Abstract
Background:
As the number of total hip arthroplasties (THAs) performed increases, so do the number of required revisions. Impaction bone grafting with Wagner SL Revision stem is a good option for managing bone deficiencies arising from aseptic osteolysis. We studied the results of cementless diaphyseal fixation in femoral revision after total hip arthroplasty and whether there was spontaneous regeneration of bone stock in the proximal femur after the use of Wagner SL Revision stem (Zimmer, Warsaw, IN, USA) with impaction bone grafting.
Materials and Methods:
We performed 53 hip revisions using impaction bone grafting and Wagner SL Revision stems in 48 patients; (5 cases were bilateral) for variety of indications ranging from aseptic osteolysis to preiprosthetic fractures. The average age was 59 years (range 44-68 years). There were 42 male and 6 female patients. Four patients died after surgery for reasons unrelated to surgery. 44 patients were available for complete analysis.
Results:
The mean Harris Hip Score was 42 before surgery and improved to 86 by the final followup evaluation at a mean point of 5.5 years. Of the 44 patients, 87% (n=39) had excellent results and 10% (n=5) had good results. The stem survival rate was 98% (n=43).
Conclusion:
Short term results for revision THA with impaction bone grafting and Wagner SL revision stems are encouraging. However, it is necessary to obtain long term results through periodic followup evaluation, as rate of complications may increase in future.
Keywords: Impaction bone grafting, revision arthroplasty, total hip arthroplasty, Wagner SL revision stem
INTRODUCTION
Severe proximal femoral bone loss is a formidable problem in reconstructive hip surgery.1 The results of surgery using a cemented revision femoral component are poor compared with those using a primary component.2,3 Use of cemented components in revision surgery for femoral loosening without biologic reconstruction of deficient bone stock carries a high risk of loosening.2,4,5 There are various techniques for the biological reconstruction of the proximal femur. Because the amount of autogenous bone graft is limited, allograft is widely used. When the proximal femoral shaft is sufficiently stable, the Exeter technique (impaction grafting) can be employed.6 Other authors prefer massive allografts combined with a long stem prosthesis.7 One of the methods to address this issue is by using diaphyseal fitting cementless stem which does not rely on proximal femoral bone stock for primary fixation.8 Also, with the possibility of second or third revision in future, restoration of bone stock is thought to be desirable. In 1987, Wagner presented a technique in which a cementless long stem prosthesis was fixed in the diaphysis and he reported excellent spontaneous osseous regeneration.8
We studied the results of cementless diaphyseal fixation stem in femoral revision after total hip arthroplasty using a Wagner SL Revision stem (Zimmer, Warsaw, IN, USA) with impaction bone grafting.
MATERIALS AND METHODS
53 revision total hip arthroplasties in 48 patients performed at our institution using the Wagner SL Revision stem with impaction bone grafting in a retrospective study conducted between July 1999 and December 2008.
Patients were evaluated clinically as well as serologically to rule out infection. History of hip pain at rest and/or night pain or painful range of motion was noted. Blood erythrocyte sedimentation rate (ESR) and C reactive protein level (CRP) were assessed in all the cases. Preoperative hip aspiration was reserved for the cases which had high levels of ESR or CRP or if prior hip arthroplasty failed within first 5 years of index hip arthroplasty. Radiologic analysis was done to determine the areas of osteolysis and to assess the amount of bone loss on the femoral and the acetabular side. Femoral bone defects were classified according to the system of Paprosky et al.9 Preoperative templating of femur was done in all cases to get an idea of minimum length and diameter of the stem required for optimal bone fixation in the diaphysis. In all cases, vertical offset was measured and restored peroperatively to address the issue of limb length discrepancy.
We used impaction bone grafting and Wagner SL Revision stems for femoral revision and bone grafting with uncemented cups for acetabular revision in all cases.
The choice of stem was diaphyseal fitting Wagner SL Revision stem which is made of a titanium–aluminum–niobium alloy with a rough-blasted surface. The shaft of the prosthesis has a conus angle of 2° and eight longitudinal ridges arranged in a circle around the stem.3 The stem is available in lengths of 190-385 mm. Cementless anchoring of the stem is achieved after implantation in a conically reamed femoral shaft. The longitudinal ridges give rotational stability. If there are larger defects in the proximal part of the femur, stable stem fixation can be achieved only distally in the diaphyseal part of the femur. The head is available in diameters of 22, 28 and 32 mm.
In all the cases, we used a straight stem (as curved stem was not available during the study period). Two different designs of Wagner stem were used in the study period. In the initial 11 cases, we used standard design Wagner prosthesis with 34 mm horizontal offset and in the rest 41 cases, increased offset design with 44 mm horizontal offset was used. This difference was due to the availability of increased offset stem during the latter part of the study period. Advantage of using a diaphyseal fitting stem is that it by passes the proximal femoral osteolytic area, completely relying for fixation on diaphysis which is not affected by aseptic osteolysis.
We used a mixture of autograft and allograft in all cases, as autograft alone is often not sufficient to fill bone defects. Autografts were harvested from the posterior iliac crest in the lateral position before the beginning of actual revision surgery. A commercially available bone mill was used to harvest the proper graft size from allografts. The source of allografts was fresh-frozen femoral heads preserved in the bone bank after retrieval from hemireplacement arthroplasty in patients with fractured femoral necks. A dedicated instrument set with the option of sequentially increasing diameter impaction broach was used for impaction bone grafting.
We used a posterolateral approach in all patients. A transfemoral approach was needed in 27. This was achieved by creating an open door osteotomy with the base on the anterolateral aspect of the femoral shaft, keeping the width of the osteotomy to less than one third of the femoral diameter. The location of the osteotomy corresponded to the middle and lower third of the stem for better access to the distal cement plug and easy removal of the cement mantle around the stem. The open door osteotomy was fixed with tensioned encirclage wires of minimum 20 Gauze stainless steel wire loop in all the cases. Reamers of progressively increasing sizes were introduced up to a marked depth. The stem was inserted into the medullary canal and was driven into position with a few strikes of a mallet. The prosthesis was advanced until the required stability was achieved and the prosthesis did not move any further. For the last 2 cm, the prosthesis drops only 1 mm with each forceful blow from a 2-lb mallet. A clue that the prosthesis has reached its final seating is the change in the sound of the mallet blow.
The surgeon implanted the shortest stem that ensured sufficient biomechanical stability. The conically reamed osseous bed in the medullary cavity should ideally be 100 mm long, with a minimum length of 70 mm.10 The diameter of the stems ranged from 14 to 19 mm (mean, 16 mm) [Figure 1]. For many of the patients, we used stems that were 265 mm long and had a diameter of 16 mm. Of 53 femoral stems, 32 were 265 mm long, 18 were 225 mm and 3 were 305 mm. In 10, the diameter was 14 mm; in another 10, 15 mm; in 28, 16 mm; in 4, 18 mm; and in 1, 19 mm. The size of the femoral stem was guided by preoperative templating. It is important for the tip of the stem to extend into the intact medullary canal at least 7 cm distal to the end of the previous prosthetic bed. In choosing the diameter, it is important to remember that the reaming removes a thin layer of bone and the sharp longitudinal ribs cut slightly into the bone during insertion. Therefore, the outline of the stem on the template must overlap the inner outline of the cortex in the region of middle third of the stem by 1 mm on each side.
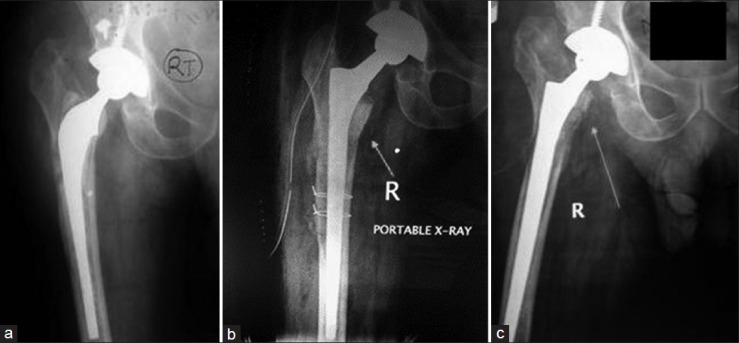
Figure 1.

Anteroposterior X-ray left hip (a) preoperative, showing failed THA (b) immediate postoperative, showintg long wagner stem in situ (c, d) 5 years followup, showing well incorporated impaction graft and long wagner stem in situ
Vertical offset was restored by deciding the final position of the stem in the last 1 cm in such a way that the distance between the proximal tip of prosthesis and superior portion of lesser trochanter equaled the preoperatively measured vertical offset distance. All the patients were given prophylactic low molecular weight heparin to prevent deep vein thrombosis. The indomethacin (75 mg) was given for 6 weeks to all patients to prevent heterotrophic ossification.
As soon as the effects of anesthesia wore off after surgery, usually by evening, we had the patients begin static quadriceps and abductor-strengthening exercises and foot-pump exercises. Full weight bearing was allowed from the third postoperative day at the earliest to as late as 6 weeks after surgery, depending on the type of bone defect and the stability of reconstruction. In type 2 bone defects, immediate weight bearing was permitted; in type 3 bone defects or in cases involving fracture of the greater trochanter, full weight bearing was delayed up to a maximum of 6 weeks. We did not use braces of any kind for immobilization. Any patient having persistent discharge from the wound after the first week of surgery was considered as early postoperative infection and early surgical intervention was done in all such cases.
For the first year after revision surgery, patients were examined monthly; after that, they were examined every 6 months or till the time when radiographic and clinical findings show incorporation of impaction graft. They were monitored for improvement in Harris Hip Score, as well as for any complications. Of the 48 patients, 4 died from causes unrelated to surgery; they had functioning hip joints, which were considered “survived” joints. The remaining 44 patients (39 had unilateral revision surgery and 5 had bilateral) were available for complete clinicoradiologic analysis.
Femoral component subsidence and migration were analyzed by measuring the vertical subsidence of component (from tip of the greater trochanter to shoulder of the prosthesis) according to the method of Callaghan et al.11
Allografts were assessed for incorporation into the host bone as evidenced by trabecular bridging of the host–graft interface. A clear reduction of density or breakdown of the transplanted bone was defined as bone resorption.
Since it is impossible to see bone growing into opaque metal surfaces on radiographs, the process was identified by the gradual changes in the appearance of periprosthetic bone (bone remodeling). Signs indicating successful bone ingrowth included narrowing of the intramedullary canal around the diaphyseal portion of the implant and atrophy of the bone around the proximal part of the stem. Signs of failed bone ingrowth included widening of the intramedullary space, formation of a demarcation line within the space and hypertrophy of the proximal bone, particularly around the lesser trochanter. Any signs of movement of the stem within the canal also indicated that biologic fixation has not occurred.
RESULTS
The average age of the patients at the time of surgery was 59 years (range 44-68 years). There were 42 men and 6 women in our study.
Out of 53 cases, 43 had unilateral revision surgery and 5 had bilateral revision surgery. 30 patients underwent revision surgery because of painful aseptic loosening, 11 for a periprosthetic fractures with aseptic loosening, 3 for a broken femoral stem, 3 for septic loosening and 1 for a traumatic comminuted fracture of the proximal one third of the femoral shaft with hip dislocation 6 months after the primary uncemented total hip arthroplasty (THA).
Indication on index hip replacement surgery were as follows:, 39 patients underwent index THA for avascular necrosis, 7 for posttraumatic arthritis and 2 for septic arthritis. The average time span from index to revision surgery was 7.5 years (range, 6 months-18 years). The revised stems were cemented Charnley (n=32), Muller (n=13); isoelastic total hip arthroplasty (n=3); cemented long stems (n=2); cemented bipolar hip arthroplasty (n=2) and, a Cementless Spotorno stem (n=1).
Bone defects were clarified as per Paparosky et al.,9 1 patients had type 2 defects and 37 patients had type 3 defects (32 with type 3A and 5 with type 3B).
The femoral component was revised in all cases, whereas the acetabulum was revised in 39. Regarding the intraoperative complications, 12 patients had an inadvertent fracture of the greater trochanter during surgery while undergoing dislocation or cement removal and were fixed with circlage wiring. We preferred transfemoral osteotomy instead of ETO so that patients could be rehabilitated quicker. Contributing factors to fracture were relatively older age of the patients and profound stress shielding and osteopenia.
Three patients had dislocation in the early postoperative period i.e. within 6 months. Two needed operative intervention and one was managed conservatively. Seven patients developed early postoperative infection. All were managed with early operative intervention; six of them were cured and one needed implant removal. One patient fell 7 days after surgery, during rehabilitation, which caused breakage of the wire used for fixation of the greater trochanter and resulted in stem rotation and was managed by surgical reintervention.
23 (48.91%) of our patients had subsidence of <5 mm and 2 patients (4.16%) had subsidence of >10 mm [Figure 2]. The osteointegration of grafts into the host bone was noted within 9-18 months (average 15 months) of surgery. We did not have any case of periprosthetic fracture, sciatic or femoral nerve palsy, or heterotrophic ossification. There were no instances of graft rejection, progressive osteolysis, or rerevision of Wagner stems. The mean preoperative Harris Hip Score of 42 points (range 22-52 points) had improved to 86 points (range 74-94 points) by the final followup evaluation [Figure 3]. Results were excellent in 87% of our cases (37 patients or 42 hips) and good in 10% (5 patients or 5 hips).
Figure 2.
Anteroposterior x-ray right hip joint (a) preoperative showing subsidence; (b) Immediate postoperative showing long Wagner stem in situ. Patient developed infection postoperatively. Debridement was done with removal of encirclage wires. (c) 8 months followup, showing subsidence
Figure 3.
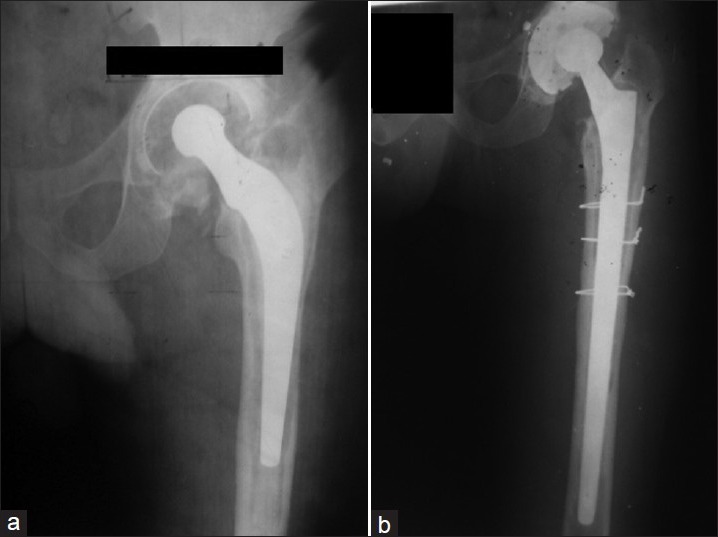
X-ray left hip joint anteroposterior view (a) preoperative, showing implant failure (b) 6 year followup, showing incorporation of impaction graft and implant in situ
DISCUSSION
The idea of impaction bone grafting was originally conceived in 1975 by Hastings and Parker to overcome the bone loss seen in patients with protrusio acetabuli secondary to rheumatoid arthritis.12 Three years later, McCollum and Nunley showed the potential of morselized allograft to treat bone stock deficiency in protrusio acetabula.13 In 1983, Roffman et al. reported the survival of bone chips under a layer of bone cement in an animal study.14 The graft appeared viable and new bone formed along the cement interface. Mendes et al. further developed the technique for use in primary hip arthroplasty with cement by reinforcing protrusio acetabuli with bone chips and mesh.15 They monitored eight patients for up to 6 years. There were no revisions and histologic examinations confirmed bone graft incorporation. In 1984, Slooff et al. modified the technique and described it as impaction bone grafting.16 The defect was contained by mesh and then bone graft was tightly packed in before an acetabular cup was inserted into the pressurized cement. Slooff et al. standardized the technique and developed special instrumentation. Impaction bone grafting of the proximal part of the femur was initially developed by Ling et al. in 1991 and reported by Gie et al. in 1993.6 The efficacy of these techniques has been extensively supported by results from animal studies as well as histologic,17,18 radiographic and biomechanical studies.19,20 We used a modified Slooff technique for impaction bone grafting, employing a mixture of autograft and allograft in patients selected for revision THA with a Wagner SL Revision stem.
The average age of patients at the time of surgery in our study was 59 years (range 44-68 years). Males outnumbered the females in revision hip surgeries, as the most common indication for primary total hip arthroplasty is avascular necrosis of femur which is more common in males.
Thirty two of 53 revised cases had cemented Charnley stem, as this is the most commonly used stem at many centers in India. Aseptic osteolysis with or without periprosthetic fracture was the number one cause of revision surgery. The average time span ranged from 6 months to 18 years. Out of 53 cases, 12 had periprosthetic fracture, one within 6 months of surgery. The patient who needed revision surgery at 6 months was the one with a traumatic comminuted fracture of the proximal one third of the femoral shaft and hip dislocation 6 months after undergoing primary uncemented THA with a CLS Spotorno stem. The reason for the high number of periprosthetic fractures on presentation was because number of patients (22.5%; 12 out of 53) missed followup examinations after index the THA with their primary surgeons and sought treatment only after fractures occurred. In our series, femur was revised in all cases, whereas acetabulum was revised in 39 cases.
The reason for choosing this revision technique over others is that it conserves bone and is a more biological surgery, allowing restoration of bone defects in view of the possibility that second or third revisions might be required. This technique is universal, meaning that it can be used with any type of bone defect often encountered in revision THA. The use of impaction bone grafting in addition to the use of a Wagner SL Revision stem allows consistent incorporation of the bone graft in defects [Figure 1d].
High number of immediate postoperative infection may be due to our very low tolerance in terms of wound discharge of any kind in the early postoperative period long duration of surgery, previous hip surgery, increased blood loss and the use of allograft as a source of bone graft. Patients were declared cured only after minimum 6 months of close clinical and serological monitoring at regular intervals, with all parameters consistently being negative for infection. This approach of ours resolved the issue in six patients; in the other patient, the implant was removed because of recurrent infection. This was a case of septic osteolysis in which a two stage revision was done. In the rest 2 cases, single stage revision was done.
We had 3 patients out of 53 cases who had dislocation in the early postoperative period i.e. within 6 months. In one patient, the dislocation was complicated by the dislodgement of the liner from the uncemented cup and was treated by changing the liner. The second patient had dislocation on the fourth day after surgery and was treated with closed reduction and bed rest for 4 weeks; he had no further episodes of dislocation during his 3-year followup period. The other patient had three dislocations in the first year after surgery and needed a change in the inclination of his acetabular cup.
The other postoperative complications, one patient had trauma and stem rotation. We treated the patient by changing the component's orientation and refixing the greater trochanter using the same Wagner stem; the patient was prescribed bed rest. The patient then developed a superficial infection, which we treated with surgical debridement and 6 weeks of parenteral antibiotics. After that, the patient's recuperation was uneventful.
Femoral component subsidence and migration were analyzed by measuring the vertical subsidence of component (from tip of the greater trochanter to shoulder of the prosthesis), according to the method of Callaghan et al.11 The reason for the high incidence of subsidence (within 5 mm in 23 patients) may be our aggressive rehabilitation protocol which allows the patient full weight bearing from practically the third postoperative day. None of them required any compensation. Two patients did have subsidence more than 10 mm and did require shoe raise.
High failure rates after cemented revision THA have led to the promotion of uncemented long stem femoral prostheses.21 Uncemented femoral components have several advantages: The difficulties and complications associated with cement removal are eliminated, bone loss may be reduced and implant removal is relatively easier. A review of the literature has shown lower rates of repeat revision after revision arthroplasties that use an uncemented femoral component.22 Most such repeat revisions have been performed within the first few postoperative months and have been necessary because a suboptimal stem size was used. Our results seem encouraging because the survival rate stabilized after 5.5 years. We believe that our results are comparable with those of arthroplasties employing an extensively porous-coated chromium–cobalt stem.22,23,24 Krishnamurthy et al.,23 in a series involving 297 extensively coated chromium–cobalt stems, noted a mechanical failure rate of only 2.4% at a mean followup point of 8.3 years.
New bone formation has been observed to occur regularly after femoral revision with the Wagner SL Revision stem.8,25,26,27 However, it is necessary to be aware of the limitations of the qualitative assessment of the bone formation on plain radiographs. In our experience, mechanical stability and careful removal of cement, scar and granulation tissue are the essential preconditions for spontaneous restoration of the bone stock of the proximal femur. In difficult cases, a transfemoral approach is helpful; but when this approach is used, the blood supply of the osseous lid must be preserved and detachment of the muscles must be avoided. Femoral bone restoration associated with the use of Wagner SL Revision stem may be due to the proximal transmission of force because of the conical shape of the prosthesis, the higher elasticity of the titanium alloy and the good histocompatibility of the rough-blasted surface.10 In our patients, at a mean followup point of 5.5 years after revision THA using impaction bone grafting and Wagner SL Revision stems, we observed a 97.9% survival rate for the stems, with rerevision of stems or stem removal for any cause counted as the endpoint or failure.
We conclude short term results for revision THA with impaction bone grafting Wagner SL Revision stems are encouraging. However, it is necessary to obtain long term results through periodic followup evaluation because the rate of complications, such as femoral osteolysis, aseptic loosening, periprosthetic fracture and late infection, may increase with time.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Roberson JR. Proximal femoral bone loss after total hip arthroplasty. Orthop Clin North Am. 1992;23:291–302. [PubMed] [Google Scholar]
- 2.Franzén H, Mjöberg B, Önnerfält R. Early loosening of femoral components after cemented revision. A roentgen stereophotogrammetric study. J Bone Joint Surg Br. 1992;74:721–4. doi: 10.1302/0301-620X.74B5.1527121. erratum, 1993;75:169. [DOI] [PubMed] [Google Scholar]
- 3.Wagner H. Postgraduate lectures of the first European Federation of National Associations of Orthopaedics and Traumatology (EFORT) Paris: Masson; 1993. Revision of femoral stem with important loss of bone stock; p. 64. [Google Scholar]
- 4.Engelbrecht DJ, Weber FA, Sweet MB, Jakim I. Long-term results of revision total hip arthroplasty. J Bone Joint Surg Br. 1990;72:41–5. doi: 10.1302/0301-620X.72B1.2298793. [DOI] [PubMed] [Google Scholar]
- 5.Kavanagh BF, Ilstrup DM, Fitzgerald RH., Jr Revision total hip arthroplasty. J Bone Joint Surg Am. 1985;67:517–26. [PubMed] [Google Scholar]
- 6.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 7.Gross AE, Allan DG, Lavoie GJ, Oakeshott RD. Revision arthroplasty of the proximal femur using allograft bone. Orthop Clin North Am. 1993;24:705–15. [PubMed] [Google Scholar]
- 8.Wagner H. Revision prosthesis for the hip joint in severe bone loss [in German] Orthopäde. 1987;16:295–300. [PubMed] [Google Scholar]
- 9.Paprosky WG, Valle CD. Classification and algorithmic approach to reconstruction of femoral bone deficiency in revision hip arthroplasty. J Bone Joint Surg Am. 2003;85A(Suppl 4):1–6. doi: 10.2106/00004623-200300004-00001. [DOI] [PubMed] [Google Scholar]
- 10.Wagner H, Wagner M. Hip prosthesis revision with the noncemented femoral revision stem-10 years experience. Med Orth Tech. 1997;117:138. [Google Scholar]
- 11.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year followup. J Bone Joint Surg Am. 1985;67:1074–85. [PubMed] [Google Scholar]
- 12.Hastings DE, Parker SM. Protrusio acetabuli in rheumatoid arthritis. Clin Orthop Relat Res. 1975;108:76–83. doi: 10.1097/00003086-197505000-00012. [DOI] [PubMed] [Google Scholar]
- 13.McCollum DE, Nunley JA. Bone grafting in acetabular protrusio: a biological buttress. In: Nelson CL, editor. The hip: Proceedings of the sixth open scientific meeting of the hip society. St. Louis: CV Mosby; 1978. p. 124. [Google Scholar]
- 14.Roffman M, Silbermann M, Mendes DG. Incorporation of bone graft covered with methylmethacrylate onto the acetabular wall. An experimental study. Acta Orthop Scand. 1983;54:580–3. doi: 10.3109/17453678308992892. [DOI] [PubMed] [Google Scholar]
- 15.Mendes DG, Roffman M, Silbermann M. Reconstruction of the acetabular wall with bone graft in arthroplasty of the hip. Clin Orthop Relat Res. 1984;186:29–37. [PubMed] [Google Scholar]
- 16.Slooff TJ, Huiskes R, van Horn J, Lemmens AJ. Bone grafting in total hip replacement for acetabular protrusion. Acta Orthop Scand. 1984;55:593–6. doi: 10.3109/17453678408992402. [DOI] [PubMed] [Google Scholar]
- 17.Nelissen RG, Bauer TW, Weidenhielm LR, LeGolvan DP, Mikhail WE. Revision hip arthroplasty with the use of cement and impaction grafting. Histological analysis of four cases. J Bone Joint Surg Am. 1995;77:412–22. doi: 10.2106/00004623-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Ullmark G, Linder L. Histology of the femur after cancellous impaction grafting using a Charnley prosthesis. Arch Orthop Trauma Surg. 1998;117:170–2. doi: 10.1007/s004020050221. [DOI] [PubMed] [Google Scholar]
- 19.Schimmel JW, Buma P, Versleyen D, Huiskes R, Slooff TJ. Acetabular reconstruction with impacted morselized cancellous allografts in cemented hip arthroplasty: A histological and biomechanical study on goat. J Arthroplasty. 1998;13:438–48. doi: 10.1016/s0883-5403(98)90010-9. [DOI] [PubMed] [Google Scholar]
- 20.Malkani AL, Voor MJ, Fee KA, Bates CS. Femoral component revision using impacted morsellised cancellous graft. A biomechanical study of implant stability. J Bone Joint Surg Br. 1996;78:973–8. doi: 10.1302/0301-620x78b6.1288. [DOI] [PubMed] [Google Scholar]
- 21.Gorab RS, Covino BM, Borden LS. The rationale for cementless revision total hip replacement with contemporary technology. Orthop Clin North Am. 1993;24:627–33. [PubMed] [Google Scholar]
- 22.Wirtz DC, Niethard FU. Etiology, diagnosis and therapy of aseptic hip prosthesis loosening: A status assessment [in German] Z Orthop Ihre Grenzgeb. 1997;135:270–80. doi: 10.1055/s-2008-1039388. [DOI] [PubMed] [Google Scholar]
- 23.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year followup study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12:839–47. doi: 10.1016/s0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 24.Lawrence JM, Engh CA, Macalino GE, Lauro GR. Outcome of revision hip arthroplasty done without cement. J Bone Joint Surg Am. 1994;76:965–73. doi: 10.2106/00004623-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;319:141–50. [PubMed] [Google Scholar]
- 26.Stoffelen DV, Broos PL. The use of the Wagner revision prosthesis in complex (post) traumatic conditions of the hip. Acta Orthop Belg. 1995;61:135–9. [PubMed] [Google Scholar]
- 27.Wehrli U. Wagner revision of prosthesis stem [in German] Z Unfallchir Versicherungsmed. 1991;84:216–24. [PubMed] [Google Scholar]


