Abstract
Objectives
To describe coping in mothers of adolescents with type 1 diabetes and to examine the association among mothers’ diabetes-related stress and coping strategies and maternal psychological distress (e.g., symptoms of anxiety and depression), adolescent adjustment (e.g., symptoms of depression, quality of life), diabetes-related family conflict, and glycemic control.
Methods
One hundred and eighteen mother-adolescent dyads completed measures of diabetes-related stress, coping, symptoms of anxiety and depression, quality of life, and family conflict. Data on glycemic control were collected from adolescents’ medical charts.
Results
Single/divorced mothers and mothers of color were significantly more likely to use disengagement coping strategies (e.g., avoidance) than White and married/partnered mothers. Mothers’ use of primary control coping (e.g., problem solving) and secondary control coping (e.g., acceptance) strategies was related to fewer symptoms of anxiety (r = −.51, −.39) and depression (r = −.32, −.37) and less family conflict (r = −.22, −.30, all p < .05). Mothers’ use of disengagement coping strategies was related to greater symptoms of anxiety (r = .30) and depression (r = .27, both p < .01). Further, secondary control coping was found to mediate the relationship between diabetes-related stress and maternal symptoms of anxiety and depression. Maternal coping was not significantly associated with adolescent outcomes.
Conclusions
The ways in which mothers of adolescents with type 1 diabetes cope with diabetes-related stress are associated with psychological distress and family conflict. By identifying and improving mothers’ coping through screening and targeted interventions, we may have the potential to improve both maternal and adolescent outcomes.
Keywords: coping, mothers, type 1 diabetes mellitus, adjustment
Type 1 diabetes (T1D) is one of the most common chronic diseases in childhood, affecting approximately 1 in 400 children, and the incidence is rising (1). The recommended treatment regimen is complex and demanding, including frequent daily blood sugar tests, multiple injections/boluses, monitoring carbohydrates and exercise to adjust insulin dose, and checking urine for ketones when necessary (2). Caregivers - especially mothers - report high levels of stress related to the burden of treatment management, and this stress is associated with increased risk for depression and anxiety (3). Maternal stress and depressive symptoms are linked with negative outcomes in adolescents, including deteriorating glycemic control, poorer quality of life, and greater depressive symptoms (4–6). Thus, mothers of youth with T1D need effective coping strategies for dealing with diabetes-related stress.
While fathers play an important role in diabetes management (7), mothers are typically the parents responsible for the majority of treatment management (8, 9). Mothers also experience greater stress than fathers related to the “constant vigilance” of caring for a child with diabetes (8, 10, 11). Commonly experienced stressors include food management, diabetes-related family conflict, insulin administration, and blood glucose monitoring (12). Mothers also report constantly worrying about their children’s blood sugar going too high or too low, long-term complications, and difficulty learning and mastering the complex treatment regimen (10). These high levels of diabetes-related stress are associated with increased risk for depression and anxiety (13), with rates of clinically significant symptoms frequently reported in 20–30% of mothers (14, 15), and ranging as high as 74% among parents of newly diagnosed children (8).
Based on the Transactional Stress and Coping Model (16), which views chronic illness as a stressor to which children and families attempt to adapt, the ways in which mothers cope with the stress of diabetes play an important role in both maternal and adolescent adjustment to the disease (see Figure 1). Mothers’ difficulty in coping with diabetes is related to maternal psychological and physical well-being (13), which are, in turn, related to adolescents’ quality of life, depressive symptoms, and glycemic control (4, 9). In fact, maternal depressive symptoms are one of the strongest predictors of poor outcomes in adolescents (5, 6, 17). A recent study found that caregiver strain was related to symptoms of anxiety and depression, which, in turn, mediated the relationship with adolescent adherence and glycemic control (18). Therefore, determining effective coping strategies for mothers of youth with T1D may improve outcomes in both mothers and adolescents.
Figure 1.
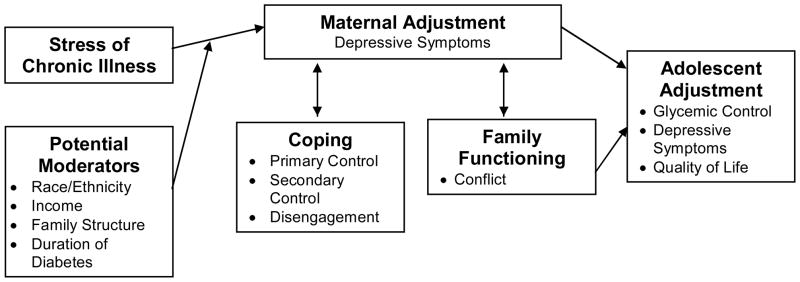
A proposed model for the risk and protective factors related to maternal and adolescent adjustment to chronic illness (adapted from the Transactional Stress and Coping Model, Thompson & Gustafson, 1996).
Despite the need to understand how mothers cope with stress related to their children’s diabetes, few studies have explicitly examined coping in this population. One study found that mothers of adolescents with T1D rated coping strategies such as talking to healthcare providers, reading more about the medical problem, and maintaining family stability as most helpful (19). Similarly, greater use of engagement or approach coping (e.g., problem solving) has been related to fewer symptoms of depression in mothers (20). Other studies have assessed coping with a single item (13) or asked mothers how well they coped with diabetes-related stress (14), without measuring their use of specific coping strategies. These studies provide initial support for the idea that ways in which mothers cope with the stress of diabetes management are associated with mothers’ psychological distress, but they did not examine connections between maternal coping and adolescent outcomes.
Demographic characteristics are also important to consider. For example, data from a national sample of children with T1D indicated that mothers of children of color and mothers from single-parents households experienced poorer psychological well-being (13). Single mothers also report greater pediatric parenting stress (11). Further, lower family income has been related to poorer coping resources in mothers of children with T1D (21). To our knowledge, however, previous studies have not examined demographic differences in maternal coping strategies, which could help to target screening efforts and interventions.
The purpose of the current study is to describe coping in mothers of adolescents with type 1 diabetes and how coping is related to maternal and child adjustment. Based on the literature, we hypothesized that mothers’ use of engagement coping would be related to fewer symptoms of anxiety and depression and to better adolescent adjustment. Finally, in line with the Transactional Stress and Coping Model, we tested whether coping mediated the relationship between diabetes-related stress and maternal psychological adjustment and family conflict.
Method
Participants
Adolescents were eligible for the study if they were between the ages of 10–16 years, were able to speak and read English, and had been diagnosed with T1D for at least six months. Mothers were eligible if they lived with the adolescent and were able to speak and read English. Of the 394 families approached, 98 were ineligible, 118 refused (most common reasons were time and distance), 60 expressed interest but were unable to schedule a visit, and 118 completed data. Demographic characteristics of the sample are described in Table 1.
Table 1.
Demographic Characteristics of the Sample (n = 118)
| Range | Mean | Standard Deviation | |
|---|---|---|---|
| Mother Age | 28–58 | 44.2 | 5.8 |
| Child Age | 10–16 | 12.8 | 2.0 |
| Duration of Diabetes | 0–14 | 4.9 | 3.6 |
| A1C | 5.4–12.9 | 7.6 | 1.1 |
| Mother Education | 4% < High School, 9% High School/GED, 18% Trade School, 40% College Graduate, 29% Advanced Degree | ||
| Marital Status | 25% Single/Divorced, 75% Married/Partnered | ||
| Annual Family Income | 9% < $40,000 | ||
| 51 % $40–80,000 | |||
| 66% > $80,000 | |||
| Child Gender | 46% female | ||
| Race/Ethnicity | 78% White, 6% Black, 3% Asian, 2% Biracial, 11% Hispanic | ||
| Therapy Type | 82% Injection, 18% Insulin Pump | ||
Procedure
In line with the protocol approved by Yale University’s Human Research Protection Program (Institutional Review Board), the study was described to mothers and adolescents during a routine visit to the outpatient diabetes clinic. If they were eligible, the mother and adolescent were invited to schedule a time to visit the laboratory, where, after giving consent/assent, they completed questionnaires and participated in a videotaped discussion of diabetes stress (not included in these analyses). The entire visit took approximately 90 minutes, and they were compensated for their time ($20 each). Clinical information (e.g., A1C) was collected from the adolescents’ medical records.
Measures
Mothers completed a demographics questionnaire, which asked about race/ethnicity, marital status, age and sex of child with T1D, mother’s relationship to the child (e.g., biological mother, foster mother), and annual family income. Clinical information regarding the child’s date of diagnosis and type of therapy (insulin pump vs. injections) was also provided by mothers5).
Maternal Stress and Coping was measured with the Responses to Stress Questionnaire (RSQ, 22). Mothers reported how often they experienced 10 items of diabetes-related stress (e.g., taking care of diabetes, frequently reminding adolescent to take care of him/herself), to yield a Total Stress Score (ranging from 0–30, higher scores indicate greater diabetes-related stress). Mothers then completed 57 items asking how they respond to these stressors. Confirmatory factor analyses (22, 23) support three separate coping factors on the RSQ: primary control engagement coping (problem solving, emotional modulation, emotional expression); secondary control engagement coping (positive thinking, cognitive restructuring, acceptance, distraction); and disengagement coping (avoidance, denial, wishful thinking). Internal consistency for the present study was .63 for total stress, .65 primary control coping, .65 for secondary control coping, and .65 for disengagement coping. To control for response bias and individual differences in base rates of item endorsement, proportion scores (i.e., type of coping in relation to total coping) were used for all analyses (22).
Maternal Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D, 24), a brief, self-report measure of depressive symptoms. A total score is calculated from 20 items and ranges from 0–60. Higher scores indicate more depressive symptoms, and a score of 16 suggests clinically significant symptoms. Mothers in our study who scored 16 or higher were evaluated for depression by a licensed clinical psychologist, and referrals were made as needed. Internal consistency for the current sample was .90.
Maternal symptoms of anxiety were measured with the State Trait Anxiety Inventory (STAI, 25). Mothers completed the 20-item State Anxiety scale, which asks about current symptoms of anxiety. Scores range from 20–80, and higher scores indicate greater symptoms of anxiety. Internal consistency for the current sample was .91.
Diabetes-related family conflict was measured with the Diabetes Responsibility and Conflict Scale (DRC, 26). This measure includes a scale that asks about the degree of diabetes-related conflict encountered by parent and child. Scores range from 15–75, and higher scores reflect more parent-child conflict. Internal consistency for the current sample was .83 for the mothers’ reports and .94 for adolescents’ reports. A composite score was created by summing the z-scores of maternal and adolescent reports of conflict, similar to other studies of diabetes-related family conflict (27).
Adolescents’ quality of life was measured with the Pediatric Quality of Life Inventory (28), developed to evaluate quality of life in children with chronic health conditions. Following recent recommendations (29), the 28 items of the Diabetes Module were summed to create a total diabetes-specific quality of life score; higher scores reflect better quality of life. Internal consistency for the current sample was 0.88.
Adolescent depressive symptoms were measured with the Child Depression Inventory (30). The CDI consists of 21 items, with scores ranging from 0–42; higher scores indicate higher current levels of depression. Scores ≥ 13 suggest clinical levels of depression, and adolescents in the current study who scored at or above this cutoff were evaluated for depression by a licensed clinical psychologist, with referrals made as needed. Internal consistency for the current sample was .90.
Glycemic control was measured with glycosylated hemoglobin (A1C). The glycosylation of the hemoglobin molecule provides objective criteria of metabolic control over the most recent 8–12 weeks, and A1C is routinely measured quarterly in patients with T1D (31). An A1C of <8% is considered acceptable control for school-age children and adolescents (32). Analyses were performed using the Bayer Diagnostics DCA2000® machine, which provides results in 6 minutes on a fingerstick blood sample (normal range = 4.2–6.3%). The reliability of this method is high, and control checks are typically run every two weeks. A1C data was collected from adolescents’ medical charts from the clinic visit closest to the completion of questionnaire data.
Data Analyses
Descriptive analyses were conducted using ANOVA to test for demographic differences in the use of the three categories of coping strategies (i.e., primary control coping, secondary control coping, and disengagement coping). Bivariate correlations were conducted to examine the associations among mothers’ diabetes-related stress and coping strategies and maternal psychological distress (i.e., symptoms of anxiety and depression), adolescent psychological adjustment (i.e., symptoms of depression, quality of life), diabetes-related family conflict, and glycemic control. To test coping as a mediator of diabetes-related stress and maternal psychological distress and family conflict, we conducted step-wise linear regression analyses, controlling for maternal race/ethnicity and marital status. With a sample of 118, we had power of .93 to detect an effect size of f2 = .10 or larger in multiple regression analysis. Sobel tests (33) were used to assess whether the mediation effects, or whether coping accounted for the relationship between the independent and dependent variables, were significant. Given that our data are cross-sectional, these analyses do not indicate a causal relationship between variables, and thus, the proposed mediational effects are considered exploratory.
Results
Maternal Psychological Distress
All of the mothers in our sample reported some diabetes-related stress on the RSQ; scores ranged from 5–22, with a mean total stress score of 12.4 (± 3.4). Approximately 18% of the mothers scored above the clinical cutoff for depression, with a mean score of 10.2 (± 8.3) on the CES-D. Approximately 13% of the mothers scored above the clinical cutoff for anxiety, with a mean score of 32.4 (± 9.3).
Demographic Differences in Coping
Analyses of variance were conducted to examine demographic differences in mothers’ use of the. Significant racial/ethnic differences emerged in the use of disengagement coping; mothers of color used significantly more disengagement coping strategies (mean = 14.1) than White mothers (mean = 12.2), F(1, 107) = 6.32, p = .013. A similar effect was found for marital status; single/divorced mothers used significantly more disengagement coping strategies (mean = 14.1) than married/partnered mothers (mean = 12.1), F(1, 109) = 8.35, p = .005. No demographic differences were found in the use of primary control or secondary control engagement coping strategies, and maternal coping was not related to child gender, maternal education, family income, or type of insulin therapy (pump vs. injection). Child age and duration of diabetes were not significantly related to maternal coping or any of the outcomes variables, so they were not included in further analyses.
Associations between Maternal Coping and Maternal and Adolescent Adjustment
Bivariate correlations indicate the associations among mothers’ diabetes-related stress and coping, maternal psychological distress, diabetes-related family conflict, adolescent adjustment, and glycemic control. As seen in Table 2, mothers’ reports of diabetes-related stress were significantly associated with their symptoms of depression (r = .25) and anxiety (r = .27, both p < .01), and family conflict (r = .30, p = .001) and secondary control coping (r = −.43, p < .001). Further, mothers’ use of primary control coping strategies was related to fewer symptoms of depression (r = −.32) and anxiety (r = −.51, both p < .001) and family conflict (r = −.22, p = .024). Similarly, mothers’ use of secondary control coping strategies was related to fewer symptoms of depression (r = −.37) and anxiety (r = −.39, both p < .001) and family conflict (r = −.30, p = .001). On the other hand, disengagement coping was related to greater symptoms of depression (r = .27) and anxiety (r = .30, both p < .005).
Table 2.
Descriptive Statistics and Correlations among Maternal Stress and Coping and Key Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. RSQ Total Stress M = 12.43 (3.43) |
-- | |||||||||
| 2. Primary Control Coping M = .23 (.03) |
−.14 | -- | ||||||||
| 3. Secondary Control Coping M = .29 (.04) |
−.43*** | .21* | -- | |||||||
| 4. Disengagement Coping M = .11 (.02) |
.13 | −.39*** | −.35*** | -- | ||||||
| 5. CES-D M = 10.15 (8.30) |
.25** | −.32*** | −.37*** | .27** | -- | |||||
| 6. STAI M = 32.36 (9.31) |
.27** | −.51*** | −.39*** | .30** | .72*** | -- | ||||
| 7. Family Conflict M = 0.00 (1.69) |
.30*** | −.22* | −.30*** | .15 | .20 | .34*** | -- | |||
| 8. CDI M = 5.28 (6.19) |
−.02 | −.03* | −.01 | .16 | .14 | .12 | .20* | -- | ||
| 9. PedsQL M = 83.66 (11.56) |
.08 | −.09 | .02 | −.09 | −.22* | −.06 | −.12 | −.66*** | -- | |
| 10. A1C M = 7.64 (1.12) |
−.04 | −.02 | −.00 | .03 | .09 | .03 | .43*** | .14 | −.11 | -- |
Note. RSQ = Responses to Stress Questionnaire; CES-D = Center for Epidemiologic Studies of Depression; STAI = State Trait Anxiety Inventory; CDI = Children’s Depression Inventory; PedsQL = Diabetes-Specific Pediatric Quality of Life. Family Conflict represents summed z-scores of parent- and adolescent-reports.
p<.05.
p<.01.
p<.001
Contrary to our hypothesis, maternal coping was not significantly related to any adolescent outcomes. However, maternal depressive symptoms were associated with poorer adolescent quality of life (r = −.22, p = .023). In addition, family conflict was related to greater depressive symptoms in adolescents (r = .20, p = .032) and, notably, to glycemic control (r = .43, p < .001).
Tests of Coping as a Mediator
Given the significant correlation between diabetes-related stress and secondary control coping, we conducted step-wise linear regression analyses to test coping as a mediator of diabetes-related stress and maternal psychological distress. Demographic variables (maternal race/ethnicity and marital status) were entered in the first step, total diabetes-related stress (as reported by mothers on the RSQ) was entered in the second step, and secondary control coping was entered in the third step. As seen in Table 3, the model predicting maternal depressive symptoms was significant, explaining 14% of the variance in depressive symptoms. Mothers’ use of secondary control coping strategies partially mediated the relationship between diabetes-related stress and depressive symptoms (see Figure 2). When coping was added to the model, the beta value for maternal depressive symptoms decreased from 0.20 to 0.04. In addition, the Sobel test for mediation (33) was significant (z = 2.88, p = .004). Similarly, the model predicting maternal symptoms of anxiety was significant, explaining 17% of the variance in symptoms. Secondary control coping also partially mediated the relationship between diabetes-related stress and symptoms of anxiety (Figure 3), with the beta value for stress decreasing from 0.23 to 0.06; the Sobel test was also significant (z = 2.83, p = .005).
Table 3.
Hierarchical Linear Regressions Predicting Maternal Psychological Distress and Family Conflict
| Predictor | CES-D
|
STAI
|
Family Conflict
|
|||
|---|---|---|---|---|---|---|
| ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Step 1 | .05 | .07* | .12*** | |||
| Race | .16 | .02 | −.10 | |||
| Marital Status | −.17 | −.26** | −.33*** | |||
| Step 2 | .04* | .05* | .06** | |||
| Diabetes-Related Stress | .20* | .23* | .25** | |||
| Step 3 | .09*** | .09** | .05* | |||
| Secondary Control Coping | −.34*** | −.34** | −.25* | |||
| Total R2 | .14*** | .17*** | .21*** | |||
Note. CES-D = Center for Epidemiologic Studies Depression Scale; STAI = State Trait Anxiety Inventory. β = standardized beta.
p< .05.
p< .01.
p< .001.
Figure 2.
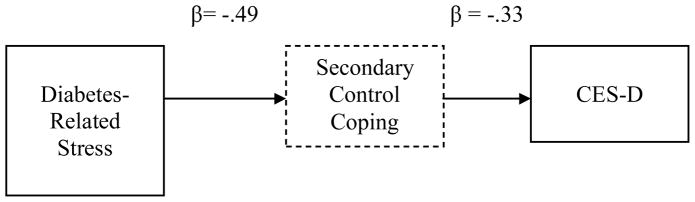
Secondary Control Coping as a Mediator of Diabetes-Related Stress and Maternal Depressive Symptoms. Standardized coefficients are presented for each step in this pathway. The model controlled for maternal race/ethnicity and marital status.
Figure 3.
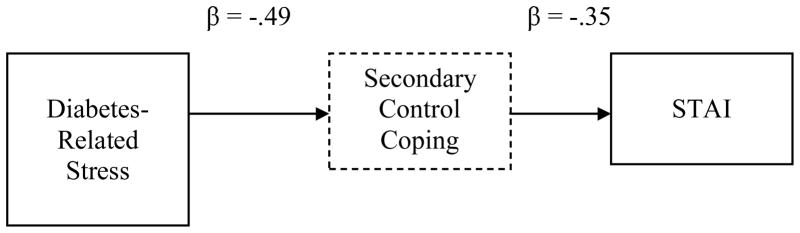
Secondary Control Coping as a Mediator of Diabetes-Related Stress and Maternal Symptoms of Anxiety. Standardized coefficients are presented for each step in this pathway. The model controlled for maternal race/ethnicity and marital status.
Finally, we tested secondary control coping as a mediator of the relationship between diabetes-related stress and family conflict. The model predicting family conflict was significant, explaining 21% of the variance in conflict. Secondary control coping partially mediated the relationship between diabetes-related stress and family conflict (see Figure 4), with the beta value for stress decreasing from 0.25 to 0.14; the Sobel test was also significant (z = 2.38, p = .017).
Figure 4.
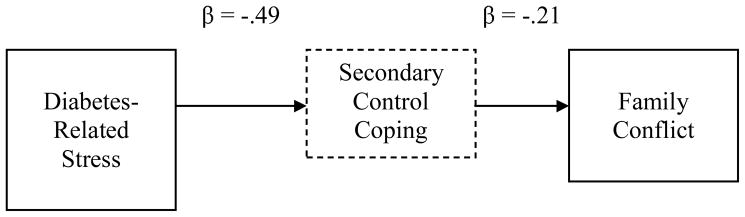
Secondary Control Coping as a Mediator of Diabetes-Related Stress and Family Conflict. Standardized coefficients are presented for each step in this pathway. The model controlled for maternal race/ethnicity and marital status.
Discussion
The current study describes specific coping strategies reported by mothers of adolescents with T1D. Mothers in our sample exhibited clinically significant levels of distress similar to the levels found in other studies that have examined depression and anxiety in mothers of children with T1D (4, 34). Mothers’ coping strategies were significantly associated with maternal psychological distress and family conflict, but not with adolescent adjustment. Further, mothers’ use of secondary control coping strategies, such as acceptance and distraction, mediated the relationship between diabetes-related stress and psychological distress, and the relationship between diabetes-related stress and family conflict.
The current study is one of the first to examine demographic differences in maternal coping in this population. Mothers’ coping strategies were not related to maternal education, family income, child sex, age, duration of diabetes, or therapy type. However, important differences emerged in the use of disengagement coping related to race/ethnicity and marital status. First, mothers of color reported using more disengagement coping strategies than White mothers. This racial/ethnic difference may reflect cultural differences in coping. Evidence suggests that Black and Latina women are more likely to have fatalistic attitudes toward health problems (35), which may result in greater use of disengagement coping strategies, such as avoidance or wishful thinking (36). Similarly, single/divorced mothers reported using greater disengagement coping than married/partnered mothers. Single mothers may not have the emotional resources or support needed to use more adaptive coping strategies (11). These findings suggest that single and mothers and mothers of color may need extra support in identifying and using adaptive coping strategies.
Further, results from the current study support that secondary control coping, or attempts to adapt to the stressor, may mediate the relationship between diabetes-related stress and maternal symptoms of depression and anxiety. Control-based models of coping (22) suggest that the most adaptive coping strategies are the strategies matched to the individual’s level of perceived control. Because the stress of T1D is largely uncontrollable for mothers of adolescents, who may not be able to monitor diabetes management as closely during this developmental period of increasing independence, the use of secondary control coping strategies, such as acceptance and positive thinking, may be most adaptive. This finding is in line with other studies showing that women coping with breast cancer, another uncontrollable stressor, had significantly fewer symptoms of anxiety and depression when using secondary control coping strategies (37).
We did not find a direct connection between maternal coping and adolescents’ psychosocial adjustment or glycemic control. This result is similar to a study of mothers of young children with diabetes, in which mothers’ coping was not related to glycemic control (38). Mothers’ coping may have an indirect effect on adolescents’ outcomes, however, through factors such as maternal depressive symptoms and family conflict. Indeed, we found a significant association between greater family conflict and poorer glycemic control in our sample. We did not find a direct association between maternal and child distress found in other studies (4, 39), perhaps because our sample was older (adolescents versus school-age or younger children) and was in relatively good glycemic control. Still, by understanding and improving mothers’ coping, we may have an indirect positive effect on adolescent outcomes, by reducing mothers’ symptoms of depression and anxiety.
Limitations
The current study is limited by the cross-sectional design, which does not allow for true tests of mediation (40); thus, the mediation analyses must be considered exploratory. Further, our sample was in relatively good glycemic control, which may limit the generalizability of our findings. Similarly, the families in our sample had fairly high socioeconomic status and income, which may also affect generalizability. Additional economic stress may impact the way that mothers cope with their adolescents’ diabetes (21). Further studies are needed to replicate these findings in a more diverse sample.
Conclusions
While the current study confirms the need to support mothers who are coping with stress related to caring for adolescents with T1D, more work is needed in this area. Maternal coping resources and psychological functioning have been related to diabetes management (18, 21), suggesting that future studies should examine maternal coping and psychological distress in relation to measures of adherence. Longitudinal studies are also needed to tease out the direction of effects between maternal stress and family conflict. Further, few interventions have focused on relieving parental stress and depressive symptoms in this population, and these interventions have typically targeted parents of young children. For example, one intervention provided mothers of young children with social support from peers, but it did not significantly improve maternal concern or worry (41). Another pilot intervention for parents of young children with T1D successfully reduced pediatric parenting stress, but it did not have an effect on parental symptoms of anxiety or depression (42). What are still needed are interventions for at-risk mothers aimed at reducing symptoms of depression and anxiety by teaching the most adaptive coping strategies.
Results highlight the need to identify and support effective coping strategies for mothers of adolescents with T1D, which may help to reduce symptoms of depression and anxiety. Specifically, secondary control engagement coping strategies, such as acceptance, positive thinking, and distraction could be taught to mothers to improve their ability to manage diabetes-related stress and reduce their symptoms of anxiety and depression. These results further support the need to screen mothers who may be at increased risk for depression and anxiety (6). By helping mothers to effectively manage diabetes-related stress, we may be able to improve both maternal and adolescent outcomes.
Acknowledgments
This research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases [K23 NK088454] and the National Center for Research Resources (UL1 RR024139]. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Contributor Information
Sarah S. Jaser, School of Nursing, Yale University
Rebecca Linsky, School of Nursing, Yale University.
Margaret Grey, School of Nursing, Yale University.
References
- 1.Liese AD. The burden of diabetes mellitus among US youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–8. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes - 2012. Diabetes Care. 2012;35:S11– S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whittemore R, Jaser SS, Chao A, et al. Psychological experience of parents of children with type 1 diabetes: A systematic mixed-studies review. Diabetes Educ. 2012;38:562–79. doi: 10.1177/0145721712445216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaser SS, Whittemore R, Ambrosino J, et al. Mediators of depressive symptoms in children with type 1 diabetes and their mothers. J Pediatr Psychol. 2008;33:509–19. doi: 10.1093/jpepsy/jsm104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kovacs M, Goldston D, Obrosky DS, et al. Psychiatric disorders in youth with IDDM: Rates and risk factors. Diabetes Care. 1997;20:36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- 6.Cameron FJ, Northam EA, Ambler GR, et al. Routine psychological screening in youth with type 1 diabetes and their parents: A notion whose time has come? Diabetes Care. 2007;30:2716–24. doi: 10.2337/dc07-0603. [DOI] [PubMed] [Google Scholar]
- 7.Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. J Pediatr Psychol. 2006;31:501–11. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]
- 8.Streisand R, Mackey ER, Elliot BM, et al. Parental anxiety and depression associated with caring for a child newly diagnosed with type 1 diabetes: opportunities for education and counseling. Patient Educ Couns. 2008;73:333–8. doi: 10.1016/j.pec.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Kovacs M, Iyengar S, Goldston D, et al. Psychological functioning among mothers of children with insulin-dependent diabetes mellitus: A longitudinal study. J Consult Clin Psychol. 1990;58:189–95. doi: 10.1037//0022-006x.58.2.189. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan-Bolyai S, Deatrick J, Gruppuso P, et al. Constant vigilance: Mothers’ work parenting young children with type 1 diabetes. J Pediatr Nurs. 2003;18:21–9. doi: 10.1053/jpdn.2003.4. [DOI] [PubMed] [Google Scholar]
- 11.Hansen JA, Weissbrod C, Schwartz DD, et al. Paternal involvement in pediatric Type 1 diabetes: fathers’ and mothers’ psychological functioning and disease management. Fam Syst Health. 2012;30:47–59. doi: 10.1037/a0027519. [DOI] [PubMed] [Google Scholar]
- 12.Beveridge RM, Berg CA, Wiebe DJ, et al. Mother and adolescent representations of illness ownership and stressful events surrounding diabetes. J Pediatr Psychol. 2006;31:818–27. doi: 10.1093/jpepsy/jsj094. [DOI] [PubMed] [Google Scholar]
- 13.Streisand R, Mackey ER, Herge W. Associations of parent coping, stress, and well-being in mothers of children with diabetes: examination of data from a national sample. Matern Child Health. 2010;14:612–7. doi: 10.1007/s10995-009-0497-7. [DOI] [PubMed] [Google Scholar]
- 14.Jaser SS, Whittemore R, Ambrosino JM, et al. Coping and Psychosocial Adjustment in Mothers of Young Children With Type 1 Diabetes. Child Health Care. 2009;38:91– 106. doi: 10.1080/02739610902813229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiebe DJ, Gelfand D, Butler JM, et al. Longitudinal associations of maternal depressive symptoms, maternal involvement, and diabetes management across adolescence. J Pediatr Psychol. 2011;36:837–46. doi: 10.1093/jpepsy/jsr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson RJ, Gustafson KE. Adaptation to Chronic Childhood Illness. Washington, DC: American Psychological Association; 1996. [Google Scholar]
- 17.Butwicka A, Zulepa A, Fendler W, et al. Maternal depressive symptoms predict acute hospitalization among children with type 1 diabetes. Pediatr Diabetes. doi: 10.1111/pedi.12010. in press. [DOI] [PubMed] [Google Scholar]
- 18.Carcone A, Ellis D, Naar-King S. Linking caregiver strain to diabetes illness management and health outcomes in a sample of adolescents in chronically poor metabolic control. J Dev Behav Pediatr. 2012;33:343–51. doi: 10.1097/DBP.0b013e31824eaac8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konradsdottir E, Svavarsdottir EK. How effective is a short-term educational and support intervention for families of an adolescent with type 1 diabetes? J Spec Pediatr Nurs. 2011;16:295–304. doi: 10.1111/j.1744-6155.2011.00297.x. [DOI] [PubMed] [Google Scholar]
- 20.Blankfeld DF, Holahan CJ. Family support, coping strategies, and depressive symptoms among mothers of children with diabetes. J Fam Psychol. 1996;10:173–9. [Google Scholar]
- 21.Frey MA, Ellis D, Templin T, et al. Diabetes management and metabolic control in school-age children with type 1 diabetes. Child Health Care. 2006;35:349–63. [Google Scholar]
- 22.Connor-Smith JK, Compas BE, Wadsworth ME, et al. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. J Consult Clin Psychol. 2000;68:976–92. [PubMed] [Google Scholar]
- 23.Compas BE, Boyer MC, Stanger C, et al. Latent variable analysis of coping, anxiety/depression, and somatic symptoms in adolescents with chronic pain. J Consult Clin Psychol. 2006;56:405–11. doi: 10.1037/0022-006X.74.6.1132. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 25.Spielberg CD. Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 26.Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38(Supplement 2):28A. [Google Scholar]
- 27.Wysocki T, Harris MA, Buckloh LM, et al. Randomized Trial of Behavioral Family Systems Therapy for Diabetes: Maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–60. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]
- 28.Varni JW, Burwinkle TM, Jacobs JR, et al. The PedsQL in type 1 and type 2 diabetes: Reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and Type 1 Diabetes Module. Diabetes Care. 2003;26:631–7. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- 29.Nansel TR, Weisberg-Benchell J, Wysocki T, et al. Quality of life in children with type 1 diabetes: a comparison of general and diabetes-specific measures and support for a unitary diabetes quality-of-life construct. Diabetic Med. 2008;25:1316–23. doi: 10.1111/j.1464-5491.2008.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacol Bull. 1985;21:995–8. [PubMed] [Google Scholar]
- 31.DCCT Research Group. The Diabetes Control and Complications Trial: Design and methodologic implications for the feasibility phase. Diabetes. 1986;35:530–45. [PubMed] [Google Scholar]
- 32.Silverstein JH, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes. Diabetes Care. 2005;28:184–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 33.Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- 34.Eckshtain D, Ellis DA, Kolmodin K, et al. The effects of parental depression and parenting practices on depressive symptoms and metabolic control in urban youth with insulin dependent diabetes. J Pediatr Psychol. 2010;35:426–35. doi: 10.1093/jpepsy/jsp068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shelton RC, Goldman RE, Emmons KM, et al. An investigation into the social context of low-income, urban Black and Latina women: implications for adherence to recommended health behaviors. Health Educ Behav. 2011;38:471–81. doi: 10.1177/1090198110382502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roesch SC, Weiner B. A meta-analytic review of coping with illness: Do causal attributions matter? J Psychosom Res. 2001;50:205–19. doi: 10.1016/s0022-3999(01)00188-x. [DOI] [PubMed] [Google Scholar]
- 37.Compas BE, Beckjord E, Agocha B, et al. Measurement of coping and stress responses in women with breast cancer. Psychooncology. 2006;15:1038–54. doi: 10.1002/pon.999. [DOI] [PubMed] [Google Scholar]
- 38.Stallwood L. Influence of caregiver stress and coping on glycemic control of young children with diabetes. J Pediatr Health Care. 2005;19:293–300. doi: 10.1016/j.pedhc.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Hilliard ME, Monaghan M, Cogen FR, et al. Parent stress and child behaviour among young children with type 1 diabetes. Child Care Hlth Dev. 2011;37:224–32. doi: 10.1111/j.1365-2214.2010.01162.x. [DOI] [PubMed] [Google Scholar]
- 40.Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychol Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- 41.Sullivan-Bolyai S, Bova C, Leung K, et al. Social support to empower parents (STEP): An intervention for parents of young children newly diagnosed with type 1 diabetes. Diabetes Educ. 2010;36:88–97. doi: 10.1177/0145721709352384. [DOI] [PubMed] [Google Scholar]
- 42.Monaghan M, Hilliard ME, Cogen FR, et al. Supporting parents of very young children with type 1 diabetes: Results from a pilot study. Patient Educ Couns. 2011;82:271–4. doi: 10.1016/j.pec.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


