Abstract
Human subcutaneous dirofilariasis is caused by filarial worms of the genus Dirofilaria. The parasites are transmitted to man by mosquitoes. We report three cases of human subcutaneous dirofilarias caused by Dirofilaria repens from Dibrugarh, Assam, north east India. The cases presented as subcutaneous nodules, on the chest, cheek and the anterior abdominal wall. Noting the frequency of the cases reported within 6 months, it is emphasized that subcutaneous dirofilariasis is a potentially emerging zoonosis in Assam and should be included in the differential diagnosis of patients presenting with subcutaneous nodules in Assam.
KEY WORDS: Dirofilariasis, human, subcutaneous infection
Dirofilariasis is a zoonotic disease, thought to be rare among human beings. The natural hosts for the Dirofilaria species that cause infection in man are dogs and wild canines like foxes, wolves and raccoons. Infected mosquito occasionally infect human with the third stage larvae during a blood meal. In man, Dirofilaria repens usually wanders in the subcutaneous tissue or produces a granulomatous nodule. Though considered rare, cases of human dirofilarias are increasingly being reported in the last few decades from all over the world, and it can be considered an emerging zoonosis.[1] Most of the cases reported from India are ocular dirofilariasis where the worm is detected most commonly in the sub-conjunctival or peri-orbital tissue.[2,3,4] Few reports of subcutaneous dirofilarias are from India.[5,6,7] It is being reported from several countries and the number is gradually increasing.[8,9,10] We report 3 cases here of human subcutaneous dirofilariasis from Assam; north eastern region of India. Ocular dirofilariasis from this region has been already reported by us in the past.
THE CASES
Case 1
A 43-year-old woman from Sibsagar district of Assam reported with a gradually increasing swelling (2 cm × 1 cm) for one year on the chest wall over the sternum. There was no associated itching, pain or discharge from the swelling. She gave a history of getting a course of oral antibiotic once without improvement. On surgical excision of the nodule, a partially disintegrated white, thread like a worm of 5 cm in length was extracted [Figure 1a]. Patient's blood was checked for microfilaremia, but no microfilaria was detected in her blood.
Figure 1.

(a-c) Macroscopic view of the worms
Case 2
A 30-year-old man attended a private hospital in Dibrugarh district with a gradually increasing swelling of 2 cm × 2 cm size for one year on the right cheek. He gave a history of periodical redness, pain and itching for which he was treated symptomatically. The swelling was attached to buccinator muscle underneath and on excision a live, intact, thin, white worm of 12 cm in length came out [Figure 1b]. Patient was checked for microfilaremia and was found to be negative.
Case 3
A 21-year-old male reported to the surgery out patient department of a teaching hospital with a swelling in the right side of the lower abdomen since 2 months. It started as a small swelling of 1 cm × 1 cm but gradually increased in size to 2 cm × 3 cm with history of periodical itching. On examination, a small movable cystic swelling was found in the right lower quadrant of the anterior abdominal wall. On surgical excision, the cyst was found to be subcutaneous with no attachment to the underlying tissue. On opening the cyst, a live, 12 cm long, white thin worm was found [Figure 1c]. The patient was tested for microfilaremia, which was found to be negative.
The worms were fixed in formalin and cleared in glycerine for proper viewing of the structures. The worms were white, elongated, 0.5 mm thick and 5 cm to 12 cm in length. The two ends of the intact worms were comparatively thin. The multi layered cuticle showed distinct longitudinal ridges [Figure 2] and transverse striations [Figure 3]. The cuticle of the first worm was disintegrated at places. The spaces between the ridges were equal to the length of the ridges themselves. The muscle cells were well developed [Figure 4]. The genus Dirofilaria was identified by its thick, multi layered cuticle with ridging and transverse striations, large muscle cells and prominent lateral cord. The paired uteri and the intestinal tube were seen in two of the worms [Figure 4]. Based on size, cuticular and internal morphologic features the second and the third worm were identified as adult female of D. repens while speciation of the first worm could not be done though it was identified as Dirofilaria.
Figure 2.
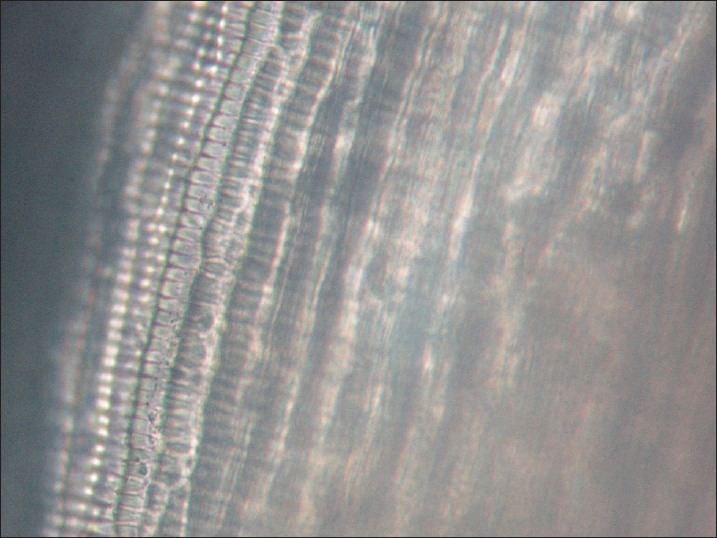
Microscopic view of worm showing longitudinal cuticular ridges
Figure 3.
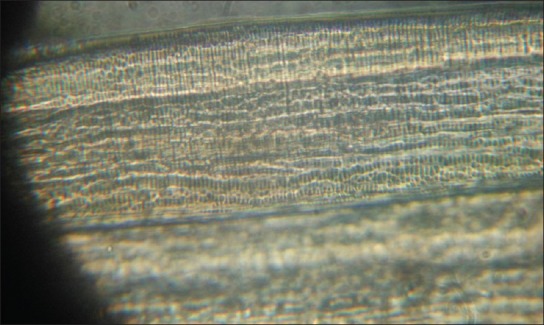
Microscopic view of the surface of a worm showing transverse striations
Figure 4.
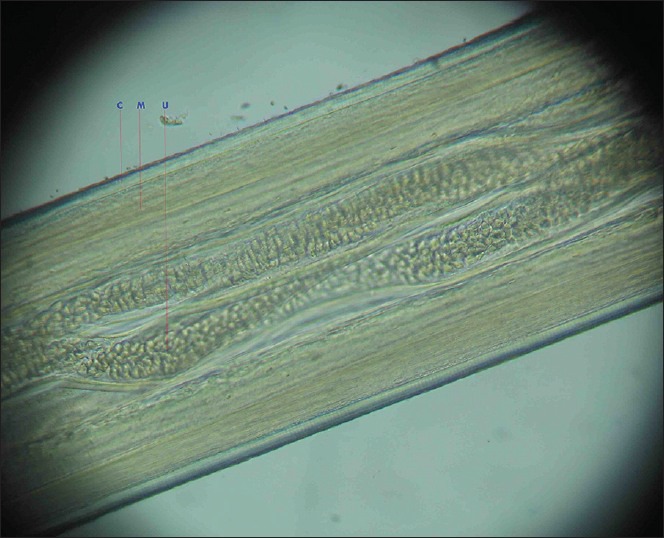
Microscopic view showing the well-developed muscle layer and uteri of the female worm. (C-Multi layered cuticle, M-Musclelayer, U-Uterinecavity)
DISCUSSION
Human dirofilariasis is a rare infection caused by Dirofilaria, the nematode. The life cycle of the worm depends upon two hosts, a vertebrate species, i.e., a domestic or wild animal which is a definitive host and a blood sucking zoo-anthropophilic arthropod like Culex, Anopheles or Aedes mosquito which acts as an intermediate host for Dirofilaria immitis and D. repens;[11,12] both species have been reported from India. The adult worm of D. repens lives in the subcutaneous tissues of the definitive host and produces microfilariae which circulate in the blood and are transmitted through blood sucking insects like mosquitoes.[13] D. immitis inhabits the right ventricle and pulmonary arteries of dogs.[14] D. immitis has also been found to be associated with human pulmonary dirofilariasis.[15,16] Both species can infect humans. The development in the mosquito takes about 2 weeks and the infective third stage larvae migrate actively through the mouth parts and enter the tissue of the vertebrate.[13] After inoculation of the infective third stage larvae into humans, who are accidental hosts, they can invade a variety of tissues and undergo some development without any response from the host.[17] However, there is a report of D. repens infection with a subcutaneous gravid female worm with development of eosinophilia and concomitant development of meningo encephalitis and aphasia.[18]
In our first case, the patient did not complain of any itching, reddening or pain. On the excision of the nodule, a dead partially disintegrated worm on the surface was detected. On the contrary, our second and third case with the nodule on the cheek and anterior abdominal wall complained of periodical reddening, itching, pain and increase in size for which they were treated symptomatically with oral antibiotics and anti-allergic drugs. On the excision of the nodules, intact live adult female D. repens were detected from both the cases.
Several reports have noted that the most significant risk factors for human infections are mosquito density, warm climate with extended mosquito breeding season, outdoor human activities with an abundance of microfilaremic dogs.[17,19] Most of these criteria are fulfilled in eastern Assam; however, the frequency of microfilaremic dogs with D. repens are not known. Anopheles, Culex and Aedes mosquito borne human diseases are prevalent in Eastern Assam. High prevalence in dogs increase the incidence of human cases. Though we searched literature we have not found any study of microfilaremia of D. repens in dogs in Assam, North East India. In one postmortem study of dogs from North-East India, they found D. immitis in 34% cases.[20] Two recent surveys of microfilaraemic dogs in Kerala and Karnataka States in Southern India, found only D. repens at the prevalence of 7% and 21% respectively.[21,22] Both D. immitis and D. repens were isolated at post-mortem examination from 57% and 14% of dogs respectively in Orissa.[23]
One indigenous human infection of D. immitis is recently reported from Bangladesh.[24] Earlier we have reported 3 cases of human ocular dirofilariasis cases from Dibrugarh and Tinsukia districts of Eastern Assam presenting as peri-orbital as well as subconjunctival cyst caused by D. repens.[4] These 3 sub cutaneous cases are also reported from Dibrugarh and Sibsagar districts from Eastern Assam within a period of 6 months in 2011. Therefore, we can assume that many more people may have been infected than those that are already reported. Asymptomatic cases usually do not report to the hospital, which may be one reason for lesser case reports.
Subcutaneous nodules are most commonly found in the head, neck, extremities and thoracic wall as in our cases.[25] Subcutaneous infections are also being reported from lip, breast, axilla, peri-orbital tissue, and abdomen as in our third case.[6,17,26] Excision and biopsy is both diagnostic and therapeutic. The identification is based on morphological features of the parasite. Species identification is difficult on morphologic grounds because many other Dirofilaria species have been described that are similar morphologically with D. repens. In India, the most important species responsible is D. repens. But D. immitis is also reported from one subcutaneous nodule from South India.[27]
In India, most of the studies reported, identification is done based on morphological features. Precise identification can be achieved with DNA analysis, based on polymerase chain reaction which may not always be possible in clinical laboratories as a large number of specific probes are required for specific diagnosis.[17,28] Polymerase Chain reaction is less effective in worms that are fixed in formalin. For molecular diagnosis worms should be fixed in ethanol.
Subcutaneous dirofilariasis is considered a re-emerging zoonosis, transmitted by mosquitoes, found to be endemic in Southern and Eastern Europe and Asia, particularly Srilanka, Malaysia and India. This parasitosisis increasingly being reported from different countries and is also reported from Assam, North East India. Mosquito borne parasitic and viral diseases are quite common in Assam. To know the exact prevalence of this infection in this area needs further study of the vectors, hosts and environmental factors.
This report emphasizes that this infection is a potentially emerging zoonosis in Assam, though probably under reported. Subcutaneous dirofilariasis can be included as differential diagnosis of subcutaneous nodules in Assam.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Pampiglione S, Rivasi F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens: An update of world literature from 1995 to 2000. Parassitologia. 2000;42:231–54. [PubMed] [Google Scholar]
- 2.Mahesh G, Giridhar A, Biswas J, Saikumar SJ, Bhat A. A case of periocular dirofilariasis masqueradingasalid tumour. Indian J Ophthalmol. 2005;53:63–4. doi: 10.4103/0301-4738.15290. [DOI] [PubMed] [Google Scholar]
- 3.Sekhar HS, Srinivasa H, Batru RR, Mathai E, Shariff S, Macaden RS. Human ocular dirofilariasis in Kerala Southern India. Indian J Pathol Microbiol. 2000;43:77–9. [PubMed] [Google Scholar]
- 4.Nath R, Gogoi R, Bordoloi N, Gogoi T. Ocular dirofilariasis. Indian J Pathol Microbiol. 2010;53:157–9. doi: 10.4103/0377-4929.59213. [DOI] [PubMed] [Google Scholar]
- 5.Sathyan P, Manikandan P, Bhaskar M, Padma S, Singh G, Appalaraju B. Subtenons infection by Dirofilaria repens. Indian J Med Microbiol. 2006;24:61–2. doi: 10.4103/0255-0857.19899. [DOI] [PubMed] [Google Scholar]
- 6.Padmaja P, Kanagalakshmi, Samuel R, Kuruvilla PJ, Mathai E. Subcutaneous dirofilariasis in Southern India: A case report. Ann Trop Med Parasitol. 2005;99:437–40. doi: 10.1179/36485905X36253. [DOI] [PubMed] [Google Scholar]
- 7.Khurana S, Singh G, Bhatti HS, Malla N. Human subcutaneous dirofilariasis in India: A report of three cases with a brief review of the literature. Indian J Med Microbiol. 2010;28:394–6. doi: 10.4103/0255-0857.71836. [DOI] [PubMed] [Google Scholar]
- 8.Pampiglione S, Canestri Trotti G, De Santolo GP, Fabbri F, Garavelli PL, Mastinu A, et al. Human subcutaneous dirofilariasis: 8 new cases in Northern Italy. Pathologica. 1994;86:396–400. [PubMed] [Google Scholar]
- 9.Athari A. Zoonotic subcutaneous dirofilariasesiniran. Arch Iran Med. 2003;6:63–5. [Google Scholar]
- 10.Ratnatunga N, Wijesundera MS. Histopathological diagnosis of subcutaneous Dirofilaria repens infection in humans. Southeast Asian J Trop Med Public Health. 1999;30:375–8. [PubMed] [Google Scholar]
- 11.Simón F, Kramer LH, Román A, Blasini W, Morchón R, Marcos-Atxutegi C, et al. Immunopathology of Dirofilaria immitis infection. Vet Res Commun. 2007;31:161–71. doi: 10.1007/s11259-006-3387-0. [DOI] [PubMed] [Google Scholar]
- 12.Cancrini G, Romi R, Gabrielli S, Toma L, DI Paolo M, Scaramozzino P. First finding of Dirofilariarepensina natural population of Aedesalbopictus. Med Vet Entomol. 2003;17:448–51. doi: 10.1111/j.1365-2915.2003.00463.x. [DOI] [PubMed] [Google Scholar]
- 13.Orihel TC. Dirofilariacory nodes (Von Linstow, 1899): Morphology and life history. J Parasitol. 1969;55:94–103. [PubMed] [Google Scholar]
- 14.Byeon KH, Kim BJ, Kim SM, Yu HS, Jeong HJ, Ock MS. A serological survey of Dirofilaria immitis infection in pet dogs of Busan, Korea, and effects of chemoprophylaxis. Korean J Parasitol. 2007;45:27–32. doi: 10.3347/kjp.2007.45.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darrow JC, Lack EE. Solitary lung nodule due to Dirofilaria immitis (dog” heartworm”) J Surg Oncol. 1981;16:219–24. doi: 10.1002/jso.2930160304. [DOI] [PubMed] [Google Scholar]
- 16.Foroulis CN, Khaldi L, Desimonas N, Kalafati G. Pulmonary dirofilariasis mimicking lung tumor with chest wall and mediastinalinvasion. Thorac Cardiovasc Surg. 2005;53:173–5. doi: 10.1055/s-2004-830567. [DOI] [PubMed] [Google Scholar]
- 17.Maltezos ES, Sivridis EL, Giatromanolaki AN, Simopoulos CE. Human subcutaneous dirofilariasis: A report of three cases manifesting as breast oraxillary nodules. Scott Med J. 2002;47:86–8. doi: 10.1177/003693300204700404. [DOI] [PubMed] [Google Scholar]
- 18.Poppert S, Hodapp M, Krueger A, Hegasy G, Niesen WD, Kern WV, et al. Dirofilaria repens infection and concomitant meningo encephalitis. Emerg Infect Dis. 2009;15:1844–6. doi: 10.3201/eid1511.090936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orihel TC, Eberhard ML. Zoonotic filariasis. Clin Microbiol Rev. 1998;11:366–81. doi: 10.1128/cmr.11.2.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borthakur SK, Sarmah K, Rajkhowa TK, Das MR, Rahman S. Dirofilaria immitis infection in dog. J Vet Parasitol. 2006;20:167–9. [Google Scholar]
- 21.Sabu L, Devada K, Subramanian H. Dirofilariosis in dogs and humans in Kerala. Indian J Med Res. 2005;121:691–3. [PubMed] [Google Scholar]
- 22.Ananda KJ, D′Souza PE, Jagannath MS. Methods for identification of microfilaria of Dirofilaria repens and Dipetalone mareconditum. J Vet Parasitol. 2006;20:45–7. [Google Scholar]
- 23.Patnaik MM. On filarialnematodes in domestic animals in Orissa. Indian Vet J. 1989;66:573–4. [Google Scholar]
- 24.Fuehrer HP, Treiber M, Silbermayr K, Baumann TA, Swoboda P, Joachim A, et al. Indigenous Dirofilaria immitis in Bangladesh. Parasitol Res. 2013 Jan 29; doi: 10.1007/s00436-013-3311-9. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 25.Pampiglione S, Canestri Trotti G, Rivasi F. Human dirofilarias is due to Dirofilaria (Nochtiella) repens: Are view of world literature. Parassitologia. 1995;37:149–93. [PubMed] [Google Scholar]
- 26.Pampiglione S, Canestri Trotti G, Rivasi F, Vakalis N. Human dirofilariasis in Greece: Are view of reported cases and a description of a new, subcutaneous case. Ann Trop Med Parasitol. 1996;90:319–28. doi: 10.1080/00034983.1996.11813057. [DOI] [PubMed] [Google Scholar]
- 27.Teerthanath S, Hariprasad S. A case of Dirofilaria immitis presenting as an in tramuscular soft tissue mass. Indian J Pathol Microbiol. 2011;54:428–30. doi: 10.4103/0377-4929.81620. [DOI] [PubMed] [Google Scholar]
- 28.Favia G, Lanfrancotti A, dellaTorre A, Cancrini G, Coluzzi M. Advances in the identification of Dirofilaria repens and Dirofilaria immitis by a PCR-based approach. Parassitologia. 1997;39:401–2. [PubMed] [Google Scholar]


