Abstract
Chronic diarrhea is defined as passing watery stools that lasts for more than 2 weeks. Persistent diarrhea belongs to chronic diarrhea and is a chronic episode of diarrhea of infectious etiology. The etiology of chronic diarrhea is varied. It is important to consider the child's age and clinical manifestations with alarm signals for an application of proper treatments to children with chronic diarrhea. Vicious cycle is present in chronic diarrhea and nutritional rehabilitation can break the vicious cycle of chronic diarrhea and is one of the main one thing among treatments. We should know the exact concept of chronic diarrhea and provide appropriate treatments according to etiologies of chronic diarrhea.
Keywords: Chronic diarrhea, Child, Nutrition
INTRODUCTION
Diarrhea is the excessive loss of fluids and electrolytes in the stool [1]. When the duration of diarrhea lasts more than 14 days, it is defined as chronic and persistent diarrhea. Diarrhea is the second leading cause of death in younger children less than 5 years of age in the world [2]. We try to examine the concepts and treatments of chronic diarrhea in children though this article.
THE CONCEPTS OF CHRONIC DIARRHEA
According to the volume, diarrhea is defined as loose stools of >10 mL/kg/day in infants and >200 g/24 hr in older children [1]. It is difficult to accurately measure the volume of the stool in clinical environment. Therefore, diarrhea may be defined as the passage of ≥3 watery stools per day in the United Nations International Children's Emergency Fund and the World Health Organization (WHO) [2,3]. However, the frequency and consistency of stool passage is affected by age, diet, and medication. Weaver [4] described that one bowel action per day, adult stool passage pattern, is achieved by 4 years, that is to say that infants and early children normally has a greater stool frequency than adults. It is not right to make a diagnosis of diarrhea through the frequency of stool. To make an accurate diagnosis of diarrhea, we should consider diarrhea symptom with nutritional state and the presence of dehydration.
To be more exact, the concepts of 'persistent diarrhea' and 'chronic diarrhea' are different. Persistent diarrhea is an episode of diarrhea of infectious etiology, which develops acutely but continues for more than 14 days [5]. Chronic diarrhea is defined as diarrhea that lasts for more than 14 day and is usually not associated with only infectious cause, and associated with various causes and malabsorption [5]. Persistent diarrhea is included in a big category of chronic diarrhea. Although others use a diagnostic cut off of 4 weeks, most physicians agree that 14 days of diarrhea duration meets a diagnosis criteria for chronic diarrhea [6]. Chronic diarrhea, lasting more than 14 days, is sure to bring about weight loss, dehydration, and nutritional impairment. The patients who have had prolonged watery stool with weight loss should be differentiated from normal frequent loose stool, it is difficult to differentiate between chronic diarrhea and normal frequent loose stool not only in parents but also even in physicians, especially in infants who have normal frequent loose stool. Hwang et al. [7] recommended the stool amount scoring system using the mother's hand for easily differentiating between normal frequent loose stool and diarrhea with dehydration and nutritional impairments in children on clinical circumstance. An accurate diagnosis and the proper treatments are very important because chronic diarrhea effects physical and psychological development in children.
EPIDEMIOLOGY AND CAUSE OF CHRONIC DIARRHEA
According to an announcement of WHO, 13.2% of all childhood deaths were caused by diarrhea and the worldwide prevalence of chronic diarrhea ranges from 3 to 20% [6]. Though worldwide incidence of diarrhea has not decreased, the mortality due to diarrhea is decreasing. These changes are caused by development of vaccine (rotavirus), nutritional states, and medical substance [8].
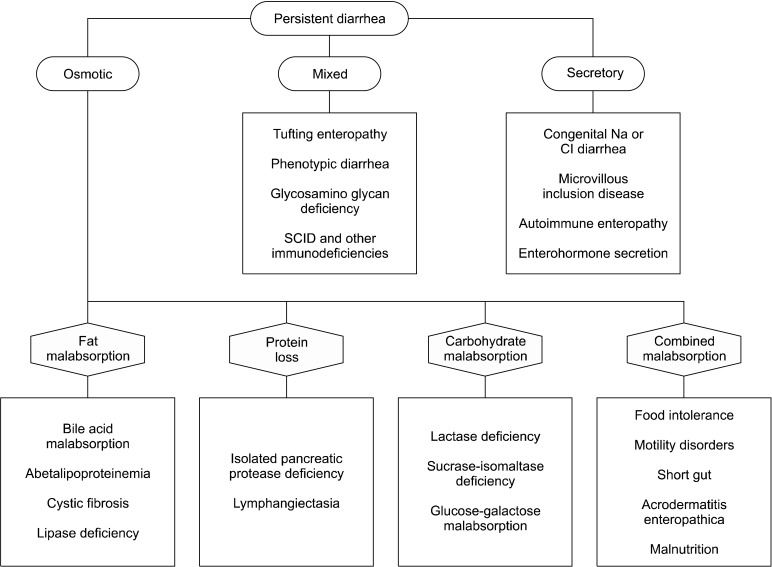
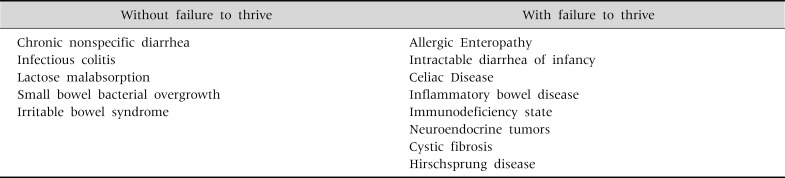
The causes of chronic diarrhea are divided into infectious and noninfectious etiologies. Furthermore, others classify chronic diarrhea according to pathophysiology, and the presence or absence of failure to thrive (Fig. 1, Table 1). The most frequent cause of chronic diarrhea is enteric infection in both in developing and industrialized countries. However, incidence of autoimmune enteropathy or inflammatory based diseases is increasing in the contrast, and incidence of infection is decreasing in developed country.
Fig. 1.
Etiologies of persistent diarrhea according to its pathophysiology. SCID: severe combined immunodeficiency. Adapted from Walker's pediatric gastrointestinal disease: physiology, diagnosis, management. 5th ed. Hamilton: BC Decker Inc., 2008:265-339 [10].
Table 1.
Causes of Chronic Diarrhea according to Presence or Absence of Failure to Thrive
Adapted from the article of Zella and Israel. Pediatr Rev 2012;33:207-17 [6].
Chronic nonspecific diarrhea (CNSD) is the most common cause of chronic diarrhea during the period from 1 to 3 years of age [6]. Patients who have CNSD pass stools only during waking periods and keep healthy state without weight loss and nutritional deficits [6]. The causes of CNSD are increased intestinal motility and osmotic effects in GI tract, due to solutes that are high in carbohydrate content.
Chronic diarrhea in early infant periods has the characteristics of high mortality and morbidity, so some physicians had denominated a severe chronic diarrhea in early infant periods as 'intractable diarrhea in infancy' (IDI). IDI defined as a severe chronic diarrhea associated with malnutrition and a high mortality in spite of an active treatment [9]. IDI was originally described by Avery et al as a diarrhea that lasts for more than 2 weeks, without an infectious etiology, starting in the first 3 months of age, and showing high mortality rate [10]. IDI are broadly divided into two groups: 1) without villous atrophy and 2) with villous atrophy [5]. Microvillous inclusion disease, tufting enteropathy, and autoimmune enteropathy have with villous atrophy. Congenital transport defects (congenital chloridorrhea, congenital sodium diarrhea), congenital glucose-galactose malabsorption are not shown villous atrophy. Infants with microvillous inclusion disease are shown with severe watery diarrhea (250 to 300 mL/kg/day) since the baby was born [11].
APPROACH TO THE CHILD WITH CHRONIC DIARRHEA
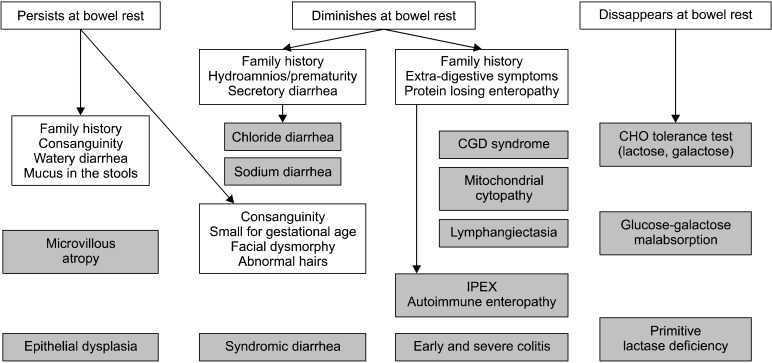
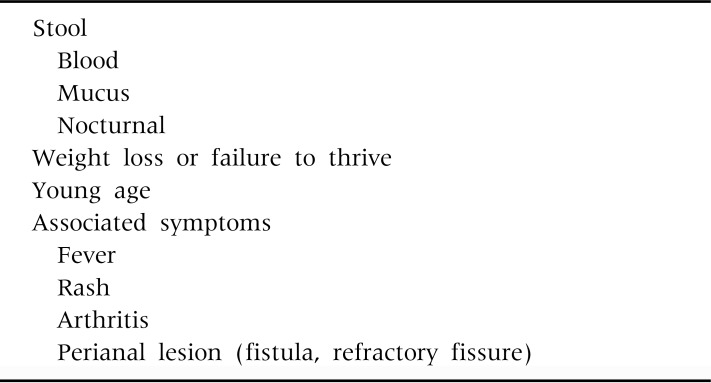
The approach to a child presenting with chronic diarrhea should be consisted of a careful history taking and physical examination at first [11]. Also, we assess the type of diarrhea (osmotic, secretory, and fatty), the severity of diarrhea, and the presence of associated symptoms. A dietary history and the child's growth chart should be obtained at the first visit, because this information allows for a differential diagnosis of CNSD and others diseases. A method of making differential diagnosis of being shown protracted diarrhea in infancy can be classified into according to the response on a bowel rest (Fig. 2) [10]. If the child has red flags or warning signals (Table 2), strongly suggest a specific organic cause [11].
Fig. 2.
Diagnostic algorithm in onset of neonatal severe diarrhea. CGD: chronic granulomatous disease, CHO: carbohydrate, IPEX: immunodysregulation, polyendocrinopathy, enteropathy, and X-linked syndrome. Adapted from Walker's pediatric gastrointestinal disease: physiology, diagnosis, management. 5th ed. Hamilton: BC Decker Inc., 2008:265-339 [10].
Table 2.
Red Flags or Warning Signals in the Patient with Chronic Diarrhea
Modified from Pediatric gastrointestinal and liver disease. 4th ed. Philadelphia: Saunders Elsevier, 2011:106-18 [11].
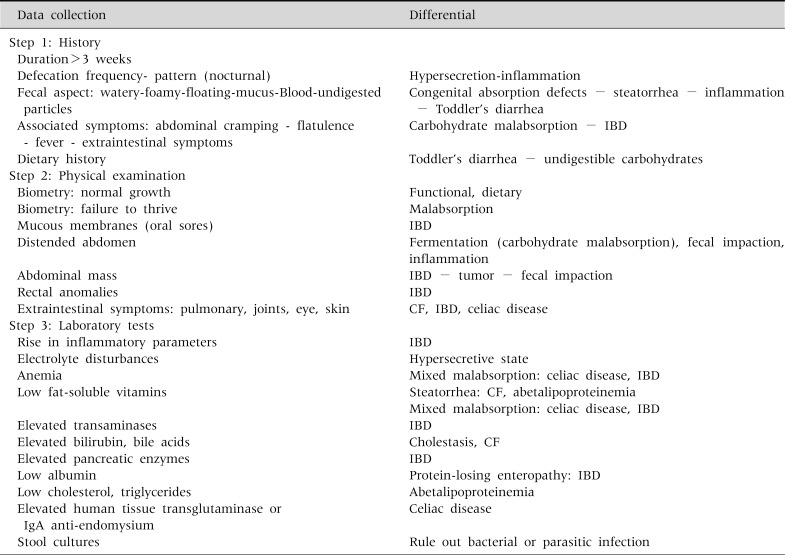
To sum it up, initial assessments of chronic diarrhea consist of 1) history taking, 2) physical examination, and 3) laboratory tests (Table 3). Pediatric gastroenterologists have a merit, which is a point of being able to perform endoscopic biopsy. Therefore, they can directly observe gastrointestinal (GI) tract and acquire GI mucosa in a child with being suspected of enteropathy or shown unexplained chronic diarrhea.
Table 3.
Initial Assessment of Chronic Diarrhea
IBD: inflammatory bowel disease, CF: cystic fibrosis. Adapted from Pediatric gastrointestinal and liver disease. 4th ed. Philadelphia: Saunders Elsevier, 2011:106-18 [11].
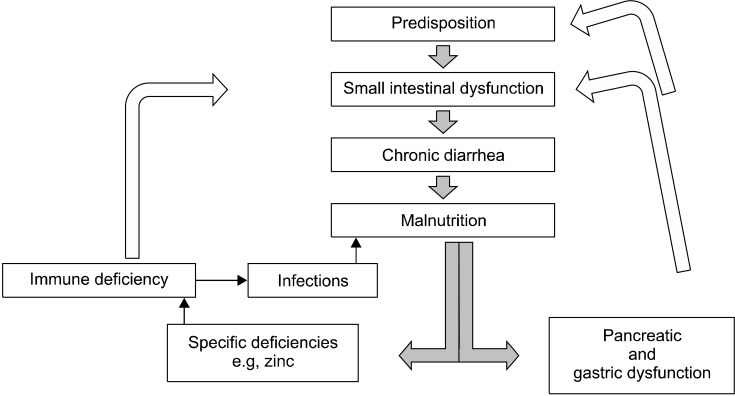
TREATMENT OF CHRONIC DIARRHEA
Identifying a specific cause of chronic diarrhea by a systemic approach is more important because it can provide the most suitable therapy and give a good prognosis [11]. The most important triggering factor of persistent diarrhea or chronic diarrhea is an acute diarrhea illness caused by enteric infection [3]. Especially, malnutrition caused by diarrhea associated with enteric infection is the most etiology of persistent diarrhea in developing countries. A vicious cycle is present not only functional constipation but also persistent diarrhea (Fig. 3). Malnutrition is an important etiology of persistent diarrhea and is associated with destruction of the intestinal barrier and villus atrophy [12].
Fig. 3.
The vicious cycle in chronic diarrhea.
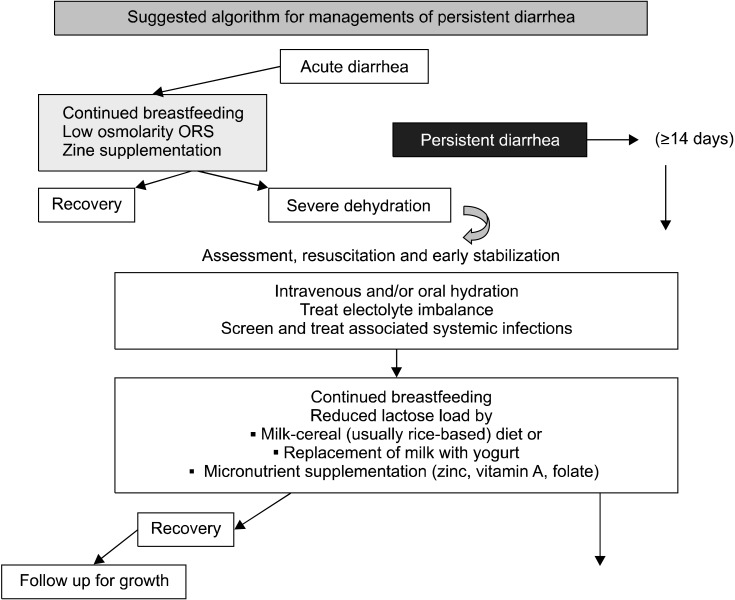
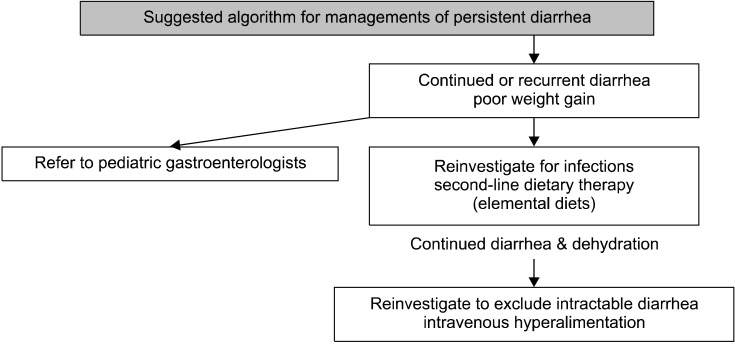
Treatments of chronic diarrhea are largely composed of nutritional rehabilitation, elimination diet, general supportive care, and drugs [1]. Nutritional rehabilitation has a general beneficial effect on patient's intestinal function, immune response, and patient's overall condition. Therefore, nutritional rehabilitation can break the vicious cycle of chronic diarrhea and is one of the main treatments for chronic diarrhea. Several nutrients and microelements effect on the regulation of intestinal epithelial proliferation, differentiation, apoptosis, and migration [12]. The enteric infection by common cause in chronic diarrhea induces secondary lactase deficiency resulting from mucosal injury of small intestine. Thus, WHO recommends a lactose-free diet preferentially should be started in all children with chronic diarrhea [1]. A lactose-free diet include specialized formulas and traditional diets in developing countries. Many reports which are shown efficacy on diarrheal illness using lactose free formula, yogurt, and other traditional diet had been published [13-17]. Especially, de Mattos et al. [17] claimed that yogurt-based diet is recommended as the first choice for the nutritional management of a mild to moderate persistent diarrhea. A cheap and an easily available yogurt-based diet can be used in mild chronic diarrhea illness of uncomplicated and without enteropathy. Bhutta et al. [18] suggested algorithm for the diagnosis and management of persistent diarrhea (Fig. 4 and 5).
Fig. 4.
The algorithm for managements of chronic diarrhea. ORS: oral rehydration solution.
Fig. 5.
The algorithm for managements of chronic diarrhea.
Elimination diet is considered when allergic enteropathy is induced by a cow's milk protein or soy protein. The degree of elimination depends on the severity of symptoms. Cow's milk protein hydrolysate formula is recommended in less severe case, but amino-acid-based formula is started in severely compromised infant if breastfeeding is not possible [1,19,20].
Micronutrient and vitamin are formed on a part of managements of chronic diarrhea. The usefulness of particularly zinc in acute and persistent diarrhea has been reported [21]. Zinc stimulates immune response, promotes ion absorption, and restores tight junction and epithelial proliferation [1].
Drug therapy includes antibiotics for bacterial diarrhea, immune suppressive agents for autoimmune enteropathy, and drugs that can inhibit fluid loss and promote cell growth [1].
Severe and protracted diarrhea (intractable diarrhea of infancy) often requires parenteral nutrition and some oral foods for a trophic effect on the small bowel mucosa [11]. Despite aggressive and specific nutritional supports, many of these infants require small bowel transplantation.
CONCLUSION
Chronic diarrhea is a major problem in pediatric patients because it induces malnutrition, general developmental defects, and an extremely death. Thus, it is important to make an accurate diagnosis, find definite etiologies, and apply proper treatments.
References
- 1.Kliegman RM, Stanton BF, St. Geme JW, 3rd, Schor NF, Behrman RE. Nelson textbook of pediatics. 19th ed. Philadelphia: Saunders Elsevier; 2011. pp. 1339–1346. [Google Scholar]
- 2.Wardlaw T, Salama P, Brocklehurst C, Chopra M, Mason E. Diarrhoea: why children are still dying and what can be done. Lancet. 2010;375:870–872. doi: 10.1016/S0140-6736(09)61798-0. [DOI] [PubMed] [Google Scholar]
- 3.Bhutta ZA, Ghishan F, Lindley K, Memon IA, Mittal S, Rhoads JM Commonwealth Association of Paediatric Gastroenterology and Nutrition. Persistent and chronic diarrhea and malabsorption: Working Group report of the second World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2004;39(Suppl 2):S711–S716. doi: 10.1097/00005176-200406002-00019. [DOI] [PubMed] [Google Scholar]
- 4.Weaver LT. Bowel habit from birth to old age. J Pediatr Gastroenterol Nutr. 1988;7:637–640. doi: 10.1097/00005176-198809000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Mathai J, Raju B, Bavdekar A Pediatric Gastroenterology Chapter, Indian Academy of Pediatrics. Chronic and persistent diarrhea in infants and young children: status statement. Indian Pediatr. 2011;48:37–42. doi: 10.1007/s13312-011-0018-9. [DOI] [PubMed] [Google Scholar]
- 6.Zella GC, Israel EJ. Chronic diarrhea in children. Pediatr Rev. 2012;33:207–217. doi: 10.1542/pir.33-5-207. [DOI] [PubMed] [Google Scholar]
- 7.Hwang JB, Kang KJ, Lee JJ, Kim AS. What is the 'objective' differential factor of diarrhea in infancy?: Normal state versus diarrheal illness in infants with chronic frequent and loose stool. Korean J Pediatr. 2010;53:1006–1011. doi: 10.3345/kjp.2010.53.12.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee KS, Lee JH. Clinical applications and limitations of a special formula for diarrhea in children. J Korean Med Assoc. 2012;55:551–561. [Google Scholar]
- 9.Walker-Smith JA. Intractable diarrhea of infancy. Saudi J Gastroenterol. 1995;1:152–156. [PubMed] [Google Scholar]
- 10.Kleiman RE, Goulet O, Mieli-Vergani G, Sanderson IR, Sherman PM, Shneider BL. Walker's pediatric gastrointestinal disease: physiology, diagnosis, management. 5th ed. Hamilton: BC Decker Inc.; 2008. pp. 265–339. [Google Scholar]
- 11.Wyllie R, Hyams JS, Kay M. Pediatric Gastrointestinal and Liver disease. 4th ed. Philadelphia: Saunders Elsevier; 2011. pp. 106–118. [Google Scholar]
- 12.Guerrant RL, Oriá RB, Moore SR, Oriá MO, Lima AA. Malnutrition as an enteric infectious disease with long-term effects on child development. Nutr Rev. 2008;66:487–505. doi: 10.1111/j.1753-4887.2008.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lasekan JB, Jacobs J, Reisinger KS, Montalto MB, Frantz MP, Blatter MM. Lactose-free milk protein-based infant formula: impact on growth and gastrointestinal tolerance in infants. Clin Pediatr (Phila) 2011;50:330–337. doi: 10.1177/0009922810390511. [DOI] [PubMed] [Google Scholar]
- 14.Mao M, Yu T, Xiong Y, Wang Z, Liu H, Gotteland M, et al. Effect of a lactose-free milk formula supplemented with bifidobacteria and streptococci on the recovery from acute diarrhoea. Asia Pac J Clin Nutr. 2008;17:30–34. [PubMed] [Google Scholar]
- 15.Heubi J, Karasov R, Reisinger K, Blatter M, Rosenberg L, Vanderhoof J, et al. Randomized multicenter trial documenting the efficacy and safety of a lactose-free and a lactose-containing formula for term infants. J Am Diet Assoc. 2000;100:212–217. doi: 10.1016/S0002-8223(00)00065-1. [DOI] [PubMed] [Google Scholar]
- 16.Nizami SQ, Bhutta ZA, Molla AM. Efficacy of traditional rice-lentil-yogurt diet, lactose free milk protein-based formula and soy protein formula in management of secondary lactose intolerance with acute childhood diarrhoea. J Trop Pediatr. 1996;42:133–137. doi: 10.1093/tropej/42.3.133. [DOI] [PubMed] [Google Scholar]
- 17.de Mattos AP, Ribeiro TC, Mendes PS, Valois SS, Mendes CM, Ribeiro HC., Jr Comparison of yogurt, soybean, casein, and amino acid-based diets in children with persistent diarrhea. Nutr Res. 2009;29:462–469. doi: 10.1016/j.nutres.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Bhutta ZA, Nelson EA, Lee WS, Tarr PI, Zablah R, Phua KB, et al. Persistent Diarrhea Working Group. Recent advances and evidence gaps in persistent diarrhea. J Pediatr Gastroenterol Nutr. 2008;47:260–265. doi: 10.1097/MPG.0b013e318181b334. [DOI] [PubMed] [Google Scholar]
- 19.Lake AM. Beyond hydrolysates: use of L-amino acid formula in resistant dietary protein-induced intestinal disease in infants. J Pediatr. 1997;131:658–660. [PubMed] [Google Scholar]
- 20.Chehade M, Magid MS, Mofidi S, Nowak-Wegrzyn A, Sampson HA, Sicherer SH. Allergic eosinophilic gastroenteritis with protein-losing enteropathy: intestinal pathology, clinical course, and long-term follow-up. J Pediatr Gastroenterol Nutr. 2006;42:516–521. doi: 10.1097/01.mpg.0000221903.61157.4e. [DOI] [PubMed] [Google Scholar]
- 21.Lukacik M, Thomas RL, Aranda JV. A meta-analysis of the effects of oral zinc in the treatment of acute and persistent diarrhea. Pediatrics. 2008;121:326–336. doi: 10.1542/peds.2007-0921. [DOI] [PubMed] [Google Scholar]