eyre HJ, et al. American Cancer Society. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52:342–362. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- 19.American College of Obstetricians and Gynecologists, Committee on Adolescent Health Care. Health care for adolescents. Washington, DC: American College of Obstetricians and Gynecologists; 2003. [Google Scholar]
- 20.Human papillomavirus. Practice Bulletin No. 61. Clinical Management Guidelines for Obstetrician-Gynecologists. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;61:905–918. doi: 10.1097/00006250-200504000-00056. [DOI] [PubMed] [Google Scholar]
- 21.Berg AO. Screening for chlamydia infection: recommendations and rationale. Am J Prev Med. 2001;20(3 suppl):90–94. [PubMed] [Google Scholar]
- 22.Armstrong KA, Stover MA. SMART START: an option for adolescents to delay the pelvic examination and blood work in family planning clinics. J Adolesc Health. 1994;15:389–395. doi: 10.1016/1054-139x(94)90262-3. [DOI] [PubMed] [Google Scholar]
- 23.Sawaya GF, Harper C, Balistreri E, Boggess J, Darney P. Cervical neoplasia risk in women provided hormonal contraception without a Pap smear. Contraception. 2001;63:57–60. doi: 10.1016/s0010-7824(01)00175-5. [DOI] [PubMed] [Google Scholar]
- 24.Schwarz EB, Saint M, Gildengorin G, Weitz TA, Stewart FH, Sawaya GF. Cervical cancer screening continues to limit provision of contraception. Contraception. 2005;72:179–181. doi: 10.1016/j.contraception.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 25.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cervical cytology screening. Practice Bulletin No. 109. American College of Obstetricians and Gynecologists. American College of Obstetricians and Gynecologists. 2009;114:1409–1420. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 27.Serlin M, Shafer MA, Tebb K, Gyamfi AA, Moncada J, Schachter J, et al. What sexually transmitted disease screening method does the adolescent prefer?. Adolescents’ attitudes toward first-void urine, self-collected vaginal swab, and pelvic examination. Arch Pediatr Adolesc Med. 2002;156:588–591. doi: 10.1001/archpedi.156.6.588. [DOI] [PubMed] [Google Scholar]
- 28.Shafer MA, Pantell RH, Schachter J. Is the routine pelvic examination needed with the advent of urine-based screening for sexually transmitted diseases? Arch Pediatr Adolesc Med. 1999;153:119–125. doi: 10.1001/archpedi.153.2.119. [DOI] [PubMed] [Google Scholar]
- 29.Blake DR, Duggan A, Quinn T, Zenilman J, Joffe A. Evaluation of vaginal infections in adolescent women: can it be done without a speculum? Pediatrics. 1998;102(4 pt 1):939–944. doi: 10.1542/peds.102.4.939. [DOI] [PubMed] [Google Scholar]
- 30.Blake DR, Maldeis N, Barnes MR, Hardick A, Quinn TC, Gaydos CA. Cost-effectiveness of screening strategies for Chlamydia trachomatis using cervical swabs, urine, and self-obtained vaginal swabs in a sexually transmitted disease clinic setting. Sex Transm Dis. 2008;35:649–655. doi: 10.1097/OLQ.0b013e31816ddb9a. [DOI] [PMC free article] [PubMed] [Google Scholar]