Abstract
Background:
Surgical treatment of adult lumbar spinal disorders is associated with a substantial risk of intraoperative and perioperative complications. There is no clearly defined medical literature on complication in lumbar spine surgery. Purpose of the study is to retrospectively evaluate intraoperative and perioperative complications who underwent various lumbar surgical procedures and to study the possible predisposing role of advanced age in increasing this rate.
Materials and Methods:
From 2007 to 2011 the number and type of complications were recorded and both univariate, (considering the patients’ age) and a multivariate statistical analysis was conducted in order to establish a possible predisposing role. 133 were lumbar disc hernia treated with microdiscetomy, 88 were lumbar stenosis, treated in 36 cases with only decompression, 52 with decompression and instrumentation with a maximum of 2 levels. 26 patients showed a lumbar fracture treated with percutaneous or open screw fixation. 12 showed a scoliotic or kyphotic deformity treated with decompression, fusion and osteotomies with a maximum of 7.3 levels of fusion (range 5-14). 70 were spondylolisthesis treated with 1 or more level of fusion. In 34 cases a fusion till S1 was performed.
Results:
Of the 338 patients who underwent surgery, 55 showed one or more complications. Type of surgical treatment (P = 0.004), open surgical approach (open P = 0.001) and operative time (P = 0.001) increased the relative risk (RR) of complication occurrence of 2.3, 3.8 and 5.1 respectively. Major complications are more often seen in complex surgical treatment for severe deformities, in revision surgery and in anterior approaches with an occurrence of 58.3%. Age greater than 65 years, despite an increased RR of perioperative complications (1.5), does not represent a predisposing risk factor to complications (P = 0.006).
Conclusion:
Surgical decision-making and exclusion of patients is not justified only by due to age. A systematic preoperative evaluation should always be performed in order to stratify risks and to guide decision-making for obtaining the best possible clinical results at lower risk, even for elderly patients.
Keywords: Lumbar spine surgery, peroperative/intraoperative complications, revision spinal surgery
INTRODUCTION
Surgical treatment of adult lumbar spinal disorders is associated with a substantial risk of intraoperative and perioperative complications.1 The improvement in perioperative management and the development of new techniques in anesthetics and surgical sciences have led to substantial reduction of complications related to lumbar spine surgery. An understanding of these complications is important and valuable for both the patient and the surgeon. Nevertheless, complications represent undesirable consequences of lumbar spine surgery in adult patients. Patients’ age, medical comorbidities and fusion extending up to the sacrum are identified as predisposing risk factors.1,2,3,4,5,6 The development of new guidelines in perioperative nutrition, pulmonary management and intraoperative neuromonitoring have been considered important measures in decreasing the complication rate.7,8 Surgical complications may be divided into major and minor categories. Major complications are those which require return to the operating room, prolonged inpatient or outpatient care or irreversible pathology directly related to surgery (neural injury, pulmonary emboli and symptomatic nonunion). Minor complications on other hand do not require prolonged inpatient or outpatient care (for example a dural tear, transient radiculopathy).9 It is important to recognize that perioperative complications are not a significant predictor of long term clinical outcome. Unintended durotomy, wound infection and thromboembolism were identified as common complications associated with spine surgery. Variety of risk factors for these complications have been identified by many authors. Patient's age, obesity, diabetes, urinary incontinence, tobacco intake, poor nutritional status, complete neurologic deficit, revision surgery, use of nonsteroidal antinflammatory drugs (NSAIDs), posterior surgical approach, increased estimated blood loss, need for blood transfusion, prolonged surgical time, multilevel surgery, fusion extended to the sacrum and use of spinal instrumentation have all been correlated to an increased risk of complications in adult spinal surgery.10,11 The purpose of this study is to evaluate intraoperative and perioperative complication rates in a retrospective series of 338 patients who underwent lumbar surgical procedures and to evaluate advanced age (more than 65 years) and its correlation with occurrence of complications in lumbar spinal surgery.
MATERIALS AND METHODS
338 patients who underwent lumbar surgical procedures at our university hospital were evaluated in a retrospective study between 2007 and 2011. There were 145 females and 193 males with a mean age of 68.4 years (range 53-85 years). The incidence of complications was evaluated for the following surgical procedures: microdiscetomy, decompression in lumbar stenosis (with or without instrumentation), treatment for traumatic pathology, spondylolisthesis and correction of kyphotic and scoliotic deformities. All cases were classified depending on age, intensive care unit stay, fusion, fusion extended to sacral 1, open versus minimally invasive approach and surgical time. The type of surgical approach was considered; registering the complication incidence in the posterior, anterior and combined approach. The registered complications were divided into minor and major complications and intra and perioperative complications. Ictus cerebri, vascular lesions, deep venous thrombosis and pulmonary embolism were considered as major complications. Screw misplacement (type 3 according to Youkilis criteria),12 unintended durotomy, local infection, urinary infection and postoperative anemia were considered as minor complications. Intraoperative complications were considered as those occurring during the surgical procedure. Perioperative complications were those which occurred within 48 hours following the main surgical procedure. For every surgical procedure, the number and type of complications were recorded and were correlated to each factor in order to establish a possible statistically significance in a multivariate analysis. A correlation was made in the same group of diseases, between the presence and the absence of fusion and between the minimally invasive and open surgery. Patients were stratified in three groups considering age: group 1 had patients between 20 and 44 years, group 2 had patients between 45 and 64 years and group 3 had patients between 65 and 85 years. All variables were then correlated to the patients’ age, in order to establish a head role of this factor in increasing the relative risk (RR) for complications.
Statistics
Statistical analysis was performed using SPSS software version 16.0 (SPSS Inc.). The results obtained were analyzed using the student's t-test and χ2 test; and verified with Fisher's exact test. Significance was accepted at P < 0.05.
RESULTS
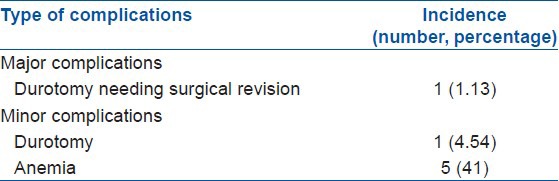
133 were microdiscectomies for lumbar disc herniation, 88 were lumbar stenosis, (36 cases were treated only with decompression and 52 with decompression and instrumentation with a maximum of two levels) lumbar fracture in 26 patients treated with percutaneous or open screw fixation. Scoliotic or kyphotic deformity in 12 patients treated with decompression, fusion and osteotomies with a maximum of 7.3 levels of fusion (range 5-14) in 70 cases, spondylolisthesis (treated with one or more level of fusion), in 34 cases a fusion till S1 was performed. A total of 60 (17.75%) complications in 55 patients were registered: 9 (2.6%) were classified as major complications and 51 (15%) as minor complications. 17 (35.3%) were intraoperative complications while 43 (64.7%) were perioperative complications. The surgical complications are summarized in Table 1. A complication rate of 4.5% (6 complications) with only one major complication was seen in the microdiscectomy group [Table 2], a rate of 14.77% (13 complications) was registered in the lumbar stenosis group with a higher incidence of major complication in the fusion group [Table 3]. A rate of 11.53% (three minor complications) was registered in the traumatic group [Table 4]. A complication rate of 25.7% (18 complications) was seen in the spondylolisthesis group with seven major complications using pedicle screw fixation and posterior interbody fusion with cage [Table 5]. A higher rate of complication (58.3%) was noted in the deformity correction group [Table 6]. There were five minor and one major complication in this group. In combined anterior and posterior approaches we registered a higher incidence of complications with one iliac vein lesion, one deep vein thrombosis with a consequent pulmonary embolism in the same patient and two case with postoperative hemorrhagic anemia with an haemoglobin level <7. A combined anterior and posterior approach increases the RR of complications in our series till 2.6 when compared to single anterior or posterior approach.
Table 1.
Intraoperative and perioperative major and minor complications in all 338 patients
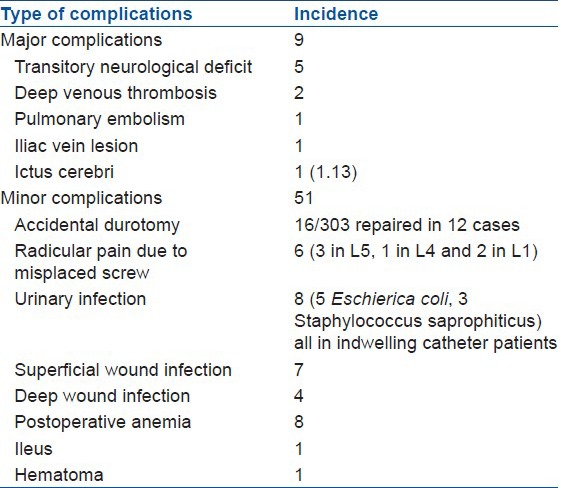
Table 2.
Incidence and type of complications in the microdiscectomy group (n=133)
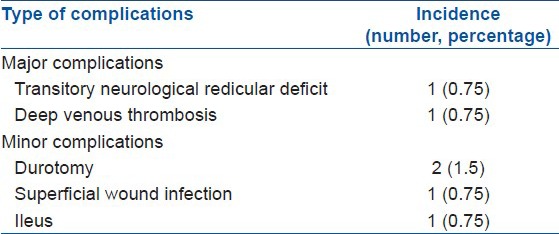
Table 3.
Complications in lumbar stenosis group treated with decompression with or without fusion (n=88)
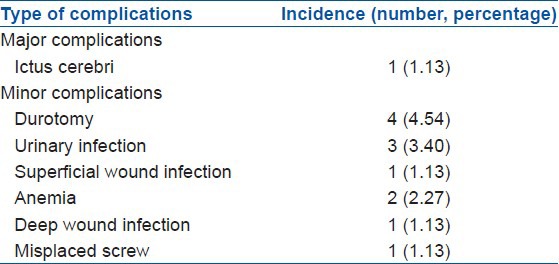
Table 4.
Complications in the lumbar fracture group (n=26)
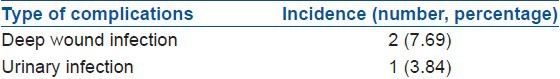
Table 5.
Complications in for the spondylolisthesis group (n=70)
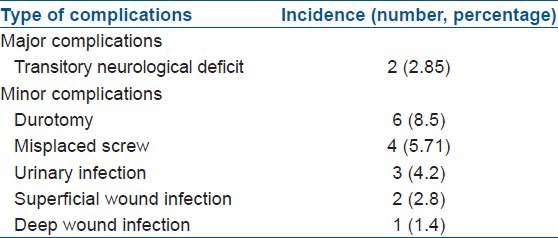
Table 6.
Complications in the kyphotic or scoliotic deformity correction group (n=12)
We noted that the type of surgical treatment, that is instrumentation use versus non-instrumentation use increases the RR of complication of 2.8. Instrumentation longer than three levels increases the RR of 2.5 and arthrodesis of 3.1. also the type of surgical approach (open) increases the RR of 4.1 and surgical time of 4.5 [Table 7]. The presence of instrumentation showed an increase in the infection risk compared to non-instrumental procedure of 5.6 (5.9 versus 1.07%, P = 0.005). The use of an open approach with respect to minimally invasive surgery (MIS) appears to be a predisposing factor in developing deep or superficial infections (4.47 versus 1.45%, RR 4.3), also surgical time longer than 4 hours is an important risk factor for deep site infections (RR 4.5). Intensive care unit stay showed no statistically significant role in development of superficial and deep wound infections (1.3 versus 1.8%). An age over 65 years, despite an increased RR of perioperative complications 1.5, does not represent to be a predisposing factor to complications, P = 0.006 as shown in Figure 1.
Table 7.
Complications based on different predisposing factors
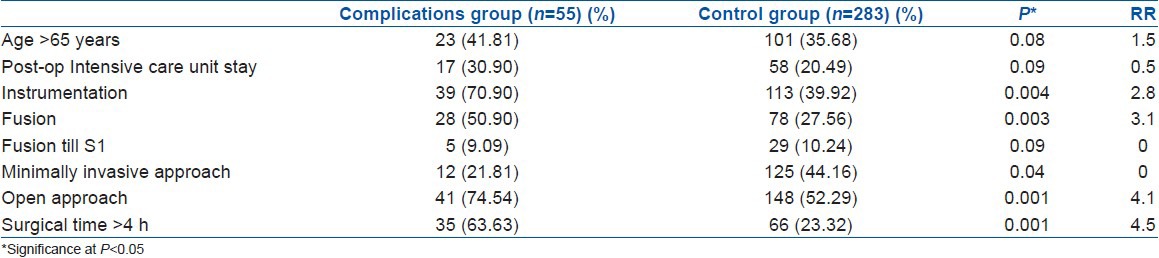
Figure 1.
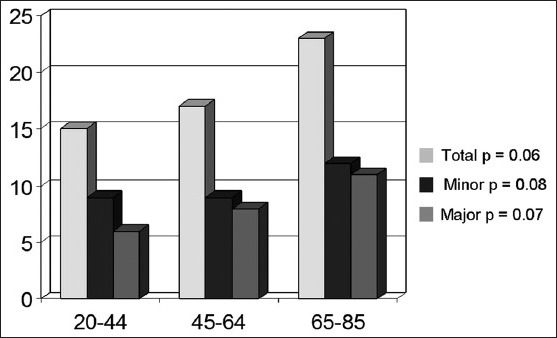
Histogram showing the relationship between age and incidence of total, major and minor complications
DISCUSSION
Complications and adverse events are an inevitable risk of surgical procedures. Different studies in literature have examined the predisposing factors for development of complications.11,13 The goal to ameliorate spinal surgical procedures is to identify the main predisposing factors and the strategies which may mitigate the risk of complications. Patients’ age and comorbidities have a clear impact on the incidence of perioperative complications in spine surgery.14 The role of patients’ age as predisposing risk factor for complications in spine surgery is a largely debated issue in literature. Several authors have underlined an age-related increase of surgical and general complications.9,15,16 Others, such as Silver et al.,17 or recently Ragab et al.,18 and Okuda et al.,19 found no age-related differences in outcome. An advanced age is not associated with higher morbidity and mortality and complications rates are comparable between patients younger and older than 65 years. Our findings are comparable with these results. In our series an age over 65 years is not a predisposing factor in developing intra and perioperative complications, despite an increased RR of 1.5 times in developing general complications in patients over the age of 75 years with more than four comorbidities. A specific preoperative evaluation in order to analyze cardiac, pulmonary, hematologic, mental status, nutrition status, bone density, alcohol and tobacco use, preoperative medication, social environment and home resources acquires a fundamental role in our series. This evaluation should be performed by a multidisciplinary team with familiarity to the type of spine surgery that is being pursued. Specifically a systematic approach to preoperative evaluation that includes cardiac and pulmonary function and an assessment of fitness of the patient for surgery that encompasses evaluation by the anesthesia team and a primary care physician is important to identify risk factors for perioperative complication. The magnitude of surgery planned is an important consideration in preoperative risk assessment and an accurate estimation of length of surgery, estimated blood loss and pulmonary or abdominal exposures during surgery will be useful for anesthesiologists and primary care doctors in their preoperative evaluations. The choice of surgical approach, fusion levels and operative versus nonoperative care may be influenced by knowledge of potential complications and adverse outcomes. Even with complete preoperative preparation, perioperative complications cannot be prevented entirely. In this general evaluation, age itself is not a complete contraindication for spinal surgery however it may influence the surgical planning, especially for complex spinal procedures. Patients over the age of 69 years, as shown by Daub et al.,16 are nine times more likely to have a major complication, when a complex spinal procedure is performed. In our series, patients over the age of 65 years did not show a greater incidence of complications compared to younger patients because our elderly patients underwent generally minor surgical procedures such as laminectomy alone or short posterior rigid fixation/fusion (one or two instrumented levels).
According to previous studies20,21 we identify a major incidence of complications (58.3%) in posterior fusion, instrumentation and osteotomies performed in the surgical treatment of adult scoliotic or kyphotic deformities. All the adverse events which occured in this cohort of patients represent important complications with a particular incidence of postoperative anemia (41%), secondary to the usual intraoperative excessive blood loss registered in these procedures.20 Preoperative sagittal imbalance is an adjunctive risk factor for perioperative complications as shown by Schwabb et al.22 The major rate of complications in these patients has to be related to the surgical technique that requires long segment instrumentation and pedicle subtraction osteotomies. In our study; the use of instrumentation, presence of fusion, long surgical time and open surgical approach have demonstrated a statistically significant predisposing role in developing a complication in all the surgical procedures. A long surgical time (>4 h) and the use of conventional open surgery have demonstrated a consistent risk factor in developing superficial and deep wound infections.14,23 In our cohort, the rate of wound infection was significantly lower for cases treated using a minimally invasive approach as compared with those using more traditional open approach. An open approach compared to MIS increases 4.3 times the risk of developing deep or superficial infections. Our results demonstrated an incidence of 4.47% in the open procedures as compared to only a 1.45% in the MIS approach. It is important to recognize that this data does not necessarily suggest a causation link between infection and traditional open surgery, but rather reflects greater complexity and a consequent major associated risk for cases that require open approaches. An increase in the infection index was registered in our series with a surgical time longer than 3.30 hours. A surgical time longer than 4 hours increases 4.5 times the risk of developing a deep or superficial infection. Postoperative wound infections remain a relatively common source of morbidity and increased costs.24 It has been estimated that spine surgical infection (SSI) can increase health care costs up to four-fold.25 A study of the Scoliosis Research Society Morbidity and Mortality Committee based on 108,419 procedures reports an overall total infection rate of 2.1% (superficial = 0.8%, deep = 1.3%). The rate of infection in adult patients with a primary diagnosis of degenerative disease varied based on spinal location, with the highest rate for thoracic procedures (2.1%), followed by lumbar (1.6%) and cervical (0.8%) procedures. In our cohort we observed a total infection rate of 2.3%. Postlaminectomy kyphosis was associated with the highest rate of infection amongst the adults (5.1%). In addition, the overall infection rate for cases with implants was 28% higher than the rate for cases without implants. Revision cases had a 65% higher overall rate of infection when compared with primary cases.12 This data also confirmed that in our series implant use increases 1.9 times the risk of infection independently from the surgical technique. Administration of intravenous antibiotics is a well-established system to reduce infection rate but local delivery of antibiotics has become an attractive possibility of prophylaxis because high concentrations are achieved directly at these sites and systemic toxicity is limited.25
An incidence comparable to world literature was seen in our series for an unintended durotomy. We found a durotomy incidence comparable to those reported by Williams et al.,8 both in the lumbar disc herniation group (1.5 versus 1.6%), as in the lumbar stenosis group (4.5 versus 3.1%) and in the spondylolisthesis group (8.5 versus 6.5%). The mean age of patients with durotomy was 56 years which was significantly older than patients who did not have durotomy. The greater age of patients in lumbar stenosis group may be the cause of a major incidence of unintended durotomy associated to the presence of significant scar adhesions typical of degenerative process of the lumbar stenosis.26 Revision surgery was generally associated with a greater incidence of unintended durotomy when compared with primary surgery. In our series, all patients affected by spondylolisthesis were treated with posterior lumbar interbody fusion (PLIF) procedure. The cage insertion procedure may be responsible of a durotomy secondary to medial retraction of the dural sac.
In the spondylolisthesis group, a major incidence of transitory neurological deficit (2.85%) was seen as compared to the other groups. This complication was registered in L5-S1 spondylolisthesis and was consequent to the reduction technique. As shown by Petraco et al.,27 71% of the total L5 nerve strain occurring during the second half of reduction in spondylolisthesis. A reduction in neurological complications may be obtained with a constant use of intraoperative neuromonitoring especially in surgical procedures at high neurological risks like spondylolisthesis reduction or osteotomies in deformity surgery.28
Deep venous thrombosis (DVT) and pulmonary embolism (PE) are significant potential complications of spinal surgery.29 A limited number of reports have documented these events in relatively small populations of patients. As shown by Dearbone et al.,29 the true incidence of thromboembolic complications in spinal surgery remains unknown. Generally, the real incidence of this complication is underestimated because only symptomatic patients are considered in studies. A radiographic analysis with doppler or thoracic computed tomography (CT) scan, as shown in previous studies, could better estimate the real value of this complication even in asymptomatic patients.30 Smith et al.,30 reported significantly greater rates of PE and DVT for cases that included implants compared with cases not using implants and the rate of DVT for revision cases was greater than that of primary cases. In our series, the incidence of DVT and PE was greater in patients who underwent combined access. Low-dose heparin regimens reduce the frequency of DVT and PE in spinal surgery but pose some risk of postoperative hemorrhage threatening neurologic function. Therefore, in patients at higher risk because of coagulation disorders, a mechanical prophylaxis could also have an important role, demonstrating an efficacy comparable to the low-dose heparin regimens.31
Despite the small number of patients and the limitations of a retrospective analysis, our results suggest that several factors have to be considered in surgical planning in order to avoid complications. The surgical decision-making and exclusion of patients is not justified only due to age but a systematic preoperative clinical evaluation should be performed in order to stratify risks and to guide decision making for obtaining the best possible clinical results at lower risk.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976) 1995;20:1592–9. doi: 10.1097/00007632-199507150-00007. [DOI] [PubMed] [Google Scholar]
- 2.Macdonnell MF, Glassman SD, Dimar JR, 2nd, Puno RM, Johnson JR. Perioperative complications of anterior procedures of the spine. J Bone Joint Surg Am. 1996;78:839–47. doi: 10.2106/00004623-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Edwars CC, 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusion to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976) 2004;29:1996–2005. doi: 10.1097/01.brs.0000138272.54896.33. [DOI] [PubMed] [Google Scholar]
- 4.Urban MK, Jules-Elysee KM, Beckmann JB, Sivjee K, King T, Kelsey W, et al. Pulmonary injury in patients undergoing complex spine surgery. Spine J. 2005;5:269–76. doi: 10.1016/j.spinee.2004.10.049. [DOI] [PubMed] [Google Scholar]
- 5.Byron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine (Phila Pa 1976) 2006;31(19 Suppl):S106–18. doi: 10.1097/01.brs.0000232713.69342.df. [DOI] [PubMed] [Google Scholar]
- 6.Proietti L, Pola E, Nasto LA, Scaramuzzo L, Logroscino CA. Onset of a Charcot spinal arthropathy at a level lacking surgical arthrodesis in a paraplegic patient with traumatic cord injury. Eur Spine J. 2010;19(Suppl 2):S83–6. doi: 10.1007/s00586-009-1055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lapp MA, Bridwell KH, Lenke LG, Baldus C, Blanke K, Iffrig TM. Prospective randomization of clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2001;26:809–17. doi: 10.1097/00007632-200104010-00023. [DOI] [PubMed] [Google Scholar]
- 8.Williams BJ, Sansur CA, Smith JS, Berven SH, Broadstone PA, Choma TJ, et al. Incidence of unintended durotomy in spine surgery based on 108,478 cases. Neurosurgery. 2011;68:117–23. doi: 10.1227/NEU.0b013e3181fcf14e. [DOI] [PubMed] [Google Scholar]
- 9.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–92. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Clapham LM, Bukley J. Outcome-directed clinical practice in lumbar spine surgery. Clin Perfom Qual Health Care. 1999;7:167–71. doi: 10.1108/14664109910315587. [DOI] [PubMed] [Google Scholar]
- 11.Pull ter Gunne AF, Cohen DB. Incidence, prevalence and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 2009;34:1422–8. doi: 10.1097/BRS.0b013e3181a03013. [DOI] [PubMed] [Google Scholar]
- 12.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48:771–8. doi: 10.1097/00006123-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Browne JA, Cook C, Pietrobon R, Bethel MA, Richardson WJ. Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976) 2007;32:2214–9. doi: 10.1097/BRS.0b013e31814b1bc0. [DOI] [PubMed] [Google Scholar]
- 14.Klein JD, Garfin SR. Nutritional status in the patient with spinal infection. Orthop Clin North Am. 1996;27:33–6. [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine: The influence of age, diagnosis and procedure. J Bone Joint Surg Am. 1992;74:536–43. [PubMed] [Google Scholar]
- 16.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: Complications and outcomes in patiens over age 60. Spine (Phila Pa 1976) 2007;32:2238–44. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 17.Silvers HR, Lewis PJ, Asch HL. Decompressive lumbar laminectomy for spinal stenosis. J Neurosurg. 1993;78:695–701. doi: 10.3171/jns.1993.78.5.0695. [DOI] [PubMed] [Google Scholar]
- 18.Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine (Phila Pa 1976) 2003;28:348–53. doi: 10.1097/01.BRS.0000048494.66599.DF. [DOI] [PubMed] [Google Scholar]
- 19.Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M. Surgical outcome of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 2006;88:2714–20. doi: 10.2106/JBJS.F.00186. [DOI] [PubMed] [Google Scholar]
- 20.Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL. Risk-benefit assessment of surgery for adult scoliosis: An analysis based on patient age. Spine (Phila Pa 1976) 2011;36:817–24. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 21.Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232–7. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 22.Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 2008;33:2243–7. doi: 10.1097/BRS.0b013e31817d1d4e. [DOI] [PubMed] [Google Scholar]
- 23.Sasso RC, Garrido BJ. Postoperative spinal wound infections. J Am Acad Orthop Surg. 2008;16:330–7. doi: 10.5435/00124635-200806000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Calderone RR, Garland DE, Capen DA, Oster H. Cost of medical care for postoperative spinal infections. Orthop Clin North Am. 1996;27:171–82. [PubMed] [Google Scholar]
- 25.O’Neill KR, Smith JG, Abtahi AM, Archer KR, Spengler DM, McGirt MJ, et al. Reduced surgical site infections in patients undergoing posterior spinal stabilization of traumatic injuries using vancomycin powder. Spine J. 2011;11:641–6. doi: 10.1016/j.spinee.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 26.Strὃmqvist F, Jὃnsson B, Strὃmqvist B. Swedish Society of Spinal Surgeons. Dural lesions in decompression for lumbar spinal stenosis: Incidence, risk factors and effect on outcome. Eur Spine J. 2012;21:825–8. doi: 10.1007/s00586-011-2101-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An ananatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976) 1996;21:1133–8. doi: 10.1097/00007632-199605150-00002. [DOI] [PubMed] [Google Scholar]
- 28.Thuet ED, Padberg AM, Raynor BL, Bridwell KH, Riew KD, Taylor BA, et al. Increased risk of postoperative neurological deficit for spinal surgery patient with unobtainable intraoperative evoked potential data. Spine (Phila Pa 1976) 2005;30:2094–103. doi: 10.1097/01.brs.0000178845.61747.6a. [DOI] [PubMed] [Google Scholar]
- 29.Dearborn JT, Hu SS, Tribus CB, Bradford DS. Thromboembolic complications after major thoracolumbar spine surgery. Spine (Phila Pa 1976) 1999;24:1471–6. doi: 10.1097/00007632-199907150-00013. [DOI] [PubMed] [Google Scholar]
- 30.Smith JS, Fu KM, Polly DW, Jr, Sansur CA, Berven SH, Broadstone PA, et al. Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures: A report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2010;35:2140–9. doi: 10.1097/BRS.0b013e3181cbc8e7. [DOI] [PubMed] [Google Scholar]
- 31.Mohit AA, Fisher DJ, Matthews DC, Hoffer E, Avellino AM. Inferior vena cava thrombosis causing acute cauda equina syndrome. Case report. J Neurosurg. 2006;104(1 Suppl):46–9. doi: 10.3171/ped.2006.104.1.46. [DOI] [PubMed] [Google Scholar]


