Abstract
The evidence for optimal management of Mason type III fracture of radial head is unclear hence a systematic review of the published literature was performed in April 2012. This review includes 5 prospective studies (including 2 randomized trials), 4 retrospective studies and 9 case series. No study can be interpreted as level 1 evidence. Level 2 and 3 evidence provides some insight into the success of each modality through subjective and objective measurements of function and complication rates. Radial head replacement, open reduction internal fixation (ORIF) and radial head resection all provide satisfactory outcomes for patients in most cases. One treatment modality cannot be recommended over any other due to the small number of clinical trials and cases included in each study. Further randomized control trials are needed to evaluate the full benefits and shortcomings of each of the different surgical treatment modalities.
Keywords: Radial head fracture, radial head open reduction internal fixation, radial head replacement, type III Mason fracture, radial head resection
INTRODUCTION
The Mason classification of radial head fractures was described by Mason in 1954.1 Mason type III fracture of the radial head is defined as a comminuted, displaced fracture involving the entire radial head.1 The optimal management of Mason type III fractures of the radial head is controversial and the evidence for it is unclear. The aim of this systematic review is to explore what evidence exists regarding the clinical outcomes of radial head replacement [Figure 1], open reduction and internal fixation (ORIF) [Figure 2a and b] and radial head resection for Mason type III fractures. We aimed to provide an overview of the existing evidence on how Mason type III fractures of the radial head should be optimally managed by comparing the outcomes and complications of each modality of management.
Figure 1.
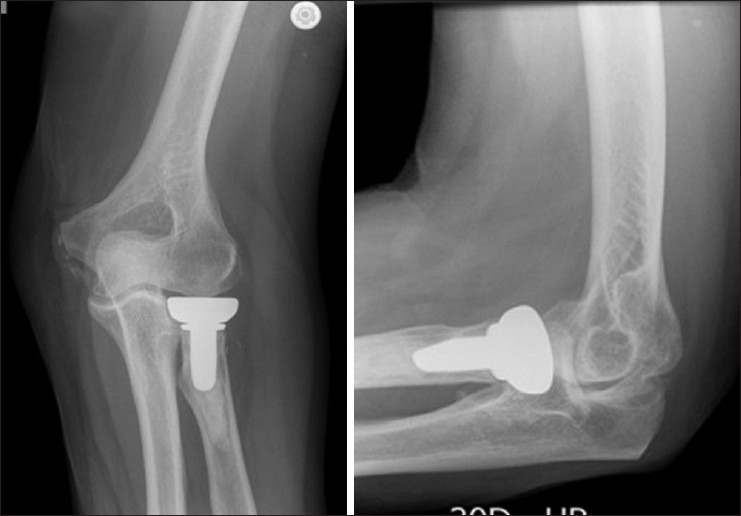
Anteroposterior (AP) and lateral radiographs showing radial head prosthesis (Acumed LLC, Hillsboro, OR, USA)
Figure 2.

Anteroposterior (a) and lateral (b) radiograph of the elbow showing ORIF of the radial head
Search strategy and criteria
A review of the current literature was performed in April 2012. To establish the current evidence that exists for Mason type III fracture management, we searched current literature through common medical databases including The Cochrane Library, PubMed, Medline and Cinahl. All randomized control trials, nonrandomized studies and case series were included in our data search.
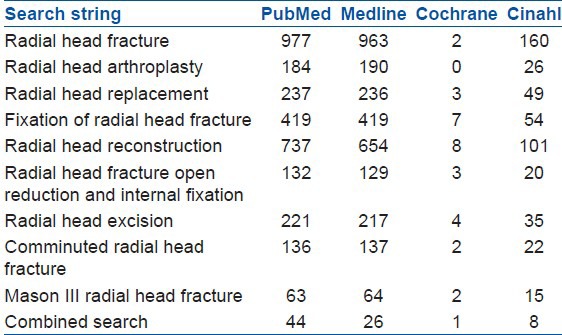
We used several search strings targeting the topic for review. The resultant number of articles produced by each search string is listed according to database [Table 1]. We also performed a combined search using all the search terms simultaneously. The total number of articles produced from the combined search is listed.
Table 1.
Search strings used and the number of results generated from databases
Inclusion criteria
(a) Articles relevant to Mason type III radial head fractures and their surgical management (b) Published in English language (c) Articles with eight or more patients in a single treatment modality (d) Minimum followup of 12 months.
Exclusion criteria
(a) Review articles (b) Undefined number of patients with Mason type III radial head fracture.
All studies were reviewed by two authors (AH, GM) independently and where disparity between the authors was noted, a third party (RH) co-reviewed.
From the initial 79 references from the combined search, 63 were excluded due to irrelevance, duplication, or in accordance with our exclusion criteria. Further articles were also sought from relevant references of the articles extracted from the search. Two articles were included following independent review. The total number of articles included for final review were 18. The level of evidence was based on the categories as outlined by the Centre for Evidence Based Medicine, Oxford, UK.2 No level 1 evidence was found.
Level II and III evidence
Radial head replacements
There are only two small cohort studies on radial head replacements for treatment of Mason type III radial head fractures. Smets et al.3 reported results from their multicenter trial using a bipolar prosthesis (Tornier Inc., Montbonnot Saint Martin, France) after 25.2 months of average followup. In this study, 13 Mason type III fractures were managed by radial head replacements. The average age was 46 years (range 20-64 years). Functional outcomes of these 13 patients using the Mayo Elbow Performance Index (MEPI)4 were evaluated. Their results showed seven excellent, three good, one fair and two poor outcomes. One patient with a poor outcome required removal of prosthesis. Average range of motion at the elbow showed moderate deficits. Active flexion averaged 135.5° (range 120°-140°), extension deficit averaged 16.3° (range 0-45°), active pronation averaged 79.3° (range 0-90°) and active supination averaged 83° (range 0-90°). The authors believed that these results were comparable to the successful outcomes presented in several case series of radial head replacements.
Moro et al.5 completed a retrospective study of 10 patients with Mason type III fractures treated with radial head replacements (Smith and Nephew Richards, Memphis, TN, USA) over an average of 2 years. The average age was 47 years (range 28-63 years). Patients in this study had injuries deemed too severe to have undergone ORIF and most cases had other significant injuries of the upper limb as a result of trauma. The study monitored functional outcomes according to the MEPI and the Disability of Arm, Shoulder and Hand (DASH) score.4 Both assessments compared the function of the injured arm with the contralateral arm. Average grip strength was significantly reduced with an average measurement of 28 kg compared with 34 kg in the uninjured arm (P < 0.05). Range of motion was also reduced compared to the uninjured arm. Average pronation was 78° compared to 79°, supination 69° compared to 77°, elbow flexion 140° compared to 143° and elbow extension deficit was 8° compared to full extension on the uninjured side (P < 0.05). Hand dominance was not reported. Six patients suffered complications, including elbow stiffness, ulnar nerve dysesthesia, varying levels of heterotopic ossification, one superficial infection and one patient developed a regional sympathetic-mediated pain syndrome. It was noted by the authors that three patients were not able to return to preinjury activities and/or employment, thus accordingly the MEPI had poor outcomes. Some of the poor outcomes documented in this article could be attributed to other concomitant injuries and other comorbid conditions.
Radial head replacement compared with ORIF
Chen et al.6 conducted a prospective randomized trial on radial head prosthesis versus ORIF in 45 patients with Mason type III radial head fractures between January 2004 and June 2007. The average age of the patients was 37 years (range 19-68 years). There were 45 patients randomly allocated as 22 patients in the radial head replacement group and 23 patients in the ORIF group. The average followup was 2.8 years (range 1-5 years). Postoperative management of the patients receiving radial head replacements involved early mobilization after 3-7 days. Those who underwent ORIF had a 4-week period of immobilization. The patients were assessed according to the Broberg and Morrey scoring system.7 Complication rates including range of motion deficit >30°, stiffness, fragment displacement, deep infection, heterotopic ossification and lack of bone healing. The satisfaction levels according to the Broberg and Morrey Rating Index were higher in the replacement group. The postoperative complication rate was lower in the replacement group (P < 0.01). There were three complications in the replacement group with one case of stiffness and two cases losing range of motion >30°. There were 11 complications in the ORIF group with 4 losing range of motion >30°, 3 loss of fixation, 2 heterotopic ossification, 1 nonunion and 1 deep wound infection. The significance of this finding must also be analyzed with consideration of the two different postoperative rehabilitation protocols involved and their potential influence. There is no mention of whether assessors were blinded to the treatment group postoperatively.
Another prospective trial was conducted by Ruan et al.,8 comparing the outcome after radial head replacement and ORIF. Twenty two consecutive patients with Mason type III fractures were randomized into ORIF or replacement groups. Fourteen patients had cemented bipolar radial head replacements (Tornier Inc., Montbonnot Saint Martin, France) and eight had ORIF using cannulated screws and K-wires. Average age in the replacement group was 37.4 years, compared to an average age of 40.1 years in the ORIF group (P > 0.05). The mean followup was 15.9 months for those who underwent replacement and 14 months for those who underwent ORIF. Their postoperative management protocol was similar to that in Chen et al.'s study.6 Early motion was allowed in the replacement group, while a period of 4 weeks of immobilization was used post ORIF. The outcome measures were also similar to those of Chen et al.,6 using the Broberg and Morrey system to assess functional outcomes. Complications were recorded. 92.9% of those who underwent radial head replacement had satisfactory functional scores, compared with only 12.5% in those who underwent ORIF (P < 0.001). Complications included nonunion, bone resorption and K-wire loosening in four of the eight ORIF patients. There were three patients who developed differing levels of heterotopic ossification in the replacement group, but there were no other significant complications in the replacement group. The authors concluded that using cemented bipolar radial head prosthesis was better than ORIF for the treatment of Mason type III radial head fractures.
Open reduction internal fixation
Koslowsky et al.9 evaluated 90 patients with radial head fractures between 1997 and 2002 in a prospective study. Average patient age was 38 years (range 45-63 years). The aim of their study was to evaluate the outcome of patients following ORIF using 1.2-mm and 1.6-mm Fragment Fixation System (FFS; Orthofix, Bussolengo, Italy) of different Mason types of radial head fractures. All patients underwent a period of immobilization with an above-elbow plaster for a period of 6 days. After 6 days, each patient received daily physiotherapy and 50 mg of indomethacin twice daily for 6 weeks. Koslowsky et al. found that the 12 patients with Mason type III fractures achieved an average Broberg and Morrey score of 97 (range 84-100) after 12-43 months. There was no joint instability or deformity. The average range of motion was 120° flexion, 5° loss of extension, 85° pronation and 85° supination. Complications included two cases of partial migration, one of which required partial hardware removal. There were four cases of mild arthritis.
A comprehensive study of ORIF in radial head fractures by Ring10 shows the relatively poor outcome from the operation in Mason type III fracture. This study followed up 16 of 26 original cases to an average of 44 months (range 25-102 months). Twenty two patients were treated with plate and screws (Synthes., Paoli, Pennsylvania, USA), four cases with oblique screws alone and in three cases ancillary K-wires were used. Of the 26 original cases of Mason type III fractures in this study, 10 required radial head resection at an average of 8 months following their original operation. The major indication for resection was painful crepitus, but other indications included hardware loosening and nonunion. The results were then based on the remaining 16 cases. Results in this study are poor compared to many of the other studies analyzed in this review. Using the Broberg and Morrey Index,7 only five cases scored an excellent rating, seven were rated good, three fair and one poor. The mean score was 86 (range 51-99). Average range of motion was 111° arc, 129° flexion, 18° loss of extension, 59° supination and 67° pronation. The authors noted that there was a significant relationship between the degree of articular comminution (more than three articular fragments) and the prevalence of an unsatisfactory result (P < 0.001).10
Open reduction internal fixation compared to radial head resection
In a small prospective study, Ikeda et al.11 compared ORIF to resection of the radial head for treatment of Mason type III fractures in 28 patients. Fifteen patients underwent radial head resection and 13 underwent ORIF. Treatment selection and method of randomization is not reported. Average age was 41.1 years in the resection group and 38.2 years in the ORIF group. Outcome measures included a functional assessment using the Broberg and Morrey scoring system, pain scores, radiographic findings and arm strength by Cybex testing. Patients who underwent ORIF had significantly higher Broberg and Morrey score (90.7-81.4, P < 0.01) and higher American Surgeons’ Elbow Assessment Scoring System4 scores (P < 0.01), compared to those who had a radial head resection. Their results report an overall greater loss in strength, pronation and supination in the resection group compared with the ORIF group. Patients who underwent ORIF had a subsequent procedure to remove the plates, usually 5-7 months after the initial operation. The influence of a second procedure on any potential loss of motion should be considered with the analysis of these results.
Radial head resection
Janssen et al.12 performed a long term retrospective study to evaluate the outcome of 21 patients who underwent radial head resection. They followed up 21 patients to 6 and 12 years, but only 18 patients were followed up at 16 and 30 years postinjury. Three patients were lost to the latest (16 and 30 years) followup. The age range and hand dominance of the patients were not reported. They used a modified version of the Morrey scoring system to assess the patients. Seventeen out of the 18 patients followed up at 16-30 years had continued their previous occupation. Only one patient had a poor outcome, having to change his job and his recreational activities because of poor postoperative function. From the data including all 21 patients initially enrolled in this study, 17 scored excellent, 3 good and 1 fair at their most recent evaluation (ranging from 6 to 30 years). No patients had symptoms of instability, wrist degeneration, or limited elbow flexion. Eleven patients had mild elbow degeneration, four had ongoing pain, eight had loss of extension, one had limited pronation and two had limited supination. The authors recommend early resection and mobilization for Mason type III fractures to avoid future functional impairment. The authors also discuss the importance of humeral chondral damage and heterotopic ossification on the functional outcome of the elbow. This series does not have the statistical power to conclude on the statistical significance of such factors.
Goldberg et al.13 completed a retrospective study to evaluate the outcome of 36 radial head fractures, 16 of which were Mason type III fractures and were treated with excision of the radial head. The followup for this study was 3-27 years (mean 16.4 years). They reported on elbow carrying angles, range of motion, stability, strength and radiographic findings. Goldberg et al. did not report data on different Mason types of radial head fractures. However, 31 of 36 patients reported subjective satisfaction with their elbow function. Nine of the 36 reported varying levels of pain. Nineteen of the 36 reported weakness of the affected arm. It is unclear from this article what proportions of these outcomes are specifically following Mason type III fractures.
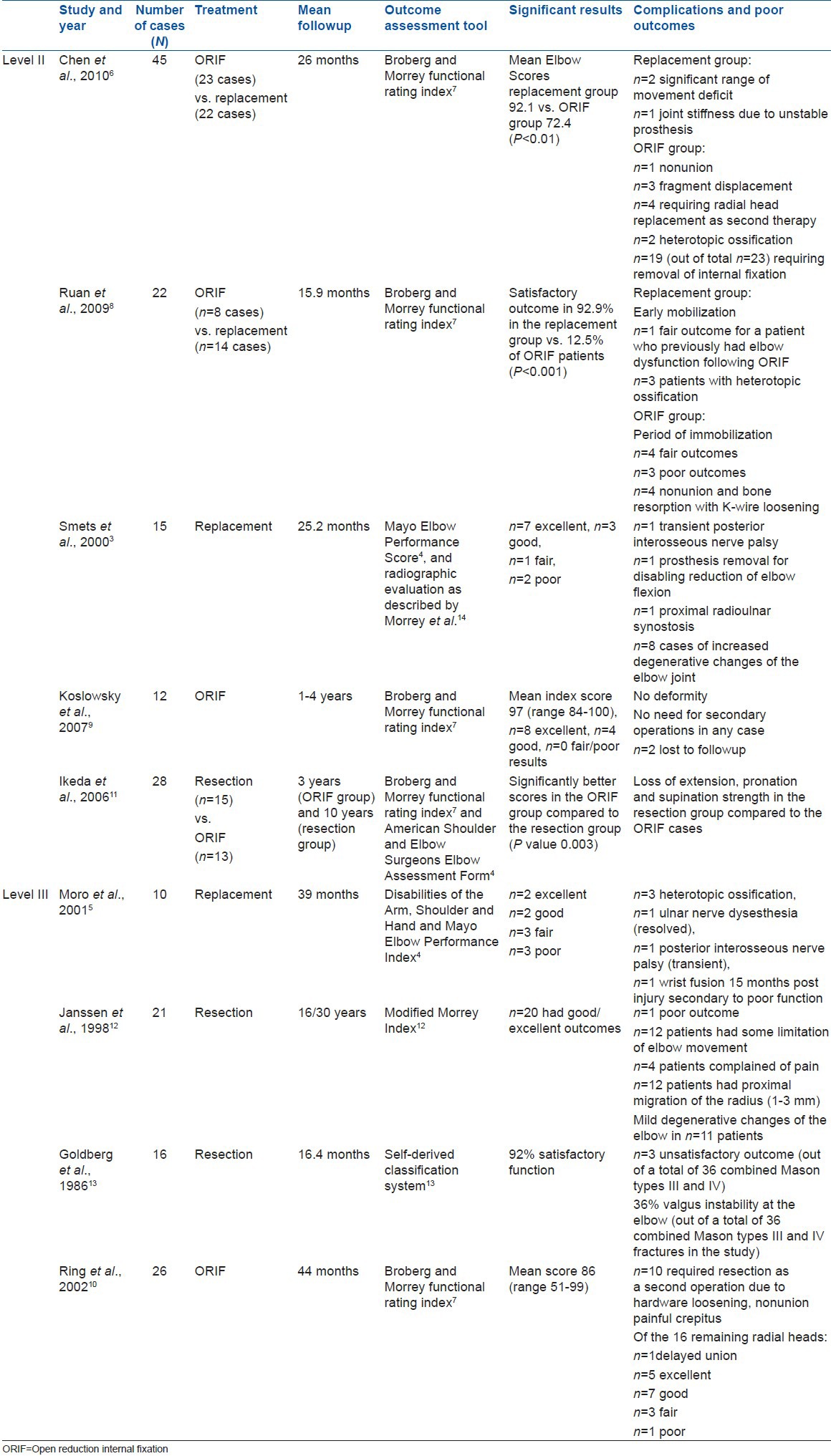
A summary of the findings reported in each article (levels 1-3 only) is given in Table 2.
Table 2.
Summary of findings for each study
Level IV evidence
Several articles provided long term data regarding patients’ functional outcomes after surgical management of Mason type III radial head fractures.
Radial head resection
Five articles presented their results following radial head resection. Iftimie et al.15 reported their results on 16 patients with Mason type III fractures who underwent radial head resection after a mean followup of 17 years. The average age of patients was 37 years (range 18-61 years). The authors concluded that radial head resection provides a satisfactory preservation of functional range at the elbow. The mean DASH score was 4.49 and the mean MEPI was 96.8, which were similar to the outcomes of patients undergoing the same treatment for Mason type II fractures. All patients continued with their previous activities. Fifty six percent of the patients had moderate to severe elbow degenerative changes. However, the degree of radiographic elbow degeneration showed no correlation with the functional outcome.
Antuña et al.16 presented a retrospective study with a mean followup of 25 years (minimum 15 years) of 26 patients who were treated with radial head resection for Mason type III fractures in a group of young manual workers. The average age was 29 years (range 15-39 years). They assessed elbow function according to the MEPI and DASH scales. The authors reported a satisfactory functional outcome in 90% of these patients. Two of the twenty six patients had moderate elbow pain and evidence of instability at the time of last followup. These two patients were not satisfied with the outcome and reported a DASH score of 28 and 38, respectively. The authors attributed these poor outcomes to iatrogenic injury to the lateral collateral ligament or a non-recognized associated ligamentous injury at the time of the procedure. All other patients in this study reported a satisfactory outcome.
Leppilahti et al.17 evaluated the outcomes of 17 patients with Mason type III fractures with a mean age of 42 years (range 13-77 years) who underwent early radial head resection. This article also included 6 patients with Mason type II fractures who underwent radial head resection, making a total of 23 patients. The mean delay until surgery was 9 days. The mean followup was 5 years. Range of motion averages were 135° flexion, 21° fixed flexion, 77° pronation and 75° supination. Mean strengths of hand grip and elbow flexion were significantly lower compared to the uninjured arm, whilst the other seven movements were not significantly altered.
Herbetsson et al.18 published their evaluation on the long term results of 24 patients with a Mason type III radial head fracture who underwent a delayed excision of the radial head. Average age was 47 years (range 18-73 years). Of the 24 patients, 9 had ongoing occasional but not daily pain and 1 had daily pain. Range of motion and functional scores were not separately reported for Mason type III fractures, but the measurements for Mason types II and III were combined to give an overall data. These measurements reported an elbow flexion deficit of 2°, extension deficit of 3° and reduced supination of 3°, compared to the uninjured arm. Nine patients of the 100 overall patients (including Mason types II and III) included in this study needed a secondary excision for ongoing pain following the initial operation. The authors concluded that delayed excision is comparable to acute excision in successfully preserving elbow function.
Broberg and Morrey7 reported the outcomes of 17 patients with Mason type III fractures who underwent delayed radial head excision. The average age was 32 years (range 10-60 years). The average followup was 15 years. They reported that 90% of patients were subjectively satisfied with the functional outcome; however, objectively, only 77% had excellent or good outcomes. Mean postoperative range of motion was not reported for the Mason type III fractures, but was reported for the overall data including Mason type II fractures. The authors concluded that delayed excision could be considered a viable option for patients with a fracture of the radial head in whom nonoperative management fails. Whether this can be considered an alternative to failed surgical management such as ORIF or replacement is an interesting question without documented supporting evidence.
Faldini et al.19 retrospectively evaluated 32 Mason type III radial head fractures that underwent resection of the radial head. Average patient age at the time of injury was 34 years (range 18-64 years). Average followup was 18 years (range 10-25 years). Patient function and satisfaction was measured using the Broberg and Morrey Index,7 the DASH questionnaire,4 and the visual analogue scale (VAS) for pain. The results were reported with 10 Mason type II radial head fractures, equating to a total of 42 cases. Mean Broberg and Morrey score was 91.2 (range 78-100) and mean DASH score was 10.1 (range 0-40). No intraoperative or short term postoperative complications occurred. All 42 patients were satisfied with their outcome. Thirty six patients stated they had no limitation and no pain and only six reported they had a mild limitation and mild pain. Mild loss of grip strength (less than 20% reduction compared to the uninjured side) was reported in seven cases. Eleven patients were noted to have a mild valgus deformity, 8 to have mild instability (5 of which were not perceived by the patients) and 28 cases were shown to have almost complete range of motion (less than 10° reduction in the range of motion). Radiographic followup found only eight of these patients had a positive ulnar variance, which bore no correlation to lower functional scores.19 This article documents the success proven with radial head resection in the short and long term.
Open reduction internal fixation
Only one level IV article reporting the outcomes of ORIF is included in this review. Pelto et al.20 reported their results from fixation of 19 Mason type III fractures with absorbable pins (Biofix, Bioscience Ltd, Tampere, Finland). The average age was 33 years (range 13-64 years). The average followup period for these patients was 27 months (range 10-44 months). Nine of these 19 patients had full range of motion. Seven had restriction of extension by an average 7°. One patient had limited pronation by 10°. Three patients had reduced supination at an average of 13°. Two patients reported activity-based mild pain and one patient complained of moderate pain during heavy labor. One patient underwent radial head resection at 6 months after fixation due to poor range of motions and functional scores. The results following this patient's secondary resection were not reported.
Radial head replacement
Two case series provide the results of radial head replacements following Mason type III fractures. Between January 1994 and September 1996, Popovic et al.21 evaluated the elbow function and complication rates following 11 Mason type III fractures treated with radial head replacement using the bipolar prosthesis (Tornier SA Inc., Saint-Ismier, France). Average age of the patients was 52 years (range 22-68 years). Based on a modified Morrey Scoring System, four had an excellent outcome, four were good, two were fair and one had a poor outcome at a mean followup of 32 months (range 24-56 months). Reported average motion deficits were 10° of lost flexion, 13.7° of lost pronation and 16.1° loss of supination, compared to the uninjured arm. Five of the 11 cases reported mild elbow pain with heavy activity and two reported moderate pain with daily activities. The one poor result was reported in a patient who had sustained other multiple injuries to the affected upper limb. The patient had significantly reduced mobility at the elbow and forearm rotation with associated moderate pain with daily activities.
Ashwood et al.22 published the outcomes of 16 patients with Mason type III fractures treated with atitanium radial head prosthesis (Wright Medical Technology, Arlington, TN, USA) over a 5-year period. Average age was 45 years (range 21-72 years). Six of these patients had a delayed replacement with an average of 37 days after injury. All patients were followed up for a mean of 2.8 years clinically and radiographically. Eight patients had excellent outcomes, five were good, three were fair and no cases had a poor outcome. All three fair results occurred in patients who had delayed surgery. The authors concluded that this method of treatment for Mason type III fractures was satisfactory and noted that early mobilization is important for preserving the elbow range of movement and function.
DISCUSSION
Mason Type III radial head fractures have been treated with radial head resection, ORIF and more recently with radial head replacement, with no clear advantage of one over the other. We attempted to isolate which of the three modalities would provide patients with the best functional outcome with the lowest complication rates.
The literature provides limited comparative information regarding each treatment modality. Due to the difficulty of conducting randomized controlled trials and the relatively small number of Mason type III fractures seen even in large centers, there is little statistical power to any of the studies included.
Throughout the literature there is evidence that all three modalities provide satisfactory outcomes. Many of these studies are single-arm studies looking at the functional outcome of resection, replacement, or ORIF alone. The long term success of radial head resection has been shown in some long term studies. However, while some recent articles outline the short term success using radial head replacement, long term data on the outcome of ORIF or radial head replacement in the current literature is limited. Thus, radial head resection has an advantage over the other of proven longevity.
There are very few comparative studies. The sole comparative study between radial head resection and ORIF by Ikeda et al. shows that ORIF had better outcomes than resection, although systematic internal fixation removal was not considered a complication.11 This was a study with a small sample size and is yet to be supported by further studies comparing these treatment modalities.
Two randomized studies by Chen et al.6 and Ruan et al.8 attempt to provide evidence comparing ORIF and radial head replacement. Both of these studies provide data to suggest that radial head replacement provides a better functional outcome with few complications. However, the rehabilitation protocols were vastly different between the two treatment groups and this could account for the different clinical outcomes. The significance of the findings in these studies is therefore difficult to conclude upon due to this confounding factor. The optimal management of elbow injuries involves early motion following anatomical reduction and stabilization.23–25 Articles have outlined the benefits of static progressive or dynamic splinting as an additional option after injury to ensure mobilization while reinforcing stability.24,25 The outcomes of these articles, therefore, cannot be attributed to the treatment modality alone, but may be due to the key rehabilitation factor of early mobilization after elbow surgery.
Significant concomitant injuries and mechanical faults following surgical management also influence the outcome following Mason type III fractures. Particular concomitant injuries such as capitellar chondral damage, collateral ligament injury and Essex-Lopresti lesions negatively affect the outcome following treatment.22,26,27,28 Postoperative mechanical factors such as proximal radial migration, suboptimal anatomical reduction and valgus instability correlate to poorer outcomes.26,28,29
Capitellar chondral damage is common with high grade radial head fractures. The reported incidence of capitellar chondral injury is as high as 20% in Mason types II and III according to one study.30 There are few articles with long term outcomes following capitellar cartilage injury. Further investigation would provide surgeons with information regarding prognosis from such injuries.
The Essex-Lopresti lesion is an axial instability of the forearm due to the distal radioulnar joint (DRUJ) dislocation with rupture of the interosseous ligament in association with a radial head fracture.26,31 The diagnosis of this instability may be subtle and delayed. The correct diagnosis is reported to be made in as low as 38% of acute cases.26 It is an important diagnosis in the setting of radial head fracture and should be considered with any radial head fracture caused by axial force. Thorough clinical, radiologic and intraoperative examination of the elbow and wrist is required to ensure the patient receives the optimal surgical management.32 The important step of intraoperative interosseous membrane (IOM) assessment should be diligently practiced to minimize complications.
Radial head resection has a poor outcome with this injury as radial migration is common. The proportion of radiographically confirmed migration is reported to be 50-80% following radial head resection and symptoms are reported in as high as 25% of patients.33,34 Despite varied proportions reported in the literature, this phenomenon is a well described complication following radial head resection. Proximal radial migration produces DRUJ subluxation and can cause a poor long term outcome due to elbow and wrist symptoms.12,31,34,35,36 Radial head replacement or radial head ORIF and immobilization of the DRUJ should be considered rather than resection in this instance. Many authors have suggested that ORIF or radial head replacement should be used when possible to restore normal anatomy and avoid DRUJ dysfunction.22,26,35,37 Some have advocated the use of K-wires to immobilize the forearm to assist DRUJ and IOM repair.26 The intrinsic capacity of the IOM to heal could be minimal according to some authors.27 Long term sequelae of mistreated or undiagnosed Essex-Lopresti lesions can include DRUJ dysfunction, ulnar-positive variance, wrist pain and forearm weakness. There is commonly a need for secondary surgical management following this type of injury.26,31,35,36 One study38 shows delayed and primary radial head resection provides the same long term functional outcome; however, a further operation was much more common in patients who underwent primary surgery compared to those which were delayed.38 Therefore, if this type of injury is diagnosed or suspected, we recommend radial head replacement or ORIF to be undertaken. However, if resection is seen as a necessary surgical procedure, then restoring forearm stability (either by intrinsic healing with immobilization or by reconstruction) prior to resection is crucial to a satisfactory outcome.
A major complication following elbow fractures and surgical procedures at the elbow joint is stiffness. Early mobilization is essential in the prevention of long term elbow stiffness. To allow early mobilization following surgical procedure, the presence of an intact medial collateral ligament is vital.22 Medial collateral ligament rupture or damage can lead to ongoing valgus instability at the elbow. Repair of the medial collateral ligament should be considered if it improves stability and allows safe early mobilization postoperatively.12,22,37 Radiocapitellar contact is as important for the elbow stability as the surrounding ligaments. In the scenario of an unstable elbow, restoring this contact improves this stability. Radial head resection would not be suitable in this instance.
The achievement of optimal anatomical reduction by ORIF may also contribute to long term outcomes, although it is difficult to perform in these types of fractures. No studies target the level of optimal anatomical reduction achieved and its effect on long term outcomes. A poor reduction with a large articular step or gap may influence the long term function at the elbow due to accelerated arthritis. Future studies would give surgeons more accurate criteria for satisfactory ORIF and when to accept converting an ORIF to another modality such as resection or replacement.
CONCLUSION
Given the small number of quality trials on the treatment of Mason type III fractures, we cannot recommend one treatment modality over any other. All three treatment modalities discussed provide satisfactory outcomes for patients in the majority of cases at short term followup. Radial head resection is just as successful after a delayed period as it is in the acute setting; therefore, we recommend using either radial head replacement or ORIF in the acute setting, specifically in an unstable elbow. Radial head resection would be an option if the outcome of an acute operation was not satisfactory, but only following restoration of forearm stability. Given the complexity of Mason type III radial head fractures, concomitant injuries and prognostic factors, we cannot generalize that all Mason type III radial head fractures are the same and should receive the same treatment. The long term outcomes following Mason type III radial head fractures depend on multiple variables, not solely the treatment method.
The difficulty to undertake randomized controlled trials due to the small numbers of Mason type III fractures is one obstacle limiting data regarding this topic. Of these fractures seen even in large centers, a multicenter trial would provide the benefit of increased case numbers for analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Mason ML. Some observations on fracture of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–32. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 2.Group. OLoEW. The Oxford 2011 Levels of Evidence. [Last cited in 2011]. Available from: http://www.cebm.net/index/aspx?o=5653 .
- 3.Smets S, Govaers K, Jansen N, Van Riet R, Schaap M, Van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: A multicentric study. Acta Orthop Belg. 2000;66:353–8. [PubMed] [Google Scholar]
- 4.Longo UG, Franceschi F, Loppini M, Maffulli N, Denaro V. Rating systems for evaluation of the elbow. Br Med Bull. 2008;87:131–61. doi: 10.1093/bmb/ldn023. [DOI] [PubMed] [Google Scholar]
- 5.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–11. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Chen XW, Cao LH, Yang GQ, Li M, Su JC. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop. 2011;35:1071–6. doi: 10.1007/s00264-010-1107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–74. [PubMed] [Google Scholar]
- 8.Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type III. Int Orthop. 2009;33:249–53. doi: 10.1007/s00264-007-0453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koslowsky TC, Mader K, Gausepohl T. Pennig D Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device: 23 patients followed 1-4 years. Acta Orthop. 2007;78:151–6. doi: 10.1080/17453670610013565. [DOI] [PubMed] [Google Scholar]
- 10.Ring D, Quintero JJ. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811–5. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda M, Sugiyama K, Kang C, Takagaki T, Oka Y. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 1):11–23. doi: 10.2106/JBJS.E.00841. [DOI] [PubMed] [Google Scholar]
- 12.Janssen RP, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: Followup at 16 to 30 years. J Bone Joint Surg Br. 1998;80:231–3. doi: 10.1302/0301-620x.80b2.8255. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg I, Peylan J, Yosipovitch Z. Late results of excision of the radial head for an isolated closed fracture. J Bone Joint Surg Am. 1986;68:675–9. [PubMed] [Google Scholar]
- 14.Morrey BF. An KN Biomechanics of the elbow. In: Morrey BF, editor. The elbow and its disorders. Philadelphia: WB Saunders; 1985. pp. 43–61. [Google Scholar]
- 15.Iftimie PP, Calmet Garcia J, de Loyola Garcia Forcada I, Gonzalez Pedrouzo JE, Gine Goma J. Resection arthroplasty for radial head fractures: Long term followup. J Shoulder Elbow Surg. 2011;20:45–50. doi: 10.1016/j.jse.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Anturia SA, Sanchez-Marquez JM. Long term results of radial head resection following isolated radial head fractures in patients younger than forty years old. J Bone Joint Surg Am. 2010;92:558–66. doi: 10.2106/JBJS.I.00332. [DOI] [PubMed] [Google Scholar]
- 17.Leppilahti J, Jalovaara P. Early excision of the radial head for fracture. Int Orthop. 2000;24:160–2. doi: 10.1007/s002640000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herbertsson P, Josefsson PO, Hasserius R, Karlsson C, Besjakov J, Karlsson M. Uncomplicated Mason type-II and III fractures of the radial head and neck in adults. A long term followup study. J Bone Joint Surg Am. 2004;86:569–74. doi: 10.2106/00004623-200403000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Faldini M, Nanni M, Leonetti D, Capra P, Bonomo M, Persiani V, et al. Early radial head excision for displaced and comminuted radial head fractures: Considerations and concerns at long term followup. J Orthop Trauma. 2012;26:236–40. doi: 10.1097/BOT.0b013e318220af4f. [DOI] [PubMed] [Google Scholar]
- 20.Pelto K, Hirvensalo E, Bostman O, Rokkanen P. Treatment of radial head fractures with absorbable polyglycolide pins: A study on the security of the fixation in 38 cases. J Orthop Trauma. 1994;8:94–8. doi: 10.1097/00005131-199404000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Popovic N, Gillet P, Rodriquez A, Lemaire R. Fracture of the radial head with associated elbow dislocation: Results of treatment using a floating radial head prosthesis. J Orthop Trauma. 2000;14:171–7. doi: 10.1097/00005131-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Ashwood N, Bain GI, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair and early mobilization. J Bone Joint Surg Am. 2004;86:274–80. doi: 10.2106/00004623-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Maripuri SN, Debnath UK, Rao P, Mohanty K. Simple elbow dislocation among adults: A comparative study of two different methods of treatment. Injury. 2007;38:1254–8. doi: 10.1016/j.injury.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 24.Isaack PS, Egol KA. Posttraumatic contracture of the elbow. Bull Hosp Jt Dis. 2006;63:129–36. [PubMed] [Google Scholar]
- 25.Nandi S, Maschke S, Evans PJ, Lawton JN. The Stiff Elbow. Hand. 2009;4:368–79. doi: 10.1007/s11552-009-9181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams JE, Steinmann SP, Osterman AL. Management of injuries to the Interosseous Membrane. Hand Clin. 2010;26:543–8. doi: 10.1016/j.hcl.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Ruch DS, Chang DS, Koman LA. Reconstruction of longitudinal stability of the forearm after disruption of the interosseus ligament and radial head excision (Essex-Lopresti lesion) J South Orthop Assoc. 1999;8:47–52. [PubMed] [Google Scholar]
- 28.Morrey BF, Chao EY, Hui FC. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am. 1979;61:63–8. [PubMed] [Google Scholar]
- 29.Duckworth AD, Watson BS, Will EM, Petrisor BA, Walmsley PJ, Court-Brown CM, et al. Radial head and neck fractures: Functional results and predictors of outcome. J Trauma. 2011;71:643–8. doi: 10.1097/TA.0b013e3181f8fa5f. [DOI] [PubMed] [Google Scholar]
- 30.Nalbantoglu U, Gereli A, Kocaoglu B, Aktas S, Turkmen M. Capitellar cartilage injuries concomitant with radial head fractures. J Hand Surg Am. 208;3:1602–7. doi: 10.1016/j.jhsa.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 31.Duckworth AD, Clement ND, Aitken SA, Ring D, McQueen MM. Essex-Lopresti lesion associated with an impacted radial neck fracture: Interest of ulnar shortening in the secondary management of sequelae. J Shoulder Elbow Surg. 2011;20:e19–24. doi: 10.1016/j.jse.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 32.Bain GI, Ashwood N, Baird RU. Management of mason type-III radial head fractures with a titanium prosthesis, ligament repair and early mobilization. surgical technique. J Bone Joint Surg Am. 2005;87(Suppl 1Pt 1):136–47. doi: 10.2106/JBJS.D.02710. [DOI] [PubMed] [Google Scholar]
- 33.Postacchini F, Morace GB. Radial head fracture treated by resection. Long term results. Ital J Orthop Traumatol. 1992;18:323–30. [PubMed] [Google Scholar]
- 34.Mikic ZD, Vukadinovic SM. Late results in fractures of the radial head treated by excision. Clin Orthop Relat Res. 1983;181:220–8. [PubMed] [Google Scholar]
- 35.Geel CW, Palmer AK. Radial head fractures and their effect on the distal radioulnar joint. A rationale for treatment. Clin Orthop Relat Res. 1992;275:79–84. [PubMed] [Google Scholar]
- 36.Jungbluth P, Frangen TM, Muhr G, Kalicke T. A primarily overlooked and incorrectly treated Essex-Lopresti injury: What can this lead to? Arch Orthop Trauma Surg. 2008;128:89–95. doi: 10.1007/s00402-007-0431-7. [DOI] [PubMed] [Google Scholar]
- 37.Cooney WP. Radial head fractures and the role of radial head prosthetic replacement: Current update. Am J Orthop. 2008;37(8 suppl):21–5. [PubMed] [Google Scholar]
- 38.Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Nyqvist F, Karlsson MK. Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am. 2004;86:1925–30. doi: 10.2106/00004623-200409000-00010. [DOI] [PubMed] [Google Scholar]


