Sir,
Diarrhea refers to the passage of loose or watery stools, and occurs at some point in the life of nearly every child. It continues to be a global problem in children, which accounts for 18% of child deaths and 13% of all disability-adjusted life years (DALYs).[1] In India diarrhea kills nearly 650 children a day.[2] WHO/UNICEF (2004) officially recommended reduced osmolarity oral rehydration salt (reduced ORS) solution and zinc supplement for the treatment of childhood diarrhea.[1,2] Many cases of acute diarrhea are caused by rotavirus. But diarrheal illnesses caused by viruses will improve in 2 or 3 days without the use of antibiotics. So the role of antimicrobials in the treatment of acute diarrhea is limited. Antimicrobials are indicated only in case of bloody diarrhea (shigella), suspected cholera, and severe malnutrition.[3] In many developing countries, suboptimal prescribing and overuse of marginally effective drugs have lead to treatment failure, spread of disease, increased resistance, high health care costs, and adverse effects.[4] Hence this study was undertaken to determine the extent of irrational prescribing of antibiotics for diarrhea in children under 5 years at a tertiary care hospital in Puducherry.
The scope of this study focuses on an audit of antimicrobials prescribed according to the standard WHO/UNICEF (2005) treatment guidelines for acute diarrhea. This was a prospective cross-sectional study with the objective of evaluating the appropriateness of antibiotics prescribed for childhood diarrhea and to establish the extent of advising ORS and zinc supplementation for childhood diarrhea. The study protocol was approved by the institute review board. Methodology of the study was simple, which used the data from a prospective prescription audit of 100 cases of acute diarrhea in children under 5 years visiting the outpatient department (OPD) at a tertiary care hospital in Puducherry for 2 months. Data regarding duration and type of diarrhea, intensity of dehydration, other co-morbid illnesses, degree of malnutrition, and laboratory tests to confirm infection was noted from medical record files. From the data, the generic name, dose, frequency, duration, and route of antibiotics prescribed were obtained. Zinc supplements prescribed were also noted. The personal information of the patients was not obtained and all the details of the patients obtained for the purpose of study were kept confidential.
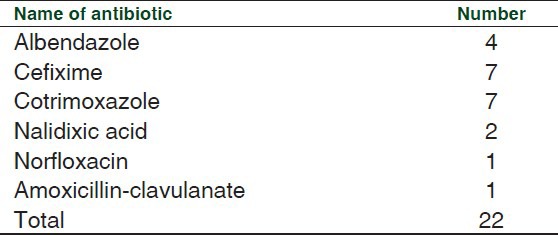
The percentage of patients receiving antibiotics and the patients prescribed with ORS and zinc adjunct was calculated. The appropriateness of the antimicrobials prescribed was also figured. Laboratory investigations were done for 16% of the patients. Out of which three samples had traces of red blood cells (RBCs) in stool culture and microscopy. A total of 71% of the patients were advised ORS and 68% were prescribed zinc [Figure 1]. Only 22 patients out of the 100 were prescribed antibiotics. The most commonly prescribed antibiotics were cotrimoxazole (7 cases) and cefixime (7 cases). The other drugs used were albendazole, nalidixic acid, norfloxacin, and amoxicillin-clavulanate [Table 1].
Figure 1.
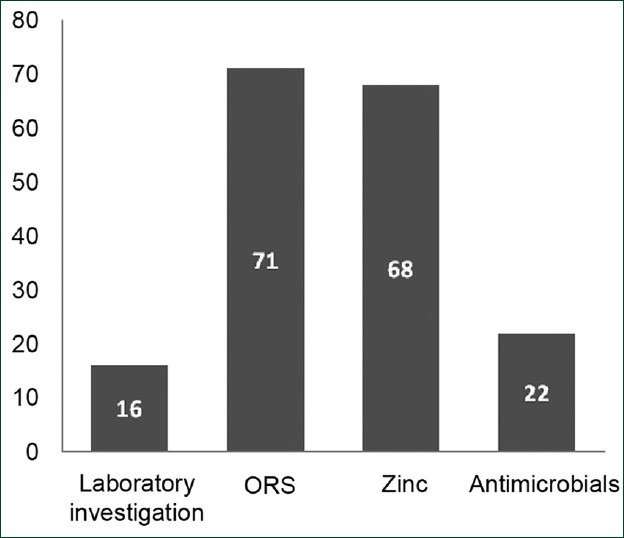
Number of patients in whom laboratory investigations done and ORS, zinc, antimicrobials prescribed
Table 1.
The antibiotics prescribed and the number of patients
Morbidity and mortality associated with childhood diarrhea continues to be a major concern despite the encouraging results of concerted efforts by National Community Driven Development (CDD) program. In developing countries, the scenario is worse due to infection, malnutrition, and illiteracy. One out of every five children who die of diarrhea worldwide is an Indian.[5] Indian Academy of Pediatrics (IAP) National task force have recommended ORS and oral zinc for childhood diarrhea.[6] But these guidelines are often violated and there are practitioners who do not usually follow the standard protocol for management of diarrhea. The problem is even more alarming because current teaching of medical students completely lacks thrust on proper case management of diarrhea. Antimicrobial treatment is recommended in a small fraction of cases such as dysentery, parasitic diseases, and severe cholera. In our study only 22% of the patients were prescribed antibiotics. The remaining patients were treated with ORS or zinc, whereas other studies have shown that the use of antibiotics were more and in most cases antibiotics were irrational too. According to the studies by Howteerakul et al. and Singh et al., the percentage of patients prescribed on antibiotics were 72.6% and 64%, respectively.[4,7] In a study by Lazzerini and Ronfani in Italy, it is evident that in children aged greater than 6 months with acute diarrhea, zinc supplementation may shorten the duration of diarrhea by around 10 hours.[8] Another study by Kouame et al., also supports the fact that oral zinc decreases the severity and reduces the number of episodes of diarrhea.[9] A study tested the hypothesis that daily supplementation of zinc had an effect on the clinical course of acute diarrhea, that is, frequency of stool, stool amount, and duration of acute diarrhea, in 117 children. Reduction in stool frequency per day was found to be 62% in the zinc-supplemented group and 26% reduction was found in the placebo-supplemented group.[5] The number of patients in whom zinc was not prescribed in our study was 32, hence from our observations we can state that prescriptions of 32% of the patients have violated the standard treatment protocol suggested by the IAP.
From the 100 patients considered in the study, stool culture and microscopy was done for only 16 cases. Among them, only three samples have shown traces of blood or pus and these patients were treated with antibiotics according to the treatment guidelines. Other than these 3 patients, antimicrobials were prescribed for 19 more patients. Irrational prescriptions were encountered in our study to a lesser extent. Antimicrobials should not be started unless the child has pus cells or RBC in the stool microscopy, severe protein energy malnutrition, obvious blood and mucus diarrhea, or associated systemic illness.[3] A relatively smaller sample size could also be a disadvantage of the study.
CONCLUSION
This study demonstrates that the number of irrational prescription of antibiotics in childhood diarrhea is less in our hospital and most of the prescriptions follow the standard treatment protocol suggested by the WHO.
REFERENCES
- 1.Fischer Walker CL, Fontaine O, Young MW, Black ER. Zinc and low osmolarity ORS for diarrhoea: A renewed call to action. Bull World Health Organ. 2009;87:780–6. doi: 10.2471/BLT.08.058990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gitanjali B, Weerasuriya K. The curious case of zinc for diarrhea: Unavailable, unprescribed and unused. J Pharmacol Pharmacother. 2011;2:225–9. doi: 10.4103/0976-500X.85933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanmaya M, Patil VD, Rajsekhar W, Hiremath MB. The role of antibiotics in childhood diarrhoea. Rec Res Sci Tech. 2010;2:55–6. [Google Scholar]
- 4.Howteerakul N, Hogginbotham N, Dibley MJ. Antimicrobial use in children under five years with diarrhoea in a central region province of Thailand. Southeast Asian J Trop Med Public Health. 2004;35:181–7. [PubMed] [Google Scholar]
- 5.Kouame KS, Verga ME, Pittet A, Rey-Bellet CG, Gehri M, Fontaine O, et al. Zinc and diarrhoea in children under 5 years: WHO recommendations implemented in Switzerland. Rev Med Suisse. 2012;8:1244–7. [PubMed] [Google Scholar]
- 6.Bhatnagar S, Lodha R, Choudhary P, Sachdev HP, Shah N, Narayan S, et al. IAP guidelines 2006 on management of acute diarrhea. Indian Pediatr. 2007;44:380–9. [PubMed] [Google Scholar]
- 7.Singh J, Bora D, Sachdeva V, Sharma RS, Verghese T. Prescribing patterns by doctors for acute diarrhea in children in Delhi, India. J Diarrhoeal Dis Res. 1995;13:229–31. [PubMed] [Google Scholar]
- 8.Bajait C, Thawani V. Role of zinc in pediatric diarrhea. Indian J Pharmacol. 2011;43:232–5. doi: 10.4103/0253-7613.81495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazzerini M, Ronfani L. Oral zinc for treating diarrhoea in children. Cochrane Database Syst Rev. 2012;6:CD005436. doi: 10.1002/14651858.CD005436.pub3. [DOI] [PubMed] [Google Scholar]


