Abstract
Background:
Relapse of clubfoot deformity following correction by Ponseti technique is not uncommon. The relapsed feet progress from flexible to rigid if left untreated and can become as severe as the initial deformity. No definitive classification exists to assess a relapsed clubfoot. Some authors have used the Pirani score to rate the relapse while others have used descriptive terms. The purpose of this study is to analyze the relapse pattern in clubfeet that have undergone treatment with the Ponseti method and propose a simple classification for relapsed clubfeet.
Materials and Methods:
Ninety-one children (164 feet) with idiopathic clubfeet who underwent treatment with Ponseti technique presented with relapse of the deformity. There were 68 boys and 23 girls. Mean age at presentation for casting was 10.71 days (range 7-22 days). Seventy three children (146 feet, 80%) had bilateral involvement and 18 (20%) had unilateral clubfeet. The mean Pirani Score was 5.6 and 5.5 in bilateral and unilateral groups respectively. Percutaneous heel cord tenotomy was done in 65 children (130 feet, 89%) in the bilateral group and in 12 children (66%) with unilateral clubfoot.
Results:
Five relapse patterns were identified at a mean followup of 4.5 years (range 3-5 years) which forms the basis of this study. These relapse patterns were classified as: Grade IA: decrease in ankle dorsiflexion from15 degrees to neutral, Grade IB: dynamic forefoot adduction or supination, Grade IIA – rigid equinus, Grade IIB – rigid adduction of forefoot/midfoot complex and Grade III: combination of two or more deformities: Fixed equinus, varus and forefoot adduction.
In the bilateral group, 21 children (38 feet, 28%) had Grade IA relapse. Twenty four children (46 feet, 34%) had dynamic intoeing (Grade IB) on walking. Thirteen children (22 feet, 16%) had true ankle equinus of varying degress (Grade IIA); eight children (13 feet, 9.7%) had fixed adduction deformity of the forefoot (Grade IIB) and seven children (14 feet, 10.7%) had two or more fixed deformities. In the unilateral group seven cases (38%) had reduced dorsiflexion (Grade IA), six (33%) had dynamic adduction (Grade IB), two (11%) had fixed equinus and adduction respectively (Grade IIA and IIB) and one (5%) child had fixed equinus and adduction deformity (Grade III). The relapses were treated by full time splint application, re-casting, tibialis anterior transfer, posterior release, corrective lateral closing wedge osteotomy and a comprehensive subtalar release. Splint compliance was compromised in both groups.
Conclusion:
Relapse pattern in clubfeet can be broadly classified into three distinct subsets. Early identification of relapses and early intervention will prevent major soft tissue surgery. A universal language of relapse pattern will allow comparison of results of intervention.
Keywords: Classification, clubfoot, Ponseti technique, relapse
INTRODUCTION
The Ponseti technique of clubfoot has gained considerable popularity in the last decade, with a success rate of over 90% for initial correction1,2,3 However, relapses are not uncommon and the rate varies from 10% to 30% depending on the amount of followup.4,5,6,7
Most authors define “relapse” as any foot requiring further intervention following successful correction with the Ponseti technique.8,9,10 Some authors use descriptive terms depending on foot morphology, i.e., adductus, varus, equinus, or combination. Others have used the Pirani or Dimeglio score to rate the relapses.4,5,6,7 Clubfeet relapses have also been classified as minor and major depending on the extent of invasive surgery required on these feet.11 However, no definitive classification exists to grade clubfeet relapse after the completion of Ponseti's technique.
We have observed that the relapse pattern in clubfeet undergoing correction with the Ponseti regime follows a pattern: The initial relapses are supple, as the muscle imbalance causes dynamic deformities which, if not addressed in time, can lead to static or rigid deformities. This relapse pattern may also be influenced by the foot abduction orthosis (FAO) which is an important component of the Ponseti regimen until 3-4 years of age.1,12,13,14,15
The purpose of our study was to analyze the pattern of relapse after Ponseti treatment of idiopathic clubfoot and propose a simple classification to grade these feet. We feel that a universal language to grade relapses will help in planning and standardizing further treatment.
MATERIALS AND METHODS
Two hundred and six children (362 feet) with idiopathic clubfeet treated with the Ponseti method from 2004 to 2008 were reviewed for relapse of their deformities. Forty three children (78 feet) from the above cohort treated at our institute and 48 (86 feet) children who had undergone treatment elsewhere were identified with a relapse. Inclusion criteria were those children who had been treated with conventional Ponseti technique and had complete correction of their deformity at the initial treatment and had their complete records and charts available for assessment. Thus, there were 91 children (164 feet) available for the final analysis. Neurogenic feet, atypical clubfoot and syndromic deformities were excluded. There were 68 boys and 23 girls. Seventy three children (146 feet) had bilateral clubfeet and in 18 (18 feet) children the deformity was unilateral. Mean interval between first presentation of virgin clubfeet and initial casting was 10.71 days (range 7-22 days). The charts and records of all patients were reviewed for the (a) Pirani score at the onset of treatment, (b) amount of serial cast changes required, (c) need for heel cord tenotomy and (d) compliance with splint wear.
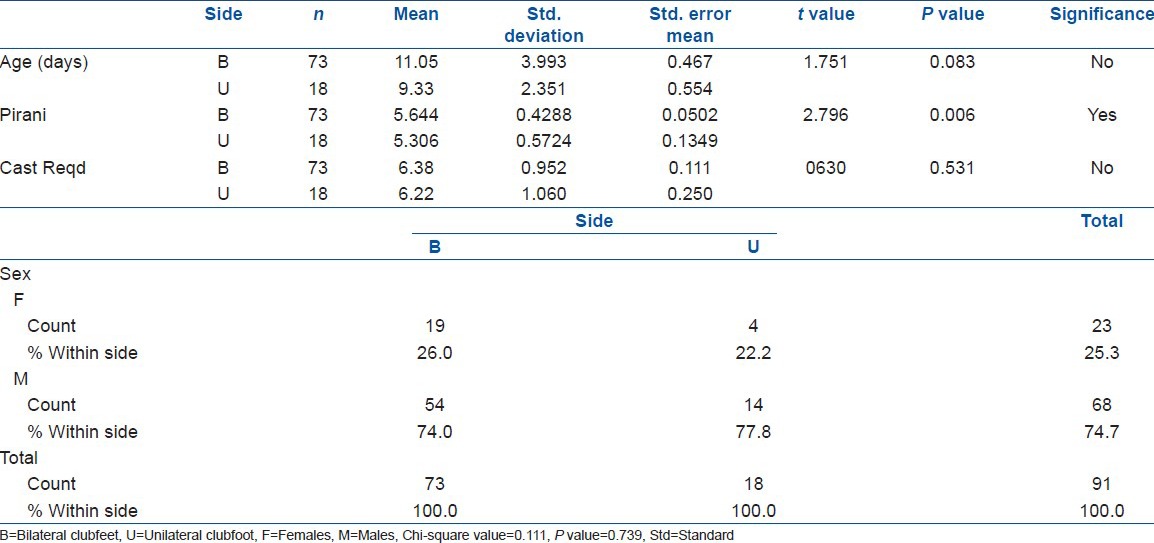
The mean Pirani score in the bilateral clubfeet group was 5.5 (range 5-6) and in the unilateral clubfeet group was 5.2 (range 4-6). The mean number of casts required in the bilateral and unilateral groups was 6.3 (range 5-8 casts) and 5.3 (range 4-7 casts), respectively [Table 1]. Cast changes were done at weekly intervals in the plaster room and no anesthesia was used during this casting procedure. Percutaneous heel cord tenotomy was performed on both sides in 65 out of 73 children (130 feet; 89%) in the bilateral group and 12 out of 18 children (12 feet; 66%) children in the unilateral clubfeet group.
Table 1.
Age at presentation, sex distribution, Pirani score and number of casts required in bilateral and unilateral clubfoot
The last cast was applied for 4 weeks following which the Steenbeek Foot Abduction Orthosis (SFAB) manufactured locally was fitted (Maooli Surgical Inc., Mumbai, India). The foot piece of this SFAB was set at 15° dorsiflexion and 70° of external rotation. In unilateral cases, the normal foot was set at 45° external rotation. All children wore the orthosis for 22 h/day for initial 3 months and later, a minimum of 12 h/day. After 3 months, a static ankle foot orthosis (AFO) was used at daytime. At walking age, straight last shoes (medial border of the shoe was straight) were used during the day with continuation of night time SFAB. The SFAB was recommended for 3 years.
The mean age at presentation of relapse was 4 years (range 2-6 years). Relapse was defined as recurrence of any component of the clubfoot deformity requiring treatment after commencement of FAO.
Five relapse patterns were identified at followup: Grade IA, decrease in ankle dorsiflexion from 15° neutral with the knee in extension with passive stretch [Figure 1a and b]; Grade IB, dynamic supination or adduction on walking [Figure 2a]; Grade IIA, fixed ankle equinus of any degree [Figure 2b]; Grade II B, fixed adduction which is not correctable by passive abduction of foot [Figure 3a and b]; and Grade III, combination of fixed hind foot equinus plus forefoot adduction and cavus or complete rigid equino-cavo-varus foot [Figure 4a-d] [Table 2].
Figure 1.
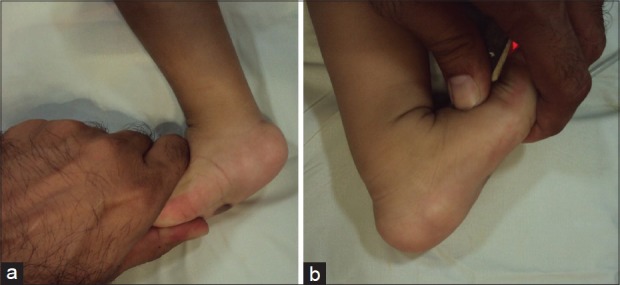
(a) Clinical photograph showing decrease in ankle dorsiflexion to neutral while stressing the foot (b) Comparative view of the opposite foot showing ankle dorsiflexion of 15°
Figure 2.
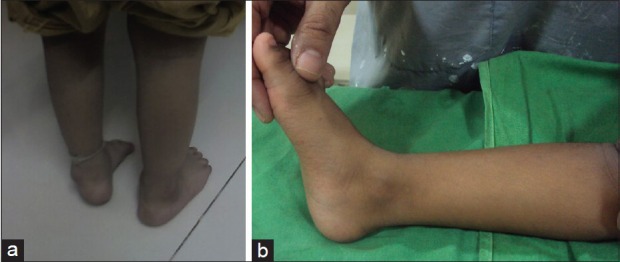
(a) Clinical photograph of a case of bilateral clubfoot. Left foot shows dynamic forefoot adduction and supination. The heel varus is flexible and this pattern manifests as intoeing gait on walking. This child has Grade IB relapse pattern (b) Clinical photograph of a 4-year-old child with unilateral clubfoot foot showing the hind foot is in equinus and passive correction to neutral is not possible. This child has Grade IIA relapse pattern
Figure 3.

Clinical photograph of a five year old child with bilateral clubfoot. (a) Plantar view showing bilateral forefoot adduction deformity. The heel position is neutral. (b) Frontal view showing the forefoot/midfoot adduction. This child had Grade IIB relapse pattern
Figure 4.

Clinical photographs showing (a) Plantar and (b) lateral view of the foot showing complete relapse with heel varus, equinus, adduction and deformity. (c) Plantar view of the foot showing adduction deformity of the foot in a 5 year old child. (d) Prone view showing equinus deformity in the same child. These children had Grade III relapse
Table 2.
Classification of relapse pattern in clubfoot following Ponseti treatment
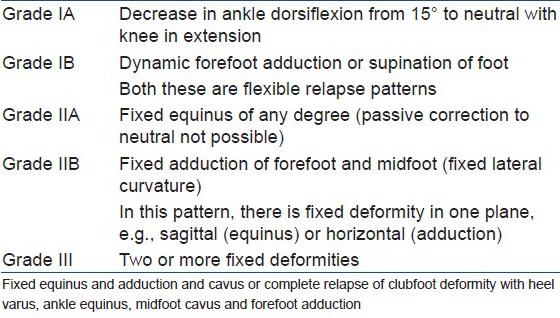
These relapse patterns were grouped into three categories: In Grade I relapse pattern, the feet were supple. In Grade II relapse pattern, there is fixed deformity in one plane, either sagittal or coronal, rigid equinus or rigid adduction in the midfoot manifested by lateral curvature of foot that is not correctable with passive stretching. Movements of the foot in the other planes are supple. Grade III relapses have two or more fixed deformities in sagittal, coronal and horizontal planes. The “A” and “B” suffix indicates the two planes of movement of the foot. This forms the basis of our classification.
Children were questioned on their ability to run, climb stairs, squat at floor and for ease of shoe wear.
Statistical analysis was done with the SPSS 20.0 version using Chi-square analysis and unpaired “t,” test and with significance at P < 0.05.
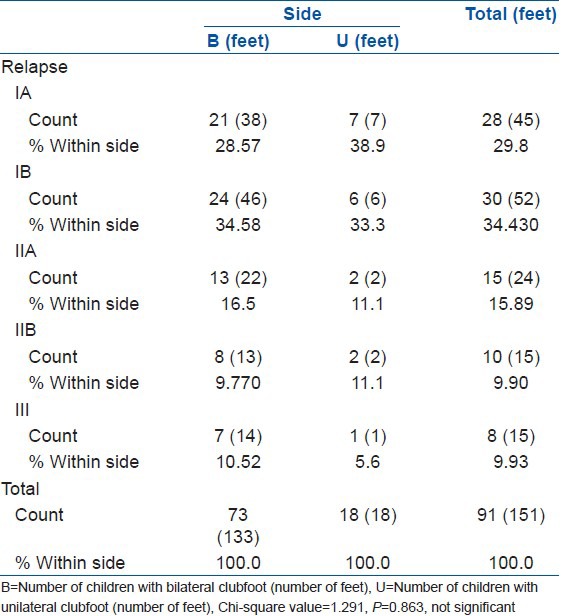
Age at presentation, Pirani score and number of casts are all quantitative variables and for them, the differences between bilateral and unilateral clubfeet groups were compared using unpaired “t” test [Table 1]. The Pirani score distribution among the two groups was found to be statistically significant (P = 0.006). The sex distribution is a binomial variable and the differences between bilateral and unilateral clubfeet groups were compared using Chi-square test. The classification of relapse pattern is a multinomial variable and the differences between bilateral and unilateral groups were compared using the Chi-square test [Table 3].
Table 3.
Rate of occurrence of various relapse patterns in bilateral and unilateral clubfeet in 91 children (151 feet out of 164 clubfeet)
RESULTS
There was no significant difference between the two groups for age at presentation, sex ratio, mean Pirani score and mean number of casts required for correction (Chi-square value = 0.111, P = 0.739). The mean followup period after application of FAO was 4.5 years (3-5 years).
The mean followup of the relapsed cases was 24 months (range 12-28 months) however we continued to monitor these feet. In the bilateral clubfeet group, 21 children (38 feet; 28%) had a decrease in ankle dorsiflexion from the recommended 15° up to neutral (Grade IA). An average of 4 readings was taken with a goniometer by the surgeon or his assistant on a single occasion. Twenty four (46 feet; 32%) children had dynamic adduction or supination (Grade IB) on walking and the foot progression angle was negative (intoeing). This could be due to muscle imbalance between the abductor hallucis and tibialis anterior on the medial side and peroneal muscle on the lateral side. Thirteen children (22 feet; 17%) had true ankle equinus of varying degrees (Grade IIA), i.e., the foot could not be positioned in neutral plantigrade position with passive dorsiflexion. Eight children (13 feet; 10%) had fixed adduction deformity of the forefoot (Grade IIB), i.e., the lateral border of the foot was curved and could not be straightened. The heel was in neutral position and ankle position varied from neutral to varying degrees of dorsiflexion. Four children (8 feet; 5%) had both equinus at the ankle and adduction at the forefeet with heel varus and three children (6 feet; 4%) had complete relapse of equinus, varus and adduction with cavus. The last two groups were combined as Grade III relapse pattern. Thirteen children had no relapse in the opposite feet in the bilateral group.
In the unilateral group, the distribution of children in various groups was as follows: Seven children (7 feet; 38%) had reduced dorsiflexion (Grade IA), six (6 feet; 33%) had dynamic adduction (Grade IB), two (2 feet; 11%) had fixed equinus and adduction, respectively (Grade IIA and IIB) and one child (5%) had fixed equinus and adduction deformity (Grade III). There was no difference between the rate of relapse in the bilateral group as compared to that in the unilateral group [Table 3]. Children in Grade II relapse had difficulty in squatting on floor, running and climbing stairs. Shoe wear did not pose a problem. In Group III, children had same discomfort as in group II and also had difficulties in normal shoe wear. Group I children had no problems with the above functional activities.
Splint compliance was compromised in both the groups. Only 10 (10.98%) children wore the FAO for the recommended 12 h at bedtime. These 10 children had mild flexible relapses: 4 had Grade IA relapse and 6 had Grade IB relapse. Eighty one children had poor compliance (89%); 39 of these were flexible relapses, 25 progressed to rigid equinus or adduction deformity and 8 progressed to full relapse of their clubfoot deformity requiring a complete subtalar release. Thus, noncompliance with FAO was associated with worse outcome. Given the low numbers in each group, the statistical analysis was not performed.
DISCUSSION
The Ponseti method of clubfoot correction has considerably decreased the need for radical surgery and its attending complications.16,17,18,19,20 Relapses following clubfoot surgery are complicated by skin problems, foot stiffness, bony deformities and soft tissue scarring.19 Relapses following the Ponseti method are more subtle and the foot stays supple due to minimum surgical intervention.21
The Pirani score and Dimeglio classification are useful to grade the initial extent of the deformity and to assess the progress of foot correction.22,23 These scores can predict the number of casts required, need for tenotomy and recurrences, but cannot predict compliance with the FAO which is imperative for a successful outcome at long term.8,24,25,26 A relapsed clubfoot after Ponseti technique rarely present as an untreated clubfoot. The typical deep medial and posterior creases are uncommon and the talar head is often reducible unless the relapse is very severe. No specific classification exists to rate relapse profile of clubfoot deformity after Ponseti correction. Goriainov et al.27 defined relapse as any deformity occurring after commencement of the FAO that required further treatment. In their study seventeen feet out of 80 relapsed after a mean interval of 23 months after the initiation of the FAO. They excluded children who had had primary treatment elsewhere. Their observation was that a higher initial Pirani score was associated with late relapse. Haft et al.11 have classified recurrence as minor if the child required a tendon transfer or an Achilles tendon lengthening and major if the child needed a full posterior or posteromedial release (P).
Masrouha and Morcuende7 recently reviewed the relapse rate after tibialis anterior tendon transfer (TATT) in feet treated with Ponseti technique. Relapse was defined as presentation with one or more components of the deformity (e.g., equinus, hind foot varus, forefoot adductus and cavus) that required further treatment. Ten (15 feet) of 66 (102 clubfeet) children had a relapse which required casting (6 cases) and bracing and one case needed a cuboid osteotomy.
Porecha et al. studied 49 children with clubfeet treated with the Ponseti technique after a mean followup at 5 years. They used the functional Ponseti scoring system to analyze their results. Fourteen children (28%) presented with relapse at varying age groups and poor compliance with the orthosis was identified as the main cause.28 Thus, relapse is an important component of the Ponseti technique and early recognition with prompt treatment gives the best long term results.29 However, different authors have used varying terms to describe a relapse. There seems to be no common consensus and therefore interpretation of results can be difficult.30 Early relapse presents as decrease in ankle dorsiflexion (Grade IA) and the hind foot may not have any posterior creases; the heel may be well palpable and hence will be scored zero on the Hind Foot Score (HFS) of Pirani. Dynamic intoeing will also be underestimated on the Pirani score. With rigid equinus deformity (Grade IIA), the heel is never completely empty as in a virgin clubfoot and an HFS of 2 or 3 may not have any quantitative difference and thus will need similar treatment. HFS includes deep posterior creases, empty heel and reduced dorsiflexion, which essentially records the same thing and all components of the Pirani score are not equally weighted.26 The Dimeglio score assesses stiffness of the foot across four planes: Sagittal (equinus), frontal (varus), horizontal (forefoot adduction) and rotation around the talus-calcaneo-forefoot axis; these are present in varying degrees in the virgin clubfeet, but not in all grades of relapsed feet. Relapses will be classified as moderate, severe and very severe with individual description of the deformity. Thus, the classification of relapses with these two methods will have several permutations for ascribing specific treatment.
During our assessment of clubfoot deformity at followup, we envisaged five different patterns of relapse which required specific treatment. The equinus deformity that is corrected last, is the first to reappear in a relapsed foot. Persistent dynamic intoeing is usually associated with poor brace compliance. The importance of decreasing dorsiflexion of the ankle (Grade IA) is still unclear. Some ankle dorsiflexion is lost with subsequent growth of the foot, but many children have no functional limitations. We do not hesitate to recast once the ankle dorsiflexion reaches neutral with knee extension, or the child has difficulty in squatting, as this would inevitably lead to a fixed equinus.
Dynamic forefoot adduction or supination that manifests as intoeing (Grade IB) is the most common type of relapse pattern seen with the Ponseti technique and was seen in 24 children. The heel usually stays in the neutral position or there is flexible hind foot varus. In this group of patients, we encouraged parents to improve the compliance with FAO and in 10 cases, we even reintroduced full time FAO (22 h/day). Almost 30% children require TATT to support the evertor power of the forefoot. This observation also reinforces the need to maintain the FAO for long term use to prevent intoeing secondary to foot invertor–evertor muscle imbalance. The role of abductor hallucis in causing adduction deformity and intoeing has received scant attention. We now routinely do abductor hallucis tenotomy during TATT surgery to prevent recurrence. Six cases have undergone this procedure and we continue to monitor these children. In 24 children, the dynamic intoeing improved after introduction of full time bracing (22 h/day for 3 months).
We recommend a formal posterior release rather than re-tenotomy for the rigid equinus deformity (Grade IIA relapse). The scarring due to previous tenotomy causes fibrosis right up to the posterior capsule and achieving 15° of dorsiflexion needs repeated casting under anesthesia. We prefer a single surgery to obtain correction which reduces the need for repeat casting and consequent stiffness of foot. For fixed adduction deformity (Grade IIB relapse pattern), a lateral column closing wedge osteotomy based on the apex of deformity is indicated. A medial column lengthening can be combined with this procedure. Seven children (10 feet) have undergone this procedure and the feet are supple and well corrected at 18 months followup. For Grade III relapse, we proceed with a comprehensive subtalar release. At last followup four children had undergone surgery to achieve a plantigrade foot and four were awaiting surgery.
Rigid deformities in an adequately corrected clubfoot are almost always preceded by flexible muscle imbalances. We particularly noted from our study that relapses are usually preceded by discontinuation of night time FAO or poor compliance. Duration of splint wear less than 12 h/day compromises the result after Ponseti technique and leads to less satisfactory outcome.
The search for the perfect orthosis is still on. Several designs have been used and even a unilateral FAO has been fabricated with limited success.31,32,33 The FAO also is an integral part of the Ponseti regimen and outcome studies in typical idiopathic clubfeet will certainly revolve around an orthosis which can influence the remodeling of a foot.34
There are several limitations of this study. Since it is a review from a single center, there are chances of bias in patient selection. Also, clubfeet which had undergone treatment elsewhere were included. It is possible that some of these had partial correction. It is often difficult to distinguish incomplete correction from true relapses at long term followup. It is not uncommon to see undercorrected feet fitted with an FAO, which can then present with a stiff relapse at a later followup. Our incidence of clubfoot tenotomy was comparable to other series.3,15,30 Although children with bilateral clubfeet had a higher incidence of tenotomy, we did not specifically look at the relapse rate versus tenotomy in our study. The sample size is small. The lower number of children in the unilateral group and non-tenotomy groups could have led to bias in results. Only long term outcome studies with adequate numbers in each group will address the factors responsible for relapse and whether flexible or minor relapses have any functional consequences.
To conclude, relapse pattern observed after Ponseti regimen can be graded to plan further treatment. Early identification of relapses and early intervention will prevent major soft tissue surgery. A universal language of relapse pattern will allow comparison of results of intervention.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Ponseti IV. Current concepts review: Treatment of congenital clubfoot. J Bone Joint Surg Am. 1992;74:448–54. [PubMed] [Google Scholar]
- 2.Ponseti IV, Smoley EN. Congenital club foot: The results of treatment. J Bone Joint Surg Am. 1963;45:261–75. [Google Scholar]
- 3.Bor N, Coplan JA, Herzenberg JE. Ponseti treatment idiopathic clubfoot: Minimum 5-year followup. Clin Orthop Relat Res. 2009;467:1263–70. doi: 10.1007/s11999-008-0683-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owen RM, Kembhavi G. A critical review of interventions for clubfoot low and middle income countries: Effectiveness and contextual influences. J Pediatr Orthop. 2012;21:59–67. doi: 10.1097/BPB.0b013e3283499264. [DOI] [PubMed] [Google Scholar]
- 5.Ponseti IV. Relapsing clubfoot: Causes, prevention and treatment. Iowa Orthop J. 2000;22:55–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Chu A, Lehman WB. Persistent clubfoot deformity following treatment by the Ponseti method. J Pediatr Orthop. 2012;21:40–5. doi: 10.1097/BPB.0b013e32834ed9d4. [DOI] [PubMed] [Google Scholar]
- 7.Masrouha KZ, Morcuende JA. Relapse after tibialis anterior tendon transfer in idiopathic clubfoot treated by the Ponseti method. J Pediatr Orthop. 2012;32:81–4. doi: 10.1097/BPO.0b013e31823db19d. [DOI] [PubMed] [Google Scholar]
- 8.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86-A:22–7. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Lehman WB, Mohaideen A, Madan S, Scher DM, Van Bosse HJ, Iannacone M, et al. A method of early evaluation of Ponseti (Iowa) technique for the treatment of clubfoot. J Pediatr Orthop. 2003;12:134–40. doi: 10.1097/01.bpb.0000049579.53117.4a. [DOI] [PubMed] [Google Scholar]
- 10.Bouchoucha S, Smida M, Saı¨ed W, Safi H, Ammar C, Nessib MN, et al. Early results of the Ponseti method using the Steenbek foot abduction brace: A prospective study of 95 feet. J Pediatr Orthop B. 2008;17:134–8. doi: 10.1097/BPB.0b013e3282fa5f0d. [DOI] [PubMed] [Google Scholar]
- 11.Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89:487–93. doi: 10.2106/JBJS.F.00169. [DOI] [PubMed] [Google Scholar]
- 12.Bhaskar AR, Rasal S. Results of treatment of clubfoot by Ponseti's technique in 40 cases: Pitfalls and problems in the Indian scenario. Indian J Orthop. 2006;40:196–9. [Google Scholar]
- 13.Thacker MM, Scher DM, Sala DA, van Bosse HJ, Feldman DS, Lehman WB. Use of foot abduction orthosis following Ponseti casts: Is it essential? J Pediatr Orthop. 2005;25:225–8. doi: 10.1097/01.bpo.0000150814.56790.f9. [DOI] [PubMed] [Google Scholar]
- 14.Ponseti IV. Oxford, England: Oxford University Press; 1996. Congenital clubfoot: Fundamentals of treatment. [Google Scholar]
- 15.Hattori T, Ono Y, Kitakoji T, Iwata H. Effect of the Denis Browne splint in conservative treatment of congenital club foot. J Pediatr Orthop Br. 2003;12:59–62. doi: 10.1097/01.bpb.0000043722.21564.b5. [DOI] [PubMed] [Google Scholar]
- 16.Tindall AJ, Steinlechner CW, Lavy CB, Mannion S, Mkandawire N. Results of manipulation of idiopathic clubfoot deformity in malawi by orthopaedic clinical officers using the Ponseti method a realistic alternative for the developing world? J Pediatr Orthop. 2005;25:627–9. doi: 10.1097/01.bpo.0000164876.97949.6b. [DOI] [PubMed] [Google Scholar]
- 17.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Paediatrics. 2004;113:376–800. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 18.Boden RA, Nuttall GH, Paton RW. A 14-year longitudinal comparison study of two treatment methods in clubfoot: Ponseti versus traditional. Acta Orthop Belg. 2011;77:522–8. [PubMed] [Google Scholar]
- 19.Dobbs HB, Nunley R, Schoenecker P. Long term followup of patients with clubfoot treated with extensive soft tissue release. J Bone Joint Surg Br. 2009;91:949–54. [Google Scholar]
- 20.Hsu WK, Bhatia NN, Raskin A, Otsuka NY. Wound complications from idiopathic clubfoot surgery: A comparison of the modified Turco and the Cincinnati treatment method. J Pediatr Orthop. 2007;27:329–32. doi: 10.1097/BPO.0b013e3180340d86. [DOI] [PubMed] [Google Scholar]
- 21.Halanski MA, Davison JE, Huang JC, Walker CG, Walsh SJ, Crawford HA. Ponseti method compared with surgical treatment of clubfoot: A prospective comparison. J Bone Joint Surg Am. 2010;92:270–8. doi: 10.2106/JBJS.H.01560. [DOI] [PubMed] [Google Scholar]
- 22.Pirani S, Outerbridge HK, Sawatzky B, Stothers K. Sydney, Australia: Proceedings of the 21st SICOT World Congress; 1999. A reliable method of clinically evaluating a virgin clubfoot. [Google Scholar]
- 23.Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129–36. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 24.Dyer PJ, Davis N. The role of Pirani scoring system in the management of clubfoot by the Ponseti method. J Bone Joint Surg Br. 2006;88:1082–4. doi: 10.1302/0301-620X.88B8.17482. [DOI] [PubMed] [Google Scholar]
- 25.Chu A, Labar AS, Sala DA, van Bosse HJ, Lehman WB. Clubfoot classification: Correlation with Ponseti cast treatment. J Pediatr Orthop. 2010;30:695–9. doi: 10.1097/BPO.0b013e3181ec0853. [DOI] [PubMed] [Google Scholar]
- 26.Scher DM, Feldman DS, Van Bosse HJ, Sala DA, Lehman WB. Predicting the need for tenotomy in the Ponseti method of correction of clubfeet. J Pediatr Orthop. 2004;24:349–52. doi: 10.1097/00004694-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Goriainov V, Judd J, Uglow M. Does the Pirani score predict relapse in clubfoot. J Child Orthop. 2010;4:439–44. doi: 10.1007/s11832-010-0287-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porecha MM, Parmar DS, Chavda HR. Mid-term results of Ponseti method for the treatment of congenital idiopathic clubfoot- study of 67 clubfeet with mean five year followup (Open access publisher –Biomed Central) J Orthop Surg Res. 2011;6:3–7. doi: 10.1186/1749-799X-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dietz FR. Treatment of a recurrent clubfoot deformity after initial correction with the Ponseti technique. Instr Course Lect. 2006;55:625–9. [PubMed] [Google Scholar]
- 30.Jowett CR, Morcuende JA, Ramachandran M. Management of congenital talipes equinovarus using the Ponseti method: A systematic review. J Bone Joint Surg Br. 2011;93:1160–4. doi: 10.1302/0301-620X.93B9.26947. [DOI] [PubMed] [Google Scholar]
- 31.Staheli L. 3rd ed. USA: Global Help; 2009. Clubfoot: Ponseti Management. [Google Scholar]
- 32.Janicki JA, Wright JG, Weir S. A comparison of ankle foot orthoses with foot abduction orthoses to prevent recurrence following correction of idiopathic clubfoot by the Ponseti method. J Bone Joint Surg Br. 2011;93:700–4. doi: 10.1302/0301-620X.93B5.24883. [DOI] [PubMed] [Google Scholar]
- 33.George HL, Unnikrishnan PN, Garg NK, Sampath J, Bruce CE. Unilateral foot abduction orthosis: Is it a substitute for Denis Browne boots following Ponseti technique? J Pediatr Orthop B. 2011;20:22–5. doi: 10.1097/BPB.0b013e32833fb8a5. [DOI] [PubMed] [Google Scholar]
- 34.Ramírez N, Flynn JM, Fernández S, Seda W, Macchiavelli RE. Orthosis noncompliance after the Ponseti method for treatment of idiopathic clubfoot: A relevant problem that needs re-evaluation. J Pediatr Orthop. 2011;31:710–5. doi: 10.1097/BPO.0b013e318221eaa1. [DOI] [PubMed] [Google Scholar]


