Abstract
The present study examined the associations between religion and spirituality (R/S), presurgical distress, and other psychosocial factors such as engagement coping, avoidant coping, and social support. Participants were 115 men scheduled for surgery for urologic cancer. Before surgery, participants completed scales measuring intrinsic religiosity, organized religious activity, and nonorganized religious activity (IR, ORA, NORA); social support (Medical Outcomes Study Social Support Survey); and distress (Impact of Event Scale [IES], Perceived Stress Scale [PSS], Brief Symptom Inventory-18 [BSI-18], and Profile of Mood States [POMS]). R/S was positively associated with engagement coping. Social support was positively associated with engagement coping and inversely associated with POMS and PSS scores. Engagement coping was positively associated with IES and BSI scores, and avoidant coping was positively associated with all distress measures. R/S moderated the association between engagement coping and IES scores, such that the association between engagement coping and IES was not significant for men with high R/S scores (greater religious belief). R/S moderated the association between social support and distress; the inverse association between social support and PSS and POMS scores was only significant for men who scored high on R/S. This study replicated findings from previous studies suggesting that engagement and avoidant types of coping can lead to increased distress prior to surgery. Although R/S was associated with engagement coping, it was not associated with any of the distress measures. The finding that R/S moderated the associations between engagement coping and distress and social support and distress suggests that the association between R/S, coping style, social support, and adjustment to stressful life situations is not simplistic, and indirect associations should be explored.
Keywords: oncology, cancer, spirituality, religion, distress, surgery
Introduction
Psychosocial factors play an important role in psychological adjustment and emotional well-being during various stages of illness. Active coping and social support are among the psychosocial variables that have received the most consideration in this domain. Although such factors are often central to adjustment and recovery from illness, mounting evidence suggests that religion and spirituality (R/S) are also an important part of adjustment in many patient populations, particularly in those who have been diagnosed with a chronic and/or life-threatening disease.1 R/S has been reported to have a wide range of beneficial effects, including reduced levels of anxiety, depression, and pain2,3; increased ability to find meaning in illness4,5; increased hope and optimism6,7; and fewer admissions and shorter hospital stays.8 Specifically in cancer populations, R/S has been associated with self-reported enhanced well-being,9–11 decreased depression and anxiety,10,12 better role functioning and perceived physical health,13 improved family and social interactions,14,15 increased meaning and feelings of hope,16,17 increased optimism and inner peace, and preventing end-of-life despair.18,19
Several recent studies exploring nonreligious factors that may underlie or mediate the beneficial effects of R/S on various outcomes suggest that (1) R/S is used as a means of coping and social support in adjustment to illness; (2) R/S is often associated with factors such as active coping,20 optimism,13 social support,21 and social functioning13; and (3) the role of R/S in illness is often indirect, yet mediated by these nonreligious factors.6,7 For instance Ai and colleagues6,7 reported that R/S variables assessed preoperatively in cardiac patients were not directly associated with the main outcome of interest—postoperative adjustment—but were positively associated with positive coping styles6 and optimism,7 both of which were associated with adjustment following surgery.
Similar indirect or mediating associations between R/S and adjustment have also been reported in cancer populations. For instance, Canada et al20 reported that the associations between R/S and well-being and overall quality of life in ovarian cancer patients were mediated by active coping. In addition, Holland and colleagues22 did not find significant direct associations between R/S and mood, social support, or measures of distress in patients with malignant melanoma; however, R/S was associated with greater levels of active coping, which has been associated with better psychological adjustment during illness.23,24
In prostate cancer patients, mediating factors have helped explain the association between spirituality and mental and physical aspects of health-related quality of life25 and depression.26 Zavala et al25 reported that spirituality was associated with better mental health, fewer disease-specific symptoms, and reduced pain in men with metastatic prostate cancer; the authors attributed these results to individuals’ ability to find meaning/peace (which can be experienced in nonreligious individuals) as opposed to other factors such as religious faith. Similarly, Nelson et al26 reported that R/S was strongly associated with reduced depression and that the effect was mediated by the construct of meaning/peace. Taken together, these findings suggest that to better understand the role of R/S in health, nonreligious factors need to be explored in order to further elucidate potential mechanisms underlying the association.
Thus far, the majority of studies investigating R/S in cancer patients have been conducted during periods of time when patients have had several months to accept their diagnosis; are dealing with chronic, longer-term stressors such as undergoing chemotherapy or radiation; or when they have already completed much of their treatment. Under these circumstances, social support and engagement-type coping strategies have been found to be associated with better psychological and physical outcomes.23,24,27 In contrast, studies that have specifically studied adjustment prior to surgery, when patients are still trying to adjust to the recent news that they have a life-threatening illness, found that active/engagement and emotional support coping strategies are associated with greater distress before and directly following surgery.28–30 Furthermore, presurgical distress is likely exacerbated when scheduled to confirm a diagnosis. For example, in women who were scheduled for major gynecologic surgery, Cohen et al29 found that planning, reframing, emotional support, and religious coping were associated with distress and/or negative affect prior to surgery and positively predicted pain and morphine use following surgery. It should be noted, however, that avoidant forms of coping (eg, behavioral disengagement and denial) were associated with worse presurgery and postsurgery outcomes more consistently than the other forms of coping. These results suggest that many coping strategies (including forms of coping that are typically found to be adaptive during illness and treatment) may have a negative effect on recovery and adjustment around the time of diagnosis and surgery.
It is important to note, however, that these studies did not examine the effects of R/S coping, which has been indirectly associated with positive recovery outcomes.6,7 Thus, the aim of the present study was to explore the associations between R/S and distress during the early postdiagnosis and presurgical period. Given the lack of studies that have examined R/S during this time period and the association reported in previous studies between R/S and active coping, the present study investigated the possible direct and indirect effects of R/S on several measures of distress, coping, and social support preoperatively. We specifically studied men who were scheduled to have surgery for genitourinary cancer for 2 reasons. First, surgery is typically the first and primary treatment option for many genitourinary cancers,31 which underscores the importance of studying presurgical distress in this population and increases the likelihood of obtaining a large sample that had not yet undergone other treatment (thus precluding previous long-term psychological adjustment to cancer prior to surgery). Second, R/S has been associated with positive health outcomes during long-term survivorship in prostate cancer survivors.13 Assuming that there would be a range of R/S beliefs and coping styles, we sought to examine the associations between R/S and non-religious coping and social support during the early postdiagnosis and preoperative period.
Based on previous findings regarding the association between R/S and engagement-type coping20,22 and coping and presurgical distress,29 we developed the following hypotheses. First, we hypothesized that R/S would be positively associated with engagement-type coping behaviors (eg, active coping) and social support and inversely associated with measures of distress. Engagement coping and social support would also be positively associated with pre-surgical distress, based on the previously discussed findings. We also examined whether coping and social support would mediate effects of R/S on presurgical distress. In addition, we examined whether the association between engagement coping and social support would differ based on level of R/S. Thus, we were interested in exploring potential mediating and moderating effects among R/S, coping or social support, and distress.
Method
Participants
In all, 135 men who were scheduled to undergo surgery for urologic cancer were approached in the Urology Clinic at The University of Texas MD Anderson Cancer Center and 115 (85%) were eligible and gave consent. Patients were eligible if they were scheduled for surgery, were 18 years of age or older, did not have a serious comorbid illness, and spoke and read English. The majority of participants were diagnosed with prostate cancer (89%), 10% had renal cancer, and 1% had bladder cancer.
Procedures
During the preoperative visit, patients were approached by a research nurse who explained the nature of the study and obtained informed consent after patients agreed to participate. Participants completed a battery of measures that assessed several psychosocial factors, in addition to R/S assessments. The entire battery took about 30 minutes to complete. Participants who were unable to complete the entire battery during the presurgical appointment were able to take the questionnaires home and return them by mail. This study was approved by the Institutional Review Board at MD Anderson.
Measures
The questionnaires assessed a wide range of factors, including demographic variables such as age, gender, race, marital status, religious affiliation, and education; religious and spiritual beliefs and activities; coping style; social support; and distress.
R/S was assessed by 2 scales: The first scale measured intrinsic religiosity (IR). IR was measured by a 10-item scale that contains statements about religious beliefs or experience.32 Patients were asked to mark on a 1 to 5 scale the extent to which they believed each statement was true for them (score range: 10–50). Lower scores on this scale indicate greater religious beliefs; however, for analyses and interpretation purposes, we reversed the scores, such that higher IR scores represent greater religious beliefs. In this study sample, the internal reliability was high (Cronbach’s α = .90).
The second scale measured R/S activity using the Multidimensional Measurement of Religious/Spirituality for use in Health Research.33 The 2 subscales measured organized religious activity (ORA; a 2-item subscale) and nonorganized religious activity (NORA; a 3-item subscale). The ORA measured “religious service attendance” and “other public religious activities.” In the current sample, the reliability was moderate (Cronbach’s α = .75). The NORA measured private prayer and bible reading; in the current sample, the reliability was good (Cronbach’s α = .80). Because the correlations between IR, ORA, and NORA were high (rs range from 0.68 to 0.81; all P < .001) and results were similar whether analyses were conducted with individual R/S measures or combined, scores from the IR, ORA, and NORA were combined into a total R/S score to decrease the number of overall analyses. The internal reliability for the total R/S score in the current sample was very high (Cronbach’s α = .93). Although potential differences could exist between, for example, IR and ORAs, in this population, that was not the case.
Coping style was assessed using the Brief Coping Operations Preference Enquiry (Brief-COPE).34 The COPE measures a set of conceptually distinct coping subscales that include active coping, use of social support, turning to religion, positive reframing of the situation, and avoidant coping. In the present study, we examined the effects of coping sub-scales that would be characterized as either engagement- or avoidant-type coping based on a factor analysis reported by Perczek and colleagues.35 Using the Brief COPE, Perczek et al35 examined the effects of engagement- and avoidant-type coping on psychological adjustment in men being tested for urologic cancer. Based on this factor analysis, the subscales active coping, planning, acceptance, and positive reframing loaded onto 1 factor that was labeled “engagement coping,” whereas the subscales denial and behavioral disengagement loaded onto another distinct factor labeled “avoidant coping.” Because this cohort’s demographic, medical, and treatment stage characteristics were similar to the sample in the current study, we grouped these particular subscales into engagement- and avoidant-type coping classifications. Internal reliability for engagement-type coping was high (Cronbach’s α = .81). Internal reliability for avoidant-type coping in this sample was .69, which was higher than the internal reliability found by Perczek and colleagues (Cronbach’s α = .55).35
The Brief COPE also contains a subscale that measures religious coping. Although religious coping did not load onto the engagement or avoidant factors,35 we examined the extent to which it was associated with the IR, ORA, and NORA measures. Religious coping was highly correlated with each of the individual R/S measures (rs ranged from 0.64 to 0.83; all P < .001) as well as the combined R/S score (r = 0.82; P < .001). It should be noted that we did not include the religious coping subscale in the overall analyses because we selected R/S measures that were more comprehensive and specifically designed to assess a broader range of R/S beliefs and activities.
Social Support was measured using the Medical Outcomes Study Social Support Survey (MOS-SSS),36 which was developed with the 36-item Medical Outcomes Study Short-Form General Health Survey (SF-36) quality-of-life index and other MOS measures in one of the largest and most comprehensive studies of health status in the chronically ill. The scale focuses on the perception of the availability of social support in several areas, including emotional/information support, tangible support, positive interactions, and affective support. In the present sample, the internal reliability was very high (Cronbach’s α = .97).
Distress was measured using the Perceived Stress Scale (PSS),37 the Impact of Event Scale (IES),38 the Brief Symptom Inventory-18 (BSI-18),39 and the Profile of Mood States (POMS).40 The PSS is a 14-item scale that measures perceptions of ongoing stress. In the current sample, the internal reliability was .82.
The IES measures intrusive thoughts or the tendency to ruminate on or avoid thoughts about stressors. It is a 15-item self-report scale that assesses the 2 most common categories of responses to stressful events: intrusion (intrusively experienced ideas, images, feelings, or bad dreams) and avoidance (consciously recognized avoidance of certain ideas, feelings, or situations).38 This scale assesses cognitive processing in terms of how effectively patients are adapting to a stressful, traumatic event. For this study, patients were asked to rate the frequency of intrusive thoughts and avoidance behaviors related to their cancer. In the present sample, the internal reliabilities for the intrusive and avoidance subscales were .86 and .82, respectively. As the intrusive and avoidance subscales were highly correlated (r = 0.63; P < .001), we have reported and conducted analyses on the total IES scores; the internal reliability of the IES total was .89.
The BSI-18 consists of 18 items that assess different aspects of psychological distress, including depression, anxiety, and somatization, providing subscales in these areas and a global score.39) The internal reliabilities of the somatization, depression, and anxiety subscales were .60, .77, and .87, respectively. Because the correlations among the 3 sub-scales were high (rs range from 0.47 to 0.71; all P < .001), only the BSI global score was included in the analyses for simplification purposes. The internal reliability of the BSI global score for this sample was good (Cronbach’s α = .88).
The POMS, commonly used in cancer research, is a mood adjective checklist containing 6 subscales: tension-anxiety, depression-dejection, anger-hostility, vigor, fatigue, and confusion-bewilderment. A shortened version of the POMS (POMS-SF) that included 37 items was used, for which convergent and discriminant validity of the 6 sub-scales and total mood disturbance (TMD) score have been established.41 The reliability for the TMD in this sample was high (Cronbach’s α = .91).
Statistical Analyses
Descriptive statistics, including means, standard deviations (SDs), and ranges, were computed for each of the demographic variables and overall and subscale scores for the psychosocial measures. The associations of interest were examined first by calculating partial correlation coefficients between variables after covarying age, race, and education level (see below). Subsequently, multiple regression equations were computed to test whether coping or social support mediated the effects of R/S on distress and to assess whether R/S moderated the effects of coping or social support on distress. The criteria to conduct mediator analyses on R/S, coping or social support, and distress were not met because R/S was not directly associated with any of the measures of presurgical distress.42
Results
Descriptive Analyses
The participants’ average age was 58.3 years (range: 19–84 years; SD = 11.3), and most were Caucasian (75%), married or living with a partner (90%), were of Christian faith (either Catholic or Protestant) (93%), and had some college education (71%). On average, patients completed questionnaires 7 days prior to surgery (range: 1–29 days; SD = 6.7). The descriptive analyses for the psychosocial variables are reported in Table 1.
Table 1.
Psychosocial Variablesa
| Variable | Mean | SD | Range |
|---|---|---|---|
| R/S (combined IR, ORA, and NORA) | 45.7 | 18.2 | 16–88 |
| Brief COPE | |||
| Engagement | 15.3 | 5.5 | 3–24 |
| Avoidant | 1.2 | 2.1 | 0–10 |
| Social support | 63.8 | 10.4 | 27–72 |
| PSS | 19.8 | 6.2 | 4–38 |
| IES | 16.0 | 9.3 | 0–38 |
| BSI Global | 48.4 | 10.7 | 34–74 |
| POMS | 5.9 | 19.7 | −22 to 87 |
Abbreviations: SD, standard deviation; R/S, religion and spirituality; IR, intrinsic religiosity; ORA, organized religious activity; NORA, nonorganized religious activity; COPE, coping operations preference enquiry; PSS, Perceived Stress Scale; IES, Impact of Event Scale; BSI, Brief Symptom Inventory; POMS, Profile of Moods States.
It should be noted that some measures include an n lower than 115; the lowest n for any measure was 96.
Participants reported low to moderate levels of distress (see Table 1). Based on normative data from cancer populations, the patients’ mean BSI global scores fell within the 42nd and 46th percentiles.43 However, mean total POMS scores of the current sample were quite a bit lower than normative data based on a male mixed cancer population (mean = 18.0).44 Patients’ mean total IES and PSS scores were similar to those of patients with urologic cancer in other studies (eg, IES = 17.5445; PSS = 19.7646).
Correlation Analyses
To identify covariates, we examined associations between demographic and medical factors (ie, age, race, marital status, level of education, and diagnosis) and R/S, distress, and coping and social support measures. Age was inversely associated with BSI scores (r = −.20; P = .032). In addition, there were significant differences across race and level of education with regard to avoidant coping, such that participants who were not Caucasian (non-Caucasian mean = 2.23; Caucasian mean = 0.86; SD = 2.07; P = .002) and had not completed some level of college (no college mean = 2.03; some college mean = .85; SD = 1.19; P = .006) engaged in more avoidant coping. No other medical or demographic factors were significantly related to the outcome measures. Thus, age, race, and level of education were entered into regression analyses as covariates.
Correlation coefficients for R/S, coping, social support, and outcome measures are presented in Table 2. After controlling for age, race, and education level, R/S was significantly positively correlated with engagement coping (r = 0.43; P < .001). Social support was inversely correlated with POMS scores (r = −0.27; P = .011) and PSS scores (r = −0.20; P = .033) and positively correlated with engagement coping (r = 0.25; P = .016). Engagement coping was positively associated with both IES (r = 0.36; P < .001) and BSI scores (r = 0.32; P = .002). In addition, avoidant coping was positively associated with all outcome measures: PSS (r = 0.49; P < .001), POMS (r = 0.57; P < .001), IES (r = 0.42; P < .001), and BSI (r = 0.51; P < .001). All the distress measures were moderately to highly correlated with each other (r’s ranging from 0.50 to 0.84; all P < .001). No other associations were statistically significant.
Table 2.
Partial Correlations Between R/S, Coping, Social Support, and Distress Measuresa
| POMS | PSS | BSI Global | IES | Social Support | Avoidant Coping | Engagement Coping | |
|---|---|---|---|---|---|---|---|
| IR_ORA_NORA | 0.17 | 0.16 | 0.03 | −0.03 | −0.14 | 0.06 | 0.43** |
| Engagement coping | 0.01 | 0.14 | 0.32** | 0.36** | 0.25* | 0.17 | — |
| Avoidant coping | 0.57** | 0.49** | 0.51** | 0.42** | −0.16 | — | — |
| Social support | −0.27** | −0.31* | −0.09 | 0.03 | — | — | — |
| IES | 0.54** | 0.50** | 0.55** | — | — | — | — |
| BSI Global | 0.84** | 0.53** | — | — | — | — | — |
| PSS | 0.70** | — | — | — | — | — | — |
Abbreviations: R/S, religion and spirituality; IR, intrinsic religiosity; ORA, organized religious activity; NORA, nonorganized religious activity; POMS, Profile of Moods States; PSS, Perceived Stress Scale; BSI, Brief Symptom Inventory; IES, Impact of Event Scale.
Partial correlations controlling for age, race, and education level.
P < .05;
P < .005.
Mediator Analyses
The criteria to conduct mediator analyses on R/S, coping or social support, and distress were not met because R/S was not directly associated with any of the distress measures.42
Moderator Analyses
We examined whether R/S moderated the effects of coping and social support on distress. Individual regression equations were computed in SAS for each predictor by entering the predictor (engagement coping and avoidant coping or social support), the moderator (R/S), and the interaction between the predictor and moderator and the covariates (age, race, and level of education). A similar approach was taken to examine whether age, education, or race moderated the association of R/S and coping or social support with distress. The interactions were tested as continuous variables; however, we used median splits to further examine the nature of the interaction.47 Standard ordinary least-squares statistical and graphical diagnostic procedures were conducted for regression analyses. Based on statistical and graphical criteria, no heteroscedasticity was detected and no observations were excluded as outliers or influential points. In addition, problematic levels of multicollinearity were not observed among the explanatory variables within the regression models.
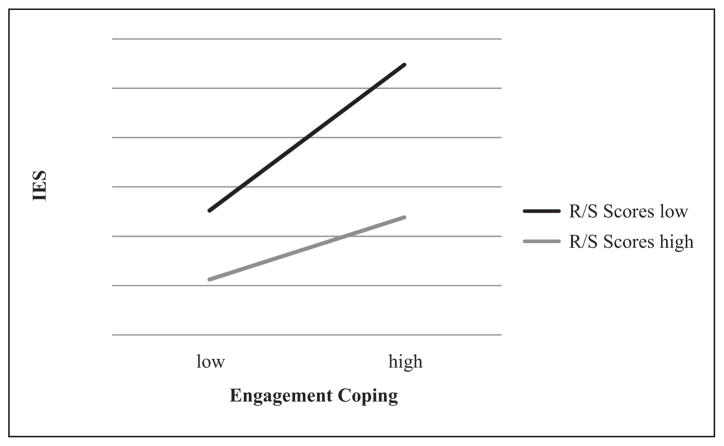
Regression analyses revealed that the interaction between R/S and engagement coping was significantly associated with IES scores (β = 0.85; P = .006; Figure 1). A graph of simple slopes, derived by plotting the regression line at 1 SD above and below the mean, demonstrated that for those who had lower R/S scores (based on a median split of R/S scores), greater engagement coping was associated with greater distress (r = 0.64; P < .001); however, there was no significant association between engagement coping and IES scores in men who had higher R/S scores (r = 0.08; P = .6).
Figure 1.
Association between engagement coping and IES moderated by R/S
Abbreviations: R/S, religion and spirituality; IES, Impact of Event Scale.
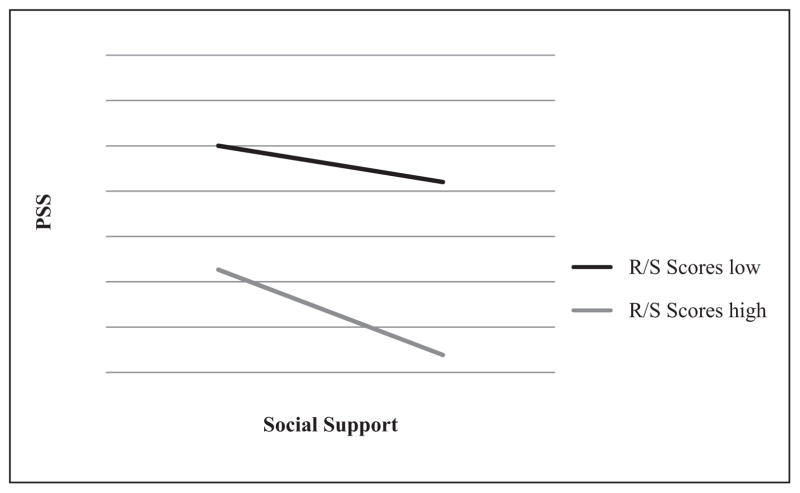
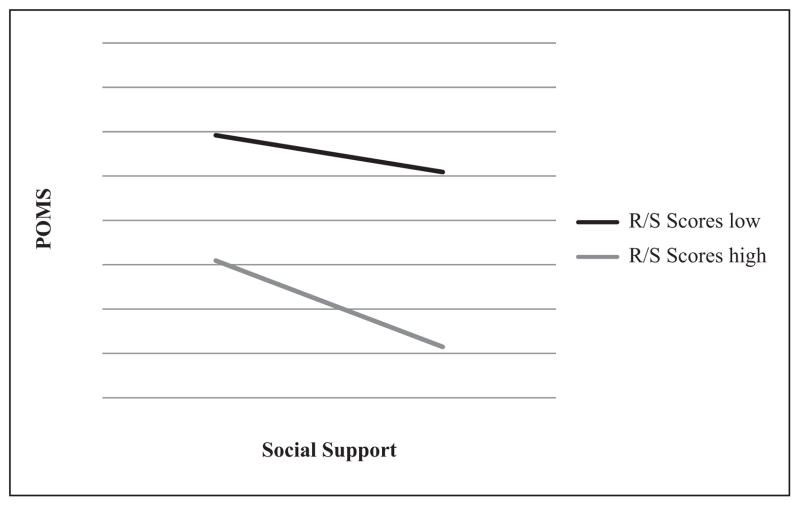
Regression analyses also revealed that the interaction between R/S and social support was significantly associated with PSS (β = 1.43; P < .02) and POMS (β = 1.43; P < .03) scores (Figures 2 and 3). A graph of simple slopes, derived by plotting the regression lines at 1 SD above and below the mean, revealed a nonsignificant association between social support and PSS (r = −0.18; P = .188) and POMS (r = −0.20; P = .160) scores for men who scored low on R/S. In contrast, there was a significant inverse association between social support and PSS (r = −0.43; P = .002) and POMS (r = −0.35; P = .016) scores among men who scored high on R/S. The interaction between R/S and avoidant coping was not associated with any of the distress measures.
Figure 2.
Association between social support and PSS moderated by R/S
Abbreviations: R/S, religion and spirituality; PSS, Perceived Stress Scale.
Figure 3.
Association between social support and POMS moderated by R/S
Abbreviations: R/S, religion and spirituality; POMS, Profile of Moods States.
Exploration of whether age, education, or race moderated any of the outcomes only revealed an interaction between R/S and education associated with PSS (β = 0.87; P < .02; Figure 4). A graph of simple slopes, derived by plotting the regression lines at 1 SD above and below the mean, illustrated that for those reporting low R/S, greater education was associated with greater perceived stress (r = −0.25; P = .047), whereas for those reporting high R/S, greater education was not significantly associated with perceived stress (r = 0.169; P = .252).
Figure 4.
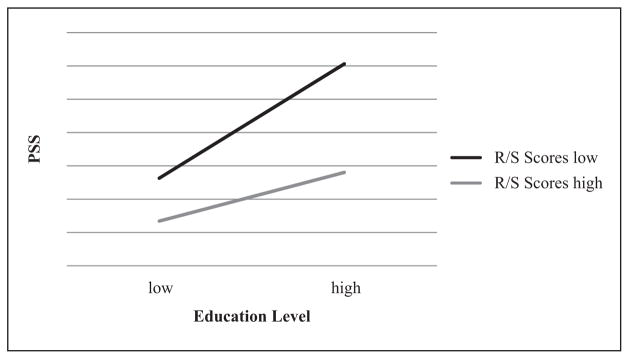
Association between education and PSS moderated by R/S
Abbreviations: R/S, religion and spirituality; PSS, Perceived Stress Scale.
Discussion
This study examined the effects of R/S, coping, and social support on presurgical distress in male urologic cancer patients and the nature (ie, direct or indirect) of the association between R/S and distress outcomes. Consistent with our hypotheses, R/S was positively associated with engagement coping; however, R/S was not associated with avoidant coping, social support, or the measures of distress. As such, a possible association between R/S and distress was not supported via a mediational model. Social support was inversely associated with distress (POMS and PSS scores) but was positively associated with engagement coping. Furthermore, engagement coping was positively associated with distress (IES and BSI measures), and avoidant coping was positively associated with all measures of distress. The finding that both forms of coping were associated with distress, with avoidant coping being associated to a greater extent, is consistent with previous findings.18
Although it was not directly associated with the measures of distress in the current study, R/S was positively associated with engagement coping, which was positively associated with IES and BSI distress measures. However, R/S was found to buffer the effects of engagement-type coping on intrusive thoughts and avoidance behaviors, suggesting that for men scoring higher on R/S, engagement coping was not associated with higher intrusive thoughts and avoidance behaviors. In addition, R/S moderated the effects of social support on distress, such that the inverse association between social support and perceived stress and mood disturbance was only significant in individuals with higher R/S scores. This suggests that the association between R/S and distress is complex, because R/S buffered the negative effects of engagement coping on presurgical distress, and that the beneficial effects of social support reducing presurgical distress was only apparent in men who scored high on R/S.
In contrast to findings reported by Cohen and colleagues,29 R/S was not associated with worse distress outcomes in the present study, which is particularly noteworthy given the high association between the religious subscale from the Brief COPE and the combined R/S scores (r = 0.82; P < .001). Although both cohorts were assessed within the presurgical environment, the sample from Cohen et al29 consisted of a large proportion of patients who did not have a cancer diagnosis. Perhaps patients who receive a cancer diagnosis contemplate life and death issues to a greater extent, finding comfort and or acceptance in R/S. However, additional studies are required to address these seemingly disparate results.
Similar to results from previous studies, both engagement and avoidant forms of coping were associated with greater distress, and the association between avoidant coping and distress was more consistent across distress measures in the presurgical environment. Such findings would seem to be counterintuitive because engagement coping behaviors are often beneficial during illness.23,24,27 However, we made the distinction previously between circumstances in which patients have had time to accept a cancer diagnosis and are undergoing long-term treatment and distress that follows a recent cancer diagnosis around the time of surgery. Under these latter conditions, patients are attempting to cope with major stressors (ie, cancer diagnosis and surgery) over which they have little control. In contrast, patients with chronic disease who undergo long-term treatment (eg, chemotherapy) have had time to adjust to their diagnosis, treatment plan, and prognosis and would likely benefit from taking a proactive approach in coping with their current and future quality of life. Because many patients typically respond to illness-related issues with engagement types of coping, the finding that R/S buffers the association between engagement coping and distress prior to surgery is a particularly interesting and important finding with regard to psychosocial factors that may prevent or alleviate presurgical distress. Although R/S could be considered a form of adaptive coping, perhaps its buffering effect on the association between engagement coping and IES scores stems from placing the burden of an uncertain outcome on a higher power, resulting in fewer intrusive thoughts or avoidant behaviors caused by distress. Of course, further investigation of the hypothesized mechanisms underlying the moderating effects of R/S on IES scores is needed.
Social support has been reported to have significant beneficial effects in cancer patients across various types and stages of disease.27 Based on these findings, the moderating effects of R/S on the association between social support and POMS and PSS scores were somewhat unexpected because the negative association between social support and distress scores was only significant for patients who characterized themselves as more religious and/or spiritual. This is especially interesting given that there was no significant association between R/S and social support. As a similar percentage of patients in the study were married or living with a partner in both high R/S (39%) and low R/S (41%) groups, the moderating effect of R/S on the benefits of social support is likely a result of some other source of support. Perhaps social support from a religious community (eg, local parish) is the driving factor of the association between social support and decreased distress in R/S patients. Such findings provide further support for the critical role of social support in R/S assessments, such as the Spiritual Beliefs Inventory (SBI) inventory.48 Our finding of an inverse association between social support and presurgical distress suggests that provision of additional social support (eg, through individual or group interventions) may be beneficial for patients prior to surgery. Extra social support for elderly men may be especially helpful because research has shown that their support network is typically limited to a spouse or partner,49 and individual and group interventions have been associated with beneficial outcomes for men with prostate cancer.50–53
There are some limitations to this study. First, the R/S measures used in this study did not address more specific aspects of R/S. For instance, several studies have found that patients can draw on R/S beliefs to cope in a negative way, such that they feel that they are being punished or abandoned by God.54 As a result, such beliefs may be linked with greater distress, which may have played a role in the associations between religious coping and worse outcomes that have been reported previously.29 In addition, we only assessed 1 aspect of adjustment (ie, distress) and not other aspects such as growth, optimism, or finding meaning/purpose in life. Indeed, future research should address the role of R/S in other aspects of adjustment during the postdiagnosis, preoperative period in cancer patients, given the lack of current research in this area.
Second, this study was conducted at a large comprehensive cancer hospital, which includes treatment regimens and resources that may differ from the standard of care offered at local hospitals and treatment centers. Third, the generalizability of these findings to other cancer populations with various demographic characteristics is limited given that the current patient sample was primarily composed of Caucasian males with prostate cancer who were of Christian faith. In addition, the cross-sectional design of the study (ie, acquiring data at 1 time point) limits the extent to which we can infer the causation of these associations. To truly understand the associations between R/S and distress in the presurgical environment, future research in this area should use a prospective longitudinal design to assess these associations and potential changes over time.
These results, as well as findings from previous studies, suggest that various factors, particularly several forms of coping, are associated with increased distress during the postdiagnosis, presurgical period in prostate cancer patients and that R/S beliefs and activities may help decrease distress in this environment. These findings have clinical implications as well. There is much evidence to suggest that physician–patient communication can influence medical outcomes.55 Accordingly, patients may benefit from physicians being open and supportive of their religious and spiritual beliefs,1 particularly as they pertain to a recent cancer diagnosis. It should be noted that because many patients may not be religious or spiritual, or participate in R/S activities, it is important to further study the mechanisms underlying the benefits of R/S (eg, additional forms of social support) reported in this study in order to address the needs of culturally diverse patient populations. In summary, our findings suggest that the associations among R/S, coping style, social support, and adjustment to stressful life situations is not simplistic, and indirect associations should be further explored.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Reprints and permission: http://www.sagepub.com/journalsPermissions.nav
This work was conducted at The University of Texas M D Anderson Cancer Center.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Koenig HG. Religion, spirituality, and medicine: research findings and implications for clinical practice. South Med J. 2004;97:1194–1200. doi: 10.1097/01.SMJ.0000146489.21837.CE. [DOI] [PubMed] [Google Scholar]
- 2.Koenig HG, George LK, Peterson BL. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998;155:536–542. doi: 10.1176/ajp.155.4.536. [DOI] [PubMed] [Google Scholar]
- 3.McCullough ME, Larson DB. Religion and depression: a review of the literature. Twin Res. 1999;2:126–136. doi: 10.1375/136905299320565997. [DOI] [PubMed] [Google Scholar]
- 4.Bush EG, Rye MS, Brant CR, Emery E, Pargament KI, Riessinger CA. Religious coping with chronic pain. Appl Psychophysiol Biofeedback. 1999;24:249–260. doi: 10.1023/a:1022234913899. [DOI] [PubMed] [Google Scholar]
- 5.Büssing A, Ostermann T, Matthiessen P. The role of religion and spirituality in medical patients in Germany. J Relig Health. 2005;44:321–340. doi: 10.1186/1477-7525-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ai AL, Park CL, Huang B, Rodgers W, Tice TN. Psychosocial mediation of religious coping styles: a study of short-term psychological distress following cardiac surgery. Pers Soc Psychol Bull. 2007;33:867–882. doi: 10.1177/0146167207301008. [DOI] [PubMed] [Google Scholar]
- 7.Ai AL, Peterson C, Tice TN, Huang B, Rodgers W, Bolling SF. The influence of prayer coping on mental health among cardiac surgery patients: the role of optimism and acute distress. J Health Psychol. 2007;12:580–596. doi: 10.1177/1359105307078164. [DOI] [PubMed] [Google Scholar]
- 8.Koenig HG, Larson DB. Use of hospital services, religious attendance, and religious affiliation. South Med J. 1998;91:925–932. doi: 10.1097/00007611-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Gall TL, Miguez de Renart RM, Boonstra B. Religious resources in long-term adjustment to breast cancer. J Psychosoc Oncol. 2000;18:21–38. [Google Scholar]
- 10.Gall T. Integrating religious resources within a general model of stress and coping: long-term adjustment of breast cancer. J Relig Health. 2000;39:167–182. [Google Scholar]
- 11.Meraviglia MG. The effects of spirituality on well-being of people with lung cancer. Oncol Nurs Forum. 2004;31:89–94. doi: 10.1188/04.ONF.89-94. [DOI] [PubMed] [Google Scholar]
- 12.Baider L, Russak SM, Perry S, et al. The role of religious and spiritual beliefs in coping with malignant melanoma: an Israeli sample. Psychooncology. 1999;8:27–35. doi: 10.1002/(SICI)1099-1611(199901/02)8:1<27::AID-PON334>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 13.Gall TL. Relationship with God and the quality of life of prostate cancer survivors. Qual Life Res. 2004;13:1357–1368. doi: 10.1023/B:QURE.0000040789.49691.59. [DOI] [PubMed] [Google Scholar]
- 14.Yoshimoto SM, Ghorbani S, Baer JM, et al. Religious coping and problem-solving by couples faced with prostate cancer. Eur J Cancer Care (Engl) 2006;15:481–488. doi: 10.1111/j.1365-2354.2006.00700.x. [DOI] [PubMed] [Google Scholar]
- 15.Chan YM, Ngan HY, Yip PS, Li BY, Lau OW, Tang GW. Psychosocial adjustment in gynecologic cancer survivors: a longitudinal study on risk factors for maladjustment. Gynecol Oncol. 2001;80:387–394. doi: 10.1006/gyno.2000.6093. [DOI] [PubMed] [Google Scholar]
- 16.Gall TL, Cornblat M. Breast cancer survivors give voice: a qualitative analysis of spiritual factors in long-term adjustment. Psychooncology. 2002;11:524–535. doi: 10.1002/pon.613. [DOI] [PubMed] [Google Scholar]
- 17.Fehring RJ, Miller JF, Shaw C. Spiritual well-being, religiosity, hope, depression, and other mood states in elderly people coping with cancer. Oncol Nurs Forum. 1997;24:663–671. [PubMed] [Google Scholar]
- 18.Ayele H, Mulligan T, Gheorghiu S, Reyes-Ortiz C. Religious activity improves life satisfaction for some physicians and older patients. J Am Geriatr Soc. 1999;47:453–455. doi: 10.1111/j.1532-5415.1999.tb07238.x. [DOI] [PubMed] [Google Scholar]
- 19.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361:1603–1607. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- 20.Canada AL, Parker PA, Basen-Engquist K, de Moor JS, Ramondetta LM. Active coping mediates the association between religion/spirituality and functional well-being in ovarian cancer. Gynecol Oncol. 2005;99(3, suppl 1):S125. doi: 10.1016/j.ygyno.2005.07.057. [DOI] [PubMed] [Google Scholar]
- 21.Choumanova I, Wanat S, Barrett R, Koopman C. Religion and spirituality in coping with breast cancer: perspectives of Chilean women. Breast J. 2006;12:349–352. doi: 10.1111/j.1075-122X.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- 22.Holland JC, Passik S, Kash KM, et al. The role of religious and spiritual beliefs in coping with malignant melanoma. Psychooncology. 1999;8:14–26. doi: 10.1002/(SICI)1099-1611(199901/02)8:1<14::AID-PON321>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 23.Fawzy FI, Cousins N, Fawzy NW, Kemeny ME, Elashoff R, Morton D. A structured psychiatric intervention for cancer patients. I. Changes over time in methods of coping and affective disturbance. Arch Gen Psychiatry. 1990;47:720–725. doi: 10.1001/archpsyc.1990.01810200028004. [DOI] [PubMed] [Google Scholar]
- 24.Heim E, Valach L, Schaffner L. Coping and psychosocial adaptation: longitudinal effects over time and stages in breast cancer. Psychosom Med. 1997;59:408–418. doi: 10.1097/00006842-199707000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Zavala MW, Maliski SL, Kwan L, Fink A, Litwin MS. Spirituality and quality of life in low-income men with metastatic prostate cancer. Psychooncology. 2009;18:753–761. doi: 10.1002/pon.1460. [DOI] [PubMed] [Google Scholar]
- 26.Nelson C, Jacobson CM, Weinberger MI, et al. The role of spirituality in the relationship between religiosity and depression in prostate cancer patients. Ann Behav Med. 2009;38:105–114. doi: 10.1007/s12160-009-9139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parker PA, Baile WF, de Moor C, Cohen L. Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psychooncology. 2003;12:183–193. doi: 10.1002/pon.635. [DOI] [PubMed] [Google Scholar]
- 28.Cohen F, Lazarus RS. Active coping processes, coping dispositions, and recovery from surgery. Psychosom Med. 1973;35:375–389. doi: 10.1097/00006842-197309000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Cohen L, Fouladi RT, Katz J. Preoperative coping strategies and distress predict postoperative pain and morphine consumption in women undergoing abdominal gynecologic surgery. J Psychosom Res. 2005;58:201–209. doi: 10.1016/j.jpsychores.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 30.George JM, Scott DS, Turner SP, Gregg JM. The effects of psychological factors and physical trauma on recovery from oral surgery. J Behav Med. 1980;3:291–310. doi: 10.1007/BF00845053. [DOI] [PubMed] [Google Scholar]
- 31.Berglund RK, Jones JS, Ulchaker JC, et al. Radical prostatectomy as primary treatment modality for locally advanced prostate cancer: a prospective analysis. Urology. 2006;67:1253–1256. doi: 10.1016/j.urology.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Hoge DR. A validated intrinsic religious motivation scale. J Sci Study Relig. 1972;11:369–376. [Google Scholar]
- 33.John Fetzer Institute. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Kalamazoo, MI: John Fetzer Institute; 1999. [Google Scholar]
- 34.Carver CS. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 35.Perczek RE, Burke MA, Carver CS, Krongrad A, Terris MK. Facing a prostate cancer diagnosis: who is at risk for increased distress? Cancer. 2002;94:2923–2929. doi: 10.1002/cncr.10564. [DOI] [PubMed] [Google Scholar]
- 36.Sherbourne CD, Stewart AL. The Medical Outcome Study Social Support Survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 37.Cohen S, Kamarck T, Mermelstein RF. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 38.Horowitz M, Wilner N, Alvarez W. Impact of Events Scale: measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Derogatis LR. Brief Symptom Inventory: Administration, Scoring and Procedures Manual. 3. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 40.McNair DM, Lorr M, Droppleman LF. Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1971/1981. [Google Scholar]
- 41.Baker F, Denniston M, Zabora J, Polland A, Dudley WN. A POMS short form for cancer patients: psychometric and structural evaluation. Psychooncology. 2002;11:273–281. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- 42.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychology research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 43.Derogatis LR. Brief Symptom Inventory: Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- 44.Cassileth BR, Lusk EJ, Brown L, Cross P. Psychosocial status of cancer patients and next of kin: normative data from the Profile of Mood States. J Psychosoc Oncol. 1985;3:99–105. [Google Scholar]
- 45.Bisson JI, Chubb HL, Bennett S, Mason M, Jones D, Kynaston H. The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU Int. 2002;90:56–61. doi: 10.1046/j.1464-410x.2002.02806.x. [DOI] [PubMed] [Google Scholar]
- 46.Joseph H, Thibault G, Ruttle-King J. Perceived stress and quality of life among prostate cancer survivors. Mil Med. 2006;171:425–429. doi: 10.7205/milmed.171.5.425. [DOI] [PubMed] [Google Scholar]
- 47.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 48.Holland JC, Kash KM, Passik S, et al. A brief spiritual beliefs inventory for use in quality of life research in life-threatening illness. Psychooncology. 1998;7:460–469. doi: 10.1002/(SICI)1099-1611(199811/12)7:6<460::AID-PON328>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 49.Antonucci T, Akiyama H. An examination of sex differences in social support among older men and women. Sex Roles. 1987;17:737–749. [Google Scholar]
- 50.Carmack Taylor CL, Demoor C, Smith MA, et al. Active for Life After Cancer: a randomized trial examining a lifestyle physical activity program for prostate cancer patients. Psychooncology. 2006;15:847–862. doi: 10.1002/pon.1023. [DOI] [PubMed] [Google Scholar]
- 51.Cohen L, Parker PA, Vence L, et al. Presurgical stress management improves postoperative immune function in men with prostate cancer undergoing radical prostatectomy. Psychosom Med. 2011;73:218–225. doi: 10.1097/PSY.0b013e31820a1c26. [DOI] [PubMed] [Google Scholar]
- 52.Parker PA, Pettaway CA, Babaian RJ, et al. The effects of a presurgical stress management intervention for men with prostate cancer undergoing radical prostatectomy. J Clin Oncol. 2009;27:3169–3176. doi: 10.1200/JCO.2007.16.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lepore SJ, Helgeson VS, Eton DT, Schulz R. Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychol. 2003;22:443–452. doi: 10.1037/0278-6133.22.5.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pargament KI, Smith B, Koenig HG, Perez L. Patterns of positive and negative religious coping with major life stressors. J Sci Study Relig. 1998;37:711–725. [Google Scholar]
- 55.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]